Abstract
This study aims to explore the clinical and epidemiological characteristics of infant patients with coronavirus disease-2019 (COVID-19) infection. Clinical and epidemiological data of a 3-month-old patient with COVID-19 were collected, including general status, clinical results, laboratory tests, imaging characteristics, and epidemiological reports. The infant had no fever but had mild respiratory symptoms. The major laboratory results included normal white blood cell counts and lymphocytopenia, notably with elevated interleukin (IL-)-17A, IL-17F, and tumor necrosis factor (TNF-)-α. The main manifestation of his chest computed tomography scan was pulmonary patchy shadows. All throat swabs and urine of the infant detected via Real-time Quantitative Polymerase Chain Reaction (RT-PCR) were negative, but his anal swab continued to test positive up to 40 days after onset of illness. Our study indicated that infants infected with COVID-19 may have relatively mild symptoms or clinical signs, IL-17A, IL-17 F, and TNF-α could be involved in the immune response of COVID-19. In addition, severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) may shed through the gastrointestinal tract and convalescent carriers may exist among infant patients. We cannot rule out the possibility that infants may acquire infection from breastfeeding. Intensive care and nutrition support are recommended for infant patients with mild symptoms.
Keywords: COVID-19, Infant, SARS-CoV-2, Immune response, Transmission
Introduction
Coronavirus disease-2019 (COVID-19), which was first discovered in December 2019 in Wuhan, Hubei Province, China, has now developed into a global infectious disease. As of April 19, 2020, the number of laboratory-confirmed cases had exceeded 80,000 in China and over 2,000,000 in the rest of the world [1], The World Health Organization(WHO) has characterized the COVID-19 outbreak as a pandemic, but data regarding infected children or infants are limited [2]. According to a review by the Chinese Center for Disease Control and Prevention [3], which included 72,314 cases, less than 1% of the cases were in children younger than 10 years old. In Guangzhou, more than 500 confirmed cases of COVID-19 were reported [4], with the youngest being 3 months after birth. Current studies suggest that people of all ages are vulnerable to COVID-19 infection [3], but that a few infections among infants have been reported. Most of the current diagnosis, treatment, and prevention guidelines used globally were developed based on experience collated from COVID-19 in adults, Therefore, there is a need to explore more regarding the clinical manifestation and prognosis in infants.
Thus, there is still a lack of evidence regarding whether COVID-19 can be transmitted from mother to child, especially through breastfeeding [5]. A number of recent studies have examined nucleic acids in the breast milk of lactating women [[6], [7], [8]], but only one study [9] detected SARS-CoV-2 RNA in the breast milk of a mother for 4 consecutive days, and her baby developed mild symptoms and was diagnosed with COVID-19. However, it remains uncertain whether the baby developed the disease through breastfeeding [9]. Thus, more research is needed regarding transmission through breastfeeding.
We report a 3-month-old baby who was infected with COVID-19, and analyze his epidemiological investigation, pathogenic course, clinical manifestation, laboratory examination and the treatment process, to explore the characteristics of breastfeeding infants in terms of the route of infection, clinical manifestation and prognosis.
Methods
We did a retrospective review of medical records and the epidemiological investigation on a 3-month-old infant with COVID-19 pneumonia admitted to hospital in Guangzhou from February 19 to March 20, 2020. The diagnosis of COVID-19 pneumonia was based on the New Coronavirus Pneumonia Diagnosis and Treatment Program (6th edition) published by the National Health Commission of China [10]. The epidemiological investigation was conducted by experienced experts of Center for Disease Control and Prevention of Guangzhou (GZCDC). Clinical records, laboratory findings, and chest computed tomography (CT) scans were obtained from the hospital the infant had been treated. Throat swab, anal swab and urine samples were collected and tested for SARS-CoV-2 with the Chinese Center for Disease Control and Prevention recommended Kit (BioGerm, Shanghai, China), following WHO guidelines for RT-PCR. All samples were processed simultaneously at the Virus and Immune Laboratory of GZCDC. The test results were confirmed by RT-PCR with designed primers. This study was carried out with written informed consent from the patient’s parent and approved by GZCDC.
