Abstract
Background:
Trunk muscles play an important role in providing both mobility and stability during dynamic tasks in athletes. The purpose of this study was to evaluate the within-day and between-day reliability of ultrasound (US) in measuring abdominal and lumbar multifidus muscle (MF) thickness in athletes with and without hamstring strain injury (HSI).
Methods:
Fifteen male soccer players (18-30 years old) with and without HSI were evaluated using two US probes (50 mm linear 7.5 MHZ and 70 mm curvilinear 5 MHz). The abdominal muscle thickness as well as the cross sectional area (CSA) of the MF was measured. To determine within and between days reliabilities, the second and third measurements were repeated with two hours and one week intervals, respectively.
Results:
Intraclass correlation coefficients for athletes with and without HSI demonstrated good to high reliability for the abdominal muscle thickness (0.82 and 0.93) and CSA of the MF muscle (0.84 and 0.89, respectively).
Conclusion:
Our results indicated that US seemed to be a reliable instrument to measure abdominal and lumbar multifidus muscle thickness in soccer players with and without HSI. However, further studies are recommended to support the present study findings in other athletes.
Key Words: ower limb, train, Ultrasound imaging
Introduction
Hamstring strain injury (HSI) is a commonly seen soft tissue injury in athletes doing sports activities with rapid acceleration and deceleration, such as soccer (1, 2). The rate of HSI has been shown from 12% to 16% for various sports, like soccer, Australian football, and other sports (3, 4). Following HSI, athletes may miss at least two to three games that it is often harmful physically and costly (5). Hamstring strain injury often occurs at the late of swing phase of kicking or sprinting when the knee is fully extended (6). Regarding to several risk factors in HSI, functional, anatomical, and morphological characteristics of the hamstring muscle partly demonstrate the causes of injury (7-10). As the biarticular nature of the hamstring muscle links this muscle to lumbopelvic region, screening the lumbopelvic muscles seems valuable to identify more related risk factors.
Correct dynamic neuromuscular control and intact passive structures are necessary to create stability in lumbopelvic region (11). This stable base is created by lumbopelvic muscles during the dynamic athletic activities (12, 13). Thus, disturbed neuromuscular control and impaired passive structure in this region may potentially develop HSI (14).
All abdominal muscles such as internal oblique (IO), transversus abdominis (TrA), external oblique (EO), and lumbar multifidus (MF) muscles are possibly associated with the lumbopelvic region stability (15-19).
To assess the alterations in the muscles’ role and morphology, different methods such as electromyography (EMG), magnetic resonance imaging (MRI), and rehabilitative ultrasound (US) are available (20-25). Among these methods, US seems to be an efficient and non-invasive technique to evaluate muscle thickness and cross sectional area (26, 27).
Hides (2014) et al. assessed MF muscle size in elite football players using US and reported a mean ICC of 0.93 for the reliability (28). In other study, Mf muscle and quadratus lumborum muscle size were measured using US in Australian Football League players and findings demonstrated high reliability (ICC = 0.93 to 0.99) (21). Numerous studies examined muscles size of lumbopelvic region in athletes using MRI, but there are few studies indicating the US reliability regarding quantitative assessment of lumbar and abdominal muscle width in soccer players with and without HSI (14, 22, 29, 30). As it seems that lumbar stabilizer muscles may have different sizes in athletes with and without hamstring injuries, reliability study is necessary for both evaluating the muscle dimensions and assessing the effect of any therapeutic intervention. Therefore, the present study aimed at determining the within and between-day reliability of US for assessing abdominal and lumbar multifidus muscles width among athletes with/without HSI.
Materials and Methods
Subjects
Fifteen male soccer players without HSI and 15 male soccer players with HSI were included in this methodological study (31, 32). All participants were free of any current low back pain, history of surgery in lumbar and lower limb, neurological disease, knee injuries, and ankle sprain. Hamstring strain injury was defined as a sudden pain in the thigh muscles (hamstring region) during training or competition which makes athletes to miss their physical activities for at least one week (33). Healthy soccer players were free of HSI, but soccer players with HSI had a history of grade II HSI during the last 6 months to one year. All participants were assessed by team physiotherapist or physician using MRI studies or medical documents. The subjects signed and completed an informed consent form.
