Highlights
-
•
7.4% of the participants bore four various somatic symptoms.
-
•
Male gender was associated with anxiety comorbid somatization.
-
•
Chronic disease history was associated with anxiety comorbid somatization.
-
•
Muscle soreness and feeling weak in the body were associated with anxiety.
Keywords: somatization, somatic symptoms, anxiety, COVID-19 epidemic, infectious disease
Abstract
Background
Somatization is a common comorbidity in anxious people. From January 31 to February 2, 2020, a high prevalence of moderate to severe anxiety was detected due to COVID-19 outbreak. The purpose of this study was to investigate the prevalence and correlates of somatization among Chinese participants with anxiety receiving online crisis interventions from Feb 14 to Mar 29 during the COVID-19 epidemic.
Methods
A total of 1134 participants who participated in online crisis interventions completed the Generalized Anxiety Disorder-7 (GAD-7) scale and the Symptom Checklist-90 (SCL-90) and demographic questions online. Somatization was defined as the average score of each item ≥ 2 in SCL-90 somatization subscale. Moderate to severe anxiety was defined as a score ≥ 10 in the GAD-7 scale.
Results
Among all participants, 8.0% reported moderate to severe anxiety and 7.4% reported somatization. After March 1, the prevalence of anxiety with or without somatization did not significantly change (both p > 0.05), while the prevalence of somatization increased significantly (p < 0.01). Logistic regression analysis indicated that somatization was associated with chronic disease history (with an odds ratio of 4.80) and female gender (with an odds ratio of 0.33).
Conclusions
Our findings suggest that the history of chronic diseases is associated with somatization in individuals with anxiety, indicating some stress-related mechanisms. Chinese men in crisis intervention need more attention because they are more likely to report anxiety comorbid somatization.
1. Introduction
The 2019 coronavirus disease (COVID-19) epidemic is a global health threat and the largest outbreak of epidemic after the severe acute respiratory syndrome (SARS) outbreak. Previous research has revealed a wide range of psychological effects caused by infectious disease outbreaks (e.g. Wang et al., 2020; Bao et al., 2020; Lima et al., 2020), such as the SARS outbreak (e.g. Ko et al., 2006). At the beginning of this year, the WHO declared that the COVID-19 outbreak was a Public Health Emergency of International Concern (Sohrabi et al., 2020; Ho et al., 2020). By that time, the number of cases had exceeded the total number of SARS cases of in 2003 (World Health Organization 2003, World Health Organization 2020a). Therefore, the fear or panic of ordinary people may be more intense than those in the SARS outbreak. Earlier than the WHO declaration, on Jan 26, the National Health Commission of China released basic principles to guide emergency psychological crisis intervention for the COVID-19 epidemic. The notice referred to mental health interventions during the SARS outbreak in 2003, and stated that mental health care should cover the public in need (National Health Commission of China, 2020). Up to now, a number of psychological intervention programs have been released online in China, but only some of them are very popular. Epidemiological data on the mental health problems of the people involved in these intervention programs will help to tailor future interventions and better respond to challenges during and after the outbreak.
Understandably, in the outbreak of infectious diseases, anxiety among people spreads quickly, because anyone can be infected regardless of gender and socio-demographic status. In the general population, people may experience anxiety about falling sick or death, regardless of exposure or not. This is especially true for COVID-19, because the mode and rate of transmission are striking, and there is no definite treatment available (Ho et al., 2020). The major psychological problems during outbreaks of infectious disease include anxiety, somatic symptoms, panic attacks and depression (Ho et al., 2020). Wang et al. (2020) found that in China, 31.2% of people reported at least moderate anxiety symptoms, and 53.8% reported at least moderate psychological impact of the COVID-19 outbreak. Another large-scale national survey conducted in China collected data from January 31 to February 10, 2020. Respondents were asked to report the frequency of anxiety, specific phobias, depression, avoidance and compulsive behavior, cognitive change, physical symptoms and social functioning impairment in the past week. According to the composite index used in the survey, nearly 35% of the respondents suffered psychological distress (Qiu et al., 2020).
It is reported that a cluster of physical symptoms may be manifestations of somatization (Lipowski, 1987), including pain (Asmundson and Hadjistavropoulos, 2007; Asmundson and Katz, 2009), musculoskeletal diseases (Vassend et al., 2017), dizziness (Russo et al., 1994), fatigue (Vassend et al., 2018), and miscellaneous symptoms. An earlier study revealed that more than 80% of the general population recalled the phenomenon of a physical symptom that caused at least mild functional impairment in the last 7 days, which could not be clearly explained by well-known medical conditions (Hiller et al., 2006). In routine clinical practice, people suffering from functional physical symptoms have accounted for a large part of the workload of general practitioners, and functional symptoms and somatization are still difficult to treat (Zantinge et al., 2005). In the early stages of the COVID-19 epidemic (31 January–2 February 2020) after WHO announced international concern, a cross-sectional survey of respondents from 194 cities was conducted online in China. Among the respondents, 60.81% reported no physical symptoms; 15.04% reported one physical symptom, 9.42% reported two physical symptoms, and 5.62% reported three physical symptoms. Specific physical symptoms (e.g., dizziness, myalgia), women and poor self-assessed health status were associated with poorer mental health status and higher stress levels (Wang et al., 2020). In the general population, similar physical symptoms of COVID-19 may cause anxiety about how to stay healthy. An important reason is that although most cases of COVID-19 infection have resolved spontaneously, some cases have developed various fatal complications including severe pneumonia, organ failure, septic shock, and acute respiratory distress syndrome (Sohrabi et al., 2020). Another important reason is that around 80% of COVID-19 infected patients experienced mild illness (WHO, 2020b). Because many people with physical symptoms want to seek non-medical or medical help to ensure their health (Budtz-Lilly et al., 2015), the healthcare system can be overburdened by repeated consultations or diagnostic tests. In order to avoid possible overload and virus transmission in hospitals nationwide, the Chinese government has made great efforts to raise public awareness of cold and flu prevention by daily updated information in the media. Therefore, it is very critical to reveal the prevalence and severity of functional physical symptoms (somatization) and related factors during COVID-19.