Results
Case presentation
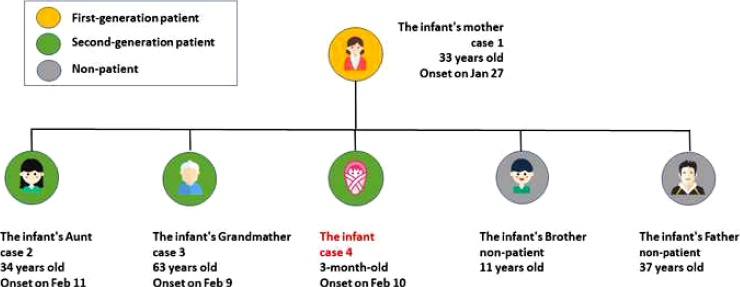
Our patient was a male infant, delivered by Caesarean Section, who was born in November, 2019 in Jingmeng, Hubei Province, China. On February 21, 2020, he was confirmed as a COVID-19 patient. The infant’s mother was the first confirmed patient in his family, with the infant, his aunt along, and grandmother being infected as second-generation patients in a similar period (Fig.1). Except for treatment for jaundice in his first month of life, the baby was healthy and developed normally. He was generally fed by breast-milk mixed with infant formulas owing to insufficient breast-milk. His mother took care of him most of the time.
Fig. 1.
The relationship of the infant’s Family and their time of onset of COVID-19.
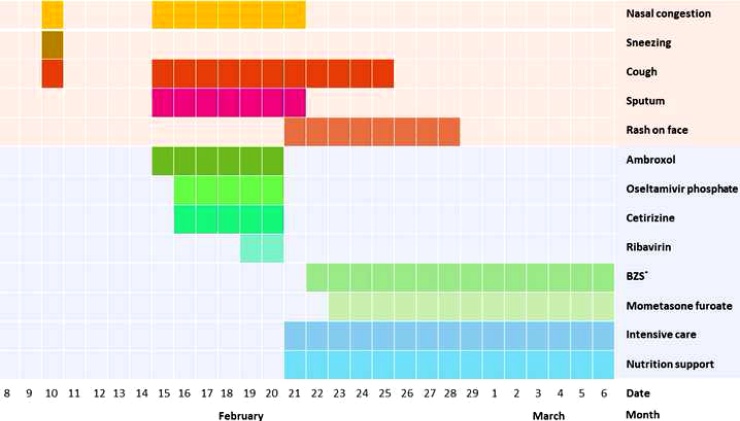
The infant’s symptoms were relatively mild and of short duration. He never developed a fever. On February 10, he demonstrated symptoms of nasal congestion, sneezing and occasional coughing, but these last only 1 day, and did not attract his family’s attention. On February 13, because of his close contact with his mother who was a confirmed patient, the infant was sent to the hospital for clinical assessment, even though he was asymptomatic. A chest computed tomography (CT) scan of the infant showed suspicious diffuse bilateral lower lobe patchy shadows. Other pertinent laboratory findings included a normal leukocyte count of 11.67 × 109/mL and elevated lymphocyte count of 8.48 × 109/mL. The real-time PCR results of SARS−COV-2 in his throat swab sample were negative in the first 3 days of admission. The tests for influenza A and B, parainfluenza, respiratory syncytial virus, rhinovirus, human bocavirus, adenovirus, human metapneumovirus, mycoplasma, and chlamydia were also conducted with negative results. The infant was highly suspicious of SAR−COV-2 infection according to his epidemiological survey and CT results, so he was been nursed in an isolation unit with his family caregivers. On February 15, cough, and a white−Color sputum developed in the infant, and he was prescribed ambroxol. A follow-up CT scan performed on February 18 showed no improvement, and he was considered to have interstitial pneumonia in consultation. Oseltamivir phosphate and cetirizine were added to his regimen, but his symptoms were not markedly improved after 2 days of medication. On February 19, ribavirin was added to his regimen (Fig.2). The results indicated that prophylactic use of antiviral drugs might be ineffective and should be limited.
Fig. 2.
The duration of symptoms and therapeutic process of the infant.
*Abbreviation: BZS, Boric acid zinc oxide ointment.