Procedure
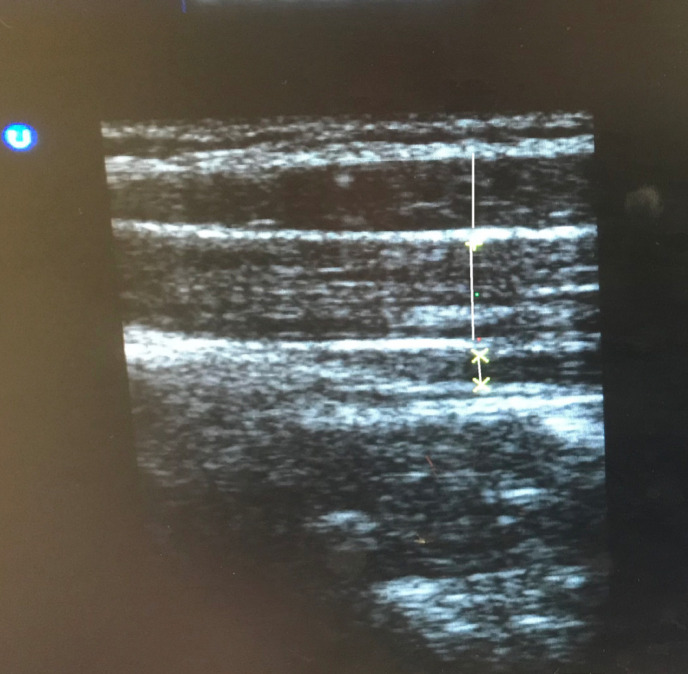
All cases were referred to the laboratory on two different days. The first and second measurements were carried out with two hours interval in one day (within-day reliability), and the third was performed following one week interval (between-day reliability). For abdominal muscle measurement (EO, IO, and TrA), participants were asked to lay on a padded wooden table in a supine hook-lying posture placing the hand beside the trunk, while locating the linear probe (7.5 MHZ) at the axial line among the iliac crest and the twelfth rib and moving to observe the muscle’s medial edge in the far medial of the screen (34) [Figure 1].
Figure 1.
Abdominal muscles thickness (In order from top to bottom; external oblique, internal oblique, and transversus abdominis)
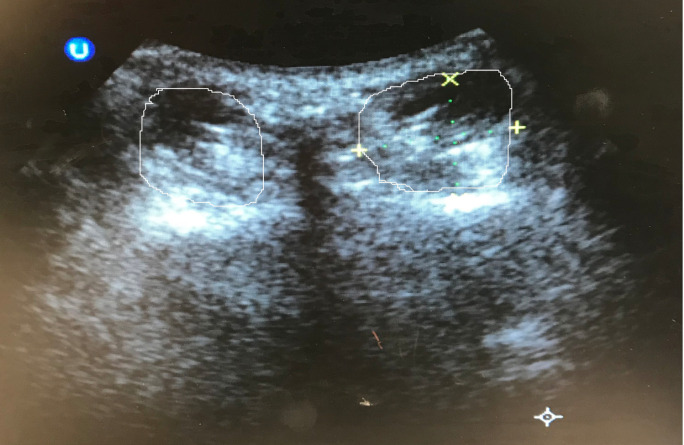
CSA of the MF was assessed in the prone posture (on an approved plinth for decreasing the lumbar curve) at the L5 level using a curvilinear 5 MHZ probe (35). The L5 spinous process was characterized through touching highlighted as the reference. The transducer was located transversely on the L5 spinous process followed by simultaneous measuring the left and right multifidus (36) [Figure 2].
Figure 2.
Lumbar multifidus cross sectional area
The images of the two positions were fixed and saved at the end of the expiration in both sides (37). The US images of abdominal and MF muscles were prepared by a B-mode US imaging system (Ultrasonix-ES500, Canada) using two curvilinear and linear-array probes operating at 5 MHz and 7.5 MHz.
Statistical analyses
For assessing the within-day (between the 1st and 2nd assessments) and between-day (between the 1st and 3rd assessments) reliabilities, standard error of mean (SEM), intraclass correlation coefficients (ICC), and minimal detectable changes (MDC) were applied.
