Abstract
The COVID-19 pandemic has resulted in enormous losses in terms of human lives and economy in United States. The outbreak has been continuing to heavily impact the mental health of people. Developing key strategies to prevent mental illnesses is extremely important for the well-being of people. A survey conducted during the last week of March 2020 showed that 72% of Americans felt that their lives were impacted by the outbreak, which was a 32% increase from the survey conducted only 2 weeks earlier. The results show a positive correlation between COVID-19 infections/casualties and growing public concern. These observations suggest possible increase in mental health illnesses in United States as a consequence of the pandemic. The authors review a recently published model on COVID-19 related fear among the people. The fear of being infected or dying from the disease is one of the most significant causes of mental health disorders. Loss of employment or the fear of losing employment is another major concern leading to mental illnesses. Several unique strategies to prevent or mitigate mental illnesses are discussed.
Keywords: COVID-19, Mental health, Anxiety disorder, Pandemic, Prevention strategies
Introduction
The COVID-19 epidemic started at Wuhan, China and within a few months became a global pandemic. The World Health Organization (WHO) declared the COVID-19 outbreak as a public health hazard of international concern on January 30, 2020 [1]. At this time, 34 regions in China had reported infections and the total number of cases exceeded that for the 2003 Severe Acute Respiratory Syndrome (SARS). On the same day, United States Centers for Disease Control and Prevention (CDC) confirmed the first case of person to person transmission in United States. On January 31, 2020 Health and Human Services (HHS) declared Coronavirus a public health emergency in United States. Again, on the same day, CDC issued a federal quarantine for 2 weeks affecting 195 American evacuees from Wuhan, China [2]. The first COVID-19 death in United States of America was reported on February 29, 2020. Over the next 71 days, the virus hit United States of America especially hard resulting in 80,787 deaths and over 1.36 million infections. During pandemics it is common for healthcare professionals and scientists to primarily focus on the pathogen to study its mechanism with an aim of containing it and treating the disease. Under these conditions, the secondary effects such as the effect of the pandemic on human psychiatry tend to be neglected [3]. Historically, disease outbreaks and epidemics have been known to cause mental illnesses. For instance, during the Korean MERS outbreak, patients who were isolated for hemodialysis reported high levels of stress [4]. In addition, several reports exist where high levels of Post-Traumatic Stress Disorders (PTSD) were reported due to isolation following a major traumatic event such as an act of terrorism, natural calamity, or a disease outbreak [5–7]. In this article, the authors critically examine the onset of the pandemic in United States of America focusing on its effect on the mental health of American people. The authors discuss various strategies to overcome the mental health challenges associated with both the outbreak and response.
The 2020 COVID-19 Pandemic in United States
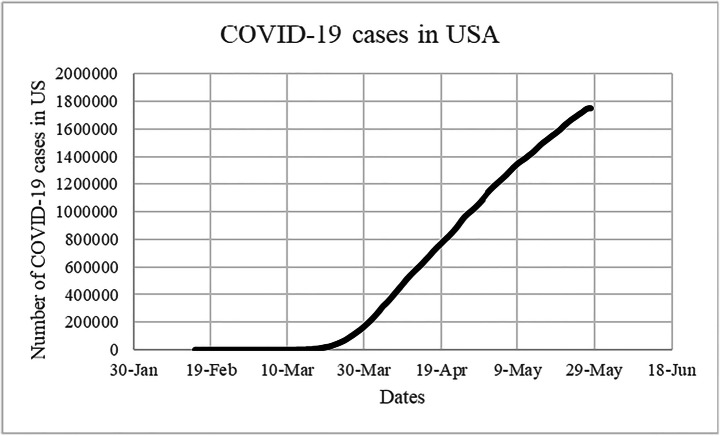
Figure 1 shows the number of COVID-19 cases in United States from beginning through May 28, 2020 [8].
Fig. 1.
