Abstract
Introduction
Efforts to enact nurse staffing legislation often lack timely, local evidence about how specific policies could directly impact the public’s health. Despite numerous studies indicating better staffing is associated with more favourable patient outcomes, only one US state (California) sets patient-to-nurse staffing standards. To inform staffing legislation actively under consideration in two other US states (New York, Illinois), we sought to determine whether staffing varies across hospitals and the consequences for patient outcomes. Coincidentally, data collection occurred just prior to the COVID-19 outbreak; thus, these data also provide a real-time example of the public health implications of chronic hospital nurse understaffing.
Methods
Survey data from nurses and patients in 254 hospitals in New York and Illinois between December 2019 and February 2020 document associations of nurse staffing with care quality, patient experiences and nurse burnout.
Results
Mean staffing in medical-surgical units varied from 3.3 to 9.7 patients per nurse, with the worst mean staffing in New York City. Over half the nurses in both states experienced high burnout. Half gave their hospitals unfavourable safety grades and two-thirds would not definitely recommend their hospitals. One-third of patients rated their hospitals less than excellent and would not definitely recommend it to others. After adjusting for confounding factors, each additional patient per nurse increased odds of nurses and per cent of patients giving unfavourable reports; ORs ranged from 1.15 to 1.52 for nurses on medical-surgical units and from 1.32 to 3.63 for nurses on intensive care units.
Conclusions
Hospital nurses were burned out and working in understaffed conditions in the weeks prior to the first wave of COVID-19 cases, posing risks to the public’s health. Such risks could be addressed by safe nurse staffing policies currently under consideration.
Keywords: health policy, health services research, nurses, patient safety
Introduction
Numerous studies and systematic reviews have described wide variation across hospitals in registered nurse (RN) staffing and have concluded that better hospital nurse staffing is associated with more favourable patient outcomes, including lower mortality,1–8 fewer complications,9 higher patient satisfaction,10 11 shorter stays and fewer readmissions,12 13 as well as better nurse outcomes such as less burnout.14 However, policy and administrative responses to this evidence have been uneven as is shown by persistent differences in nurse staffing across hospitals within the same jurisdictions15 16 and within the same countries.10 17 Policy efforts to enact safe hospital nurse staffing legislation often fail to pass because of a lack of timely, local evidence to inform how policy choices could directly impact the public’s health. The main purpose of this study is to provide relevant evidence to inform hospital nurse staffing legislation under consideration in two states (New York (NY) and Illinois (IL))18 19 by determining the variation across hospitals in patient-to-nurse staffing and its association with quality of care including nurse job outcomes (eg, burnout), nurse-reported measures of care quality and patient reports of satisfaction with their care.
The secondary purpose of this study is to discuss the policy relevance and implications of our findings in the context of the COVID-19 pandemic—a real-time example of the public health implications of chronic hospital nurse understaffing. Indeed, the pandemic has highlighted some of the pre-existing realities and inequities within the US healthcare system—among them: understaffed hospitals, a burned-out clinician workforce and poorer health outcomes among racial minorities.20 In the International Year of the Nurse, the COVID-19 pandemic brings daily images of nurses saving lives, comforting the sick, providing essential screening, all at significant personal risk. News stories abound with front-line nurses who are under-resourced to care for the surge of critically ill patients. Nurses in hospitals have long struggled with high patient workloads and burnout.7 21 22 In this study, we present evidence as of late February 2020 in NY and IL, international gateways into the USA, of widespread hospital nurse understaffing and burnout immediately prior to the surge of critically ill patients with COVID-19.
Policy efforts to address hospital nurse understaffing
In 1999, California (CA) passed, and in 2004, implemented, the first and still only comprehensive US state legislation to limit the number of patients that hospital nurses are permitted to care for at one time. In the USA, it has been 20 years since any other state than CA has passed comprehensive legislation setting hospital nurse staffing requirements, although multiple states have or are considering such legislation. In 2018, a public ballot issue to improve nurse staffing in Massachusetts hospitals failed largely because of absence of credible local evidence that legislation was in the public’s interest and would not create unintended adverse consequences disrupting access to care.23–26 Currently under consideration in both NY and IL are hospital nurse staffing bills generally patterned after the CA policy and similar to what was proposed in Massachusetts. However, as in Massachusetts, there is no local evidence to date of whether such legislation is needed. This study provides that evidence while also serving as a baseline to evaluate the impact of these policies if enacted.
Public health impacts of chronic hospital nurse understaffing: the COVID-19 context
The COVID-19 pandemic provided a highly visible public health example of the importance of having adequately resourced health systems to deliver high-quality patient care, as well as the toll under-resourced care settings take on clinician well-being.27–29 In this study, we present evidence of hospital nurse staffing, nurse burnout and quality of care in NY and IL hospitals in the weeks preceding the pandemic. This information is useful for providing context for how today’s hospital nurse staffing policy choices impact hospital outcomes now and in the future. The only study to date which has examined the public health implications of nurse understaffing for patients with COVID-19 found that countries with higher workforce concentrations of RNs had lower COVID mortality rates, which suggests that a robust nursing workforce is essential for addressing the current and future outbreaks.30
New York City (NYC) and Chicago are major gateway cities with large international airports that contribute to social diversity and economic growth but may pose public health vulnerability to pandemics. One study documenting the toll of COVID-19 on the mental health of NYC healthcare workers found that 57% of workers screened positive for acute stress and 48% for depressive symptoms, with the worst psychological symptoms observed among nurses.27 There has been renewed appreciation of the risks posed to clinician well-being and retention in clinical care as well as to patient safety due to overwork, physical and emotional exhaustion and lack of supportive work environments as detailed by a major initiative of the National Academy of Medicine.7 14 31 32 In this study, we examine the link between hospital nurse staffing and adverse nurse and quality outcomes to inform decisions about the need for hospital nurse staffing regulation in NY and IL; and discuss the implications of chronic understaffing of hospital nurses in consideration of the ongoing COVID-19 pandemic.