Results
The demographic characteristics of participants and the descriptive data (mean ± SD) of abdominal muscle (EO, IO, TrA) and MF muscle thickness in both sides are shown in Tables 1 and 2, respectively. The findings of within- and between-day reliability and the abdominal muscle and multifidus muscle thickness at rest in both sides are demonstrated in Tables 2 and 3. ICCs range of 0.88 to 0.94 confirmed high for within and between-day reliability. Also, SEM and MDC values suggested stability and high reliability of measuring width of abdominal and MF muscles in athletes with/without HSI.
Table 1.
Demographic characteristics
| Without HSI | With HSI | |
|---|---|---|
| Age (year) | 20.6 ± 3.5 | 24.4 ± 3.08 |
| Height (cm 2 ) | 177.4 ± 0.5 | 174.6 ± 0.05 |
| Weight (kg) | 70.63 ± 9.07 | 71.73 ± 6.62 |
| BMI (Kg/m 2 ) | 22.39 ± 2.48 | 22.74 ± 1.15 |
Table 2.
The Means (±SD) and ICC, SEM and MDC regarding within- and between-day measurements of the EO, IO, TrA, and MF muscles in male soccer players without HSI
| Variables | Evaluation side | Mean ± SD |
Without HIS
|
|||||
|---|---|---|---|---|---|---|---|---|
|
Within-day
|
Between-day
|
|||||||
| ICC | SEM | MDC | ICC | SEM | MDC | |||
| EO (cm) | Right | 7.24 ± 1.92 | 0.93 | 0.55 | 2.05 | 0.89 | 0.68 | 2.26 |
| Left | 6.84 ± 1.68 | 0.92 | 0.51 | 1.97 | 0.87 | 0.67 | 2.36 | |
| IO (cm) | Right | 11.18 ± 2.04 | 0.90 | 0.72 | 3.32 | 0.89 | 0.83 | 2.52 |
| Left | 11.02 ± 1.82 | 0.89 | 0.62 | 2.18 | 0.82 | 0.79 | 2.46 | |
| TrA (cm) | Right | 3.97 ± 1.75 | 0.86 | 0.38 | 1.70 | 0.85 | 0.38 | 1.70 |
| Left | 3.96 ± 1.84 | 0.88 | 0.25 | 1.38 | 0.86 | 0.27 | 1.44 | |
| MF (cm2) | Right | 9.25 ± 0.92 | 0.89 | 0.30 | 1.51 | 0.84 | 0.36 | 1.66 |
| Left | 9.24 ± 0.99 | 0.88 | 0.28 | 1.46 | 0.84 | 0.40 | 1.75 | |
Table 3.
The Means (±SD) and ICC, SEM and MDC regarding within- and between-day measurements of the EO, IO, TrA and MF muscles in male soccer players with HSI
| Variables | Evaluation side | Mean ± SD |
With HIS
|
|||||
|---|---|---|---|---|---|---|---|---|
|
Within-day
|
Between-day
|
|||||||
| ICC | SEM | MDC | ICC | SEM | MDC | |||
| EO (cm) | Right | 5 ± 0.75 | 0.90 | 0.19 | 1.20 | 0.86 | 0.27 | 1.44 |
| Left | 6.01 ± 0.87 | 0.90 | 0.29 | 1.49 | 0.89 | 0.31 | 1.54 | |
| IO (cm) | Right | 9 ± 1.85 | 0.93 | 0.48 | 1.92 | 0.91 | 0.56 | 2.07 |
| Left | 11.52 ± 1.91 | 0.91 | 0.57 | 2.09 | 0.89 | 0.70 | 2.31 | |
| TrA (cm) | Right | 3.63 ± 1.04 | 0.88 | 0.35 | 1.63 | 0.86 | 0.46 | 1.87 |
| Left | 3.09 ± 1 | 0.90 | 0.34 | 1.61 | 0.88 | 0.45 | 1.85 | |
| MF (cm2) | Right | 7.58 ± 1.55 | 0.87 | 0.58 | 2.11 | 0.85 | 0.58 | 2.11 |
| Left | 7.35 ± 1.03 | 0.88 | 0.69 | 2.30 | 0.86 | 0.76 | 2.41 | |
Discussion
The present research aimed at assessing the reliability of abdominal and lumbar multifidus muscle size in soccer players with/without HSI using US. Our findings were consistent with other investigations that assessed the reliability of US in both normal and patient subjects and support the hypothesis that US is an appropriate tool for measuring the muscle thickness in soccer players (35, 38). Hides et al. indicated that real-time US imaging in comparison with MRI can be applied for documenting MF muscle size among young adults (39). Consistent with our results, the intrarater and interrater reliability of MF muscles in 10 subjects without low back pain have been shown to be high (36). Different ICC values between the present study and those by Wallwork et al. may be associated with different methods. The within- and between-day reliability was investigated in both normal subjects and patients, which is one of the strengths of the current research. The obtained SEM values are similar to those announced by Nabavi et al. (35). Also, SEM and MDC values suggested the stability and high reliability of measuring the abdominal and MF muscles width in athletes with/without HSI.
