Abstract
Introduction
Dental professionals are at high risk of contracting coronavirus disease 2019 (COVID-19) infection because of their scope of practice with aerosol-generating procedures. Recommendation by the Centers for Disease Control and Prevention to suspend elective dental procedures and avoid aerosol-generating procedures posed significant challenges in the management of patients presenting with endodontic emergencies and uncertainty of outcomes for endodontic procedures initiated, but not completed, before shutdown. The purpose of this study was to evaluate the success of palliative care on endodontic emergencies during the COVID-19 pandemic and to evaluate the stability of teeth with long-term Ca(OH)2 placement because of delays in treatment completion.
Methods
Patients presenting for endodontic emergencies during COVID-19 Shelter-in-Place orders received palliative care, including pharmacologic therapy and/or non–aerosol-generating procedural interventions. Part I of the study evaluated the effectiveness of palliative care, and need for aerosol-generating procedures or extractions was quantified. Part II of the study evaluated survivability and rate of adverse events for teeth that received partial or full root canal debridement and placement of calcium hydroxide before shutdown.
Results
Part I: Twenty-one patients presented with endodontic emergencies in 25 teeth during statewide shutdown. At a follow-up rate of 96%, 83% of endodontic emergencies required no further treatment or intervention after palliative care. Part II: Thirty-one teeth had received partial or full root canal debridement before statewide shutdown. Mean time to complete treatment was 13 weeks. At a recall rate of 100%, 77% of teeth did not experience any adverse events due to delays in treatment completion. The most common adverse event was a fractured provisional restoration (13%), followed by painful and/or infectious flare-up (6.4%), which were managed appropriately and therefore seemed successful. Only 1 tooth was fractured and nonrestorable (3%), leading to a failed outcome of tooth extraction. The remaining 4 outcome failures (13%) were due to patient unwillingness to undergo school-mandated COVID testing or patient unwillingness to continue treatment because of perceived risk of COVID infection.
Conclusions
Palliative care for management of endodontic emergencies is a successful option when aerosol-generating procedures are restricted. This treatment approach may be considered in an effort to reduce risk of transmission of COVID-19 infection during subsequent shutdowns. Prolonged Ca(OH)2 medicament because of COVID-19 related delays in treatment completion appeared to have minimal effect on survival of teeth.
Key Words: Aerosol-generating procedure, COVID-19, endodontic emergencies, long-term calcium hydroxide, palliative care
Significance.
Palliative care for management of endodontic emergencies is a successful option when aerosol-generating procedures are restricted.
The World Health Organization declared coronavirus disease 2019 (COVID-19) as a pandemic on March 11, 2020. Shortly after, countries began to lock down their societies, shutting businesses and nonessential services. In the United States, elective dental procedures were suspended and aerosol-generating procedures were to be avoided according to the Centers for Disease Control and Prevention (CDC)1. Governor Abbot's orders of “Shelter-in-Place” were then enforced in the state of Texas, and the State Board of Dental Examiners adopted the CDC's recommended guidelines for all dentists1. This led to challenges in management of patients presenting with emergencies as well as anxiety among dentists for all in-process pending procedures started before statewide shutdown. Collectively, the global spread of severe acute respiratory syndrome–associated coronavirus 2 (SARS-CoV-2) has wreaked havoc on provision and delivery of dental care worldwide2.
An estimated two thirds of all dental emergencies are endodontic in nature3 , 4, with patients primarily seeking emergency care for a painful tooth3, 4, 5. In addition, according to Nationwide Emergency Department Sample, approximately 302,507 patients make hospital emergency room visits each year for mouth abscess/facial cellulitis in the United States6. During a critical time such as the COVID-19 pandemic, this poses a serious burden on hospital resources. During statewide shutdown, dental professionals were therefore required to work as frontline healthcare workers to help limit hospital resources being needed for management of COVID-19–affected individuals.
It is well-recognized that minor oral surgical, restorative, periodontal, as well as endodontic procedures produce aerosol and splatter contamination that exceeds permissible limits7, 8, 9, 10. Moreover, Index of Microbial Contamination reveals that endodontic procedures generate significantly greater aerosol-produced colony-forming units compared with restorative procedures10. In addition, endodontic procedures disperse aerosols as far as 2 m or 6 feet from the patient's head10. Finally, SARS-CoV-2 is estimated to stay aerosolized for 3–16 hours after dispersion11, 12, 13. Dental professionals, especially endodontists, are therefore at higher risk for nosocomial infection and transmission of SARS-CoV-2, in particular, because of aerosol-generating procedures12 , 14 , 15.
Recommendations for non–aerosol-generating interventions have been made15 to mitigate and protect dental healthcare providers. These include pharmacologic management for pain and infections as well as procedures that do not require a handpiece such as incision and drainage and nonsurgical extractions. However, the success of palliative care for endodontic emergencies has not been determined in the face of a pandemic. Moreover, data on outcome of teeth with long-term calcium hydroxide (Ca(OH)2) because of delayed completion of endodontic treatment are lacking. Therefore, the present study aimed to evaluate success of palliative care on endodontic emergencies presented at the Endodontic clinic at University of Texas Health Science Center at San Antonio and stability (survival) of teeth with long-term Ca(OH)2 placement before statewide shutdown.
