Abstract
Balancing public health physical distancing guidelines and the need to provide critical mental health services for risky and psychiatrically complex patient populations without disruption, many systems swiftly pivoted to telehealth to provide care during COVID-19. Leveraging technology, Yale New Haven Psychiatric Hospital's ambulatory services designed and deployed virtual intensive outpatient (IOP) and outpatient (OP) group-based services rapidly. Strategies for rapid deployment of group-based services, including action steps transitioning to telehealth, clinical protocols, and remote workforce training, early observations and challenges to implementation are described as helpful tools for clinical settings with similar needs to prevent infectious spread while addressing the mental health needs of patients.
Keywords: COVID-19, Telehealth, Group-based treatment
Balancing public health physical distancing guidelines and the need to provide mental health services for risky and psychiatrically complex patient populations, many systems swiftly pivoted to telehealth to continue to provide care during COVID-19. The transition to telehealth in certain domains of the psychiatry service array (e.g., group-based psychotherapy) was challenged as pre-COVID telehealth infrastructure was largely limited to individual patient and provider interactions, which did not allow for provision of the full scope of services typically provided in intensive outpatient programs (IOP) and similar levels of care (Childs et al., 2020, Hom et al., 2020). Typically, IOP services are designed to meet the needs of patients with high to moderate psychiatric distress, many of whom are transitioning from inpatient psychiatric treatment and require ongoing stabilization (Ilgen et al., 2008, Olfson et al., 2016) or are referred from psychiatric emergency departments to circumvent hospitalization. Furthermore, the bulk of interventions within these programs are delivered in group-based or multi-participant (e.g., family psychotherapy sessions) formats. Creation of IOP level of care virtually was critical to prevent patient decompensation and sustain progress toward mental health recovery by providing the needed level of psychiatric intervention. Continuing outpatient (OP) group-based services, treatment for individuals who have completed IOP level and may benefit from continued psychotherapy at lower frequency than IOP, is equally important.
Indeed, recent research indicates that individuals living with a mental health illness have expressed concerns about disruptions in their care and ability to receive services and decompensation (Costa et al.). Thus, Yale New Haven Psychiatric Hospital's (YNHPH) ambulatory services emergently designed and piloted virtual group-based psychotherapy, which was later deployed to all IOP and OP ambulatory services within YNHPH, subsequently disseminated within Yale New Haven Hopsital's larger psychiatric and behavioral health system network and recently to other independently licensed care facilities for adaptation in their care settings. To provide broader access to the strategy alongside others in similar settings (Hom et al., 2020), this brief report reviews the strategy used by YNHPH to provide telehealth group-based IOP and OP services, including the sequence of actions to transition to telehealth, the clinical protocol (as supplemental materials), remote workforce training, early observations and preliminary outcomes, lessons learned, and challenges to implementation. Informatic workflows and clinical operations for the pilot are summarized elsewhere (Childs et al., 2020).
1. Strategy and sequence of actions
1.1. Immediate treatment responses
The first positive case of COVID-19 involving a Connecticut resident was reported by the State of Connecticut Governor's Office on March 8th, 2020. According to data provided by the Connecticut Department of Public Health cases escalated significantly in mid-March and peaked in mid-April. Accordingly, on March 16th, the final day of in-person services, assessment guidelines and corresponding interim treatment recommendations (see supplemental materials) for subsequent patient treatment contacts were developed to stratify psychiatric acuity of enrolled IOP and OP patients. Namely, multidisciplinary clinical teams reviewed all enrolled IOP and OP patients, established corresponding treatment plans and conveyed plans by phone to patients (and where pertinent in adolescent programs, caregivers) the same day. Plans were effective immediately. New referrals for IOP and OP ambulatory services were limited to referrals from within the health system's psychiatric emergency services and inpatient units. Community referrals were temporarily diverted to alternative resources. Social work and psychiatrist intakes continued on-site with infection control precautions (pre-visit symptom screening, arrival symptom screening and vitals, PPE for patients and staff, physical distancing, capacity limits, on-site environmental services providing sanitization), and transitioned to telehealth using Epic MyChart (Epic Systems Corporation, Verona, WI) video visits wherever possible.