The reliability of EO, IO, and TrA muscles at rest seems to be high with ICC values from 0.86 to 0.93, which are consistent with other studies (35, 38, 40). The SEM for the EO, IO, and TrA was about 0.19 to 0.83 at rest. However, the minimal detectable change represents 1.38 to 3.32.
Richman et al. indicated the reliability coefficient of 0.80 - 1.00 as high reliability, 0.60 - 0.79 as moderate reliability, and 0.59 or smaller as uncertain reliability, which confirm the findings of the present study to have a good to high reliabilities (41).
For improving the generalizability of the findings, further relevant studies using a longer interval, larger sample size and on female athletes are recommended. Also, it is suggested to evaluate the US reliability in measuring the other muscles among athletes. Comparison of various protocols and postures for finding the most reliable method of evaluating the abdominal muscle and MF muscle are also recommended. Small sample size and studying only male athletes can be considered as limitations of the present study. Rehabilitative US as a trusted and non-invasive approach can be employed in clinical setting for measuring muscle dimensions. The used technique in the present research was a trusted method for measuring trunk stabilizing muscles.
Patient Consent:
The subjects signed and completed an informed consent form.
Disclosure:
This study did not receive funding from any organization, and no conflicts of interest have been reported by the authors or any individuals in control of the content of this article.
Acknowledgements
The authors would like to thank all the participants in this study.
References
- 1.Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Intrinsic risk factors for hamstring injuries among male soccer players a prospective cohort study. The American Journal of Sports Medicine. 2010;38(6):1147–53. doi: 10.1177/0363546509358381. [DOI] [PubMed] [Google Scholar]
- 2.Heiderscheit BC, Sherry MA, Silder A, Chumanov ES, Thelen DG. Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. journal of Orthopaedic & Sports Physical Therapy. 2010;40(2):67–81. doi: 10.2519/jospt.2010.3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawkins R, Hulse M, Wilkinson C, Hodson A, Gibson M. The association football medical research programme: an audit of injuries in professional football. British Journal of Sports Medicine. 2001;35(1):43–7. doi: 10.1136/bjsm.35.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woods C, Hawkins R, Maltby S, Hulse M, Thomas A, Hodson A. The Football association medical research programme: an audit of injuries in professional football—analysis of hamstring injuries. British Journal of Sports Medicine. 2004;38(1):36–41. doi: 10.1136/bjsm.2002.002352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnason A, Andersen T, Holme I, Engebretsen L, Bahr R. Prevention of hamstring strains in elite soccer: an intervention study. Scandinavian Journal of Medicine & Science in Sports. 2008;18(1):40–8. doi: 10.1111/j.1600-0838.2006.00634.x. [DOI] [PubMed] [Google Scholar]
- 6.Marshall PW, Lovell R, Jeppesen GK, Andersen K, Siegler JC. Hamstring muscle fatigue and central motor output during a simulated soccer match. PloS one. 2014;9(7):e102753. doi: 10.1371/journal.pone.0102753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Visser H, Reijman M, Heijboer M, Bos P. Risk factors of recurrent hamstring injuries: a systematic review. British Journal of Sports Medicine. 2012;46(2):124–30. doi: 10.1136/bjsports-2011-090317. [DOI] [PubMed] [Google Scholar]
- 8.Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and reinjury. Sports Medicine. 2012;42(3):209–26. doi: 10.2165/11594800-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Sole G, Milosavljevic S, Sullivan SJ, Nicholson H. Running-related hamstring injuries: a neuromuscular approach. Physical Therapy Reviews. 2008;13(2):102–10. [Google Scholar]
- 10.Willardson JM. Core stability training: applications to sports conditioning programs. The Journal of Strength & Conditioning Research. 2007;21(3):979–85. doi: 10.1519/R-20255.1. [DOI] [PubMed] [Google Scholar]