Methods
Study design and setting
Survey data were collected between 16 December 2019 and 24 February 2020 from direct-care RNs in NY and IL hospitals to estimate nurse staffing and its associations with nurse-reported outcomes. Staffing data were linked to patient data from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) and American Hospital Association (AHA) Annual Survey. HCAHPS data provided information on patient satisfaction, an outcome evaluated in this study. AHA provided data on hospital characteristics which were used for risk adjustment.
Emailed surveys were sent by the National Council of State Boards of Nursing to all actively licensed RNs in NY and IL. Non-respondents received follow-up reminders at regular intervals. Responses were anonymised. The survey took 10–15 min to complete.
Nurses working in hospitals provided their hospital’s name, which enabled the aggregation of individual nurse responses to create hospital-level measures of staffing and quality measures. Using front-line RNs as informants of hospital staffing has been previously validated and produces unbiased and representative estimates.33 Nurses were also queried about their personal characteristics and job outcomes (ie, burnout, job dissatisfaction and intent to leave their current job), and the quality of care and patient safety in their institution (ie, infection prevention, missed nursing care, operational failures).
Sample
All non-federal acute care general hospitals were included in our sample, so long as they provided enough nurse responses to reliably estimate medical-surgical and/or intensive care unit (ICU) staffing. This resulted in two samples of hospitals and nurses. The first sample included 4298 RNs working on medical-surgical units in 254 hospitals; the second sample included 2182 RNs working on ICUs in 179 hospitals. Nurses were included in the sample if they were direct-care staff RNs on either a medical-surgical unit or an adult ICU in an acute care non-federal hospital. Nurses who were not employed in direct inpatient care of adults or who worked on other units were excluded.
Variables
Patient-to-nurse staffing
Direct-care RNs reported the number of patients and RNs on their unit during their last shift. The number of patients was divided by the number of RNs to create a ratio of patients per nurse. Nurse responses were aggregated to the hospital level by taking the mean number of patients per nurse among RNs working in the same unit types in the same hospitals. Only staffing reports from nurses working medical-surgical and ICUs were used to create measures of staffing, since nurses working in specialty units like labour-delivery, the emergency room and operating room can have highly variable staffing due to the nature of the unit.
Nurse outcomes
Burnout, job dissatisfaction and intent to leave were derived from the nurse survey. Burnout was measured using the Maslach Burnout Inventory 9-item emotional exhaustion subscale.34 Nurses who scored greater than 27—the average among healthcare workers—were classified as having high burnout.35 Job dissatisfaction was measured by dichotomising responses to the survey question ‘Overall, how satisfied are you with your job?’ to contrast nurses who were ‘very/moderately dissatisfied’ and ‘very/moderately satisfied’. Intent to leave was measured by responses to the question ‘Do you plan to be with your current employer one year from now?’.
Quality of care and safety
Nurses rated quality of nursing care in their unit on a 4-point scale from ‘excellent’ to ‘poor’ (ie, In general, how would you describe the quality of nursing care delivered to patients in your practice setting?). Responses of ‘fair’ or ‘poor’ were considered poor quality. Nurses were also asked to give their practice setting an overall grade on patient safety and prevention of infections, ranging from A to F. Grades of C, D or F were considered unfavourable. Nurses reported whether they would recommend their hospital to family or friends; we compared nurses reporting ‘definitely yes’ with other nurses. Nurses were asked to report which care tasks, including adequate patient surveillance, administering medications on time and administering treatments and procedures on time, were important but left undone due to a lack of time on their last shift, and whether important patient care information was lost during handoffs. These too were dichotomised. Nurses reported on operational failures in their practice setting including: how frequently their work is interrupted or delayed by insufficient staff, non-nursing tasks, missing supplies/broken equipment, missing medications, missing/late/wrong diet and electronic documentation problems. For these items, nurses who reported ‘frequently’ were contrasted with all other nurses.
Patient satisfaction
Measures of patient satisfaction were obtained from publicly available HCAHPS data. Risk-adjusted measures are reported at the hospital level as the percentage of patients who gave their hospital a favourable rating. Two global HCAHPS items are used to contrast patients who rated their hospital 8 or less on a 10-point scale and would not definitely recommend their hospital to family or friends.
Risk-adjustment variables
From AHA Annual Survey data hospitals were categorised as small (≤100 beds), medium (101–250 beds) or large (>250 beds). Teaching status was categorised based on the ratio of medical residents/fellows per bed. Non-teaching hospitals had no residents/fellows, minor had <1:4, major teaching hospitals had ≥1:4. High-technology hospitals had the capacity to perform open-heart surgery or major organ transplantation. Controls for state (IL vs NY), location (NYC vs elsewhere) and public versus private hospitals were included, as were individual nurse characteristics from the nurse survey. NYC hospitals included hospitals in the five boroughs (ie, Brooklyn, Bronx, Manhattan, Queens, Staten Island) as well as Westchester and Nassau counties.
Analysis
We report the number of hospitals and medical-surgical and ICU nurses in our samples of hospitals, overall and by state and location, and selected characteristics including staffing ratios and hospital characteristics. We show the percentages of nurses reporting unfavourable outcomes, overall and by location. χ2 statistics, t-tests and F-tests are used, as appropriate, to test the significance of the differences found across states and locations. Data are reported by state because policies related to the nurse workforce are largely the domain of state government. NYC hospitals are compared with hospitals elsewhere since NYC experienced the initial brunt of the COVID-19 epidemic. Mixed-level logistic regression models, adjusting for hospital and nurse characteristics, are used to test associations between nurse staffing and outcomes, and to assess for differences across hospitals in NYC and elsewhere. Finally, we analyse HCAHPS patient data using ordinary least squares models to determine whether nurse reports of quality, at least generally, are corroborated by patient reports.