Materials and Methods
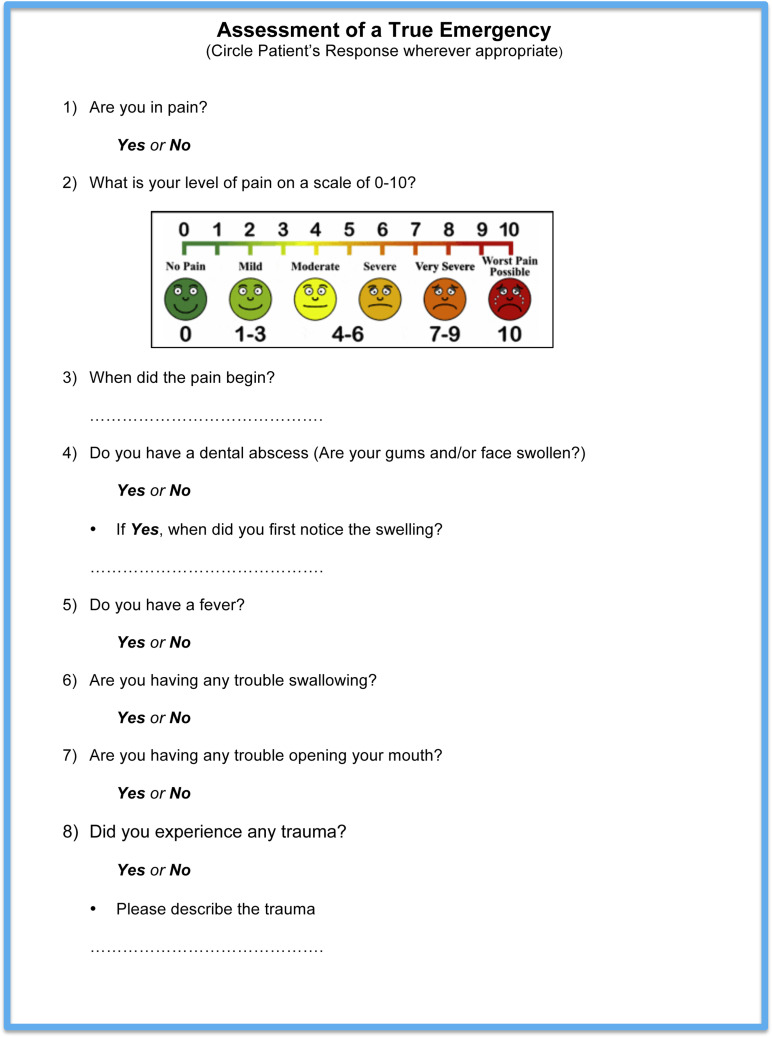
Part I: Management of Endodontic Emergencies
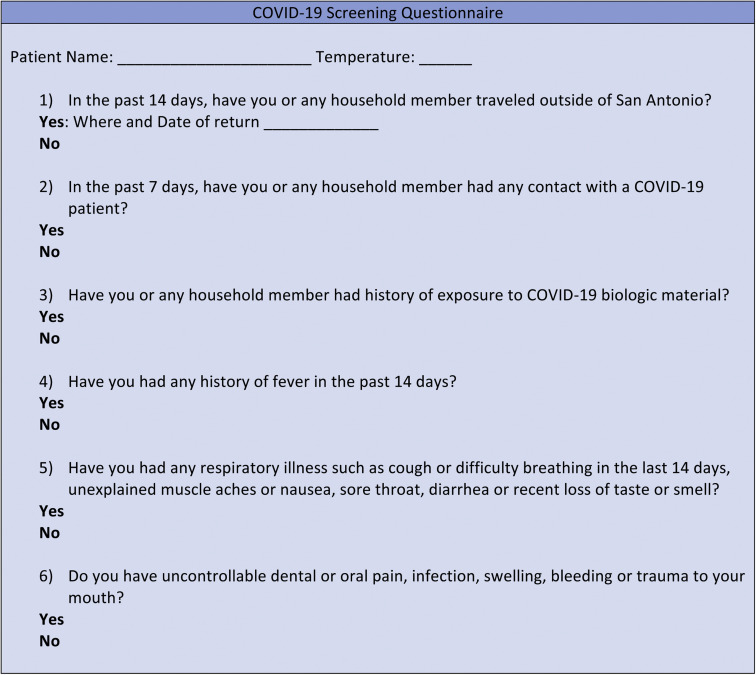
All records of patients presenting for endodontic emergencies to the Endodontic clinic at the University of Texas Health Science Center San Antonio between March 23, 2020 and May 20, 2020 (COVID-19 Shelter-in-Place) were assessed. During the COVID-19 statewide Shelter-in-Place, all patients reporting pain level of 7/10 on visual analogue pain scale or a “Yes” response to any of the questions on the “Assessment of a True Emergency” (Fig. 1 ) were included in the analysis. All patients were seen in person, and no use of teledentistry was performed. Only patients with a “No” response to the COVID-19 screening questionnaire and body temperature between 97°F and 99°F (Fig. 2 ) were seen in the clinic.
Figure 1.
Assessment of a true emergency.
Figure 2.
COVID-19 screening questionnaire.
All patients were provided with treatment on the basis of the treatment guidelines outlined in Table 1 . Type of intervention (palliative or nonpalliative care) and pulpal and periapical diagnoses were collected for analysis. Palliative care was defined as treatment approaches devoid of aerosol-generating procedures and was divided into procedural intervention and pharmacologic intervention.