In addition to the current COVID-19 epidemic, a challenge of relieving functional physical symptoms is the low recognition rate of psychological problems in hospitals, especially in China. Previous studies have indicated that Chinese people who expressed emotional distress in a “psychological” way tend to rely on themselves or their family members, while those who are “somatized” often seek medical help (Wang et al., 2019). The preferences of Chinese patients may reduce their chances of getting help from mental health workers when they need it. Furthermore, the clinical outcomes of patients with medically unexplained heterogeneous symptoms are suboptimal (Röhricht et al., 2019). Although the symptoms are placed in a broader context according to the biopsychosocial model, many physicians and mental health professionals still find it difficult to deal with psycho-somatic symptoms (Rosmalen et al., 2020). Therefore, there is urgent need to explore the related factors of somatization during the COVID-19 epidemic and their relationships with anxiety, especially in those who come to seek psychological help.
Earlier studies has shown a high rate of comorbidities between anxiety and somatization (Asmunson et al. , 2009; Hanel et al., 2009), while moderate to severe anxiety seems to be the most common psychological problem in China during the COVID-19 epidemic (Wang et al., 2020). As the epidemic continues, more and more Chinese psychologists and psychiatrists share strategies for dealing with psychological stress through internet platforms (e.g. WeChat, Weibo). Hospitals, counseling centers, and universities have set up many special hotlines to provide psychological service (Bao et al., 2020). How to help people cope with anxiety and somatization has become an important issue. Therefore, we need to investigate the somatization and its relationship with anxiety in Chinese people who received crisis interventions during the COVID-19 epidemic. We hypothesized that there would be significant differences in somatization between persons with and without anxiety who sought self-help emotion regulation strategies through crisis interventions.
2. Method
2.1. Measures
2.1.1. The GAD-7 scale
The scale is a self-report questionnaire indicating the severity of generalized anxiety disorder. It has an excellent internal consistency (Cronbach's α = 0.92) (Spitzer et al., 2006). Each of seven items is scored on a 4-point Likert scale (0 =“not at all,” 1 = “several days,” 2 = “more than half the days,” 3 =“almost every day,”). This measure has been widely used in China with good reliability and validity (He et al., 2010). In the current study, the Cronbach's α coefficient of the scale was 0.86. Subjects were identified as having (moderate) anxiety symptoms when they scored ≥ 10 on GAD-7.
2.1.2. The Chinese version of the symptom checklist-90 (SCL-90)
SCL-90 consists of 90 items, and measures psychological distress with 9 different subscales. The SCL-10 somatization subscale (SCL-90-SOM) summarizes the problems caused by physical dysfunction with good internal consistency (Cronbach's α = 0.86) (Derogatis et al., 1976). SCL-90-SOM has 12 items, and each item is rated on a 5-point scale (1= “not at all” to 5 = “extremely serious”). The Chinese-version of SCL-90 has excellent reliability and validity, and has been widely used in clinical practice and research in China (Tang et al., 1999). In the current study, the Cronbach's α coefficient of the subscale was 0.93. Somatization was identified when the subjects scored an average of ≥ 2 for every item.
2.2. Procedure
All subjects participated in the online crisis intervention initiated by the Institute of Psychology, Chinese Academy of Sciences. Subjects were invited through the Wechat link used in the crisis intervention to minimize face-to-face interaction. Before starting the crisis intervention, the subjects completed the questionnaires. If a person was interested in this self-help 7-day online crisis intervention, he or she could click the button to enter the intervention program. A pop-up window was designed to invite people to complete the evaluation in the Wechat mini-program. The pop-up window contained an invitation to use questionnaires for self-evaluation. The invitation criterion for this study is that the subjects must be an adult Chinese citizen. The subjects completed a set of questionnaires including demographic and socioeconomic information (age, sex, education years, marital status, and family income), health behaviors (smoking and drinking), history of chronic illness, experience related to SARS epidemic, the GAD-7 scale and SCL-90-SOM. The enrollment of subjects was in accordance with the principles in the Declaration of Helsinki. This study was approved by the Institutional Review Board of Institute of Psychology, Chinese Academy of Sciences.
The data were collected over a period of one and a half month (February 14 to March 29, 2020) when online interventions were conducted in a large number of people to help them cope with the COVID-19 outbreak. The subjects with moderate to severe anxiety symptoms (A) were defined as scoring ≥ 10 on GAD-7, and the subjects with somatization (S) were defined as having average scores ≥ 2 for each item in the SCL-90-SOM. Then we divided all subjects into four groups: subjects without either anxiety or somatization (Asymptomatic Group), subjects with moderate to severe anxiety symptoms (Group A), subjects with somatization (Group S), and subjects with both anxiety and somatization (Group A+S).