Results
Table 1 shows the numbers of nurses and hospitals from which staffing could be estimated. These estimates were provided by an average of 16.9 medical-surgical nurses and 12.2 ICU nurses per hospital. The average patient-to-nurse ratio was significantly higher (worse) for medical-surgical nurses in NY than in IL (5.9 vs 5.2), especially for hospitals in NYC (6.5 vs 5.4); the average patient-to-nurse ratio for ICU nurses was also significantly higher for hospitals in NYC (2.4 vs 2.2). Medical-surgical patient-to-nurse staffing ranged considerably across hospitals (3.3 to 9.7) and across NYC hospitals (4.0 to 8.8); variation was also observed for ICUs (1.5 to 4.0 overall; 1.6 to 4.0 in NYC).
Table 1.
Number of hospitals with medical-surgical units and with intensive care units, numbers of nurses on them, and staffing and other hospital characteristics, by hospital location
| Medical-surgical | Intensive care | |||||||||||||
| Characteristics of hospital sample | NY | IL | NYC | Non-NYC | Total | NY | IL | NYC | Non-NYC | Total | ||||
| Counts | ||||||||||||||
| Hospitals | 135 | 119 | 47 | 207 | 254 | 99 | 80 | 37 | 142 | 179 | ||||
| Nurses | 2820 | 1478 | 877 | 3421 | 4298 | 1345 | 837 | 439 | 1743 | 2182 | ||||
| Nurses per hospital | 20.9 | 12.4 | 18.7 | 16.5 | 16.9 | 13.5 | 10.3 | 11.9 | 12.1 | 12.2 | ||||
| Staffing—patients per nurse | ||||||||||||||
| Mean | 5.9 | 5.2 | *** | 6.5 | 5.4 | *** | 2.3 | 2.2 | NS | 2.4 | 2.2 | ** | ||
| Minimum | 3.4 | 3.3 | 4.0 | 3.3 | 1.5 | 1.6 | 1.6 | 1.5 | ||||||
| Maximum | 8.8 | 9.7 | 8.8 | 9.7 | 4.0 | 3.6 | 4.0 | 3.6 | ||||||
| Hospital characteristics (%) | ||||||||||||||
| Size (number of beds) | ||||||||||||||
| Small (≤100) | 18.5 | 24.4 | NS | 2.1 | 25.6 | *** | 54 | 9.0 | 8.6 | NS | 0.0 | 11.1 | *** | 16 |
| Medium (101–250) | 30.4 | 36.1 | 23.4 | 35.3 | 84 | 27.0 | 37.0 | 13.5 | 36.1 | 57 | ||||
| Large (>250) | 51.1 | 39.5 | 74.5 | 39.1 | 116 | 64.0 | 54.3 | 86.5 | 52.8 | 108 | ||||
| Teaching status | ||||||||||||||
| Non-teaching | 32.5 | 58.2 | *** | 19.2 | 50.8 | *** | 105 | 26.6 | 55.4 | *** | 16.2 | 45.8 | *** | 66 |
| Minor teaching | 38.1 | 28.2 | 23.4 | 36.0 | 79 | 39.4 | 25.7 | 21.6 | 36.6 | 56 | ||||
| Major teaching | 29.4 | 13.6 | 57.5 | 13.2 | 52 | 34.0 | 18.9 | 62.2 | 17.6 | 46 | ||||
| High technology status | 29.6 | 54.7 | *** | 33.3 | 43.5 | NS | 84 | 40.0 | 71.6 | *** | 43.8 | 56.3 | NS | 80 |
Source: Nurse survey data.
Non-NYC hospitals refer to hospitals in the sample outside of the five NYC boroughs and Westchester and Nassau counties. NS refers to differences which are insignificant at the 0.05 level.
** and *** denote differences in hospital characteristics which are significant with p<0.01 and p<0.001, respectively, using F-statistics (for staffing) and χ2 tests for size, teaching status and technology.
IL, Illinois; NS, not significant; NY, New York; NYC, New York City.
Figure 1 shows the variation in staffing among medical-surgical units across the 254 study hospitals. Each bar represents a hospital, with NYC hospitals denoted in blue. There is substantial variation in nurse staffing across all hospitals and NYC hospitals. While the average number of patients per nurse in some NYC hospitals was below the mean (5.6 patients per nurse), nurses in most NYC hospitals carried patient loads well above the mean.
Figure 1.
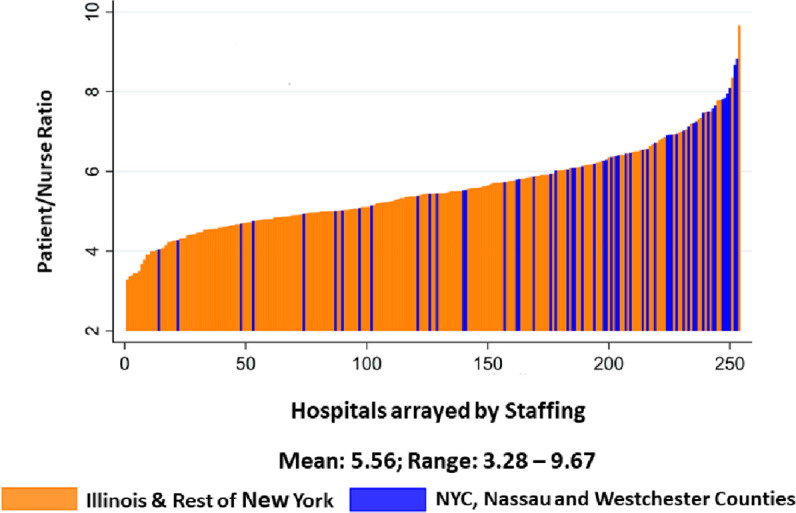
Hospital variation in medical-surgical staffing. NYC, New York City. Source: Nurse survey data.