However, on February 21, the infant’s first anal swab was positive via real-time PCR. Thus he was diagnosed as a laboratory-confirmed COVID-19 patient. The symptoms of stuffy nose, sneeze and intermittent cough remained but were slightly relieved, and a red rash appeared on his face (Fig.2). The sound of his breathing was rough, and his chest auscultation was normal. Other laboratory findings were basically normal, except for the elevated B lymphocytes, T lymphocytes, and NK cells, which indicated an unstable immune response (Table. 1). Particularly, IL-17A, IL-17 F and TNF-α were increased in the serum by 102.7 % (from 56.1% to 157.7%), 24.6 % (from 14.6% to 34.5%) and 27.0 % (from 18.6% to 32.1%) compared with the upper limit for normal people, respectively. These findings indicated that IL-17A, IL-17 F and TNF-α might function as an immune response against COVID-19 in infants.
Table 1.
Laboratory test results for a SARS−COV-2 infected infant during hospitalization, China, Feb-Mar 2020a.
| Programs | Reference range | Feb 13, Illness day 4, hospital day 1 | Feb 22, Illness day 13, hospital day 10 | Feb 24, Illness day 15, hospital day 12 | Feb 29, Illness day 19, hospital day 16 | Mar 2, Illness day 20, hospital day 17 | Mar 4, Illness day 23, hospital day 20 | Mar 5, Illness day 24, hospital day 21 |
|---|---|---|---|---|---|---|---|---|
| CRP, ng/L | 0−8.2 | <0.50 | <0.50 | – | 0.9 | – | 0.50 | – |
| Leukocytes,×109 cells/L | 5.0–12.0 | 11.67 | 12.5 | – | 5.2 | – | 6.9 | – |
| Neutrophils,×109cells/L | 2.0–7.2 | 2.23 | 1.70 | – | 2.59 | – | 0.86 | – |
| Lymphocytes,×109 cells/L | 1.55−4.8 | 8.48 | 9.84 | – | 1.94 | – | 5.42 | – |
| Platelets,×109 cells/L | 140−440 | 393 | 479 | – | 339 | – | 349 | – |
| NK cell, cells/μL | 90−590 | – | – | 1192.72 | – | 718.02 | – | 219.97 |
| B lymphocytes, cells/μL | 90−660 | – | – | 1440.63 | – | 278.98 | – | 1067.59 |
| T lymphocytes, cells/μL | 690−2540 | – | – | 6633.60 | – | 975.88 | – | 3889.25 |
| helper T lymphocyte | 410−1590 | – | – | 4313.47 | – | 492.03 | – | 2850.21 |
| suppressor T lymphocyte | 190−1140 | – | – | 1914.71 | – | 341.03 | – | 986.53 |
| Lactic acid, mmol/L | 0.9−1.7 | – | 4.20 | – | – | – | 1.60 | – |
| Creatinine, μmol/L | 18−62 | – | 29 | – | – | – | 15 | – |
| ALT, U/L | 5.0–40.0 | – | 25 | – | – | – | 29 | – |
| AST, U/L | 8.0–40.0 | – | 27 | – | – | – | 33 | – |
| CK, U/L | 45−390 | – | 91 | – | – | – | 166 | – |
| IL-2, pg/mL | 0–5.03 | – | – | – | – | 3.23 | – | 5.01 |
| IL-4, pg/mL | 0−4.62 | – | – | – | – | 5.57 | – | 3.82 |
| IL-5, pg/mL | 0–3.73 | – | – | – | – | 2.25 | – | 3.89 |
| IL-6, pg/mL | 0–8.88 | – | – | – | – | 6.23 | – | 0.62 |
| IL-10, pg/mL | 0–8.14 | – | – | – | – | 1.84 | – | 4.69 |
| IL-17A,pg/mL | 0−3.71 | – | – | – | – | 5.79 | – | 9.56 |
| IL-17 F, pg/mL | 0−4.66 | – | – | – | – | 6.27 | – | 5.34 |
| TNF-α, pg/mL | 0–5.35 | – | – | – | – | 6.53 | – | 7.06 |
| IFN-γ, pg/mL | 0−6.56 | – | – | – | – | 4.17 | – | 6.57 |
| IgM,g/L | 0.44−1.44 | – | 1.69 | – | – | – | – | – |
| IgG,g/L | 5.00−10.60 | – | 8.64 | – | – | – | – | – |
| IgA,g/L | 0.34−1.38 | – | 0.84 | – | – | – | – | – |
ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; IFN, interferon; IL, interleukin; TNF, tumor necrosis factor; –, not available.