Cumulative COVID-19 cases in United States till May 28, 2020
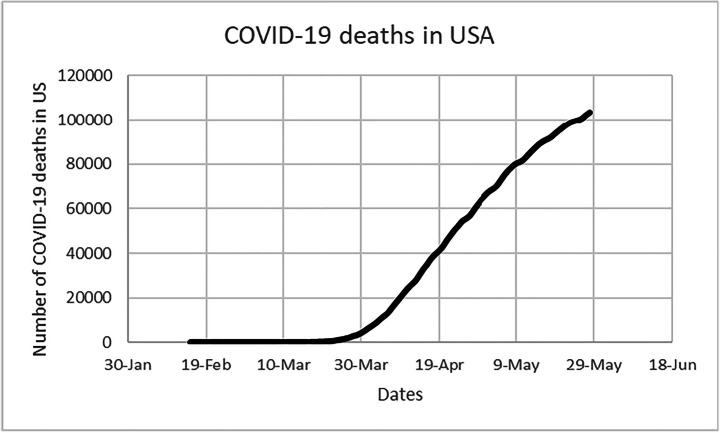
Figure 2 shows the total number of COVID-19 deaths in United States respectively between February 15, 2020 and May 28, 2020. The total number of COVID-19 cases and deaths started increasing rapidly from March 20, 2020. Currently, the total number of COVID-19 deaths in United States has already crossed 100,000.
Fig. 2.
Cumulative COVID-19 deaths in United States till May 28, 2020
With the increase in the number of COVID-19 cases in United States from March through April 2020, there has been a rise in fear in the minds of people. In addition to the uncertainties caused by the disease itself, people have been experiencing additional insecurities due to conflicting and dubious information about disease transmission, inadequate control measures, and lack of efficient therapeutic mechanisms. Non availability of adequate protective gear for healthcare professionals has created additional barriers [9, 10]. Besides, the lockdown required to slow down the spread of the disease has resulted in tremendous losses to the economy resulting in widespread loss of employment. All of the factors mentioned above contribute towards mental health disorders among people.
Health Tracking Polls
Kaiser Family Foundation (KFF) conducts health tracking polls in United States. There were two such polls conducted: (a) March 11–15, 2020, and (b) March 25–30, 2020. Following are some of the findings from the two polls [11–13]:
The poll conducted on March 25–30, 2020 reported 72% of Americans expressing that their lives were disrupted “a lot” or “some” by the COVID-19 outbreak. This is a 32% increase from the poll conducted 2 weeks earlier [12].
While 57% of the adults expressed concerns over being exposed to coronavirus while they were at work, 53% were worried that they or someone in their family would be sick from coronavirus [12].
About 59% worried that their investments would be negatively impacted by coronavirus for a long time [12].
While 52% worried that the economic downturn due to coronavirus would cause them to lose their jobs, 45% worried that they would lose income due to workplace closure or reduced work hours [12].
About 74% were worried that the worst from the outbreak was yet to come [12].
The above findings are directly related to the sharp increase in COVID-19 cases and COVID-19 related deaths in United States during the same period as indicated by Figs. 1 and 2. This suggests that the COVID-19 pandemic and its effect on the economy in United States may lead to an increase in mental health illness in the country.
Population Groups Prone to Mental Illnesses
In order to completely assess the effect of the 2020 COVID-19 outbreak on the mental health, it is important to learn about the population groups susceptible to mental health illnesses:
Elderly people: Elderly people are particularly prone to mental illness during the current pandemic. Over the past 10 years in United States, the population age group 65 and above increased from 37.2 million in 2006 to 49.2 million in 2016. The population of this age group is projected to almost double to 98 million in 2060. Likewise, between 2006 and 2016, the population age group 60 and above increased by 36% from 50.7 million to 68.7 million. Currently, approximately 15.2% of the American population comprises of the elderly [14, 15].
Professionals: People who are employed are under immense mental stress regarding their job security during the current economic downturn. Currently, 144 million professionals are employed in United States and approximately 10% of them are employed in occupations where exposure to the disease or infection may occur atleast once a week [16].