Table 2 shows the percentages of unfavourable ratings by nurses on both medical-surgical units and ICUs. Close to half of nurses exhibit high burnout. Nearly half give their hospitals unfavourable grades on patient safety, a third give unfavourable grades on infection prevention and almost 70% would not definitely recommend their hospitals. The majority of nurses report their work was frequently interrupted or delayed by insufficient staff and a third of nurses report interruptions or delays from missing supplies including medications and missing/broken equipment. The bottom rows of table 2 show the percentage of patients who rated their hospital 8 or less on a 10-point scale and who would not definitely recommend it. As with nurses, substantial percentages of patients report unfavourably, and differences in both patient outcomes and a sizeable number of the differences between nurse outcomes in NYC hospitals and elsewhere are significant.
Table 2.
Percentages of medical-surgical and intensive care nurses reporting unfavourable outcomes for themselves and their patients, by location
| Percentage of nurses reporting: | Medical-surgical | Intensive care | ||||||
| NYC | Non-NYC | Total | NYC | Non-NYC | Total | |||
| High burnout | 52.9 | 53.1 | NS | 53.1 | 49.4 | 46.1 | NS | 46.9 |
| Job dissatisfaction | 32.2 | 31.1 | NS | 31.4 | 31.8 | 27.5 | * | 28.6 |
| Intent to leave their job | 21.5 | 21.9 | NS | 21.8 | 21.7 | 24.6 | NS | 23.8 |
| Poor/fair quality of care | 29.2 | 21.8 | *** | 23.6 | 24.2 | 17.4 | ** | 19.1 |
| Unfavourable patient safety grade | 53.8 | 47.7 | *** | 49.1 | 51.6 | 45.0 | * | 46.7 |
| Unfavourable infection prevention grade | 34.0 | 31.4 | NS | 32.0 | 40.4 | 32.4 | ** | 34.4 |
| Not definitely recommend hospital | 76.1 | 68.4 | *** | 70.3 | 74.2 | 67.8 | ** | 69.4 |
| Missed patient surveillance | 44.8 | 42.2 | NS | 42.8 | 32.8 | 30.4 | NS | 31.0 |
| Missed administering medications on time | 39.0 | 41.1 | NS | 40.6 | 33.0 | 31.4 | NS | 31.8 |
| Missed treatments and procedures | 29.2 | 25.0 | * | 26.0 | 23.0 | 20.8 | NS | 21.4 |
| Important patient care information lost during handoffs | 36.6 | 38.6 | NS | 38.2 | 33.8 | 35.6 | NS | 35.2 |
| Work frequently interrupted/delayed by: | ||||||||
| Insufficient staff | 71.8 | 63.2 | *** | 65.3 | 64.5 | 55.0 | *** | 57.4 |
| Non-nursing tasks | 48.9 | 45.9 | NS | 46.6 | 55.2 | 53.2 | NS | 53.7 |
| Missing supplies/broken equipment | 43.7 | 37.9 | *** | 39.3 | 48.1 | 38.6 | *** | 40.9 |
| Missing medications | 43.3 | 37.2 | *** | 38.6 | 44.4 | 37.8 | * | 39.4 |
| Missing, late or wrong diet | 26.3 | 20.9 | *** | 22.2 | 28.5 | 21.1 | ** | 23.0 |
| Electronic documentation system problems | 14.9 | 12.8 | NS | 13.3 | 22.7 | 14.4 | *** | 16.4 |
| Percentage of patients reporting: | ||||||||
| Ratings of their hospital 8 or less (on a 10-point scale) | 39.4 | 31.3 | *** | 33.0 | ||||
| They would not definitely recommend their hospital | 37.5 | 32.2 | *** | 33.3 | ||||
Source: Nurse survey data.
Non-NYC hospitals refer to hospitals in the sample outside of the five NYC boroughs and Westchester and Nassau counties. NS refers to differences which are insignificant at the 0.05 level.
*, **, *** denote differences in reports between locations which are significant with p <0.05, p <0.01 and p <0.001, respectively, using χ2 tests.
NS, not significant; NYC, New York City.
For nurse reports, the first column of the left and right panels of table 3 shows the unadjusted associations of medical-surgical and ICU staffing with the nurse and patient outcomes. The second column in each panel shows the associations between staffing and outcomes after adjusting for location and other characteristics, while the third column shows the association between location (NYC vs elsewhere) and outcomes after adjusting for staffing and other characteristics. The effect of medical-surgical and ICU staffing is sizeable (ORs range from 1.12 to 1.60 and 1.10 to 3.63, respectively) and significant on every outcome, before and after adjustment, except the adjusted effect of ICU staffing on missed treatments and procedures. There are virtually no significant differences by location after adjusting for staffing, despite the unadjusted differences shown in table 2. We tested for interactions, or differences in the effect of staffing by state and location but found none. Thus, the effect of staffing is of similar importance to outcomes in all hospitals, and partly accounts for differences we find in NYC hospitals. The bottom panel shows that after adjustments for nurse staffing and other hospital characteristics the differences in patient reports across locations are virtually nil. Here too, as with nurses, the medical-surgical staffing effect was similar across all hospitals (ie, no interactions were found), and workloads that were greater by a single patient per nurse had roughly 3% more patients rating their hospitals 8 or lower and who were unwilling to definitely recommend it.
Table 3.