1.2. Telehealth group task force and protocol development
Next, a multidisciplinary task sub-group was created, comprised of psychologists, psychiatrists, social workers, support staff, and ambulatory leadership to develop a comprehensive protocol for the virtual group-based psychotherapy programming. Overarching tasks of the protocol development included selection of a viable and readily accessible technology platform, identification of technology access and training needs for staff, new development or reconfiguration of existing workflows and corresponding documentation for patient intakes and program onboarding, delivery of interventions (groups, crisis management, medication management, family sessions, etc.) including adaptation of evidence-based psychotherapy content for virtual platform, and evaluation of progress. Accordingly, the sub-group met daily virtually with frequent interim electronic communication and the dyadic leaders of this task subgroup, reported out efforts three times weekly during the psychiatry and behavioral health site-based incident command center (SICCS), linked to the larger Hospital Incident Command System (HICS) (Persoff et al., 2018).
First, Zoom for healthcare was the identified technology platform to facilitate the IOP services, clinical team communications and pertinent staff trainings, due to allowances issued by the Office of Civil Rights (HHS Office of the Secretary, Office for Civil Rights, Ocr) permitting the use of Zoom. Next, the Task Force created the virtual group protocol, including workflows for clinicians and staff delivering the interventions as well as patient enrollment, consenting and onboarding. Fuller details of this process are included as supplemental materials and pertinent elements are described in brief below.
As successful deployment would turn on communication, a comprehensive communication plan for the interdisciplinary virtual teams was developed, including a daily virtual safety huddles to review major concerns for actively enrolled patients, review patient clinical needs (e.g., med management; family meeting), and scheduled intakes. Huddles were also designed to include a “tech check” to allow for identification of any clinician/staff or patient related IT concerns, review staffing assignments or needed supports, and pertinent workflow reminders or changes for each treatment day (supplemental materials). Consistent with other recently released protocols (Hom et al., 2020), descriptions of roles and responsibilities for each team member from clinicians, to outpatient psychiatric counselors, to administrative staff were also detailed and provided to team members.
Next, procedures for the group psychotherapy, medication management and other critical elements of the IOP service array (e.g., crisis management/clinician check-ins, family meetings, individual therapy), were developed. Group protocols were designed to provide a minimum of three-hours of structured clinical services per scheduled IOP treatment day and fewer than three-hours of the same for OP level of care. Specifically, a dyad model, in which one clinician delivered the psychotherapy and the other facilitated IT considerations and managed individual patient needs, was chosen to deliver the interventions. This model also allowed for management of the risk of the facilitator being disconnected and supported monitoring and management of patient engagement in the treatment. Psychiatrist medication management and evaluation visits were streamlined into the workflow by using the ‘breakout’ rooms feature in Zoom and were thus able to receive these services in the fashion replicating the in-person practice patterns of the IOPs. Likewise, breakout rooms were utilized to support individual patient-clinician interactions, during the larger group sessions without needed to switch platforms, should a patient request to do so or provide report or interaction during the group requiring additional evaluation (e.g., reviewing safety plan after reporting high suicide ratings in group; see supplemental materials). Ideal patient cap for each group was 8-10, with a maximum capacity of 12. The protocol piloted on March 30th, 2020 and 8 patients were provided on-boarding into the group. The model was elected for dissemination within two adolescent and two adult (one large and one smaller) programs and workforce training and IOP and OP group-based services began in earnest on April 6th, 2020 following the pilot and trainings.