2.3. Statistical analysis
Normal distribution of each variable was examined by Shapiro-Wilk test. None of the variables was normally distributed (all p < 0.01). Descriptive statistics of the four groups (Group A, Group S, Group A+S, and Asymptomatic Group) are described. Categorical variables, such as gender, family income level, were expressed as percentages. Continuous variables, such as age and GAD-7 score, were expressed as mean ± standard deviation (M ± SD). Mann-Whitney U test or chi-square test was used to examine the differences between Group A and A+S, and between Group S and Asympmatic Group. Multiple logistic regression analysis was used to analyze features related to anxiety or/and somatization (four groups). Independent variables included sex, marital status (married vs unmarried), smoking (yes or no), drinking (yes or no), history of chronic illness (yes or no), experience of SARS epidemic (yes or no), participation in crisis intervention before March 1st (yes or no), age (<40 years or ≥ 40 years), overweight (body mass index ≥ 24 kg/m² vs < 24 kg/m²), education (≥high school or below), family income (annual income ≤8 .0000 RMB vs > 8 .0000 RMB).
A binary logistic regression analysis was conducted to test the potential somatic symptoms associated with moderate anxiety (yes/no). The independent variables were the four somatic symptoms in SCL-90, which were Faintness (yes/no), Soreness (yes/no), breath (yes/no), and Weakness (yes/no), when controlling for gender (male/female), history of chronic illness (yes or no), and experience of SARS epidemic (yes or no). Finally, multiple linear regression analysis was used to confirm correlations between GAD-7 score and the independent variables in the binary logistic regression. The significance level of p < 0.05 was applied to all tests. SPSS Statistic 21.0 was used to perform all analyses.
3. Results
3.1. Demographic characteristics of subjects
A total of 7227 participants in the crisis intervention were invited, and 1172 of them responded. We found that 38 respondents submitted unqualified questionnaires. In the end, 1,134 subjects (337 men and 797 women) from 31 provinces in China were included. Among them, 374 were from Shandong, 191 from Liaoning, 177 from Beijing, 163 from Hunan. In addition, there were 34 in Hubei, and 20 in Wuhan city. Among all provinces, these five provinces were the top five in the total number of subjects, accounting for 82.8% of the current sample. The privacy of the subjects was guaranteed.
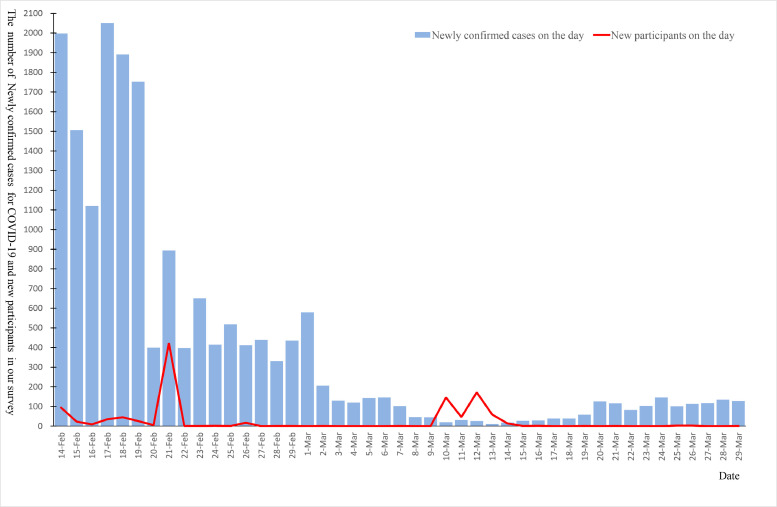
Among all subjects, 60.2% (683) participated in crisis intervention before March 1, and 39.8% (451) participated in crisis intervention after March 1 (Fig. 1 ). The average age of the subjects was 28.44 years (SD = 10.48). Among all subjects, 86.4% of the subjects had completed high-school education or above. 42.1% of the subjects had an annual family income of less than 80,000 RMB, and 0.9% had annual family income exceeding 1000,000 RMB. 26% of the subjects had a body mass index (BMI) of 24 kg/m² and above. 7% of the subjects were smokers and 18.5% consumed alcohol in their daily life. Among all subjects, 12.9% had a history of chronic diseases, and 48.1% had experienced SARS epidemic (see Table 1 ).
Fig. 1.
The number of the newly confirmed COVID-19 cases in China and new subjects of our survey during the study period.
Table 1.
Comparison of demographic characteristics between the subjects with and without somatization.