Unadjusted and adjusted ORs estimating the effects of staffing and location on medical-surgical and intensive care nurses reporting unfavourable outcomes
| Odds on nurses reporting: | Unadjusted and adjusted ORs (for nurses) and differences (for patients) related to the association between the outcome and: | |||||
| Medical-surgical staffing | Intensive care staffing | |||||
| Unadjusted hospital staffing | Adjusted effects | Unadjusted hospital staffing | Adjusted effects | |||
| Hospital staffing | NYC | Hospital staffing |
NYC | |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| High burnout | 1.13** (1.03 to 1.24) |
1.17** (1.05 to 1.30) |
0.80 (0.64 to 1.02) |
1.49* (1.10 to 2.03) |
1.62** (1.14 to 2.30) |
0.92 (0.69 to 1.23) |
| Job dissatisfaction | 1.29*** (1.17 to 1.42) |
1.32** (1.19 to 1.47) |
0.81 (0.64 to 1.02) |
1.91*** (1.39 to 2.63) |
2.07** (1.45 to 2.97) |
0.94 (0.63 to 1.40) |
| Intent to leave their job | 1.16** (1.05 to 1.29) |
1.23** (1.11 to 1.37) |
0.83 (0.63 to 1.11) |
1.51** (1.11 to 2.04) |
1.72** (1.21 to 2.43) |
0.79 (0.58 to 1.08) |
| Poor/fair quality of care | 1.53*** (1.39 to 1.69) |
1.50** (1.32 to 1.70) |
0.91 (0.65 to 1.27) |
3.07*** (2.15 to 4.39) |
3.08** (2.00 to 4.75) |
1.26 (0.83 to 1.92) |
| Unfavourable patient safety grade | 1.44*** (1.26 to 1.65) |
1.44** (1.22 to 1.69) |
0.77 (0.55 to 1.09) |
2.38*** (1.59 to 3.58) |
3.04** (1.88 to 4.94) |
0.85 (0.57 to 1.29) |
| Unfavourable infection prevention grade | 1.25*** (1.12 to 1.39) |
1.28** (1.11 to 1.48) |
0.76 (0.54 to 1.07) |
1.76** (1.18 to 2.64) |
2.19** (1.44 to 3.34) |
1.06 (0.69 to 1.62) |
| Not definitely recommend hospital | 1.60*** (1.37 to 1.87) |
1.52** (1.27 to 1.83) |
0.97 (0.68 to 1.39) |
2.99** (1.55 to 5.75) |
3.63** (1.85 to 7.12) |
0.90 (0.53 to 1.52) |
| Missed patient surveillance | 1.21*** (1.10 to 1.32) |
1.24** (1.10 to 1.40) |
0.80 (0.63 to 1.02) |
1.68** (1.24 to 2.28) |
2.21** (1.56 to 3.13) |
0.83 (0.63 to 1.09) |
| Missed administering medications on time | 1.13* (1.03 to 1.23) |
1.23** (1.11 to 1.36) |
0.94 (0.73 to 1.20) |
1.97*** (1.42 to 2.74) |
1.98** (1.37 to 2.87) |
1.13 (0.78 to 1.64) |
| Missed treatments and procedures | 1.19*** (1.08 to 1.31) |
1.20** (1.08,1.33) |
0.99 (0.79 to 1.25) |
1.10 (0.76 to 1.60) |
1.32 (0.92 to 1.90) |
0.95 (0.69 to 1.29) |
| Important patient care information is lost during handoffs | 1.12** (1.03 to 1.21) |
1.15** (1.03 to 1.28) |
0.73* (0.58 to 0.93) |
1.28 (0.94 to 1.75) |
1.51* (1.04 to 2.18) |
0.70 (0.46 to 1.05) |
| Percentages of patients reporting: | ||||||
| Ratings of their hospital 8 or less (on a 10-point scale) | 4.5*** (3.59 to 5.49) |
2.7*** (1.69 to 3.72) |
1.1 (−2.04 to 4.14) |
|||
| They would not definitely recommend their hospital | 4.3*** (3.25 to 5.37) |
2.9*** (1.72 to 4.05) |
0.08 (−3.47 to 3.62) |
|||
Source: Nurse survey data.
ORs for nurse reports are from multilevel logistic regression models. Adjusted models for nurses include controls for individual nurse staffing (or differences in workloads across nurses within hospitals) as well as nurse characteristics (gender, years of experience and full-time status) and hospital characteristics (including size, teaching status, technology and separate dummy variables for public hospitals and Illinois hospitals). Percentage differences for patient reports are additive coefficients from ordinary least squares models, since the data from Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) are reported, risk adjusted, at the hospital level. Adjusted models for patients include controls for hospital size, teaching status, technology and separate dummy variables for public hospitals and Illinois hospitals.
*, **, *** denote differences in reports between locations which are significant with p <0.05, p <0.01 and p <0.001, respectively, using χ2 tests.
NYC, New York City.
Discussion
In the weeks before the surge of patients with COVID-19, hospital nurses in NY and IL were already struggling with high patient workloads and frequent operational failures including missing supplies and missing or broken equipment. Patient-to-nurse ratios ranged considerably across hospitals in both states from means of 3.3 to 9.7 on adult medical-surgical units. Half of nurses were experiencing high burnout, and one in four planned to leave their job within a year. Over two-thirds of nurses would not recommend their hospitals to family and friends needing care, and almost half reported unfavourable patient safety ratings. Patients corroborated nurses’ assessments with over a third of patients rating their hospitals less than excellent and reporting they would not definitely recommend it. Unfavourable patient and nurse outcomes are strongly associated with poorer nurse staffing.
