Abstract
Background:
Conventional fixation methods of posterior wall acetabular fractures feature the use of plating and lag screws. However, fixation of posterior wall fractures with buttress plating alone offers potential advantages by avoiding the hardware complications related to hardware placement through the wall fragment. The purpose of this study was to examine if buttress plating alone, without screw fixation through the wall would be a viable method of treating these fractures. Our hypothesis was that this technique would not result in loss of reduction.
Methods:
Consecutive series of patients with isolated posterior wall acetabular fractures treated by two independent surgeons at two Level I Trauma centers without screw fixation across the fracture (Boston Medical Center/Harborview Medical Center).
Results:
All 72 fractures treated without a screw through the posterior wall fragment maintained reduction at an average of 1.6 years post-operatively. For fractures fixed with buttress plating alone, 92 % were reduced within 2 mm of being anatomic compared to 94 % of fractures that had screws cross the fracture.
Conclusion:
The described buttress plating technique without screw fixation in the wall is an acceptable form of fixation for posterior wall acetabular fractures without the theoretical risk of intra-wall screw fixation.
Key Words: Acetabular fractures, Buttress plating, Loss of reduction, Marginal impaction, Posterior wall
Introduction
Posterior wall acetabular fractures are the most common type of acetabular fracture generally requiring surgical intervention due to hip joint instability or incongruity (1-3). Currently described methods of fixation of posterior wall fractures involve fixation with lag screws alone, lag screw fixation with buttress plate, buttress plating with screws placed through the plate and wall or use of a spring plate to aid in fixation. Lag screw fixation with buttress plate is currently the most popular and conventional method of fixation (3-5). For fractures with large fragments, fixation with screws alone has also been known to be a viable option, especially in those able to tolerate partial weight bearing for a prolonged period of time (6, 7). Use of a spring plate has also been shown to be a possible option for fixation of small peripheral and for comminuted fractures (8-10).
To our knowledge, no reports have ever been made describing the clinical use of buttress plates alone, without screw fixation across the wall for the fixation of posterior wall acetabular fractures [Figure 1]. The theoretical risk of using this technique is that the wall fragment can potentially “escape,” laterally and cranially. One cadaveric study demonstrated that fixation with spring plates and reconstruction plates had a higher load to failure than reconstruction plates alone, especially in concentrically comminuted fractures, though whether or not this difference is clinically relevant has yet to be determined (11). Nevertheless, fixation of posterior wall fractures with buttress plating alone offers potential advantages due to the fact that screws are not placed within the wall fragment and therefore drill and screw intrusion into the hip joint is completely avoided (12). Some surgeons advocate the use of spring plates to avoid this risk, however these plates can also be malpositioned and cause impingement and compromise of the femoral head (5).
Figure 1.
Example Case: 56 year-old female status post motor vehicle collision (MVC)
A. Anteroposterior (AP) and obturator oblique radiographs demonstrating a right posterior wall acetabular fracture with associated hip dislocation.
B. Post-reduction Radiographs after closed reduction of the right hip.
C. Post-operative radiographs demonstrating fixation of the posterior wall fracture with a 7-hole buttress plate. Note the absence of screw fixation across the fracture.
D. Follow-up radiographs 10 months post-operative demonstrating maintained fracture reduction as well as absence of any joint space narrowing or avascular necrosis.
Our hypothesis is that this technique contains the wall fragment without the additional need of lag screw placement or intra-wall screw placement.
Materials and Methods
Chart Review
Operative isolated posterior wall cases were obtained from billing records of two orthopaedic surgeons (Senior author from 1998-2014, primary author from 2012-2017). For each case, information was obtained from past medical records regarding the patient’s initial injury characteristics, demographic factors, operative details, and post-operative course. The data was gathered at the two respective Level 1 trauma centers.