Table 1.
Treatment Guidelines for Various Emergencies
| Diagnosis | Primary management | Secondary management |
|---|---|---|
| Symptomatic irreversible pulpitis/ symptomatic apical periodontitis | Pain management:First line:• 400–600 mg ibuprofen + 325–500 mg APAP or• naproxen sodium 220 mg + 500 mg APAP 16, 17, 18Second line:• Dexamethasone 0.07–0.09 mg/kg (19) and• Consideration for supplementation with long-acting local anesthetic - bupivacaine for immediate pain relief (20) | Full pulpotomy 21, 22 |
| Acute apical abscess | Intraoral swelling:Incision and drainage• Augmentin 500 mg/clindamycin 300 mg (23) and• 400–600 mg ibuprofen + 325–500 mg APAP 17, 18, 19 orConsideration for supplementation with long-acting local anesthetic - bupivacaine for immediate pain relief (20)Extraoral swelling:• Augmentin 500 mg/clindamycin 300 mg (23) and• 400–600 mg ibuprofen + 325–500 mg APAP 17, 18, 19 | Call Oral Maxillofacial Surgery for further instructions for a possible referral |
| Avulsion/luxation | If tooth is replanted, follow pain management protocol:Pain management: dosage dependent on ageFirst line: ibuprofen + APAP 17, 18, 19 | If tooth is not reimplanted, replant and follow IADT guidelines 24, 25 as best as possible |
| Tooth fracture resulting in pain | Pain management: dosage dependent on age ibuprofen + APAP 17, 18, 19 | Vital pulp therapy 21, 22, 26 |
| Trauma involving facial bones, potentially compromising the patient’s airway | Refer to Oral Maxillofacial Surgery | |
| Cellulitis or a diffuse soft tissue bacterial infection with intraoral or extraoral swelling that potentially compromises the patient’s airway | Refer to Oral Maxillofacial Surgery |
IADT, International Association for Dental Traumatology.
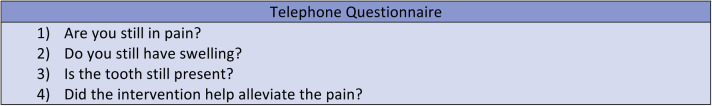
All patients were followed up with a telephone questionnaire (Fig. 3 ) to assess effectiveness of palliative care on endodontic emergencies, length of time until the tooth remained stable after palliative care, and need for additional interventions such as endodontic treatment, extraction, and/or visit to the emergency department or another dental clinic. A successful outcome was defined as tooth was present in the mouth and no further intervention using an aerosol-generating procedure was required. Assessment of restorability and appropriate referral to Oral Maxillofacial Surgery for extraction were considered a successful outcome. Extraction of tooth because of proposed delay in definitive treatment was considered a failed outcome.
Figure 3.
Follow-up telephone questionnaire.
Part II: Management of In-Process Treatments
Before March 23rd, 28 patients with 31 teeth were seen in the Endodontic clinic at the University of Texas Health Science Center San Antonio. All patients had received partial or full root canal debridement, followed by placement of Ca(OH)2. Completion of treatment for these patients was delayed because of the statewide shutdown due to the COVID-19 pandemic.
After reopening of clinic operations, patients were scheduled for completion of treatment, with the school-wide mandate of a negative nasopharyngeal COVID test before initiating aerosol-generating procedures. All teeth were assessed for any adverse events due to delay in completion of treatment. Adverse events included loss of provisional restoration, tooth fracture, painful and/or infectious flare-up, the need to present for emergency treatment, extraction, or patient's unwillingness to undergo nasopharyngeal COVID test.
A successful outcome was defined as a tooth that was deemed restorable and obturated to completion.
Results
Part I
A total of 21 patients presented with endodontic emergencies during statewide shutdown. A total of 25 teeth were evaluated and managed for emergencies. Table 2 lists total patient demographics and pulpal and periapical diagnoses. Table 2 lists patient sex, tooth number, pulpal and periapical diagnoses, procedural and pharmacologic interventions, and outcome for each patient. As noted in Table 3 , all patients were managed conservatively without using any aerosol-generating procedures at first visit.
Table 2.
Patient Demographics and Tooth Information for Patients Presenting for Emergencies
| Temperature at screening | Range, 97°F–98.4°F; mean, 97.5°F |
| Sex | |
| Male | 3 |
| Female | 18 |
| Age (y) | |
| Average | 42 |
| Range | 8–71 |
| Teeth | |
| Anterior | 3 |
| Bicuspid | 4 |
| Molar | 17 |
| Pulpal diagnoses | |
| Reversible pulpitis | 0 |
| Asymptomatic irreversible pulpitis | 0 |
| Symptomatic irreversible pulpitis | 11 |
| Pulp necrosis | 6 |
| Previously initiated | 1 |
| Previously treated | 7 |
| Periapical diagnoses | |
| Normal | 0 |
| Asymptomatic apical periodontitis | 0 |
| Symptomatic apical periodontitis | 20 |
| Acute apical abscess | 5 |
| Chronic apical abscess | 0 |
Table 3.