As the infant’s respiratory status was stable, no other medicine except for boric acid zinc oxide ointment and mometasone furoate were used for treating the rash. In addition, intensive care, nutrition support was adopted. After 5 days of care, his cough disappeared. On February 28, the red rash was dissipated after 6 days of treatment with topical boric acid zinc oxide ointment and mometasone furoate, and a follow-up CT scan showed bilateral lower lobe patchy shadows and considered as hypostatic pneumonia, and was placed in a prone position to prevent choking cough. He was transferred to a general isolation ward on March 6 after 2 negative throat swabs. For tracking detection, various types of specimens were tested by real-time PCR during the 40 days he spent in hospital, all throat swabs and urine tests were negative, but his anal swab was still positive up to 40 days after the onset of COVID-19(Table. 2).
Table 2.
The nucleic acid detection results of SARS-CoV-2 of the infant in 2020a.
| Date of detected | Feb 13 | Feb 14 | Feb 15 | Feb 20 | Feb 21 | Feb 22 | Feb 24 | Feb 25 | Feb 27 | Feb 29 | Mar 2 | Mar 3 | Mar 4 | Mar 5 | Mar 13 | Mar 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Illness day | 4 | 5 | 6 | 11 | 12 | 13 | 15 | 16 | 18 | 20 | 22 | 23 | 24 | 25 | 33 | 40 |
| Hospitalized day | 1 | 2 | 3 | 8 | 9 | 10 | 12 | 13 | 15 | 17 | 19 | 20 | 21 | 22 | 30 | 37 |
| Throat swab | – | – | – | NA | – | – | – | NA | NA | NA | NA | NA | – | – | – | – |
| Anal swab | NA | NA | NA | + | + | NA | + | + | + | + | + | NA | + | NA | + | + |
| Urine | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | – | – | NA | – | NA | NA |
Abbreviation: NA, not available; -, negative; +, positive.
Analysis of the source and route of infection of the infant
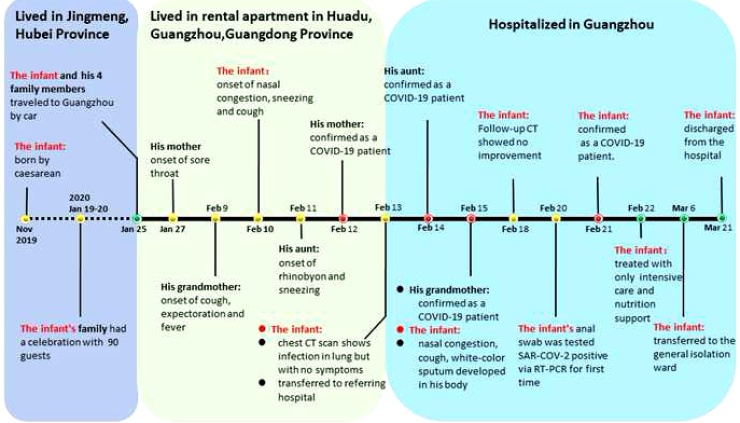
The source of infection of the infant’s mother, the first confirmed patient in this family, was most likely one or more of the guests that his family invited to a celebration according to our epidemiological investigation. On January 19 and 20, 2020, the infant’s family had hosted a feast celebrating his first month birthday at their home in Jingmeng. The two-day party included approximately 90 friends and family members, some of whom were from Wuhan, where COVID-19 was already spreading rapidly in that period. None of the participants wore masks during the dinner. The infant’s family, including his parents, grandparents, aunt and brother was in contact with their guests without effective protective measures. Although it was not possible for us to test these guests, it is reasonable to suspect that one or more of them could be the source of infection.