Radiographic review
Pre-operative radiographs and CT scans were reviewed for fracture type, displacement, intra-articular fragments, comminution, marginal impaction, and femoral head injury. The roof depth of the fracture was measured as distance between the most superior slice fracture (defined as full cortical disruption) and the most superior aspect of the roof of acetabulum (a fracture apex superior to the roof was assigned a negative value). Ipsilateral posterior wall coverage was measured as the distance from most medial aspect of fracture line to a vertical line that crosses the center of the femoral head (fracture lines medial to the center of the femoral head were assigned negative values). Contralateral posterior wall coverage was defined as the distance from lateral edge of posterior wall to a vertical line that crosses the center of the femoral head at the same distance inferiorly from the superior aspect of the femoral head as the ipsilateral side [Figure 2A]. The per cent acetabular wall intact was a measurement modified from Acetabular fracture index, here defined as the radio of the remaining posterior acetabular wall at the level of the most medial aspect of the fracture compared to the intact wall on the contralateral side measured on CT [Figure 2B] (13). The differences between the ipsilateral and contralateral posterior wall coverage were used to estimate the fracture width.
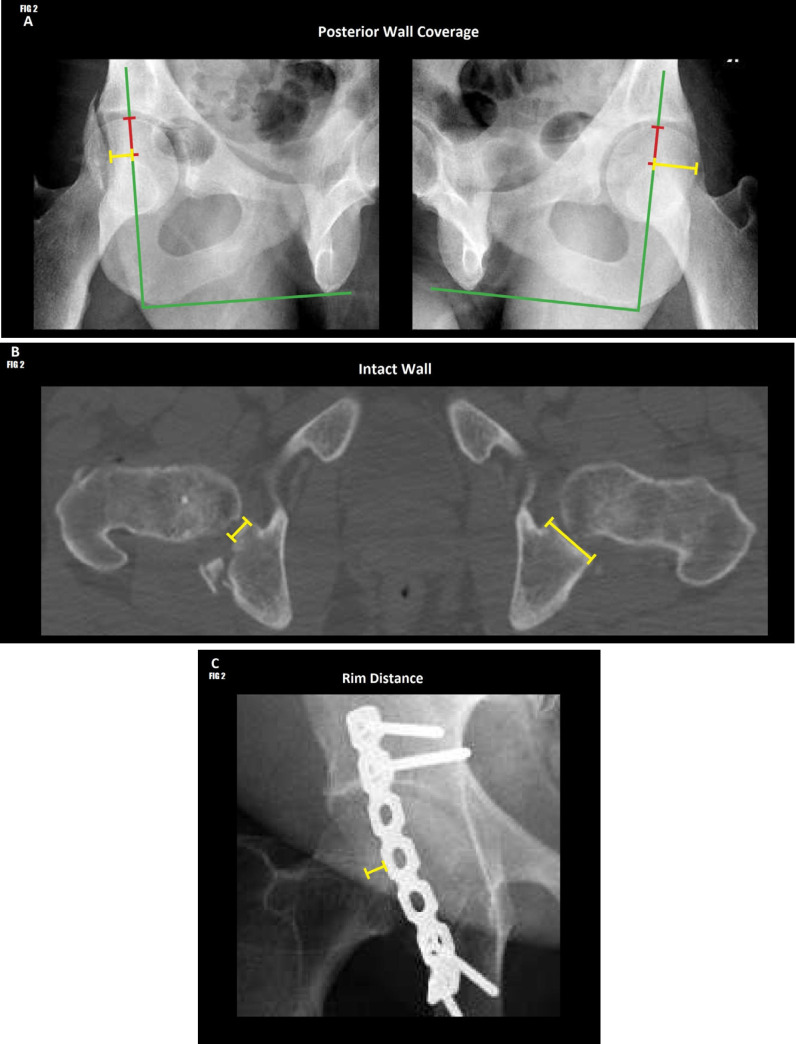
Figure 2.
Radiographic Measurements
A. Posterior Wall Coverage: Ipsilateral wall coverage defined as the distance from the medial aspect of fracture to a vertical line that crosses the centre of the femoral head (green line). Contralateral coverage was measured as the distance from the lateral edge of posterior wall to a line that crosses the centre of the femoral head at the same distance inferiorly from the superior aspect of the femoral head (red lines).