| with Anxiety | without Anxiety | |||||||
|---|---|---|---|---|---|---|---|---|
| Group A+S | Group A | Group S | AsymptomaticGroup | |||||
| n=36 | n=55 | Z or χ2 | p | n=48 | n=995 | Z or χ2 | p | |
| Female | 61.1% | 65.5% | 0.18 | 0.673 | 77.1% | 71.6% | 0.95 | 0.331 |
| Age | 30.2±11.5 | 26.9±10.5 | 3.06 | 0.080 | 31.6±10.0 | 28.3±10.5 | 0.37 | 0.544 |
| Overweight | 28.6% | 25.5% | 0.11 | 0.744 | 22.90% | 26.10% | 0.25 | 0.620 |
| Less Educated | 25.7% | 7.3% | 5.89* | 0.015 | 12.50% | 13.60% | 0.05 | 0.833 |
| Married | 47.2% | 21.8% | 6.47* | 0.011 | 54.20% | 35.20% | 7.16⁎⁎ | 0.007 |
| Lower family income | 52.8% | 49.1% | 0.12 | 0.731 | 39.60% | 41.40% | 0.06 | 0.802 |
| Smoking | 2.8% | 7.3% | 0.85 | 0.358 | 8.30% | 7.00% | 0.12 | 0.732 |
| Drinking | 19.4% | 25.5% | 0.44 | 0.506 | 25.00% | 17.80% | 1.61 | 0.205 |
| History of chronic illness | 36.1% | 10.9% | 8.37⁎⁎,Δ | 0.004 | 25.00% | 11.60% | 7.74⁎⁎,Δ | 0.005 |
| Having experienced the SARS epidemic | 41.7% | 47.3% | 0.28 | 0.599 | 68.80% | 47.30% | 8.40⁎⁎,Δ | 0.004 |
| GAD-7 | 14.2 ± 3.0 | 13.1 ± 3.2 | -1.97* | 0.048 | 5.2 ± 3.1 | 2.8 ± 2.4 | -5.12⁎⁎⁎,ΔΔ | 0.000 |
| SCL-90-SS | 2.7 ± 0.8 | 1.4 ± 0.3 | -8.05⁎⁎⁎,ΔΔ | 0.000 | 2.7 ± 1.1 | 1.2 ± 0.2 | -11.93⁎⁎⁎,ΔΔ | 0.000 |
Note:
A: anxiety; S: somatization; A+S: anxiety comorbid somatization; Z: outcome of Mann-Whittney U test; Overweight: BMI ≥24 kg/m², BMI=body mass index; 8W means 80,000; SCL-90-SS: somatization subscale of SCL-90. Less educated: lower than high school level; Lower family income: annual family income ≤ 80,000 RMB.
p < 0.05
p < 0.01
p < 0.001
Bonferroni corrected p < 0.05
Bonferroni correctedp < 0.01
3.2. Development of the COVID-19 epidemic and the prevalence of anxiety and somatization
Fig. 1 shows the daily number of the newly confirmed COVID-19 cases in China during our investigation period, from February 14 to March 29, 2020. There was a sharp decrease in the number of confirmed cases in China after 1 March 2020, with about 100 or less confirmed cases every day.
After March 1, the prevalence of either moderate to severe anxiety or anxiety comorbid somatization did not change significantly (5.6% vs 3.8%, χ 2 = 1.90, p > 0.05 for anxiety; 2.9% vs 3.5%, χ 2 = 1.90, p > 0.05 for anxiety comorbid somatization); however, the prevalence of somatization increased significantly (2.6% vs 6.7%, χ 2 = 10.81, p < 0.01).
3.3. Comparison of demographic characteristics between subjects with and without somatization
Among all subjects, 7.4% reported at least mild somatization. Table 1 provides descriptive statistics of the demographic characteristics of four groups of subjects. In the anxiety group, there were differences in education years (25.7% vs 7.3% ≤ 12 years, χ 2 = 5.89, p < 0.05; Bonferroni corrected p > 0.05), and history of chronic disease (36.1% vs 10.9%, χ 2 = 8.37, p < 0.05; Bonferroni corrected p < 0.05) between subjects with and without comorbid somatization.
In non-anxiety group, more subjects with somatization experienced SARS outbreak (68.8% vs 47.3%, χ 2 = 8.40, p < 0.005; Bonferroni corrected p < 0.05) and had a history of chronic disease (25.0% vs 11.6%, χ 2 = 7.74, p < 0.01; Bonferroni corrected p < 0.05) compared with subjects without somatization. The marriage rate in the somatization group was significantly higher than that in the non-somatization group (for those with anxiety: 47.2% vs 21.8%, χ 2 = 6.47, p < 0.05; Bonferroni corrected p > 0.05; for those without anxiety: 54.2% vs 35.2%, χ 2 = 7.74, p < 0.01; Bonferroni correctedp > 0.05).
3.4. Association of somatic symptoms and anxiety
The results of multinomial logistic regression were presented in Table 2 . Subjects who had a history of chronic disease were 4.80 times more likely to report anxiety comorbid somatization (odds ratio = 4.80, 95% CI = 2.08– 11.07, Wald χ 2 = 13.49, df = 1, p < 0.001), and were 2.402 times more likely to report somatization without anxiety (odds ratio = 2.40, 95% CI = 1.15 – 5.03, Wald χ 2 = 5.39, df = 1, p < 0.05). Compared with men, female subjects were less likely to report anxiety comorbid somatization (odds ratio = 0.33, 95% CI = 0.14 – 0.81, Wald χ 2 =5.95, df = 1, p < 0.05). In addition, subjects who had experienced the SARS outbreak tended to be more likely to report somatization without anxiety (odds ratio = 1.86, 95% CI = 0.95 – 3.66, Wald χ 2 =5.95, df = 1, p = 0.072). Notably, 3.2% of the subjects experienced dizziness or faintness (SCL-90-SOM-Faintness), 3.1% reported dyspnea (SCL-90 item-Breath), 7.8% had muscle soreness (SCL-90-SOM-Soreness), and 6.3% felt weak in certain parts of the body (SCL-90-SOM-Weak). Among all subjects, 8.0% reported moderate anxiety. Binary logistic regression analysis showed that subjects with moderate Soreness were 6.46 times more likely to have anxiety than that in those without soreness (odds ratio = 6.46, 95% CI = 3.39 – 12.30, Wald χ 2 = 32.17, df = 1, p < 0. 001), and subjects with moderate Weak were 6.46 times more likely to have anxiety compared with those without (odds ratio = 5.16, 95% CI = 2.54 – 10.50, Waldχ 2 = 20.57, df = 1, p < 0. 001) after adjusting for gender, experience of SARS outbreak, and history of physical diseases (Table 3 ). In addition, women were less likely to be anxious than men (odds ratio = 0.59, 95% CI = 0.36 – 0.96, Wald χ 2 = 32.17, df = 1, p < 0. 001). Further multiple linear regression showed that chronic disease history (beta = 0.09, t = 3.16,p < 0.01), having experienced the SARS epidemic (beta = -0.05, t = -1.98, p < 0.05), Soreness (beta = 0.17,t = 4.89, p < 0.001) and Weak (beta = 0.30,t = 7.83, p < 0.001) were still associated with the GAD-7 score.