Patient Age, Sex, Tooth Type, Pulpal and Periapical Diagnoses, Procedural and Pharmacologic Intervention, and Outcome for Each Patient Attending for Endodontic Emergencies
| Tooth no. | Sex | Age (y) | Pulpal diagnosis | Periradicular diagnosis | Procedural intervention | Pharmacologic intervention | Outcome | Success/failure |
|---|---|---|---|---|---|---|---|---|
| 19 | F | 13 | PN | AAA | First visit: incision and drainage | First visit: 400 mg ibuprofen & 325 mg APAP | Intraoral swelling and pain resolved, and no further interventions were required | Success |
| 18 | F | 63 | SIP | SAP | First visit: 400 mg ibuprofen & 325 mg APAP | Patient had tooth extracted shortly after because of pain and concerns of waiting for definitive treatment | Failure | |
| 31 | M | 21 | PN | SAP | Fourth visit: incision and drainage | First visit: 400 mg ibuprofen + 500 mg amoxicillin Second visit: 6 mg dexamethasone Third visit: 6 mg dexamethasone Fourth visit: 400 mg ibuprofen + 500 mg amoxicillin |
Intraoral swelling and pain resolved after fourth visit, and no further interventions were required | Success |
| PN | AAA | |||||||
| 18 | F | 30 | PI | SAP | First visit: 400 mg ibuprofen & 325 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 12 | F | 40 | PN | AAA | First visit: 400 mg ibuprofen & 325 mg APAP | Lost to follow-up | No response | |
| 19 | F | 44 | PT | SAP | First visit: referred to Oral surgery | Extraction | Success | |
| 8 | F | 62 | PT | SAP | First visit: referred to Oral surgery | Extraction | Success | |
| 10 | F | 62 | PT | SAP | First visit: referred to Oral surgery | Extraction | Success | |
| 4 | F | 66 | PT | AAA | First visit: incision and drainage | First visit: 875 mg augmentin | Intraoral swelling resolved, and no further interventions were required | Success |
| 28 | F | 71 | PN | SAP | Tooth extracted by general dentist, deemed unrestorable | Success | ||
| 19 | F | 61 | PN | AAA | First visit: incision and drainage | First visit: 600 mg ibuprofen & 500 mg APAP | Pain resolved, and no further interventions were required | Success |
| 3 | F | 71 | PN | AAA | Incision and drainage | First visit: 600 mg ibuprofen, 500 mg APAP, & 675 mg augmentin | Pain resolved, and no further interventions were required | Success |
| 30 | F | 45 | SIP | SAP | First visit: long-acting anesthetic- 0.5% Marcaine | First visit: 600 mg ibuprofen & 325 mg APAP | Pain resolved, and no further interventions were required | Success |
| 19 | F | 38 | SIP | SAP | Hand excavation of caries + calcium hydroxide dressing | First visit: 6 mg dexamethasone | Pain resolved, and no further interventions were required | Success |
| 12 | F | 68 | PT | SAP | First visit: 600 mg ibuprofen & 500 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 2 | M | 16 | SIP | SAP | First visit: 600 mg ibuprofen & 500 mg APAP | Patient reported prolonged pain | Failure | |
| 7 | M | 16 | SIP | SAP | First visit: 600 mg ibuprofen & 500 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 14 | F | 16 | SIP | SAP | First visit: referred to Oral surgery | First visit: 600 mg ibuprofen and 4 mg dexamethasone (IM) | Extraction | Success |
| 3 | F | 8 | PN | SAP | First visit: 400 mg ibuprofen & 325 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 31 | M | 64 | PT | SAP | First visit: 400 mg ibuprofen & 325 mg APAP | Extraction | Success | |
| 2 | M | 64 | PT | SAP | First visit: 400 mg ibuprofen & 325 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 18 | F | 43 | SIP | SAP | First visit: naproxen sodium 220 mg & 500 mg APAP | Patient pain did not resolve; after 5 days patient requested tooth be extracted | Failure | |
| 30 | F | 29 | SIP | SAP | First visit: naproxen sodium 220 mg & 500 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 29 | F | 29 | SIP | SAP | First visit: naproxen sodium 220 mg & 500 mg APAP | Pain resolved, and no further interventions were required | Success | |
| 15 | F | 17 | SIP | SAP | First visit: 400 mg ibuprofen & 325 mg APAP | Symptoms did not resolve; patient required pulpotomy | Failure |
AAA- acute apical abscess; IM-intramuscular; PI, previously initiated; PN-pulp necrosis; PT-previously treated; SAP-symptomatic apical periodontitis; SIP-symptomatic irreversible pulpitis.
The most common presenting endodontic pulpal diagnosis was symptomatic irreversible pulpitis (44%), followed by pulp necrosis (24%) and previously treated (24%). The most common periapical diagnosis was symptomatic apical periodontitis (80%), followed by acute apical abscess (20%). A total of 5 teeth (20%) were deemed nonrestorable and appropriately referred for extraction.
One patient with 1 tooth was lost to follow-up, providing a follow-up rate of 96%. Of the remaining 20 patients who were followed up, 16 patients (80%) with 20 teeth (83%) reported no need for further intervention, and emergency was managed with pertinent recommendations using non–aerosol-generating procedures. Four patients (20%) with 4 teeth (17%) reported the need to seek further treatment or intervention. Of these, 2 patients resorted to seek extraction of the offending tooth because of the proposed delay in definitive treatment. One patient reported being in pain with 1 tooth throughout the shutdown but did not seek further intervention. Finally, 1 patient required intervention with an aerosol-generating procedure (definitive pulpotomy) because of lack of reduction in pain with the prescribed pharmacologic recommendations.