The infant was most likely infected by his mother. The main reasons for this belief are as follows. First, his mother had the symptom of a sore throat on January 27, and was hospitalized in an isolation unit until February 10. She was confirmed as a COVID patient on February 12. The infant’s family lived together without using effective protective measures in that period. Second, the secondary cases of COVID-19 reported in his family showed an onset within the same incubation period after the infant’s mother (Fig.3). Third, the infant, his aunt, and his grandmother experienced onset during a similar period of time, so it can be reasonably inferred that they were not infected by each other. Last, most of time during the period of January 25 to February 9, the infant was in contact only with his family members in their rental houses in Guangzhou, and was cared for by his mother most of this time. The infant was never in contact with other confirmed COVID-19 patients, except his mother.
Fig. 3.
Timeline of epidemic and clinical progress of the infant and the other confirmed COVID-19 patients in his family (n = 4).
In our investigation, it is commonly perceived that the infant was infected through close contact or droplet because his family members did not wear masks or gloves. However, we cannot rule out the possibility that the infant was infected from breastfeeding, which was a suspected exposure to his mother.
Discussion
We reported the case of a 3-month-old infant who was confirmed as a COVID-19 patient with pneumonia. His symptoms were similar to the flu, but he had no fever, and his chest CT scan manifestation was not paralleled with clinical symptoms. In line with other studies, our research suggested that infants may have relative mild symptoms and clinical signs compared to adults. One possible reason is that infants were not able to over-activated immune systems like adults during the dysregulation phase, thus causing less organ impairment [11]. The prognosis for infants is generally good, but there is no evidence to suggest the long-term effect. As of 19 days after onset, our patient remains a CT appearance of pneumonia. Considering that SARS−COV-2 is similar to SARS in sequence, we reviewed relative studies of SARS. Based on 1 follow-up study [12], all children were clinically asymptomatic 6 months after infection with SARS, but approximately 10 % of the children had a mild obstructive or restrictive defect on lung function assessment, and substantially more patients (34 %) had abnormal high-resolution CT scan of the thorax. To assess the short-and long-term effects of COVID-19, intensive follow-up of these infected infants is needed.
In most studies [13], lymphocytopenia has generally been observed in COVID-19 patients and has been established as a defining characteristic for COVID-19. However persistent lymphocytosis in COVID patients has been reported recently [14]. We observed a persistent elevated lymphocyte in our patient, further study showed that both the B and T lymphocytes were elevated, in which elevated helper T cells is the main factor. According to a previous study [15], patients infected with SARS-CoV-2 showed that higher levels of proinflammatory cytokines, including IL-2, IL-7, IL-10, and TNF-α were elevated only in severe COVID-19 cases. Although it was observed that IL-17A, IL-17 F, and TNF-α rose steadily in our patient, we posit that infants may have a different immune response compared with adults owing to their immature immune system. IL-17 is a cytokine mainly produced by Th17 and γδT cells that is best known for its protective properties during bacterial infections and involvement in inflammatory responses during viral infection [16]. The combination of IL-17 with TNF-α-induced a synergistic response on the stabilization of KC mRNA [17]. Therefore, more clinical data and research are needed to explore the underlying pathogenesis on COVID-19.
In our patient, all throat swabs were negative, but the anal swab remained positive up to 40 days after the onset of illness. Although we have not detected viral nucleic acid in the patient’s urine sample, recent research has detected viral nucleic acid from stool [18]. This suggested that SARS−COV-2 may shed through the gastrointestinal tract, and that convalescents may carry the virus for a long period. Our results agree with those of Wu et al. and Shi et al. [19,20], but not with those of Kim et al. [21], which showed positive testing up to day 16 of admission with nasopharynx swab of a 6-month-old patient. It is suggested that infants infected with SARS−COV-2 may follow different viral excretion patterns during their infected period. Owing to the scarce detection of throat swabs in the early stage, our patient was diagnosed in the first 7 days after admission. Thus, to improve early diagnosis of cases, we recommend that different types of samples should be collected. In addition, to prevent possible fecal-oral transmission, sufficient quarantine and reinforcing disinfection monitoring is needed for infant patients.