Pending nurse staffing legislation in both NY and IL, which continue to be actively considered despite societal and economic disruptions caused by COVID-19,18 19 stipulates that nurses take care of not more than four adult medical or surgical patients at a time outside of intensive care. The data presented in figure 1 demonstrate that the vast majority of NY and IL hospitals currently staff worse than the level proposed in pending legislation. In CA, the only state with implemented staffing legislation, nurses are not allowed to care for more than five adult medical or surgical patients at a time.36 The majority of NY and IL hospitals are currently understaffed relative to the benchmarks in pending legislation in their own states and the benchmark passed 20 years ago in CA. Similar variation in staffing and widespread understaffing were observed in ICU units across hospitals in NY and IL. Although CA had somewhat better staffing before implementing its nurse staffing policy, nurse staffing levels have experienced greater sustained improvement in CA compared with both NY and IL, as well as other states.37 Our findings demonstrate wide variation in staffing within NY and IL, as well as significant understaffing relative to currently proposed legislation.18 19 AHA Annual Survey data derived from reports by hospital administrators confirm worse staffing in these two states relative to many other states, including CA where minimum nurse staffing has been legislated.37
There are several reasons why hospital nurse staffing legislation efforts often fail to garner widespread support among key stakeholders. The first barrier, which our paper directly addresses, is the lack of local and timely evidence to demonstrate a need for such legislation. Using recent data in two states currently considering staffing legislation we describe the variation in hospital nurse staffing and the associated consequences in terms of nurse burnout and patient care quality and safety.
The second major barrier is the common misconception about a US shortage of nurses, which would make the proposed legislation difficult to implement. However, the USA has more than doubled graduations of RNs over the past 15 years and the number of new RNs entering the workforce is at an all-time high of over 150 000 a year, more than enough to replace annual retirements.38 39 Moreover, CA, which successfully implemented minimum safe nurse staffing requirements, has fewer RNs (11.3 per 1000 population) than most other states and far fewer than NY (18.7 per 1000 population) or IL (16.7 per 1000 population).40 Differences in hospital nurse staffing by state have little to do with the supply of nurses.
During the COVID-19 emergency, some states approved temporary provisions to permit nurses licensed in one state to practise in another.41 This enabled greater mobility of nurses to work across state lines and in regions with high care needs. There is already an existing policy solution to local and short-term nurse shortages that might arise from implementing new nurse staffing legislation and during epidemics or other mass casualty situations—the Nurse Licensure Compact. Passed in 34 states but not in NY or IL or Massachusetts,42 the Compact enables nurses licensed in any Compact state to practise in any other via multistate nurse licensure. Adoption of the Nurse Licensure Compact by the remaining states could alleviate local or short-term nursing shortages.
The third major barrier to enacting nurse staffing legislation is the potential additional costs hospitals would undertake in order to comply with regulations. While an evaluation of the costs associated with implementing the proposed policies was outside the scope of this analysis, previous research demonstrates a favourable business case for hospital investments in nurse staffing, including cost savings through shorter lengths of stay and avoided readmissions.13 43–46 After implementing their nurse staffing policy, CA hospitals saw sustained improvement in staffing including in safety-net hospitals which often operate on razor-thin financial margins.47 48 Moreover, there has been no evidence of hospital closures in CA as a result of the staffing legislation.
Limitations
We lack objective clinical data on patient outcomes in 2020 due to reporting lags but other studies we cite here have demonstrated relationships with nurse reports of quality and objective outcomes such as mortality.49 We lack information on physician staffing and burnout. Given their shared work environments and patients, our findings are likely a good proxy for what doctors are also experiencing with their high rates of burnout reported by the National Academy of Medicine.50 Though the findings do not establish causal links between nurse staffing and outcomes, other studies have found similar relationships using longitudinal and cross-sectional analyses.15 16 51 52 While data in this analysis are from two states, other recent studies using 2016 data in four states (ie, CA, Florida, New Jersey, Pennsylvania) and a similar study in Queensland, Australia53 show similar findings of widespread hospital nurse understaffing associated with adverse consequences for patients and nurses.21 54
Conclusion
We do not yet know how variation in hospital nurse staffing has impacted patient deaths during this unprecedented crisis. We do know from our data that the needed nursing care surge required to treat patients with COVID-19 is being created from a deficit status quo in which the nurse workforce was already emotionally depleted prior to the surge in patients with COVID-19. While differences in state-wide average hospital nurse staffing levels between NY and IL exist, our findings are consistent with what much of past research has shown, namely that chronic nurse understaffing has persisted in a significant share of US hospitals for decades, and poses significant risk to patients even without the presence of a pandemic.1 7 8 15 16
The COVID-19 pandemic has highlighted shortcomings in US healthcare. Our findings point specifically to the risks posed to the public’s health of wide variation in hospital nurse staffing if allowed to persist. Pending legislation in NY, IL and other states and international jurisdictions can be better informed by the availability of current local empirical data on existing variation in hospital staffing and its consequences for the public.
Acknowledgments
The authors wish to acknowledge Tim Cheney for his contributions to data management and analysis.
Footnotes
Twitter: @k_lasater, @LindaAiken_Penn, @rachel_e_french
Funding: National Council of State Boards of Nursing; National Institute of Nursing Research (grant number: R01NR014855); Leonard Davis Institute of Health Economics.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. US Nurse survey data: These data were collected under the NCSBN grant (KBL, principal investigator) for purposes of improving nurse and patient outcomes and were granted a certificate of confidentiality through the National Institutes of Health/Department of Health and Human Services as per section 301(d) of the Public Health Service Act 42 USC 241(d).
Ethics statements
Patient consent for publication
Not required.