- 11.Willson JD, Dougherty CP, Ireland ML, Davis IM. Core stability and its relationship to lower extremity function and injury. Journal of the American Academy of Orthopaedic Surgeons. 2005;13(5):316–25. doi: 10.5435/00124635-200509000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Loram ID, Kelly SM, Lakie M. Human balancing of an inverted pendulum: is sway size controlled by ankle impedance? The Journal of Physiology. 2001;532(3):879–91. doi: 10.1111/j.1469-7793.2001.0879e.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loram ID, Lakie M. Human balancing of an inverted pendulum: position control by small, ballistic-like, throw and catch movements. The Journal of Physiology. 2002;540(3):1111–24. doi: 10.1113/jphysiol.2001.013077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hides J, Stanton W, McMahon S, Sims K, Richardson C. Effect of stabilization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. Journal of orthopaedic & sports physical therapy. 2008;38(3):101–8. doi: 10.2519/jospt.2008.2658. [DOI] [PubMed] [Google Scholar]
- 15.Bergmark A. Stability of the lumbar spine: a study in mechanical engineering. Acta Orthopaedica Scandinavica. 1989;60(sup230):1–54. doi: 10.3109/17453678909154177. [DOI] [PubMed] [Google Scholar]
- 16.Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Physical Therapy. 1997;77(2):132–42. doi: 10.1093/ptj/77.2.132. [DOI] [PubMed] [Google Scholar]
- 17.Hodges PW, Richardson CA. Delayed postural contraction of transversus abdominis in low back pain associated with movement of the lower limb. Clinical Spine Surgery. 1998;11(1):46–56. [PubMed] [Google Scholar]
- 18.Panjabi MM. The stabilizing system of the spine Part I Function dysfunction adaptation and enhancement. Journal of Spinal Disorders & Techniques. 1992;5(4):383–9. doi: 10.1097/00002517-199212000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Panjabi MM. The stabilizing system of the spine Part II Neutral zone and instability hypothesis. Journal of Spinal Disorders & Techniques. 1992;5(4):390–7. doi: 10.1097/00002517-199212000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Emami M, Arab AM, Ghamkhar L. The activity pattern of the lumbo-pelvic muscles during prone hip extension in athletes with and without hamestring strain injury. International Journal of Sports Physical Therapy. 2014;9(3):312. [PMC free article] [PubMed] [Google Scholar]
- 21.Hides J, Stanton W. Predicting football injuries using size and ratio of the multifidus and quadratus lumborum muscles. Scandinavian Journal of Medicine & Science in Sports. 2017;27(4):440–7. doi: 10.1111/sms.12643. [DOI] [PubMed] [Google Scholar]
- 22.Hides JA, Stanton WR. Can motor control training lower the risk of injury for professional football players. Medicine and Science in Sports and Exercise. 2014;46(4):762–8. doi: 10.1249/MSS.0000000000000169. [DOI] [PubMed] [Google Scholar]
- 23.Mohseni-Bandpei MA, Watson MJ, Richardson B. Application of surface electromyography in the assessment of low back pain: a literature review. Physical therapy reviews. 2000;5(2):93–105. [Google Scholar]
- 24.Rahmani N, Mohseni-Bandpei MA, Vameghi R, Salavati M, Abdollahi I. Application of ultrasonography in the assessment of skeletal muscles in children with and without neuromuscular disorders: a systematic review. Ultrasound in medicine & biology. 2015;41(9):2275–83. doi: 10.1016/j.ultrasmedbio.2015.04.027. [DOI] [PubMed] [Google Scholar]
- 25.Vasseljen O, Fladmark AM. Abdominal muscle contraction thickness and function after specific and general exercises: a randomized controlled trial in chronic low back pain patients. Manual therapy. 2010;15(5):482–9. doi: 10.1016/j.math.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Teyhen D, Koppenhaver S. Rehabilitative ultrasound imaging. Journal of physiotherapy. 2011;57(3):196. doi: 10.1016/S1836-9553(11)70044-3. [DOI] [PubMed] [Google Scholar]
- 27.Whittaker JL, Stokes M. Ultrasound imaging and muscle function. Journal of Orthopaedic & Sports Physical Therapy. 2011;41(8):572–80. doi: 10.2519/jospt.2011.3682. [DOI] [PubMed] [Google Scholar]