Healthcare Professionals: Healthcare professionals are highly vulnerable because they are directly involved with treating patients. According to the Centers for Disease Control and Prevention, currently 18 million workers are working in the healthcare industry. Healthcare is the fastest growing sector of the US economy [17].
Children and teenagers: Children and teenagers are prone to mental disorders during the current situation. In United States, the population group under 18 years of age has increased from 47.3 million in 1950 to 73.7 million in 2017 [18].
People with past and family psychiatric history: People with past and family psychiatric history are particularly prone to mental illnesses. Currently 18.57% of American adult population has been experiencing mental health problems. This is equivalent to 45 million people in United States [19].
Characteristics of Mental Disorders
The pandemic and the associated economic downturn may trigger mental disorders of varying complexity within the American society. Some of the common mental disorders may be classified as (i) psychotic disorders, (ii) mood disorders, and (iii) anxiety disorders [20].
Psychotic disorders are characterized by significant impairment of reality testing, and may be classified as disorders such as schizophrenia, schizophreniform disorders, schizoaffective disorders, brief psychotic disorders, and delusional disorders. Schizophrenia is usually diagnosed through two or more of the following disorders being present for significant amount of time through a period of 1 month. These disorders may be delusions, hallucinations, formal thought disorder, anhedonia, and avolition. Anhedonia is the inability to feel pleasure and avolition is associated with decrease in motivation to perform self-directed purposeful activities. Schizophrenia is characterized by at-least 6 months of continuous disturbance. The influenza pandemic of 1957 was caused by an influenza A viral strain. Several reports exist that related the pandemic to onset of schizophrenia among the people [21–23]. Schizophreniform Disorder is similar to schizophrenia with the exception that the episode of the disorder lasts for at least 1 month but less than 6 months. Brief psychotic disorder is similar to schizophrenia, and is characterized by delusions, hallucinations, formal thought disorder, and avolition. The duration of this disorder is at least 1 day but is less than 1 month. Schizoaffective disorder is characterized by delusions, hallucinations, formal thought disorder, anhedonia, and avolition. This may also be accompanied by a major mood episode and an uninterrupted period of illness. These are also characterized by delusions or hallucinations for 2 weeks or more in the absence of a major mood episode during the period of illness. Delusional Disorder is associated with the presence of one or more delusions through a period of 1 month or more. However, the other criteria for schizophrenia are never met.
In addition to psychotic disorders, mood disorders may be very common among people during an outbreak [24, 25]. These are characterized by combination of symptoms comprising a predominant mood state of abnormal quality and duration. Mood disorders can be classified as mood episodes and mood disorders. Major Depressive Mood Episode is associated with symptoms such as depressed mood throughout the day, markedly diminished interest and pleasure, significant and unintentional weight loss, decrease or increase in appetite, or insomnia through a 2-week period. A manic episode is associated with a distinct period of persistent and abnormally elevated, expansive or irritable mood which may lead to increased goal-directed activity or energy lasting more than a week. This is also present through most part of the day. Major depressive disorders are characterized by the depressive mood episodes which are not accounted for by schizoaffective disorder and are not superimposed on other diseases such as schizophrenia or schizophreniform disorder. Persistent depressive disorders are characterized by depressed mood for most of the day, for more days than not, for a duration of 2 years or more. These disorders are also associated with lack of appetite or overeating, insomnia or hypersomnia, fatigue, low self-esteem, poor concentration, and feeling of hopelessness. Depressive disorders are twice as prevalent in females as in males. The peak prevalence age of depressive disorders is 15–25 years. Recent stressors associated with the 2020 COVID-19 pandemic such as illnesses, social isolation, depressive home environment, and financial hardship can cause depressive disorders.