Table 2.
Demographic correlates of somatization in anxious and nonanxious individuals
| Group A+S (n = 36) | Group A (n = 55) | Group S (n =48) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wald | df | OR | 95%CI | p | Wald | df | OR | 95%CI | p | Wald | df | OR | 95%CI | p | |
| Female | 5.95 | 1 | 0.33* | 0.14-0.81 | 0.015 | 0.04 | 1 | 1.08 | 0.55-2.12 | 0.835 | 0.05 | 1 | 0.91 | 0.389-2.124 | 0.825 |
| Age | 0.01 | 1 | 0.96 | 0.34-2.68 | 0.935 | 0.01 | 1 | 0.95 | 0.33-2.70 | 0.918 | 2.13 | 1 | 0.47 | 0.17-1.297 | 0.145 |
| Overweight | 0.56 | 1 | 0.73 | 0.33-1.65 | 0.455 | 0.00 | 1 | 1.00 | 0.52-1.94 | 0.993 | 0.98 | 1 | 0.69 | 0.331-1.437 | 0.322 |
| Less educated | 2.40 | 1 | 1.99 | 0.83-4.73 | 0.121 | 1.69 | 1 | 0.49 | 0.17-1.43 | 0.194 | 0.13 | 1 | 0.84 | 0.333-2.131 | 0.718 |
| Married | 1.23 | 1 | 1.79 | 0.64-5.02 | 0.268 | 2.13 | 1 | 0.53 | 0.22-1.25 | 0.144 | 1.00 | 1 | 1.50 | 0.678-3.319 | 0.317 |
| Lower family income | 1.88 | 1 | 1.70 | 0.80-3.62 | 0.170 | 0.91 | 1 | 1.33 | 0.74-2.38 | 0.341 | 1.17 | 1 | 1.43 | 0.746-2.758 | 0.280 |
| Smoking | 2.55 | 1 | 0.18 | 0.02-1.47 | 0.110 | 0.05 | 1 | 0.88 | 0.29-2.72 | 0.829 | 0.03 | 1 | 1.10 | 0.348-3.506 | 0.866 |
| Drinking | 0.15 | 1 | 1.19 | 0.49-2.90 | 0.703 | 2.75 | 1 | 1.76 | 0.90-3.44 | 0.097 | 0.78 | 1 | 1.39 | 0.672-2.859 | 0.377 |
| History of chronic illnessa,b | 13.49 | 1 | 4.80⁎⁎⁎ | 2.08-11.07 | 0.000 | 0.10 | 1 | 1.16 | 0.46-2.92 | 0.755 | 5.39 | 1 | 2.40* | 1.147-5.031 | 0.020 |
|
Having experienced the SARS epidemic |
1.78 | 1 | 0.59 | 0.27-1.28 | 0.183 | 0.31 | 1 | 1.18 | 0.66-2.12 | 0.580 | 3.24 | 1 | 1.86 | 0.946-3.658 | 0.072 |
|
Participating crisis intervention before Mar 1 |
0.47 | 1 | 0.70 | 0.25-1.93 | 0.491 | 0.01 | 1 | 1.03 | 0.48-2.22 | 0.938 | 1.92 | 1 | 0.55 | 0.232-1.284 | 0.166 |
Note:
A: anxiety; S: somatization; A+S: anxiety comorbid somatization;
Overweight: BMI ≥24 kg/m², BMI=body mass index; SCL-90-SS: somatization subscale of SCL-90; Less educated: lower than high school level; Lower family income: annual family income ≤ 80,000 RMB.
Reference group= the Asymptomatic subgroup (OR=1.0).
p < 0.05
p < 0.001
Group A+S significantly differs from Asympmatic Group.
Group S significantly differs from Asympmatic Group.
Table 3.
The association of the four somatic symptoms and moderate to severe anxiety
| Variable | n(%) | Anxiety | ||||
|---|---|---|---|---|---|---|
| Wald | df | OR | 95%CI | P | ||
| Sex | 4.51 | 1 | 0.59* | 0.36-0.96 | 0.034 | |
| female | 797(70.3) | |||||
| male | 337(29.7) | |||||
| History of chronic illness | 1.31 | 1 | 0.76 | 0.47-1.22 | 0.252 | |
| yes | 146(12.9) | |||||
| no | 988(87.1) | |||||
| Having experienced the SARS epidemic | 1.36 | 1 | 1.45 | 0.78-2.69 | 0.243 | |
| yes | 545(48.1) | |||||
| no | 589(51.9) | |||||
| Faintness | 0.91 | 1 | 0.59 | 0.20-1.76 | 0.341 | |
| yes | 36(3.2) | |||||
| no | 1098(96.8) | |||||
| Soreness | 32.17 | 1 | 6.46⁎⁎⁎ | 3.39-12.30 | 0.000 | |
| yes | 89(7.8) | |||||
| no | 1045(92.2) | |||||
| Breath | 0.01 | 1 | 0.95 | 0.33-2.76 | 0.922 | |
| yes | 35(3.1) | |||||
| no | 1099(96.9) | |||||
| Weak | 20.57 | 1 | 5.16⁎⁎⁎ | 2.54-10.49 | 0.000 | |
| yes | 71(6.3) | |||||
| no | 1063(93.7) | |||||
Note: *p < 0.05
p < 0.001.