Working to reduce the spread of infection not only to the public, but also to providers, all of whom needed to be trained rapidly, and in sizeable numbers required training to occur virtually using Zoom. Physician and clinician workforce had begun working remotely, staggering teams in small numbers and rotating one week on-site and two weeks off-site to manage any ongoing in-person clinical issues. Clinicians and support staff participated in a minimum of three-hours of training to review in-detail the virtual group workflow and gain skills practice in use of the Zoom platform. Clinicians were guided through steps on patient consent, enrollment, the comprehensive patient on-boarding protocol (IT coaching, scheduling of psychotherapy groups, group rules and expectations; see supplemental materials), pertinent documentation and billing considerations, and adaptations necessary to translate psychotherapy interventions to the virtual environment. Psychiatrists participated in a 1.5-hour training each to review the medication management workflow and how to successfully accept invitations to Zoom breakout rooms.
Communication with clinicians and physician workforce was critical in the early days of deployment. The task force group routinely convened to review findings in each phase of rollout in programs, problem solve any technological challenges and identify staff/provider education needs. Ambulatory leadership held 30-minute daily briefing meetings with clinician leads from each program to provide support, reinforce and review workflows in the provision of telehealth services and track progress.
2. Early observations
Observational data were queried from the hospital system EMR from April 6th- May 29th, 2020 to document the patterns in telehealth usage and the transition to majority services provided via virtual group. Additionally, data were queried from October 1st, 2019–May 29th, 2020 to evaluate preliminary outcomes by comparing pre-COVID rates of completed appointments, cancellations and no-shows to scheduled services to rates observed during the virtual group deployment period. Data are classified in two categories within the EMR: visits and appointments. For any given treatment day, each service a patient is scheduled to receive is classified as a unique appointment in the EMR. At the IOP level of care, patients are scheduled for a minimum of three hours of structured clinical services per treatment day (e.g., 3 psychotherapy groups; 2 psychotherapy groups and 1 family meeting, etc.). At the OP level of care, patients are scheduled for fewer than three hours of structured clinical services per treatment day. Each treatment day comprised of scheduled appointments constitutes a “visit” within the EMR. That is, a visit describes one unique patient being treated any number of times, by one site, in a single day.
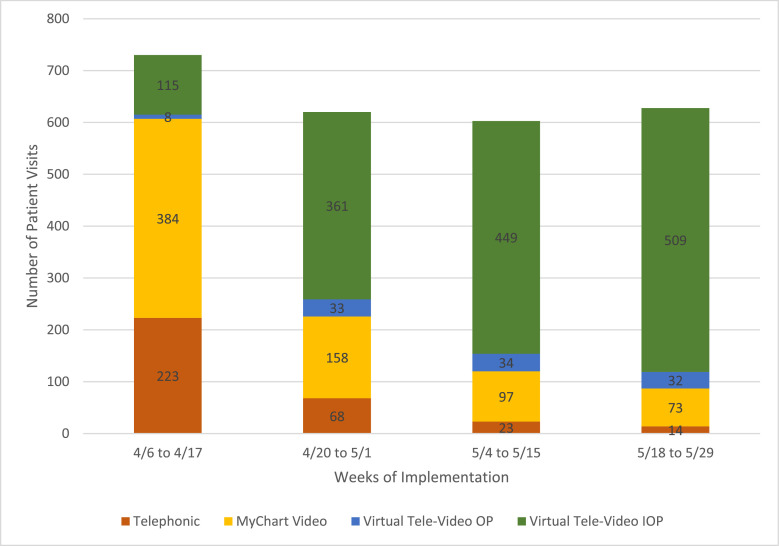
Fig. 1, displays individual patient visit volume data by week for all four ambulatory programs providing virtual group-based services. The telehealth visits were categorized into four groups: Telephonic, My Chart Video, Virtual Tele-Video OP (Group < 3 hours), and Virtual Tele-Video IOP (group ≥ 3 hours) visits. As can be seen in Fig. 1, group-based services were gradually restored within a matter of weeks, such that they comprised the majority of visit volume by week 3 of the broader implementation across these four programs.
Fig. 1.