During previous influenza outbreaks, anxiety disorders have been reported in some articles [26, 27]. Anxiety disorders may result in social or occupational functioning being impaired. Possible forms of anxiety disorders resulting from the 2020 COVID-19 pandemic may be as follows:
Panic Disorder: This is characterized by an abrupt surge of intense fear and discomfort which may reach its peak within a few minutes. Panic disorders are also characterized by symptoms such as palpitations and accelerated heart rate, perspiration, trembling, shortness of breath, feelings of choking, nausea or abdominal distress, dizziness, derealization, or depersonalization. This disorder is twice or thrice as common in women than in men. The average age of onset is early to mid-20s.
Agoraphobia: This is determined by conspicuous fear of two or more of the following: using public transportation, being in open spaces, standing in a line or being in a crowd, or being outside of the home alone. The fear or anxiety may be persistent and may last for 6 months or more. During the current COVID-19 pandemic, social distancing has been suggested as an effective method to stop the disease from spreading. However, long-term social distancing may lead to agoraphobia among people.
Obsessive-Compulsive Disorder: The obsessions are defined by recurrent and persistent thoughts or images that are experienced sometimes during the period of disturbance. These obsessions are intrusive and unwanted and cause distress and anxiety in most individuals. In the COVID-19 pandemic, people are required to wash their hands as often as possible. However, excessive handwashing may develop into an obsessive-compulsive disorder among many.
Phobic Disorder: Phobic disorders are associated with either specific phobia or social phobia. Social phobia is defined as marked and persistent fear of situations where one is exposed to unfamiliar people or possible scrutiny by others. The current situation during the COVID-19 pandemic and pro-longed social distancing although necessary, may facilitate social phobia among people.
Post-Traumatic Stress Disorder: Post-Traumatic Stress Disorder may result from someone being exposed to actual or threatened death, serious injury, or sexual violence either through direct experience, or by witnessing the event in another person. The disorder may also be developed in a person when they learn about the trauma occurring to someone they know. The increasing number of COVID-19 deaths as shown by Fig. 2 may result in widespread post-traumatic stress disorders among people.
Substance-Related and Addictive Disorders: These are neurobiological disorders that involve compulsive seeking and usage of drugs and alcohol, despite adverse consequences with loss of control over drug and alcohol. Substance abuse is common during disease outbreaks and pandemics [28, 29]. A recent report suggests as many as 150,000 Americans being at risk of dying from drug/alcohol abuse or suicide due to coronavirus related despair [30].
Illness Anxiety Disorder: This is a disorder that is defined as the preoccupation of fear of having a serious disease to the point of causing significant impairment. A person may engage in maladaptive behavior such as excessive physical checking or total healthcare avoidance. This disorder can continue for a duration longer than 6 months and the usual onset is in the 20s or 30s.
Sleep Disorders: Adequate sleep is extremely necessary for normal functioning of human body. Sleep deprivation can lead to cognitive impairment and increased mortality. Several reports suggest that influenza disease outbreaks lead to chronic sleep disorders [31, 32].
Eating Disorders: Eating disorders are characterized by persistent disturbance of eating that impairs functioning of health. Anorexia Nervosa is an eating disorder where people develop unwarranted fear of being overweight and as a result may severely impair their health by starvation and over-exercise. Binge-Eating Disorder is associated with eating much more rapidly than normal and eating until one feels uncomfortably full. Bulimia Nervosa is a disorder characterized by recurrent episodes of overeating, and a recurrent inappropriate compensatory behavior in order to prevent weight gain, such as self-induced vomiting, fasting, excessive exercise, and inappropriate use of laxatives.
Discussion of Strategies to Prevent Mental Illness during the Pandemic
A recent article argued that fear experiences during the current pandemic may be modeled as a relationship between four interrelated dialectical domains such as: (i) fear of/for the body (ii) fear of/for significant others (iii) fear of knowing/not knowing (iv) fear of taking action/fear of inaction [33]. In the following section, the authors discuss strategies that may be useful towards preventing/mitigating mental illnesses due to the above-mentioned fears.