B. Remaining Intact Wall: Ratio of the remaining posterior wall at the level of the medial aspect of the fracture compared to the contralateral intact wall.
C. Rim Distance: Distance of plate to lateral posterior wall.
Immediate post-operative radiographs were reviewed for quality of reduction (maximum displacement seen on any radiographic view, per Matta), and rim distance (defined as the distance of plate to lateral posterior wall on first post-operative anteroposterior (AP) pelvis [Figure 2C] (14). Follow-up radiographs were reviewed for any loss of reduction of the posterior wall fragment. Loss of reduction was defined as any change in posterior wall position on AP or Judet views compared to immediate post-operative imaging. Protocol for both surgeons is to obtain AP and Judet films at each postoperative visit starting at six weeks.
Statistical Analysis
Statistical analysis was performed using with Microsoft Excel (Microsoft, Redmond, WA) and R (R Core Team, Vienna, Austria). Continuous variables were compared using a Student’s t-test, and categorical variables were compared using Fisher’s exact test.
Surgical Technique
Set-up and Approach
The patient is positioned prone on a fracture table with the operative hip extended and knee flexed to protect the sciatic nerve. A standard prep and drape of the hip region is performed. Perioperative antibiotics are given per institutional protocol. A standard Kocher-Langenbeck approach is used to expose the acetabulum and posterior wall.
Reduction and Fixation
The fracture fragments are then identified and isolated. Any areas of marginal impaction are elevated and supported with cancellous allograft. The fracture fragments are then reduced in place, using the femoral head as a template. The reduction is provisionally held with Kirschner wires. A standard 3.5 reconstruction plate, usually 7-8 holes in length, is then shaped to the lateral rim of the acetabulum, slightly undercontoured to allow for some compression. Of note, Kirschner wire palpation technique is used to identify the most peripheral aspect of the wall. The plate is then placed on the lateral rim of the posterior wall and fixed with screws, typically with two screws placed in caudal segment of the plate. This routinely accentuates the undercontoured aspect of the plate with the cranial aspect of the plate elevated off the bone. Using a spike pusher, the relatively flexible plate is brought down to the posterior wall working from a caudal to cranial direction [Figure 3]. Then a 2.5 drill hole is made eccentrically in the plate hole number two in the plate, away from the fracture allowing for further compression. This hole is routinely aimed cranially and medially and is just proximal to the posterior wall fracture line. This is followed by screw placement in hole number one. If the wall fragment is large enough, an additional plate one hole shorter is added medial to the lateral plate to prevent a teetering effect.
Figure 3.
Intraoperative Images
A. 8-hole recon plate is under-contoured to allow for compression of posterior wall acetabular fracture. Note fracture line prior to plate being tensioned over posterior wall.
B. Plate is tensioned as it is brought down from a cranial to caudal direction allowing for compression across the fracture. Note that fracture line is longer evident. Subsequently, screw placed eccentrically in hole number one and two which further tensioned the plate over wall fragment (not shown).
C. Intra-op image displaying the vicinity of a plate to the lateral border of the posterior wall.
In some instances, the wall fragment extends cranially proximal to hole number two in the plate. In those cases a screw is placed first into hole number one, which buttresses and compresses the wall due to undercontoured nature of the plate. This is followed by placing a screw into hole number two, which goes through the wall fragment. An alternative method would be to use a longer plate.
Post-operative Protocol
Patients are made toe-touch weight bearing post-operatively for the first six weeks. If impaction is noted, then the patients are made toe-touch weight bearing for three months. Patients are followed regularly with radiographs and have their weight bearing status advanced gradually. Full weight bearing is usually achieved by three months post-operatively.
Results
We reviewed 101 patients (74 male, 27 female) aged 17-83 (mean 39 years) with an average body mass index (BMI) 30 who sustained OTA type 62-A1 posterior wall acetabulum fractures treated at two Level I Trauma Centers [Table 1] by two surgeons.
Table 1.