Transition to virtual group-based telehealth visits during COVID-19 by deployment week for four ambulatory programs.
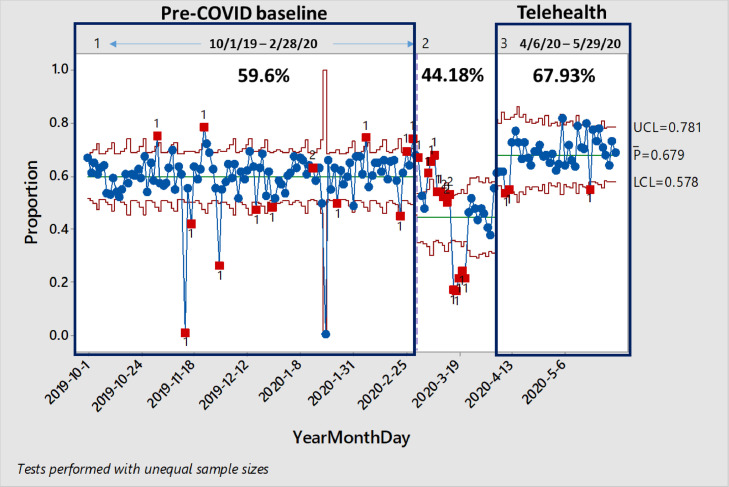
Next, preliminary outcomes were evaluated by comparing the proportion of completed, cancelled or no-showed scheduled appointments for each visit (i.e., treatment day) during pre-COVID (October 1st, 2019–February 29th, 2020) to that of the virtual group deployment time period (April 6th, 2020–May 29th, 2020). Data was obtained for one program to assess preliminary results. This program accounted for 61.2% of all patient volume, while the three smaller programs, accounted for the remaining portion of patient volume. Data were available for one program, though for the program associated with over half the total visit volume (61.2%) of all four programs as compared to the three other smaller programs. Specifically, P-charts were used to monitor the proportion of completed appointments during the pre-COVID stage as compared to the telehealth deployment stage. Analyses revealed a statistically significant increase in proportion of completed appointments during the telehealth deployment period (67.95%) as compared to the pre-COVID period (59.60%; χ2 = 106.4, p < .0001). As can be seen in Fig. 2 , there was a notable decrease in proportion of completed appointments during the month of March, when the pandemic first hit (44.18%) as compared to pre-COVID period, and the telehealth deployment period represents a significant recovery of completed appointments. Finally, to date, we have not observed increased trends of hospitalizations or worsening clinical outcomes as compared to pre-COVID rates using telehealth.
Fig. 2.
Monitoring proportion of completed appointments for one large adult ambulatory site during pre-COVID and virtual group-based deployment period.
3. Challenges and considerations
Several key challenges arose related to deployment in the COVID-19 context. First, rapid changes in national and intuitional guidance about the speed and spread of SARS-CoV2 required equally rapid responsiveness in protocols around infection prevention. Each new change impacted physician and clinician workforce training and required clinical adjustments to telehealth implementation. The pace of new learning was challenging for many staff, particularly around comfort with IT and careful attention to provider/staff needs to debrief proved useful. Patient comfort and familiarity navigating IT also required thoughtful attention, although teenagers who interacted with technology routinely needed less psychoeducation on technology than other patient populations. Special provisions for teenagers to obtain proxy access and permissions to access the MyChart associated with their medical record and health information were easily navigated, though were also important considerations. Additional considerations included troubleshooting patient access to technology and supports (i.e., WIFI), whether patients had consistent access to private space, and social supports to optimize successful participation (i.e., parent support for teens, childcare for adults, etc.) Finally, patients seen in YNHPH's ambulatory clinic, which focuses on treatment of individuals with severe and prolonged mental illness, many of whom are older and have presentations complicated by multiple social determinants of health, generally opted out of receiving virtual video services and most patients treated within this population (70-75%) continued to receive outpatient individual contacts telephonically.