Our patient was given antiviral drugs in the early onset stage but not for the late-stage, when he was treated only with intensive care and nutrition support. According to the Chinese experts’ consensus statement on diagnosis, treatment and prevention of COVID-19 in children(2nd Edition) [22], antiviral drugs are not recommended, given that their adverse reaction is not clear. The therapeutic process of our patient suggested that infants can be cured without using long-term antiviral drugs. Thus, antiviral drugs should not be abused without careful assessment.
In our research, the infant was most likely infected by his mother, and we cannot rule out the possibility that the infant acquired his infection from breastfeeding. Thus far, the transmission of SARS−COV-2 from mother to child has been controversial [23]. Some researchers [24,25] have found that SARS−COV-2 is not transmitted to infants through breast milk, amniotic fluid or placenta, but other studies [9,26] have shown that antibodies and viral RNA can be detected in breast milk, which suggests a possible mother -to -child transmission of the virus. Very recent work [27] has demonstrated that angiotensin−COnverting enzyme 2 (ACE2) is an important receptor for SARS−COV-2 to attack the human body, and both oral cavity and mammary tissues express this receptor, which undoubtedly increases the possibility of breast milk as a vector to transmit COVID-19. In this study, although there were no nucleic acids and antibodies detected in the breast milk of the patient's mother, detailed and reliable epidemiological investigation could also show evidence that the infant could potentially have been exposed by his mother. In view of its uncertain risk, the Maternal-fetal Medicine Professional Committee of Chinese Medical Doctors Association did not recommend breastfeeding [28]. However, the WHO recommends breastfeeding while applying appropriate respiratory hygiene, hand hygiene and environmental cleaning precautions [29]. Taken together, more interdisciplinary research in this field is required and should be performed rigorously and rapidly to provide best information for policies regarding clinical management of breastfeeding mothers and their infants with COVID-19.
In conclusion, although limited by sample size, this study’s findings indicate that infant patients with COVID-19 may have relatively mild symptoms and different immune responses compared with adults. In addition, infant patients may be convalescent carriers. Thus, further control measures should be taken, including early detection of different types of specimens, sufficient quarantine and reinforcing disinfection monitoring. Increased awareness of intensive follow-up after discharge are also of utmost importance.
Contributons
Yuehong Wei and Jun Yuan: Contributed significantly to the conception of the study.
Jie Shi and Xiao Zhang: Contributed to data collection and manuscript preparation.
Xuexing Liu: Performed the data analyses and wrote the manuscript.
Lin Zhang and Chaojun Xie: Helped perform the analysis with constructive discussions.
Funding
This study is supported by the National Natural Science. Foundation of China (81473034), the Science and Technology Plan Grant of Guangzhou, China (http://www.gzsi.gov.cn/, 201607010130), and the Project for Key Medicine Discipline Construction of Guangzhou Municipality (http://www.gzmed.gov.cn/rhin_gzmed/index.html, 2017-2019-07).
Ethical approval
This study was carried out with written informed consent from the patient’s parent and approved by Center for Disease Control and Prevention of Guangzhou.
Declaration of Competing Interest
None of authors has any potential conflicts to disclosed.
Acknowledgments
We thank the patient and his family for participating in this study. We also thank all the medical, nursing, environmental services and laboratory teams that were involved in the patient’s care along with the local CDC staffs and community workers.
Contributor Information
Dahu Wang, Email: 273091834@qq.com.
Lin Zhang, Email: 378563318@qq.com.
Chaojun Xie, Email: 15876582417@163.com.