4. Discussion
To our best knowledge, this is the first study to investigate the prevalence and correlates of somatization in nonclinical anxious individuals in an ongoing Chinese crisis intervention during the COVID-19 epidemic. Notably, in this online crisis intervention, when the number of newly confirmed cases suddenly increased or decreased, the number of subjects actively conducting psychological self-evaluation increased dramatically. Our findings indicated that compared with the earlier national survey (Wang et al., 2020), the prevalence of moderate to severe anxiety among Chinese people who sought self-help emotion regulation strategies from February 14 to March 29 2020 was relatively low. However, the prevalence of physical symptoms is as high as the survey before February 3. Male gender and chronic disease history were associated with anxiety comorbid somatization, while chronic disease history was associated with reports of at least mild somatization. Moderate specific somatic symptoms (Soreness andWeak) and men were associated with moderate to severe anxiety symptoms.
Overall, 7.4% of the subjects were identified as having somatization. We are particularly interested in four somatic symptoms: Faintness (“faintness, dizziness or weakness”), Soreness (“muscle soreness”), Breath (“dyspnea”) and Weak (“feeling weak in certain parts of the body”) in SCL-90. In previous surveys of the general population, Faintness and Soreness were the most common physical symptoms (Wang et al., 2020). Breath and Weak were symptoms similar to the clinical manifestations of COVID-19, which may raise anxiety or fear. All subjects who were identified as having somatization scored at least 2 (mild) on these four items. We found that 7.8% of the subjects had muscle soreness, which was similar to the prevalence in the earlier survey (7.9% for myalgia) before February 3 (Wang et al., 2020). We found that the prevalence of dizziness was 3.2%, which was lower than 7.2% in the earlier survey (Wang et al., 2020), and the prevalence of dyspnea was 3.1% which was much higher than the previous survey (0.4%) (Wang et al., 2020). These inconsistence may be attributed to the development of the COVID-19 epidemic and the different measurement methods. The current study used SCL-90 somatization subscale, while the previous survey developed a customized checklist to detect physical symptoms. Maybe more importantly, our survey was conducted after the peak period of COVID-19 in China. Although the number of newly confirmed cases decreased significantly every day during the period of our survey, the unexpected prolonged epidemic had constituted long-term stress on the general population, resulting in dramatic and long-term change in daily life and work. As a result, chronic stress may cause different psychological responses compared with the time when people first recognized the epidemic.
All four related somatic symptoms are closely related to stress or anxiety, so they may be relevant to chronic stress caused by the COVID-19 epidemic (Zhang and Ma, 2020; Wang et al., 2020; Qiu et al., 2020). First, musculoskeletal conditions, such as pain and soreness, have been shown to be associated with anxiety, but the nature of this relationship is poorly understood (Vassend et al., 2017). Stress is believed to be a physiological trigger for the descending pain regulation system, and pain can trigger an emotional response to stress (Timmers et al., 2019). Pain sensitivity may increase under chronic stress (Jenewein et al., 2016). Both chronic stress and chronic pain are associated with certain brain networks, including the corticolimbic system and thalamus, and are both associated with increased anxiety (Vachon-Presseau, 2018; Timmers et al., 2019). Second, breathlessness (trouble getting breath) is multidimensional, not only physiological, but also evokes different behaviors and feelings (Sandberg and Ekström, 2019; Parshall et al., 2012). An earlier experimental study showed that somatization-like subjects experienced more breathlessness and subjective stress than healthy controls (Rietveld and Houtveen, 2005). Previous population-based studies have shown that 9% to 13% of adult community residents have mild to moderate dyspnea (Parshall et al., 2012; Bowden et al., 2011; Currow et al., 2009). Third, it was reported that a large proportion of the genetic risk are shared between anxiety and fatigue, between pain and fatigue, and these genetic risks were independent of neuroticism (Vassend et al., 2018). Moreover, the genetic correlation between musculoskeletal pain and fatigue was particularly strong (Vassend et al., 2018). Fourth, anxiety-related dizziness is also common in the general population (Hinton et al., 2019; Lempert et al., 2009).
In our study, we found that some demographic factors were associated with somatization or anxiety. First, among subjects without anxiety, SARS's experience was associated with at least mild somatization, but it was not the case for subjects with anxiety. Among subjects who had experienced the SARS epidemic, the COVID-19 epidemic may be considered a familiar situation. As a result, they were less likely to feel anxious when coping with the life during the COVID-19 epidemic. Second, we found that the history of chronic illness was reliably related to both somatization and anxiety. This is consistent with earlier survey (Wang et al., 2020). They revealed that a history of chronic illness was associated with higher anxiety scores. Anxiety manifests as psychological and physiological activity, which may eventually lead to greater health risks (Renna et al., 2018). Various chronic diseases are closely correlated with stress and anxiety (Bernstein, 2016; Renna et al., 2018). On the other hand, anxiety sensitivity to subjects with chronic diseases may increase their anxiety (Norman and Lang, 2005). Third, an unexpected finding was that male gender was associated with moderate anxiety and comorbid somatization. This is inconsistent with earlier survey, which showed that women experienced higher levels of anxiety than men in the general population between January 31 and February 2 (Wang et al., 2020). To some extent, this may be due to the differences in the subjects. In the current study, the subjects were those who sought self-help emotion regulation strategies in online self-help crisis intervention. Online self-help interventions may have met the need of a large percentage of male subjects who were uncomfortable with initiating a counseling call or asking for help face to face. Especially in China, men tend to suppress their feelings of distress. Finally, subjects with a lower education level below high school accounted for a higher proportion of Group A+S than in the Group A, although this was only a marginal significance. Most our subjects had an education level above high school. In the future, it is necessary to discuss how to cover a wider range of subjects in online crisis interventions.