In keeping with preliminary acceptability and feasibility findings reported in similar settings elsewhere (Hom et al., 2020), early observations from the current study regarding visit volume and patient appointment completion rates may also be early indicators of support for acceptability and feasibility of the group-based telehealth protocol. However, more research is needed to more fully examine patient experience, quality and safety, as well as clinical efficacy of telehealth interventions. Finally, though these protocols were developed during the pandemic emergency and benefitted patients, they should continue to be refined over time as the need for telehealth and offsite intervention may be adjusted given payment and regulatory considerations. Different clinical needs may arise as the pandemic begins to resolve in different parts of the United States and beyond.
Disclosures
None.
Funding
None.
CRediT authorship contribution statement
Amber W. Childs: Conceptualization, Methodology, Formal analysis, Resources, Writing - original draft, Writing - review & editing. Katherine Klingensmith: Resources, Methodology, Writing - review & editing. Sandra M. Bacon: Formal analysis, Data curation, Writing - review & editing. Luming Li: Conceptualization, Writing - review & editing.
Declaration of Competing Interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to thank Amy Bradley, Carol Cestaro, and other members of the Yale New Haven Psychiatric Hospital for their supportive work in deploying these protocols and their work in the programs which helped inform this article. We would also like to thank Adam Unger for his support in obtaining observational data. Finally, thank you to the members of the multidisciplinary treatment teams for their enduring committment to high quality clinical care of high-risk patients during this time of crisis.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113425.
Appendix. Supplementary materials
References
- Childs Amber W., Unger Adam, Li Luming. Rapid design and deployment of intensive outpatient group-based psychiatric care using telehealth during COVID-19. J Am. Med. Inf. Assoc. 2020 doi: 10.1093/jamia/ocaa138. Accepted 09 June. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costa M, Pavlo A, Reis G, et al. COVID-19 concerns among persons with mental illness. Psychiatric Services. Accepted 28 April 2020. DOI: 10.1176/appi.ps.202000245. [DOI] [PubMed]
- 3.HHS Office of the Secretary, Office for Civil Rights, Ocr. Notification of Enforcement Discretion for Telehealth. HHS.gov.https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Published March 30, 2020. Accessed May 30, 2020.
- Hom MA, Weiss RB, Millman ZB, Christensen K, Lewis EJ. Cho, S et al. Development of a virtual partial hospital program for an acute psychiatric population: Lessons learned and future directions for telepsychotherapy. J. Psychother. Integr. 2020:366–382. doi: 10.1037/int0000212. [DOI] [Google Scholar]
- Ilgen MA, Hu KU, Moos RH, McKellar J. Continuing care after inpatient psychiatric treatment for patients with psychiatric and substance use disorders. Psychiatric Serv. 2008:982–988. doi: 10.1176/ps.2008.59.9982. [DOI] [PubMed] [Google Scholar]
- Olfson M, Wall M, Wang S, Crystal S, Liu SM, Gerhard T, Blanco C. Shortterm suicide risk after psychiatric hospital discharge. J. Am. Med. Assoc. Psychiatry. 2016:1119–1126. doi: 10.1001/jamapsychiatry.2016.2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persoff J, Ornoff D, Little C. The role of the hospital medicine in emergency preparedness: a framework for hospitalist leadership in disaster preparedness, response, and recovery. J. Hosp. Med. 2018:713–718. doi: 10.12788/jhm.3073. [DOI] [PubMed] [Google Scholar]
- The Connecticut Department of Public Health (2020). https://data.ct.gov/stories/s/COVID-19-data/wa3g-tfvc/. Retrieved 20 August 2020.
- The Office of the Governor of Connecticut (2020) https://portal.ct.gov/Office-of-the-Governor/News/Press-Releases/2020/03-2020/Governor-Lamont-Announces-First-Positive-Case-of-Novel-Coronavirus-Involving-a-Connecticut-Resident. Retrieved 20 August 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.