Effective Use of Electronic and Social Media to Communicate during the Pandemic
Fear of/for the body is associated with the fear of being infected and ultimately dying from the infection. The fear of being infected may be managed by curtailing physical contact. However, the authors recommend keeping close contact with family and friends through electronic and social media. A recent study suggested facetime being useful to reduce behavioral problems in nursing home patients suffering from dementia during the current COVID-19 crisis [34].
Healthy Expression of Emotions
Fear of/for significant others relates to a person’s worries regarding being infected by or infecting his/her significant others. Likewise, the fear of taking action/inaction is related to consequences related to human interpersonal behavior during the pandemic. For instance, a person’s sense of visiting and caring for his elderly parents may interfere with his fear of infecting them. People are therefore deprived of their normal roles of caring for or being cared for by their significant others, which may lead to sense of solitude. One way of preventing solitude is by developing a supportive network where people may share each other’s worries and discuss strategies. The authors suggest healthy expression of emotions and thoughts as a way of avoiding mental illnesses as they should avoid suppression of sadness or anxiety during the current crisis period.
Limiting Exposure to Pandemic Related News
The fear of knowing/not knowing concerns with the limited availability of information regarding the disease. Often times inadequate knowledge leads to misinformation and unnecessary panic among the people. Therefore, people should limit their exposure to pandemic-related news because too much information may lead to the anxiety disorders mentioned above [3].
Focusing on the Positive and Improving Skills
The pandemic and the corresponding economic downturn have resulted in unemployment, and this may lead to both anxiety and psychotic disorders among the people [35]. In many cases long term unemployment can lead to disruption of family life resulting in divorce [36, 37]. It is believed that fear of losing employment can be minimized through positive thinking. In the unfortunate event of loss of employment, a person may focus on improving his/her qualifications and skills that make him/her more marketable to the industry.
Regulating Eating and Sleeping Habits
The authors suggest maintaining healthy eating and sleeping habits as effective methods towards preventing mental illnesses during the current outbreak. A previous research has reported mindful eating being useful towards reducing depressive symptoms [38]. Several previous reports have shown direct relationships between maintaining a healthy sleep cycle and avoiding mental illnesses [39–42].
Yoga and Meditation
Performing Yoga have been proven to be beneficial towards managing mental health [43–45]. A previous study reported the effectiveness of managing trauma using yoga due to separate conditions which included unprecedented natural disasters such as Tsunami [46]. The authors suggest practicing yoga and meditation to manage mental health during the current COVID-19 crisis.
Guidelines for Healthcare Workers
The Center for Disease Control (CDC) has published several guidelines for coping with the pandemic [47, 48]. Among these are guidelines that are relevant to healthcare professionals and responders. Responding to the COVID-19 crisis could take an extremely heavy emotional toll on healthcare professionals. The healthcare professionals during the current pandemic are in the ‘war zone’ attending infected patients. Often, healthcare workers have to take very difficult decisions such as allocating scant resources to patients that are equally needy. Therefore, in addition to the risk of being infected, the healthcare professionals are subjected to secondary traumatic stress. Secondary traumatic stress reactions result from direct exposure to another individual’s traumatic experiences. Such traumatic experiences among healthcare workers may cause ‘moral injury’ or mental illnesses. Moral injury is defined as the psychological distress that arises from actions or lack of actions and violates a person’s moral or ethical code [49]. The authors suggest that healthcare professionals in the country should regularly monitor their own secondary mental traumatic stress symptoms such as fear, withdrawal, and guilt. They should allow more time for themselves and their families to recover from responding to the pandemic. The healthcare workers should be made aware of the current grim situation in hospitals. They also need to be prepared for the moral dilemma that they may be facing at work. The government should take adequate measures to prepare and train healthcare professionals for their work and associated challenges to reduce the risk of mental health illnesses among them [50]. The healthcare professionals should be provided with a complete and honest assessment of the situations that they may have to face. Forums such as Schwartz Rounds should be designed to help the healthcare workers safely discuss and share the emotional challenges associated with caring of patients [51]. Reports suggest that support from immediate supervisors, colleagues, and line managers protects mental health of professionals [49]. Medical health care professionals who are either too busy to attend meetings or avoid them altogether may need help and the immediate supervisors may need to identify such situations. Finally, during an outbreak, in addition to being subjected to uncertainty, job demands, and the fear of infecting their family members, the healthcare workers may also experience social stigmatization on certain occasions [9, 52]. Stigmatization can significantly hamper the work performances of healthcare professionals. In the current situation, the government and the people of the country should strongly support healthcare workers in order to help them perform to the best of their abilities.