Demographic Data
| Demographics | All Cases | No Lag Screws | With Lag Screws | p -value |
|---|---|---|---|---|
| Total Cases | 101 | 72 (71%) | 29 (29%) | --- |
| Age (years) | 39 (17 - 83) | 36(17 - 83) | 40 (22 - 66) | 0.25 |
| Sex (% Male) | 73% | 72% | 75% | 0.75 |
| Average BMI | 30 (21 - 46) | 29(22 - 46) | 31(21 - 42) | 0.48 |
| Smoker (%) | 50% | 49% | 52% | 0.78 |
| Head Injury (%) | 12% | 13% | 10% | 0.66 |
Fractures were of varying size, with an average intact posterior wall of 37 % compared to the contralateral side (range: 0 to 68 %), and involved the acetabular roof in 74 % of cases [Table 2]. Intra-articular fragments were present in 32 % of cases, marginal impaction in 43 % of cases, and femoral head injury in 8 % of cases. These rates were consistent with previously published reports on acetabular fractures involving the posterior wall (1, 10, 12, 14-22). Fractures with screw fixation across the wall fragment generally had smaller ipsilateral posterior wall coverage and smaller roof distance measurements. This indicates that these fractures were usually larger fragments, extending more medially and superiorly compared to the fractures treated with buttress plating alone.
Table 2.
Fracture Characteristics
| All Cases | No Lag Screws | With Lag Screws | p -value | |
|---|---|---|---|---|
| Fracture width on XR (mm) | 17.7 (0.8 - 37.1) | 16.1 (0.8 - 32.5) | 21.3 (6.8 - 37.1) | 0.08 |
| Ipsilateral wall coverage (mm) | 1.6 (-9.9 - 20.3) | 3.3 (-8.6 - 20.3) | -2.2 (-9.9 - 7.3) | 0.02 |
| Contralateral wall coverage (mm) | 19.3 (8.5 - 30.8) | 19.4 (8.5 - 28.6) | 19.1 (10.0 - 30.8) | 0.90 |
| Intact wall remaining (%) | 37% (0 - 68%) | 36% (0 - 68%) | 38% (20- 57%) | 0.75 |
| Comminution (%) | 77% (37 / 48) | 75% (24 / 32) | 81% (13 / 16) | 0.73 |
| Intraarticular fragment (%) | 27% (13 / 48) | 25% (8 / 32) | 31% (5 / 16) | 0.74 |
| Marginal impaction (%) | 44% (22 / 50) | 42% (14 / 33) | 47% (8 / 17) | 0.77 |
| Femoral Head Injury (%) | 8% (4 / 48) | 7% (2 / 30) | 11% (2 / 18) | 0.62 |
| Apex above roof (%) | 74% (29 / 39) | 66% (19 / 29) | 100% (10 / 10) | 0.04 |
| Roof distance (mm) | -7.0 (-37.5 - 16.3) | -4.8 (-36.3 - 16.3) | -13.5 (-37.5 - -2.5) | 0.05 |
Of the 101 posterior wall fractures with a minimum of six month of post-operative imaging, 72 were treated without a screw through the posterior wall (above described technique) and 29 had screws that passed through wall fragment. Of the 101 fractures, 54 had a single buttress, 39 had dual buttress plating, and 8 had a combination of spring plates and reconstruction plates without screws in the wall fragment. The primary buttress plate was placed an average of 5.5 mm from the acetabular rim measured on the AP pelvis radiograph.
For fractures fixed with buttress plating alone, 92 % were reduced within 2 mm. For fractures fixed with screws placed through the fracture fragment 94 %, reduced to < 2 mm residual displacement (P=0.16).
Post-operatively, no fracture treated with the above described technique had “escape,” or loss of reduction of the posterior wall fragment. Average follow-up was 1.6 years (Range 0.5-12 years). One case that was treated with one plate which included a screw through the wall had loss of congruence in the acute post-operative period. Eight patients were referred or had a THA for post-traumatic arthritis. Of the eight, two had small peripheral wall fractures treated with spring plates with overlapping 3.5 mm reconstruction plates. Two patients had the above described technique without spring plates and three patients had screws that were placed through the plate and across the posterior wall fracture.