References
- 1. Aiken LH, Sloane DM, Bruyneel L, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet 2014;383:1824–30. 10.1016/S0140-6736(13)62631-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Needleman J, Buerhaus P, Pankratz VS, et al. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011;364:1037–45. 10.1056/NEJMsa1001025 [DOI] [PubMed] [Google Scholar]
- 3. Blegen MA, Goode CJ, Spetz J, et al. Nurse staffing effects on patient outcomes: safety-net and non-safety-net hospitals. Med Care 2011;49:406–14. 10.1097/MLR.0b013e318202e129 [DOI] [PubMed] [Google Scholar]
- 4. Cho E, Sloane DM, Kim E-Y, et al. Effects of nurse staffing, work environments, and education on patient mortality: an observational study. Int J Nurs Stud 2015;52:535–42. 10.1016/j.ijnurstu.2014.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Griffiths P, Ball J, Drennan J, et al. Nurse staffing and patient outcomes: strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for health and care excellence safe staffing Guideline development. Int J Nurs Stud 2016;63:213–25. 10.1016/j.ijnurstu.2016.03.012 [DOI] [PubMed] [Google Scholar]
- 6. Shekelle PG. Nurse-patient ratios as a patient safety strategy: a systematic review. Ann Intern Med 2013;158:404–9. 10.7326/0003-4819-158-5-201303051-00007 [DOI] [PubMed] [Google Scholar]
- 7. Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA 2002;288:1987–93. 10.1001/jama.288.16.1987 [DOI] [PubMed] [Google Scholar]
- 8. Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and the quality of care in hospitals. N Engl J Med 2002;346:1715–22. 10.1056/NEJMsa012247 [DOI] [PubMed] [Google Scholar]
- 9. Mchugh MD, Shang J, Sloane DM, et al. Risk factors for hospital-acquired ‘poor glycemic control’: a case–control study. Int J Qual Health C 2011;23:44–51. 10.1093/intqhc/mzq067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aiken LH, Sermeus W, Van den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012;344:e1717. 10.1136/bmj.e1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jha AK, Orav EJ, Zheng J, et al. Patients' perception of hospital care in the United States. N Engl J Med 2008;359:1921–31. 10.1056/NEJMsa0804116 [DOI] [PubMed] [Google Scholar]
- 12. Lasater KB, Mchugh MD. Nurse staffing and the work environment linked to readmissions among older adults following elective total hip and knee replacement. Int J Qual Health Care 2016;28:253–8. 10.1093/intqhc/mzw007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Silber JH, Rosenbaum PR, McHugh MD, et al. Comparison of the value of nursing work environments in hospitals across different levels of patient risk. JAMA Surg 2016;151:527–36. 10.1001/jamasurg.2015.4908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cimiotti JP, Aiken LH, Sloane DM, et al. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control 2012;40:486–90. 10.1016/j.ajic.2012.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aiken LH, Cimiotti JP, Sloane DM, et al. Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Med Care 2011;49:1047–53. 10.1097/MLR.0b013e3182330b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sloane DM, Smith HL, McHugh MD, et al. Effect of changes in hospital nursing resources on improvements in patient safety and quality of care: a panel study. Med Care 2018;56:1001–8. 10.1097/MLR.0000000000001002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aiken LH, Sloane DM, Bruyneel L, et al. Nurses' reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud 2013;50:143–53. 10.1016/j.ijnurstu.2012.11.009 [DOI] [PubMed] [Google Scholar]
- 18. Illinois General Assembly . HB 2604 - Safe Patient Limits Act. Available: https://www.billtrack50.com/BillDetail/1068160
- 19. New York Senate and Assembly . S.1032/ A.2954 – safe staffing for quality care act. 2019-2020 legislative session. Available: https://www.nysenate.gov/legislation/bills/2019/a2954
- 20. Schaff E. Why Surviving Covid Might Come Down to Which NYC Hospital Admits You. The New York Times. Available: https://www.nytimes.com/2020/07/01/nyregion/Coronavirus-hospitals.html?campaign_id=9&emc=edit_nn_20200702&instance_id=19941&nl=the-morning®i_id=87729169&segment_id=32426&te=1&user_id=b5f25259c7d6d9fe6756bcddfa0e77ee [Accessed 1 Jul 2020].
- 21. Aiken LH, Sloane DM, Barnes H, et al. Nurses’ and patients’ appraisals show patient safety in hospitals remains a concern. Health Aff 2018;37:1744–51. 10.1377/hlthaff.2018.0711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McHugh MD, Kutney-Lee A, Cimiotti JP, et al. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff 2011;30:202–10. 10.1377/hlthaff.2010.0100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chen M. More nurses means better care—so why did this ballot measure fail? The nation, 2018. Available: https://www.thenation.com/article/archive/massachusetts-nurses-staffing-ballot/ [Accessed 15 Nov 2018].
- 24. Fotsch R. The people of Massachusetts decide the fate of Nurse-Patient staffing ratios. J Nurs Regul 2019;9:63–4. 10.1016/S2155-8256(19)30017-1 [DOI] [Google Scholar]
- 25. Kacik A. Massachusetts voters reject mandated nurse-to-patient staffing ratios. Modern healthcare, 2018. Available: https://www.modernhealthcare.com/article/20181106/NEWS/181109947/massachusetts-voters-reject-mandated-nurse-to-patient-staffing-ratios [Accessed 6 Nov 2018].
- 26. Sofer D. Massachusetts voters reject nurse staffing standards. Am J Nurs 2019;119:12. 10.1097/01.NAJ.0000553189.43320.dc [DOI] [PubMed] [Google Scholar]
- 27. Shechter A, Diaz F, Moise N, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry 2020;66:1–8. 10.1016/j.genhosppsych.2020.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ulrich CM. The moral distress of patients and families. Am J Bioeth 2020;20:68–70. 10.1080/15265161.2020.1754522 [DOI] [PubMed] [Google Scholar]
- 29. Sasangohar F, Jones SL, Masud FN, et al. Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth Analg 2020;131:106–11. 10.1213/ANE.0000000000004866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Padula WV, Davidson P. Countries with high registered nurse (RN) concentrations observe reduced mortality rates of coronavirus disease 2019 (COVID-19). available at SSRN 3566190 2020.