Biographies
Dr. Barnali Bhattacharjee
completed her undergraduate degree in medicine and surgery (MBBS) from Gauhati Medical College, India in 2011. Through the next 7 years, she worked as a medical and health officer employed by the State of Assam in India. She is presently preparing for a medical residency program in the field of psychiatry.
Dr. Tathagata Acharya
has a PhD in mechanical engineering from Louisiana State University. He is presently working as an assistant professor at California State University, Bakersfield. He has research interests in several areas of engineering including thermo-fluid applications into medicine.
Funding Information
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants and/or Animals
This research did not involve any human participants and /or animals.
Informed Consent
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Secretary Azar declares public health emergency for United States for 2019 novel coronavirus. In: US Department of Health and Human Services. 2020 Jan 31. https://www.hhs.gov/about/news/2020/01/31/secretary-azar-declares-public-health-emergency-us-2019-novel-coronavirus.html. Accessed 29 May 2020.
- 3.Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz J Psychiatr. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim YG, Moon H, Kim SY, Lee YH, Jeong DW, Kim K, Moon JY, Lee YK, Cho A, Lee HS, Park HC. 2019. Inevitable isolation and the change of stress markers in hemodialysis patients during the 2015 MERS-CoV outbreak in Korea. Sci Rep. 2019;9(1):1–10. doi: 10.1038/s41598-019-41964-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fagan J, Galea S, Ahern J, Bonner S, Vlahov D. Relationship of self-reported asthma severity and urgent health care utilization to psychological sequelae of the September 11, 2001 terrorist attacks on the world trade center among New York City area residents. Psychosom Med. 2003;65(6):993–996. doi: 10.1097/01.psy.0000097334.48556.5f. [DOI] [PubMed] [Google Scholar]
- 6.Guerriero RM, Pier DB, De Gusmão CM, Bernson-Leung ME, Maski KP, Urion DK, Waugh JL. 2014. Increased pediatric functional neurological symptom disorders after the Boston marathon bombings: a case series. Pediatr Neurol. 2014;51(5):619–623. doi: 10.1016/j.pediatrneurol.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Torales J, O’Higgins M, Castaldelli-Maia JM and Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatr 2020; 0020764020915212. [DOI] [PubMed]
- 8.United States. In: COVID-19 coronavirus pandemic. Worldometer 2020. https://www.worldometers.info/coronavirus/country/us/. Accessed 29 May 2020.
- 9.Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 10.Ranney ML, Griffeth V, Jha AK. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. New Engl J Med. 2020;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 11.Kirzinger A, Kearney A, Hamel L, and Brodie M. KFF Health Tracking Poll – Early April 2020: The impact of coronavirus on life in America. Kaiser Family Foundation 2020.
- 12.Hamel L, Lopes L, Muñana C, Kates J, Michaud J, Brodie M. KFF coronavirus poll: March 2020. Global Health Policy Poll, Kaiser Family Foundation 2020.
- 13.Boserup B, McKenney M, Elkbuli A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020;38:1732–1736. doi: 10.1016/j.ajem.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services, 2017. Administration for Community Living, administration on aging (AoA). A Profile of Older Americans.
- 15.Anthony M. 2018. The aging of American. [DOI] [PubMed]
- 16.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One. 2020;15(4):e0232452. doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pop1 Child Population: Number of children (in millions) ages 0–17 in the United States by age. In: Forum on Child and Family Statistics. 2020. https://www.childstats.gov/americaschildren/tables/pop1.asp. Accessed 29 May 2020.