Part II
A total of 31 teeth in 28 patients had received partial or full root canal debridement before statewide shutdown due to COVID-19 pandemic. Table 4 lists total patient demographics and pulpal and periapical diagnoses, and Table 5 lists patient sex, age, pulpal and periapical diagnoses, time to treatment completion, adverse events, and treatment outcome. Mean time to complete treatment was 13.2 weeks. All patients were followed up, giving a follow-up rate of 100%. Twenty-four teeth (77%) did not experience any adverse events because of delays in treatment completion. Among the 7 patients (25%) who experienced adverse events, the most common adverse event was a fractured provisional restoration (4 teeth, 13%), which occurred exclusively in premolars and molars (Table 5). Painful and/or infectious flare-up occurred in 2 teeth (6%), specifically in 1 vital premolar and 1 necrotic molar with a sinus tract (Table 5). Between the 2 patients who experienced interappointment pain, one patient was prescribed 3 tablets of 6 mg dexamethasone to manage interappointment pain twice, and the other did not report pain to the provider until returning back for completion of treatment. The remaining adverse event observed was a fractured, nonrestorable molar (1 tooth, 3%). Despite the 23% incidence of adverse events in individual teeth, only 1 adverse event (3%) led to a failed outcome of tooth extraction.
Table 4.
Patient Demographics and Tooth Information
| Sex | |
| Male | 11 |
| Female | 17 |
| Age (y) | |
| Average | 40 |
| Range | 11–87 |
| Teeth | |
| Anterior | 10 |
| Bicuspid | 6 |
| Molar | 15 |
| Pulpal diagnoses | |
| Reversible pulpitis | 4 |
| Asymptomatic irreversible pulpitis | 1 |
| Symptomatic irreversible pulpitis | 5 |
| Pulp necrosis | 10 |
| Previously initiated | 2 |
| Previously treated | 9 |
| Periapical diagnoses | |
| Normal | 4 |
| Asymptomatic apical periodontitis | 5 |
| Symptomatic apical periodontitis | 15 |
| Acute apical abscess | 1 |
| Chronic apical abscess | 6 |
Table 5.
Patient Demographics, Pulpal and Periapical Diagnoses, Adverse Events, and Treatment Outcomes
| Tooth # | Sex | Age (y) | Pulpal diagnosis | Periradicular diagnosis | Time to treatment completion (wk) | Adverse event | Outcome |
|---|---|---|---|---|---|---|---|
| 2 | M | 18 | PN | CAA | 14 | None | Success |
| 3 | F | 87 | SIP | SAP | 13 | None | Success |
| 4 | F | 16 | SIP | SAP | 13 | Pain/flare-up – prescribed 6 mg dexamethasone | Success |
| 5 | F | 42 | RP | SAP | 15 | Fractured restoration | Success |
| 7 | M | 17 | RP | N | 10 | None | Success |
| 8 | M | 17 | RP | N | 10 | None | Success |
| 9 | M | 17 | RP | N | 10 | None | Success |
| 8 | M | 14 | PT | AAP | N/A | Refused COVID-19 test | Failed |
| 8 | F | 37 | PN | SAP | 13 | None | Success |
| 8 | F | 17 | PN | AAP | 12 | None | Success |
| 9 | M | 23 | PN | AAP | 13 | None | Success |
| 13 | F | 54 | PT | SAP | 18 | None | Success |
| 14 | F | 39 | SIP | SAP | 17 | None | Success |
| 14 | F | 61 | PT | SAP | 13 | None | Success |
| 14 | F | 17 | PN | SAP | 12 | Fractured restoration | Success |
| 14 | F | 44 | PT | AAP | 13 | None | Success |
| 19 | M | 37 | PT | SAP | 14 | None | Success |
| 19 | F | 41 | PT | AAA | 14 | None | Success |
| 19 | F | 18 | PT | CAA | 16 | None | Success |
| 19 | M | 40 | PI | CAA | 14 | Fractured restoration | Success |
| 19 | M | 11 | PI | CAA | N/A | Refused COVID-19 test | Failed |
| 19 | F | 70 | PT | SAP | 12 | None | Success |
| 19 | M | 34 | PT | AAP | 13 | None | Success |
| 20 | F | 64 | PN | CAA | 12 | Fractured restoration | Success |
| 21 | M | 52 | AIP | N | N/A | Deferred treatment due to perceived COVID-19 infection risk | Failed |
| 22 | M | 16 | SIP | SAP | 13 | None | Success |
| 24 | M | 16 | SIP | SAP | 13 | None | Success |
| 23 | F | 74 | PN | SAP | N/A | Deferred treatment due to perceived COVID-19 infection risk | Failed |
| 30 | F | 65 | PN | SAP | 16 | None | Success |
| 31 | F | 40 | PN | SAP | 13 | Fractured tooth | Failed |
| 31 | M | 71 | PN | CAA | 10 | Pain/flare-up | Success |
AAA, acute apical abscess; AAP, asymptomatic apical periodontitis; AIP, asymptomatic irreversible pulpitits; CAA, chronic apical abscess; PI, previously initiated; PN, pulp necrosis; PT, previously treated; RP, reversible pulpitis; SAP, symptomatic apical periodontitis; SIP, symptomatic irreversible pulpitis.