Our study has several limitations. First, this was a cross sectional study. The sample we collected in this study were those who sought self-help emotion regulation strategies during the COVID-19 epidemic, rather than the general population. In this way, the collected sample was really not representative of Chinese population. Second, given the spread of our online crisis interventions and the development of the COVID-19 epidemic, our data covered much longer period than previous similar surveys. Third, after completing self-service online interventions, a prospective study should be conducted on the same group of subjects. Due to the lack of face to face interaction, prospective study may not be smooth. Fourth, self-reported levels of physical symptoms and anxiety may not always be consistent with the assessment by mental health professionals. More importantly, self-reported physical symptoms should be treated with caution, and both psychological intervention and physical examination should be recommended after the first evaluation.
5. Conclusions
Compared with the earlier survey before February 3, the incidence of moderate to severe anxiety was lower in the general population during an ongoing online crisis intervention to response to COVID-19 outbreak from February 14 to March 29. However, self-reported physical symptoms still seem to be as frequent as earlier surveys. A chronic disease history is reliably associated with somatization or anxiety, which may indicated stress-related mechanisms. Male subjects were more likely to report anxiety comorbid somatization. Our findings have important implications for crisis intervention during the COVID-19 epidemic. First, in this public health emergency, the focus of crisis intervention should be tailored to the development of the epidemic and the psychological response of the public. During this long-term epidemic, how to deal with chronic stress should be a crucial part, as people were also experiencing lock-downs and social restrictions, which in turn might bring anxiety symptoms to people. The concept of psychosomatic medicine should be emphasized, especially for those common somatic symptoms. Second, Chinese culture may have a special impact on emotional regulation and somatization, which should be paid attention to in crisis intervention. In order to develop cultural adaption interventions, traditional Chinese medicine may provide theoretical and technical support. Third, the evaluation on health beliefs and behavioral habits will help improve crisis intervention. Health education embedded in crisis interventions may have increased public awareness of the long-term impacts of health behaviors, thus effectively preventing chronic diseases. Finally, male adults should receive more attention than before, especially for the Chinese population.
Role of the funding source
None
CRediT authorship contribution statement
Fangfang Shangguan: Conceptualization, Formal analysis, Methodology, Writing - original draft, Writing - review & editing. Xiao Quan: Data curation, Formal analysis, Writing - original draft. Wei Qian: Data curation. Chenhao Zhou: Data curation, Writing - original draft. Chen Zhang: Writing - original draft. Xiang Yang Zhang: Conceptualization, Methodology, Investigation, Writing - review & editing. Zhengkui Liu: Conceptualization, Methodology, Project administration, Investigation.
Declaration of Competing Interest
All the authors declare that they have no conflicts of interest.
Acknowledgments
We thank Dr. Yongjie Zhou for her outstanding work in helping with data collection and cleaning. We are also grateful to all the other colleagues who contributed to data collection.
References
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein C.N. Psychological stress and depression: risk factors for ibd? Dig. Dis. 2016;34(1-2):58–63. doi: 10.1159/000442929. [DOI] [PubMed] [Google Scholar]
- Bowden J.A., To T.H., Abernethy A.P., Currow D.C. Predictors of chronic breathlessness: a large population study. BMC Public Health. 2011;11:33. doi: 10.1186/1471-2458-11-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currow D.C., Plummer J.L., Crockett A., Abernethy A.P. A community population survey of prevalence and severity of dyspnea in adults. J. Pain Symptom Manag. 2009;38(4):533–545. doi: 10.1016/j.jpainsymman.2009.01.006. [DOI] [PubMed] [Google Scholar]
- Derogatis L.R., Rickels K., Rock A.F. The SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br. J. Psychiatry. 1976;128:280–289. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- Hanel G., Henningsen P., Herzog W., Sauer N., Schaefert R., Szecsenyi J., Löwe B. Depression, anxiety, and somatoform disorders: vague or distinct categories in primary care? Results from a large cross-sectional study. J. Psychosom. Res. 2009;67(3):189–197. doi: 10.1016/j.jpsychores.2009.04.013. [DOI] [PubMed] [Google Scholar]
- He X., Li C., Qian J., Cui H., Reliability W.W. Validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch. Psychiatry. 2010;22(4):200–203. [in Chinese] [Google Scholar]
- Hiller W., Rief W., Brähler E. Somatization in the population: from mild bodily mis- perceptions to disabling symptoms. Soc. Psychiatry Psychiatr. Epidemiol. 2006;41(9):704–712. doi: 10.1007/s00127-006-0082-y. [DOI] [PubMed] [Google Scholar]
- Hinton D.E., Seponski D.M., Khann S., Armes S.E., Lahar C.J., Kao S., Schunert T. Culturally sensitive assessment of anxious-depressive distress in the Cambodian population: avoiding category truncation. Transcul. Psychiatry. 2019;56(4):643–666. doi: 10.1177/1363461519851609. [DOI] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of covid-19 beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020;49(3):155–160. [PubMed] [Google Scholar]
- Jenewein J., Erni J., Moergeli H., Grillon C., Schumacher S., Mueller-Pfeiffer C., Hassanpour K., Seiler A., Wittmann L., Schnyder U., Hasler G. Altered pain perception and fear-learning deficits in patients with posttraumatic stress disorder. J. Pain. 2016;17(12):1325–1333. doi: 10.1016/j.jpain.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko C.H., Yen C.F., Yen J.Y., Yang M.J. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin. Neurosci. 2006;60(4):397–403. doi: 10.1111/j.1440-1819.2006.01522.x. [DOI] [PubMed] [Google Scholar]
- Lempert T., Neuhauser H., Daroff R.B. Vertigo as a symptom of migraine. Ann. N. Y. Acad. Sci. 2009;1164:242–251. doi: 10.1111/j.1749-6632.2009.03852.x. [DOI] [PubMed] [Google Scholar]
- Lima C.K.T., Carvalho P.M.M., Lima I., Nunes J., Saraiva J.S., de Souza R.I., da Silva C.G.L., Neto M.L.R. The emotional impact of coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of China. Principles for emergency psychological crisis intervention for the new coronavirus pneumonia. [in Chinese] [accessed Jan 26, 2020]. http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.shtml.