- 31. Garrett C. The effect of nurse staffing patterns on medical errors and nurse burnout. Aorn J 2008;87:1191–204. 10.1016/j.aorn.2008.01.022 [DOI] [PubMed] [Google Scholar]
- 32. Vahey DC, Aiken LH, Sloane DM, et al. Nurse burnout and patient satisfaction. Med Care 2004;42:II57–57. 10.1097/01.mlr.0000109126.50398.5a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lasater KB, Jarrín OF, Aiken LH, et al. A methodology for studying organizational performance. Med Care 2019;57:742–9. 10.1097/MLR.0000000000001167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav 1981;2:99–113. 10.1002/job.4030020205 [DOI] [Google Scholar]
- 35. Maslach C, Jackson SE, Leiter MP, et al. Maslach burnout inventory. Vol 21. Palo Alto, CA: Consulting Psychologists Press, 1986. [Google Scholar]
- 36. California Legislative Information . A.394 - Health facilities: nursing staff. Available: http://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=199920000AB394
- 37. McHugh MD, Kelly LA, Sloane DM, et al. Contradicting fears, California’s nurse-to-patient mandate did not reduce the skill level of the nursing workforce in hospitals. Health Aff 2011;30:1299–306. 10.1377/hlthaff.2010.1118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Auerbach DI, Buerhaus PI, Staiger DO. Registered nurse supply grows faster than projected amid surge in new entrants ages 23–26. Health Aff 2011;30:2286–92. 10.1377/hlthaff.2011.0588 [DOI] [PubMed] [Google Scholar]
- 39. National Council of State Boards of Nursing . 2018 NCLEX® examination statistics. Chicago, IL: National Council of State Boards of Nursing, 2018. https://www.ncsbn.org/2018_NCLEXExamStats.pdf [Google Scholar]
- 40. United States Census Bureau . State population Totals and components of change: 2010-2019. Suitland, MD: United States Census Bureau, 2019. https://www.census.gov/data/tables/time-series/demo/popest/2010s-state-total.html [Google Scholar]
- 41. National Council of State Boards of Nursing . State response to COVID-19. Chicago, IL: National Council of State Boards of Nursing, 2019. https://www.ncsbn.org/State_COVID-19_Response.pdf [Google Scholar]
- 42. National Council of State Boards of Nursing . Is your state moving forward with the nurse licensure compact? Chicago, IL: National Council of State Boards of Nursing, 2020. https://www.nursecompact.com/index.htm [Google Scholar]
- 43. Lasater KB, McHugh M, Rosenbaum PR, et al. Valuing Hospital investments in nursing: multistate matched-cohort study of surgical patients. BMJ Qual Saf 2021;30:46–55. 10.1136/bmjqs-2019-010534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Needleman J, Buerhaus PI, Stewart M, et al. Nurse staffing in hospitals: is there a business case for quality? Health Aff 2006;25:204–11. 10.1377/hlthaff.25.1.204 [DOI] [PubMed] [Google Scholar]
- 45. Dall TM, Chen YJ, Seifert RF, et al. The economic value of professional nursing. Med Care 2009;47:97–104. 10.1097/MLR.0b013e3181844da8 [DOI] [PubMed] [Google Scholar]
- 46. Martsolf GR, Auerbach D, Benevent R, et al. Examining the value of inpatient nurse staffing: an assessment of quality and patient care costs. Med Care 2014;52:982–8. 10.1097/MLR.0000000000000248 [DOI] [PubMed] [Google Scholar]
- 47. Harless DW, Mark BA. Nurse staffing and quality of care with direct measurement of inpatient staffing. Med Care 2010;48:659–63. 10.1097/MLR.0b013e3181dbe200 [DOI] [PubMed] [Google Scholar]
- 48. McHugh MD, Brooks Carthon M, Sloane DM, et al. Impact of nurse staffing mandates on safety-net hospitals: lessons from California. Milbank Q 2012;90:160–86. 10.1111/j.1468-0009.2011.00658.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. McHugh MD, Stimpfel AW. Nurse reported quality of care: a measure of hospital quality. Res Nurs Health 2012;35:566–75. 10.1002/nur.21503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. National Academies of Sciences, Engineering, and Medicine . Taking action against clinician burnout: a systems approach to professional well-being. Washington, DC: The National Academies Press, 2019. [PubMed] [Google Scholar]
- 51. He J, Staggs VS, Bergquist-Beringer S, et al. Nurse staffing and patient outcomes: a longitudinal study on trend and seasonality. BMC Nurs 2016;15:60. 10.1186/s12912-016-0181-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chau JPC, Lo SHS, Choi KC, et al. A longitudinal examination of the association between nurse staffing levels, the practice environment and nurse-sensitive patient outcomes in hospitals. BMC Health Serv Res 2015;15:538. 10.1186/s12913-015-1198-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. McHugh M, Aiken LH, Windsor C, et al. The case for hospital nurse-to-patient ratio legislation in Queensland, Australia hospitals: an observational study. BMJ Open. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lake ET, Riman KA, Sloane DM. Improved work environments and staffing lead to less missed nursing care: a panel study. J Nurs Manag 2020. 10.1111/jonm.12970. [Epub ahead of print: 03 Feb 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request. Data may be obtained from a third party and are not publicly available. US Nurse survey data: These data were collected under the NCSBN grant (KBL, principal investigator) for purposes of improving nurse and patient outcomes and were granted a certificate of confidentiality through the National Institutes of Health/Department of Health and Human Services as per section 301(d) of the Public Health Service Act 42 USC 241(d).