Discussion
Anatomic reduction is the primary objective of surgical treatment of acetabular fractures with the goal of reconstructing a congruent hip joint and preventing the development of post-traumatic arthritis. While several methods have been described, the results of posterior wall fixation with buttress plating alone have never been reported (5-7, 11). The results of this study demonstrate that this method is a viable technique for achieving and maintaining accurate reduction of these fractures, without the additional risk of penetrating the hip joint.
Interestingly, the only case of acute loss of reduction was a patient that was in the group with fixation through the wall fragment. To our knowledge, no study has been published comparing pure buttress techniques to combination techniques. Within this study, we did have a number of patients that had screws placed through the wall fragment within the confines of the plate. We did not see a significant difference between this group and our treatment technique. However, the treating surgeons, by the nature of the more cranial fracture, placed screws through the fractured wall after the proximal aspect of the plate was brought down. The different fracture locations do not allow us to accurately compare the two fixation constructs.
Recently, Firoozabadi et al, showed that quality of reduction was the most important indicator for conversion to total hip arthroplasty for patients that had an acetabular fracture that involved the posterior wall (22). This study displayed that isolated buttress plating technique could be used to obtain and maintain near anatomic reduction in 92 % of cases, which is similar to the 94 % rate that was noted for fractures that also had fixation through the wall component.
This study has a number of limitations. First, it is important to note that due to relatively few patients treated with screw fixation through the wall fragment we could not perform definitive comparisons between the treatment groups. Furthermore, while there were no significant differences in demographic factors between these two groups, posterior wall fractures which had screw fixation across the wall fragment were typically larger, extending more superiorly. These larger posterior wall fractures have been associated with worse outcomes, especially with increased comminution and involvement of the acetabular roof (10, 23). Thus, it is difficult to attribute the seemingly poorer results within this group to the method of fixation or to the more severe nature of these fractures themselves.
The distinctive aspect of this technique is the avoidance of using screws through the posterior wall fragment. Some surgeons prefer to use lag screws to obtain reduction then place a neutralization plate others prefer to have fixation through the wall fragment due to concern that the wall fragment may “escape.” We support the use of either technique, but we believe that the above described technique eliminates the risk of the drill or screw violating the joint space and causing more injury to cartilage that is already at risk for post-traumatic arthritis. Furthermore, the quadrilateral surface which many of these screws are directed toward has poorer bone quality compared to other parts of the pelvis, and thus, the fixation of these screws may be suboptimal to begin with (4).
Buttress plating techniques can be used to obtain and maintain posterior acetabular wall fixation without increased risk of loss of reduction. However, some fracture configuration may require other modes of fixation which includes the use of screws that cross the posterior wall fracture.
References
- 1.Letournel É, Judet R, Elson R. Fractures of the Acetabulum. 2nd ed. Berlin; New York: Springer-Verlag; 1993. [Google Scholar]
- 2.Firoozabadi R, Spitler C, Schlepp C, Hamilton B, Agel J, Tornetta P. Determining stability in posterior wall acetabular fractures. Journal of orthopaedic trauma. 2015;29(10):465–9. doi: 10.1097/BOT.0000000000000354. [DOI] [PubMed] [Google Scholar]