Two outcome failures (6%) occurred in pediatric patients (ages 11 and 14 years) because of patient's and/or parent's unwillingness to undergo school-mandated nasopharyngeal COVID testing. Thus, treatment could not be completed, resulting in outcome failure. One patient sought continuation of treatment in private practice, and the other patient was stable and wished to resume care when school-wide COVID testing requirements are no longer enforced. Two additional outcome failures (6%) occurred in relatively older patients, aged 52 and 74 years, who wished to postpone treatment because of perceived risk of COVID infection by continuing treatment. Both patients are stable, without pain, and elected to continue treatment after the COVID-19 pandemic. Aside from patient-related issues with COVID-19 testing or perceived risk of COVID infection, only 1 tooth out of 31 teeth (3%) experienced an outcome failure because of delayed treatment that led to tooth extraction.
Discussion
With more than 300,000 cases in March 2020 to now more than 11 million cases in July 2020, the COVID-19 pandemic is unlikely to end soon27. Several states may be faced with a second cycle of business shutdowns, forcing dentistry to adapt to the ever-changing situation. Because of the increased occupational risk associated with COVID-19 infection and dentistry12 , 14 , 15 , 28, the present retrospective study investigated the effectiveness of conservative management (non–aerosol-generating procedures) on management of endodontic emergencies as well as outcome of long-term Ca(OH)2 because of delayed completion of treatment during the COVID-19 shutdown at Endodontics clinic at the University of Texas Health Science Center San Antonio. Specifically, this study aimed to assess the effectiveness of palliative care for endodontic emergencies and the effect of delayed endodontic treatment on survivability of teeth with long-term Ca(OH)2. We hope that findings from this study will aid clinicians in making treatment decisions during potential future shutdowns of clinic operations. To our knowledge, a pragmatic clinical study evaluating these aims is lacking.
For Part I of the study, the most common pulpal diagnosis of endodontic emergencies was symptomatic irreversible pulpitis, followed by pulpal necrosis. The most common periapical diagnosis was symptomatic apical periodontitis, followed by acute apical abscesses. These findings were comparable to a study from Wuhan, China29, which analyzed the characteristics of endodontic emergencies during the coronavirus disease outbreak. There were a higher percentage of female patients (86%) who reported with painful emergencies than male patients (14%). This is consistent with previous reports demonstrating that painful pulpitis is sexually dimorphic in nature3 , 30, and that women are more likely to seek medical attention than men when in pain31.
An overall success rate of 83% was noted for cases that were managed conservatively with non–aerosol-generating procedures and pharmacologic management. On average, teeth deemed successful were stable with conservative interventions for 8 weeks. One patient required several rounds of first and second lines of pharmacologic management, with a last visit warranting an incision and drainage procedure. However, because all recommendations were palliative in nature, this case was considered successful. All patients with a periapical diagnosis of acute apical abscess (20%) were successfully managed with incision and drainage with or without antibiotics and pharmacologic intervention for pain management. Forty-one percent of all teeth presented with a pulpal diagnosis of symptomatic irreversible pulpitis and symptomatic apical periodontitis. Of these, 60% were managed appropriately with pharmacologic interventions. Interestingly, all cases deemed unsuccessful were diagnosed with symptomatic irreversible pulpitis and symptomatic apical periodontitis. All 4 patients (3 female, 1 male) were prescribed a combination of nonsteroidal anti-inflammatory drug with acetaminophen (APAP). Two patients resorted to extraction because their pain was unmanaged with the recommended first line of pharmacologic intervention (400 mg ibuprofen with 325 mg APAP and 220 mg naproxen with 500 mg APAP, respectively). It is noteworthy that these patients did not return to clinic for second line of pharmacologic intervention. Therefore, it is unknown whether further pharmacologic interventions would have been beneficial. Nonetheless, because of the COVID-19 pandemic and the pragmatic nature of this clinical study, patient perceptions leading to untimely tooth extractions were considered a failure. A third patient was also managed with 600 mg ibuprofen with 500 mg APAP. Although this patient did not opt for tooth extraction, they reported having “unbearable” pain and did not want to return to clinic until definitive treatment was offered. A fourth patient required definitive pulpotomy because of inadequate pain management with 400 mg ibuprofen with 325 mg APAP. Collectively, findings and success rate of 83% from Part I of the study are encouraging and provide strategies to mitigate the use of aerosol-generating procedures for management of endodontic emergencies.
For Part II of the study, a total of 31 teeth were in an interim treatment phase with Ca(OH)2 placed in all teeth. The most common complication experienced by this cohort of patients was fractured restoration (13%). However, all teeth with this adverse event were deemed restorable and therefore successful. One tooth (3%) was deemed nonrestorable because of tooth fracture and therefore was considered a failure. Previous studies have raised concerns on the use of long-term Ca(OH)2 and its relationship to weakening of teeth32. Andreasen et al32 suggested that fracture strength of teeth dressed with Ca(OH)2 decreased significantly from 2 months, and at 12 months they were 50% of the original strength. The authors concluded Ca(OH)2 should not be used for longer than 30 days. Another study demonstrated that there was a significant decrease in fracture strength from 28 to 84 days with calcium hydroxide33. However, results from a third study disagree with these findings and do not demonstrate a detrimental effect of Ca(OH)2 up to 6 months34. All patients in this study had an average time of 13.2 weeks in Ca(OH)2, and only 1 tooth was lost because of tooth fracture. However, all studies referenced here are either in vitro or ex vivo animal models, and the results of our study may differ because of inherent differences in the study models used. However, long-term follow-up on survivability of all teeth included in this study is warranted.