- 18.Healthcare Workers. In: The National Institute of Occupational Safety and Health (NIOSH). https://www.cdc.gov/niosh/topics/healthcare/default.html. Accessed 29 May 2020.
- 19.Charara R, El Bcheraoui C, Kravitz H, Dhingra SS, Mokdad AH. Mental distress and functional health in the United States. Prev Med. 2016;89:292–300. doi: 10.1016/j.ypmed.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 20.Mirali S. Seneviratne A. Toronto Notes. Toronto Notes for Medical Students Inc 2020.
- 21.Torrey EF, Bowler AE, and Rawlings R. An influenza epidemic and the seasonality of schizophrenic births. In: psychiatry and biological factors. Springer, Boston, 1991. Pp, 109–116.
- 22.Chistovich AS. The value of microbiological testing in the diagnosis and therapy of mental diseases. Nauch Konferen Posvyashch. 1959;20:113–119. [Google Scholar]
- 23.Prokop H. Psychosen im Rahmen der Grippeepidemie 1957/58. Arch Psychiatr Nervenkr. 1958;197(5):484–500. doi: 10.1007/BF00353292. [DOI] [PubMed] [Google Scholar]
- 24.Usher K, Bhullar N, Jackson D. Life in the pandemic: social isolation and mental health. J Clin Nurs. 2020;29:2756–2757. doi: 10.1111/jocn.15290. [DOI] [PubMed] [Google Scholar]
- 25.Hamza Shuja K, Aqeel M, Jaffar A, Ahmed A. COVID-19 pandemic and impending global mental health implications. Psychiatr Danub. 2020;32(1):32–35. doi: 10.24869/psyd.2020.32. [DOI] [PubMed] [Google Scholar]
- 26.Bournes DA, Ferguson-Paré M. Persevering through a difficult time during the SARS outbreak in Toronto. Nurs Sci Q. 2005;18(4):324–333. doi: 10.1177/0894318405280353. [DOI] [PubMed] [Google Scholar]
- 27.Lancee WJ, Maunder RG, Goldbloom DS. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alexander GC, Stoller KB, Haffajee RL, and Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. 2020. [DOI] [PMC free article] [PubMed]
- 29.Lovegrove MC, Shehab N, Hales CM, Poneleit K, Crane E, Budnitz DS. Emergency department visits for antiviral adverse events during the 2009 H1N1 influenza pandemic. Public Health Rep. 2011;126(3):312–317. doi: 10.1177/003335491112600303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O’Donnell J. ‘Death of despair’: Coronavirus pandemic could push suicide, drug deaths as high as 150k, study says, USA Today, May 8, 2020. https://www.usatoday.com/story/news/health/2020/05/08/coronavirus-pandemic-boosts-suicide-alcohol-drug-death-predictions/3081706001/. Accessed 29 May 2020.
- 31.Dauvilliers Y, Arnulf I, Lecendreux M, Monaca Charley C, Franco P, Drouot X, d'Ortho MP, Launois S, Lignot S, Bourgin P, Nogues B. Increased risk of narcolepsy in children and adults after pandemic H1N1 vaccination in France. Brain. 2013;136(8):2486–2496. doi: 10.1093/brain/awt187. [DOI] [PubMed] [Google Scholar]
- 32.Han F, Lin L, Warby SC, Faraco J, Li J, Dong SX, An P, Zhao L, Wang LH, Li QY, Yan H. Narcolepsy onset is seasonal and increased following the 2009 H1N1 pandemic in China. Ann Neurol. 2011;70(3):410–417. doi: 10.1002/ana.22587. [DOI] [PubMed] [Google Scholar]
- 33.Schimmenti A, Billieux J, Starcevic V. The four horsemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clin Neuropsychiatry. 2020;17(2):41–45. doi: 10.36131/CN20200202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Padala SP, Jendro AM, Orr LC. Facetime to reduce behavioral problems in a nursing home resident with Alzheimer's dementia during COVID-19. Psychiatry Res. 2020;288:113028. doi: 10.1016/j.psychres.2020.113028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baek C, McCrory PB, Messer T, and Mui P. Unemployment effects of stay-at-home orders: evidence from high frequency claims data. Institute for Research on labor and employment working paper; 2020, (101-20).