- 3.Rockwood CA, Green DP, Bucholz RW. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 4.Browner BD, Jupiter JB, Krettek C, Anderson P. Skeletal Trauma: Basic science, Management, and Reconstruction. Fifth ed. Philadelphia, PA: Elsevier/Saunders; 2015. [Google Scholar]
- 5.Moed BR, McMichael JC. Outcomes of posterior wall fractures of the acetabulum: surgical technique. JBJS. 2008;90(Supplement_2_Part_1):87–107. doi: 10.2106/JBJS.G.01471. [DOI] [PubMed] [Google Scholar]
- 6.Im GI, Shin YW, Song YJ. Fractures to the posterior wall of the acetabulum managed with screws alone. Journal of Trauma and Acute Care Surgery. 2005;58(2):300–3. doi: 10.1097/01.ta.0000149329.86361.ce. [DOI] [PubMed] [Google Scholar]
- 7.Stöckle U, Hoffmann R, Nittinger M, Südkamp NP, Haas NP. Screw fixation of acetabular fractures. International orthopaedics. 2000;24(3):143–7. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Patil V, Liu J, Sanford CG, Haman SP. Reconstruction of comminuted posterior wall fractures using the buttress technique: a review of 32 fractures. International orthopaedics. 2007;31(5):671–5. doi: 10.1007/s00264-006-0246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mast J, Jakob R, Ganz R. Planning and Reduction Technique in Fracture Surgery. Berlin; New York: Springer-Verlag; 1989 [Google Scholar]
- 10.Saterbak AM, Marsh JL, Nepola JV, Brandser EA, Turbett T. Clinical failure after posterior wall acetabular fractures: the influence of initial fracture patterns. J Orthop Trauma. 2000;14(4):230–237. doi: 10.1097/00005131-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Goulet JA, Rouleau JP, Mason DJ, Goldstein SA. Comminuted fractures of the posterior wall of the acetabulum A biomechanical evaluation of fixation methods. J Bone Joint Surg Am. 1994;76(10):1457–1463. doi: 10.2106/00004623-199410000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Im G, Chung W. Fractures of the posterior wall of the acetabulum: treatment using cannulated screws. Injury. 2004;35(8):782–786. doi: 10.1016/j.injury.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 13.Calkins MS, Zych G, Latta L, Borja FJ, Mnaymneh W. Computed tomography evaluation of stability in posterior fracture dislocation of the hip. Clin Orthop Relat Res. 1988;227:152–163. [PubMed] [Google Scholar]
- 14.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78(11):1632–1645. [PubMed] [Google Scholar]
- 15.Aho AJ, Isberg UK, Katevuo VK. Acetabular posterior wall fracture 38 cases followed for 5 years. Acta Orthop Scand. 1986;57(2):101–105. doi: 10.3109/17453678609000878. [DOI] [PubMed] [Google Scholar]
- 16.Bhandari M, Matta J, Ferguson T, Matthys G. Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br. 2006;88(12):1618–1624. doi: 10.1302/0301-620X.88B12.17309. [DOI] [PubMed] [Google Scholar]
- 17.Chin F, Lo W, Chen T, Chen C, Huang C, Ma H. Fractures of posterior wall of acetabulum. Arch Orthop Trauma Surg. 1996;115(5):273–275. doi: 10.1007/BF00439052. [DOI] [PubMed] [Google Scholar]
- 18.Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG, McKee MD, Schemitsch EH, et al. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006;88(6):776–782. doi: 10.1302/0301-620X.88B6.17342. [DOI] [PubMed] [Google Scholar]
- 19.Moed BR, Willson-Carr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84-A(5):752–758. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Pantazopoulos T, Nicolopoulos C, Babis GC, Theodoropoulos T. Surgical treatment of acetabular posterior wall fractures. Injury. 1993;24(5):319–323. doi: 10.1016/0020-1383(93)90055-b. [DOI] [PubMed] [Google Scholar]
- 21.Xin Q, Liu J, Gong Y, Chen Y, Li S, Wei F. Treatment of posterior wall fractures of acetabulum. Chin J Traumatol. 2009;12(2):113–117. [PubMed] [Google Scholar]
- 22.Firoozabadi R, Hamilton B, Toogood P, Routt MC, Shearer D. Risk Factors for Conversion to Total Hip Arthroplasty After Acetabular Fractures Involving the Posterior Wall. J Orthop Trauma. 2018;32(12):607–611. doi: 10.1097/BOT.0000000000001327. [DOI] [PubMed] [Google Scholar]
- 23.Epstein HC. Posterior fracture-dislocations of the hip; long-term follow-up. J Bone Joint Surg Am. 1974;56(6):1103–1127. [PubMed] [Google Scholar]