- 28.Hides JA, Stanton WR, Mendis MD, Smith MMF, Sexton MJ. Small Multifidus Muscle Size Predicts Football Injuries. Orthopaedic Journal of Sports Medicine. 2014;2(6):1–9. doi: 10.1177/2325967114537588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hides J, Stanton W, Freke M, Wilson S, McMahon S, Richardson C. MRI study of the size, symmetry and function of the trunk muscles among elite cricketers with and without low back pain. British Journal of Sports Medicine. 2008;42(10):809–13. doi: 10.1136/bjsm.2007.044024. [DOI] [PubMed] [Google Scholar]
- 30.Hides JA, Stanton WR, Mendis MD, Gildea J, Sexton MJ. Effect of motor control training on muscle size and football games missed from injury. Medicine and Science in Sports and Exercise. 2012;44(6):1141–9. doi: 10.1249/MSS.0b013e318244a321. [DOI] [PubMed] [Google Scholar]
- 31.Cuellar W, Blizzard L, Callisaya M, Hides JA, Jones G, Ding C, et al. Test-retest reliability of measurements of abdominal and multifidus muscles using ultrasound imaging in adults aged 50–79 years. Musculoskeletal Science and Practice. 2017;28:79–84. doi: 10.1016/j.msksp.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 32.Linek P, Klepek A, Wolny T, Mikołajowski G. Reliability of the lateral abdominal muscle thickness measurements in idiopathic scoliosis patients. Musculoskeletal Science and Practice. 2018;38:151–4. doi: 10.1016/j.msksp.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 33.Hägglund M, Waldén M, Bahr R, Ekstrand J. Methods for epidemiological study of injuries to professional football players: developing the UEFA model. British journal of sports medicine. 2005;39(6):340–6. doi: 10.1136/bjsm.2005.018267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mannion AF, Pulkovski N, Gubler D, Gorelick M, O’Riordan D, Loupas T, et al. Muscle thickness changes during abdominal hollowing: an assessment of between-day measurement error in controls and patients with chronic low back pain. European Spine Journal. 2008;17(4):494–501. doi: 10.1007/s00586-008-0589-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nabavi N, Mosallanezhad Z, Haghighatkhah HR, Bandpeid MAM. Reliability of rehabilitative ultrasonography to measure transverse abdominis and multifidus muscle dimensions. Iranian Journal of Radiology. 2014;11:3. doi: 10.5812/iranjradiol.21008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wallwork TL, Hides JA, Stanton WR. Intrarater and interrater reliability of assessment of lumbar multifidus muscle thickness using rehabilitative ultrasound imaging. Journal of Orthopaedic & Sports Physical Therapy. 2007;37(10):608–12. doi: 10.2519/jospt.2007.2418. [DOI] [PubMed] [Google Scholar]
- 37.Springer BA, Mielcarek BJ, Nesfield TK, Teyhen DS. Relationships among lateral abdominal muscles, gender, body mass index, and hand dominance. Journal of Orthopaedic & Sports Physical Therapy. 2006;36(5):289–97. doi: 10.2519/jospt.2006.2217. [DOI] [PubMed] [Google Scholar]
- 38.Norasteh A, Ebrahimi E, Salavati M, Rafiei J, Abbasnejad E. Reliability of B-mode ultrasonography for abdominal muscles in asymptomatic and patients with acute low back pain. Journal of Bodywork and Movement Therapies. 2007;11(1):17–20. [Google Scholar]
- 39.Hides JA, Richardson CA, Jull GA. Magnetic resonance imaging and ultrasonography of the lumbar multifidus muscle Comparison of two different modalities. Spine. 1995;20(1):54–8. doi: 10.1097/00007632-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 40.Hides JA, Miokovic T, Belavý DL, Stanton WR, Richardson CA. Ultrasound imaging assessment of abdominal muscle function during drawing-in of the abdominal wall: an intrarater reliability study. journal of orthopaedic & sports physical therapy. 2007;37(8):480–6. doi: 10.2519/jospt.2007.2416. [DOI] [PubMed] [Google Scholar]
- 41.Richman J, Makrides L. Research methodology and applied statistics, a seven part series, part 3: Measurement procedures in research. Physiotherapy Canada. 1980 [PubMed] [Google Scholar]