- 36.Jones L. The relationship between unemployment and divorce. J Divorce. 1989;12(1):99–112. doi: 10.1300/J279v12n01_06. [DOI] [Google Scholar]
- 37.Amato PR, Beattie B. Does the unemployment rate affect the divorce rate? An analysis of state data 1960–2005. Soc Sci Res. 2011;40(3):705–715. doi: 10.1016/j.ssresearch.2010.12.012. [DOI] [Google Scholar]
- 38.Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. J Eat Disord. 2010;19(1):49–61. doi: 10.1080/10640266.2011.533605. [DOI] [PubMed] [Google Scholar]
- 39.Taub JM, Hawkins DR, Van de Castle RL. Electrographic analysis of the sleep cycle in young depressed patients. Biol Psychol. 1978;7(3):203–214. doi: 10.1016/0301-0511(78)90013-3. [DOI] [PubMed] [Google Scholar]
- 40.Pandi-Perumal SR, and Kramer M. (eds). Sleep and mental illness. Cambridge University Press. 2010.
- 41.Gold AK, Sylvia LG. The role of sleep in bipolar disorder. Nat Sci Sleep. 2016;8:207–214. doi: 10.2147/NSS.S85754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown WJ, Wilkerson AK, Milanak ME, Tuerk PW, Uhde TW, Cortese BM, Grubaugh AL. An examination of sleep quality in veterans with a dual diagnosis of PTSD and severe mental illness. J Psychiatr Res. 2017;247:15–20. doi: 10.1016/j.psychres.2016.07.062. [DOI] [PubMed] [Google Scholar]
- 43.Telles S, Naveen KV. Yoga for rehabilitation: an overview. Indian J Med Sci. 1997;51(4):123–127. [PubMed] [Google Scholar]
- 44.Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med. 2005;39(12):884–891. doi: 10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Harner H, Hanlon AL, Garfinkel M. Effect of Iyengar yoga on mental health of incarcerated women: a feasibility study. Nurs Res. 2010;59(6):389–399. doi: 10.1097/NNR.0b013e3181f2e6ff. [DOI] [PubMed] [Google Scholar]
- 46.Telles S, Singh N, Balkrishna A. Managing mental health disorders resulting from trauma through yoga: a review. Depress Res Treat. 2012;2012:1–9. doi: 10.1155/2012/401513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bahl P, Doolan C, de Silva C, Chughtai AA, Bourouiba L, and MacIntyre CR. Airborne or droplet precautions for health workers treating COVID-19? J Infect Dis. 2020. [DOI] [PMC free article] [PubMed]
- 48.Park CL, Russell BS, Fendrich M, Finkelstein-Fox L, Hutchison M, Becker J. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020:1–8. [DOI] [PMC free article] [PubMed]
- 49.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368. [DOI] [PubMed]
- 50.Iversen AC, Fear NT, Ehlers A, Hughes JH, Hull L, Earnshaw M, Greenberg N, Rona R, Wessely S, Hotopf M. Risk factors for post traumatic stress disorder amongst United Kingdom armed forces personnel. Psychol Med. 2008;38(4):511–522. doi: 10.1017/S0033291708002778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Flanagan E, Chadwick R, Goodrich J, Ford C, Wickens R. Reflection for all healthcare staff: a national evaluation of Schwartz rounds. J Interprof Care. 2020;34(1):140–142. doi: 10.1080/13561820.2019.1636008. [DOI] [PubMed] [Google Scholar]
- 52.Ramaci T, Barattucci M, Ledda C, Rapisarda V. Social stigma during COVID-19 and its impact on HCWs outcomes. Sustainability. 2020;12(9):3834. [Google Scholar]