- Norman S.B., Lang A.J. The functional impact of anxiety sensitivity in the chronically physically ill. Depress. Anxiety. 2005;21(4):154–160. doi: 10.1002/da.20076. [DOI] [PubMed] [Google Scholar]
- Parshall M.B., Schwartzstein R.M., Adams L., Banzett R.B., Manning H.L., Bourbeau J., Calverley P.M., Gift A.G., Harver A., Lareau S.C., Mahler D.A., Meek P.M., O'Donnell D.E. An official American thoracic society statement: update on the mechanisms, assessment, and management of dyspnea. Am. J. Respir. Crit. Care Med. 2012;185(4):435–452. doi: 10.1164/rccm.201111-2042ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renna M.E., O'Toole M.S., Spaeth P.E., Lekander M., Mennin D.S. The association between anxiety, traumatic stress, and obsessive-compulsive disorders and chronic inflammation: a systematic review and meta-analysis. Depress. Anxiety. 2018;35(11):1081–1094. doi: 10.1002/da.22790. [DOI] [PubMed] [Google Scholar]
- Rietveld S., Houtveen J.H. Acquired sensitivity to relevant physiological activity in patients with chronic health problems. Behav. Res. Ther. 2005;42(2):137–153. doi: 10.1016/S0005-7967(03)00104-9. [DOI] [PubMed] [Google Scholar]
- Röhricht F., Sattel H., Kuhn C., Lahmann C. Group body psychotherapy for the treatment of somatoform disorder-a partly randomised-controlled feasibility pilot study. BMC Psychiatry. 2019;19(1):120. doi: 10.1186/s12888-019-2095-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo J., Katon W., Sullivan M., Clark M., Buchwald D. Severity of somatization and its relationship to psychiatric disorders and personality. Psychosomatics. 1994;35(6):546–556. doi: 10.1016/S0033-3182(94)71723-0. [DOI] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Inter. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tang Q., Cheng Z., Yuan A., Deng Y. Application and analysis of SCL-90 in China. Chin. J. Clin. Psych. 1999;7:16–20. [in Chinese] [Google Scholar]
- Timmers I., Quaedflieg C., Hsu C., Heathcote L.C., Rovnaghi C.R., Simons L.E. The interaction between stress and chronic pain through the lens of threat learning. Neurosci. Biobehav. Rev. 2019;107:641–655. doi: 10.1016/j.neubiorev.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassend O., Røysamb E., Nielsen C.S., Czajkowski N.O. Musculoskeletal complaints, anxiety-depression symptoms, and neuroticism: a study of middle-aged twins. Health Psychol. 2017;36(8):729–739. doi: 10.1037/hea0000484. [DOI] [PubMed] [Google Scholar]
- Vassend O., Røysamb E., Nielsen C.S., Czajkowski N.O. Fatigue symptoms in relation to neuroticism, anxiety-depression, and musculoskeletal pain. A longitudinal twin study. PLoS One. 2018;13(6) doi: 10.1371/journal.pone.0198594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Murray A.M., Toussaint A.K., Chen L., Guo W.J., He N., Luo S.X., Yu J.Y., Liu Y., Huang M.J., Dong Z.Q., Zhang L. Why is the recognition rate of psychological distress under-estimated in general hospitals? A cross-sectional observational study in China. Medicine. 2019;98(27):e16274. doi: 10.1097/MD.0000000000016274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2003. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. https://www.who.int/csr/sars/country/table2003_09_23/en/.
- World Health Organization, 2020a. Coronavirus disease 2019 (COVID-19) situation report–11. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4. Accessed 31 January 2020.
- World Health Organization, 2020b. Coronavirus disease 2019 (COVID-19) situation report–41. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200301-sitrep-41-covid-19.pdf?sfvrsn=6768306d_2 Accessed 01 March 2020.
- Zantinge E.M., Verhaak P.F., Kerssens J.J., Bensing J.M. The workload of GPs: consultations of patients with psychological and somatic problems compared. Br. J. Gen. Pract. 2005;55(517):609–614. [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, china: a cross-sectional study. Int. J. Environ. Res. Public Health. 2020;17(7):E2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]