The University of Texas Health Science Center San Antonio Dental School mandated a COVID-19 test before all aerosol-generating procedures. Therefore, refusal to testing was considered a negative outcome and therefore an outcome failure. Six percent of patients refused COVID-19 test. An additional 6% deferred treatment because of perceived COVID-19 infection risk by continuing treatment. The latter were also considered an outcome failure because patient perception in retention or loss of dentition is a key component of a pragmatic clinical study. Collectively, findings from Part II of the study suggest that success of delayed endodontic treatment of teeth with Ca(OH)2 does not lead to significant tooth loss, with a success rate of 84%.
As the global expansion of the COVID-19 pandemic continues, it is accompanied by stress on supply chains for personal protective equipment (PPE)35 , 36. The CDC guidelines for dental professionals recommend the use of N95 or other higher quality filtration devices during all aerosol-generating procedures. Because of the high prevalence of endodontic emergencies3, 4, 5, it is most appropriate to manage these emergencies with definitive treatment such as root canal therapy or extraction. However, because of the likelihood for a second shutdown in many regions, a high risk of contraction of COVID-19 for dental professionals, and the shortage of PPE, alternative treatment options are warranted. Our data suggest that palliative care for a short-term duration may be applicable to endodontic practices to minimize aerosol-transmitted COVID-19 infection as well as to conserve critical PPE required by medical frontline hospital workers. It is noteworthy that none of the providers in our study contracted COVID-19 during management of emergency patients. This finding is similar to the study from Wuhan, China29, where emergencies were managed with aerosol-generating procedures such as pulpotomies and pulpectomies. However, our study included various pulpal and periapical diagnoses and therefore precludes a direct comparison. Moreover, because respiratory droplets and aerosol particles released from coronavirus-infected individuals can range from 10,000–100,000 viral particles without a protective barrier such as a mask on the patient's mouth37, a consideration for best practices during this pandemic is warranted. Finally, teeth in the interim stage of an endodontic procedure appear to remain stable and therefore restorable for completion after reopening of dental clinics.
Overall, within the limitations of this study such as a small sample size, palliative care for management of endodontic emergencies is a successful interim treatment option when aerosol-generating procedures are restricted. This treatment approach may be considered in an effort to reduce risk of transmission of COVID-19 infection during subsequent shutdowns. Finally, survivability of teeth with long-term Ca(OH)2 does not appear to pose a detrimental effect on tooth loss.
CRediT authorship contribution statement
Biraj Patel: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Michael A. Eskander: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Nikita B. Ruparel: Conceptualization, Methodology, Writing - original draft, Writing - review & editing.
Acknowledgments
The authors deny any conflicts of interest related to this study.
References
- 1.CDC: coronavirus 19 dental settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html Available at:
- 2.Coulthard P. Dentistry and coronavirus (COVID-19): moral decision-making. Br Dent J. 2020;228:503–505. doi: 10.1038/s41415-020-1482-1. [DOI] [PubMed] [Google Scholar]
- 3.Estrela C., Guedes O.A., Silva J.A. Diagnostic and clinical factors associated with pulpal and periapical pain. Braz Dent J. 2011;22:306–311. doi: 10.1590/s0103-64402011000400008. [DOI] [PubMed] [Google Scholar]
- 4.Rechenberg D.K., Held U., Burgstaller J.M. Pain levels and typical symptoms of acute endodontic infections: a prospective, observational study. BMC Oral Health. 2016;16:61. doi: 10.1186/s12903-016-0222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Owatz C.B., Khan A.A., Schindler W.G. The incidence of mechanical allodynia in patients with irreversible pulpitis. J Endod. 2007;33:552–556. doi: 10.1016/j.joen.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 6.Kim M.K., Allareddy V., Nalliah R.P. Burden of facial cellulitis: estimates from the Nationwide Emergency Department Sample. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:312–317. doi: 10.1016/j.tripleo.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 7.Timmerman M.F., Menso L., Steinfort J. Atmospheric contamination during ultrasonic scaling. J Clin Periodontol. 2004;31:458–462. doi: 10.1111/j.1600-051X.2004.00511.x. [DOI] [PubMed] [Google Scholar]
- 8.Bentley C.D., Burkhart N.W., Crawford J.J. Evaluating spatter and aerosol contamination during dental procedures. J Am Dent Assoc. 1994;125:579–584. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 9.Divya R., Senthilnathan K.P., Kumar M.P.S., Murugan P.S. Evaluation of aerosol and splatter contamination during minor oral surgical procedures. Drug Invention Today. 2019;12:1845–1848. [Google Scholar]
- 10.Manarte-Monteiroa P., Carvalhoa A., Cristina P. Air quality assessment during dental practice: aerosols bacterial counts in an universitary clinic. Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial. 2013;54:2–7. [Google Scholar]