References
- 1.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19) situation dashboard. Available at: https://covid19.who.int/Accessed 20 April 2020. [Google Scholar]
- 2.She J., Liu L., Liu W. COVID-19 epidemic: disease characteristics in children. J Med Virol. 2020;92(7):747–754. doi: 10.1002/jmv.25807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z., Mcgoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.National Health Commission of the People’S Republic of China . 2020. Update of Coronavirus disease 2019 (COVID-19) Situation in China, as of 24:00, 19 April 2020. Available at: http://www.nhc.gov.cn/xcs/yqfkdt/202004/fceb99a885cd43698- 0656f292a1c7282.shtml. Accessed 20 April 2020. [Google Scholar]
- 5.Lackey K.A., Pace R.M., Williams J.E. SARS‐CoV‐2 and human milk: what is the evidence? Matern Child Nutr. 2020 doi: 10.1111/mcn.13032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan C., Lei D., Fang C. Perinatal transmission of COVID-19 Associated SARS-CoV-2: should we worry? Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa226. ciaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang S., Guo L., Chen L. A case report of neonatal COVID-19 infection in China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa225. ciaa225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salvatori G., De Rose D.U., Concato C. Managing COVID-19-positive maternal-infant dyads: an Italian experience. Breastfeed Med. 2020;15(5):347–348. doi: 10.1089/bfm.2020.0095. [DOI] [PubMed] [Google Scholar]
- 9.Gross R., Conzelmann C., Muller J.A. Detection of SARS-CoV-2 in human breastmilk. Lancet. 2020;395(10239):1757–1758. doi: 10.1016/S0140-6736(20)31181-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Health Commission of the People’s Republic of China . 6th edn. 2020. New coronavirus pneumonia diagnosis and treatment program. Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202002/8334a8326dd94d329df351d7da8aefc2.shtmlAccessed 19 February 2020. [Google Scholar]
- 11.Li A.M. Severe acute respiratory syndrome (SARS) in neonates and children. Arch Dis Child-Fetal. 2005;90(6):F461–F465. doi: 10.1136/adc.2005.075309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li A.M., So H.K., Chu W. Radiological and pulmonary function outcomes of children with SARS. Pediatr Pulmonol Suppl. 2004;38(6):427–433. doi: 10.1002/ppul.20078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen K., Yang Y., Wang T. Diagnosis, treatment, and prevention of 2019 novel coronavirus infection in children: experts’ consensus statement. World J Pediatr. 2020 doi: 10.1007/s12519-020-00343-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ryzhakov G., Lai C.C., Blazek K. IL-17 boosts proinflammatory outcome of antiviral response in human cells. J Immunol. 2011;187(10):5357–5362. doi: 10.4049/jimmunol.1100917. [DOI] [PubMed] [Google Scholar]
- 17.Hartupee J., Liu C., Novotny M. IL-17 enhances chemokine gene expression through mRNA stabilization. J Immunol. 2007;179(6):4135–4141. doi: 10.4049/jimmunol.179.6.4135. [DOI] [PubMed] [Google Scholar]
- 18.He Y., Wang Z., Li F. Public health might be endangered by possible prolonged discharge of SARS-CoV-2 in stool. J Infection. 2020;80(5):e18–e19. doi: 10.1016/j.jinf.2020.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Y., Guo C., Tang L. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5(5):434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu Y., Li X., Zhu B. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26(4):502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kam K.Q., Yung C.F., Cui L. A well infant with Coronavirus disease 2019 (COVID-19) with high viral load. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yi J., Xiaoxia L., Runming J. Diagnosis, treatment and prevention of 2019 novel coronavirus in children: experts′consensus statement (Second Edition) Chin J Appl Clin Pediatr. 2020;35(2):143–150. [Google Scholar]
- 23.Yang N., Che S., Zhang J. Breastfeeding of infants born to mothers with COVID-19: a rapid review. Ann Transl Med. 2020;8(10):618. doi: 10.21037/atm-20-3299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang H., Wang C., Poon L.C. Novel Coronavirus infection and pregnancy. Ultrasound Obstet Gynecol. 2020;55(4):435–437. doi: 10.1002/uog.22006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen H., Guo J., Wang C. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dong L., Tian J., He S. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323(18):1846–1848. doi: 10.1001/jama.2020.4621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu H., Zhong L., Deng J. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12(1):8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maternal and Fetal Experts Committee, Obstetric Subgroup, Society of Perinatal Medicine Proposed management of COVID-19 during pregnancy and puerperium. Chin J Perinat Med. 2020;23(02):73–79. [Google Scholar]
- 29.World Health Organization . 2020. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance. Available at: https://www.who.int/publications/i/item/clinical-management-of-severe -acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed 13 April 2020. [Google Scholar]