- 11.van Doremalen N., Bushmaker T., Morris D.H. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.New York Times: coronavirus workers risk. https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html Available at:
- 13.Peng X., Xu X., Li Y. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The front line: visualizing the occupations with the highest COVID-19 risk. https://www.visualcapitalist.com/the-front-line-visualizing-the-occupations-with-the-highest-covid-19-risk/ Available at:
- 15.Ather A., Patel B., Ruparel N.B. Coronavirus disease 19 (COVID-19): implications for clinical dental care. J Endod. 2020;46:584–595. doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watts K., Balzer S., Drum M. Ibuprofen and acetaminophen versus intranasal ketorolac (Sprix) in an untreated endodontic pain model: a randomized, double-blind investigation. J Endod. 2019;45:94–98. doi: 10.1016/j.joen.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Smith E.A., Marshall J.G., Selph S.S. Nonsteroidal anti-inflammatory drugs for managing postoperative endodontic pain in patients who present with preoperative pain: a systematic review and meta-analysis. J Endod. 2017;43:7–15. doi: 10.1016/j.joen.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 18.Taggar T., Wu D., Khan A.A. A randomized clinical trial comparing 2 ibuprofen formulations in patients with acute odontogenic pain. J Endod. 2017;43:674–678. doi: 10.1016/j.joen.2016.12.017. [DOI] [PubMed] [Google Scholar]
- 19.Liesinger A., Marshall F.J., Marshall J.G. Effect of variable doses of dexamethasone on posttreatment endodontic pain. J Endod. 1993;19:35–39. doi: 10.1016/S0099-2399(06)81039-3. [DOI] [PubMed] [Google Scholar]
- 20.Gordon S.M., Mischenko A.V., Dionne R.A. Long-acting local anesthetics and perioperative pain management. Dent Clin North Am. 2010;54:611–620. doi: 10.1016/j.cden.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Eren B., Onay E.O., Ungor M. Assessment of alternative emergency treatments for symptomatic irreversible pulpitis: a randomized clinical trial. Int Endod J. 2018;51(Suppl 3):e227–e237. doi: 10.1111/iej.12851. [DOI] [PubMed] [Google Scholar]
- 22.Hasselgren G., Reit C. Emergency pulpotomy: pain relieving effect with and without the use of sedative dressings. J Endod. 1989;15:254–256. doi: 10.1016/S0099-2399(89)80219-5. [DOI] [PubMed] [Google Scholar]
- 23.Baumgartner J.C., Xia T. Antibiotic susceptibility of bacteria associated with endodontic abscesses. J Endod. 2003;29:44–47. doi: 10.1097/00004770-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Diangelis A.J., Andreasen J.O., Ebeleseder K.A. Guidelines for the management of traumatic dental injuries: 1—fractures and luxations of permanent teeth. Pediatr Dent. 2017;39:401–411. doi: 10.1111/j.1600-9657.2011.01103.x. [DOI] [PubMed] [Google Scholar]
- 25.Andersson L., Andreasen J.O., Day P. Guidelines for the management of traumatic dental injuries: 2—avulsion of permanent teeth. Pediatr Dent. 2017;39:412–419. doi: 10.1111/j.1600-9657.2012.01125.x. [DOI] [PubMed] [Google Scholar]
- 26.Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod. 1978;4:232–237. doi: 10.1016/S0099-2399(78)80153-8. [DOI] [PubMed] [Google Scholar]
- 27.Johns Hopkins coronavirus help desk. https://coronavirus.jhu.edu/map.html Available at:
- 28.OSHA dentistry: COVID-19. https://www.osha.gov/SLTC/covid-19/dentistry.html Available at:
- 29.Yu J., Zhang T., Zhao D. Characteristics of endodontic emergencies during coronavirus disease 2019 outbreak in Wuhan. J Endod. 2020;46:730–735. doi: 10.1016/j.joen.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nusstein J.M., Beck M. Comparison of preoperative pain and medication use in emergency patients presenting with irreversible pulpitis or teeth with necrotic pulps. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:207–214. doi: 10.1016/s1079-2104(02)91732-4. [DOI] [PubMed] [Google Scholar]
- 31.Hunt K., Adamson J., Hewitt C., Nazareth I. Do women consult more than men? a review of gender and consultation for back pain and headache. J Health Serv Res Policy. 2011;16:108–117. doi: 10.1258/jhsrp.2010.009131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andreasen J.O., Farik B., Munksgaard E.C. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134–137. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 33.Rosenberg B., Murray P.E., Namerow K. The effect of calcium hydroxide root filling on dentin fracture strength. Dent Traumatol. 2007;23:26–29. doi: 10.1111/j.1600-9657.2006.00453.x. [DOI] [PubMed] [Google Scholar]
- 34.Hawkins J.J., Torabinejad M., Li Y., Retamozo B. Effect of three calcium hydroxide formulations on fracture resistance of dentin over time. Dent Traumatol. 2015;31:380–384. doi: 10.1111/edt.12175. [DOI] [PubMed] [Google Scholar]
- 35.FDA: PPE shortage. https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/faqs-shortages-surgical-masks-and-gowns-during-covid-19-pandemic Availble at:
- 36.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages: the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 37.Leung N.H.L., Chu D.K.W., Shiu E.Y.C. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med. 2020;26:676–680. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]