Abstract
Public health strategies to curb the spread of the coronavirus involve sheltering at home and social distancing are effective in reducing the transmission rate, but the unintended consequences of prolonged social isolation on mental health have not been investigated. We focused on Hong Kong for its very rapid and comprehensive response to the pandemic and strictly enacted social distancing protocols. Thus, Hong Kong is a model case for the population-wide practice of effective social distancing and provides an opportunity to examine the impact of loneliness on mental health during the COVID-19. We conducted an anonymous online survey of 432 residents in Hong Kong to examine psychological distress in the community. The results indicate a dire situation with respect to mental health. An astonishing 65.6% (95% C.I. = [60.6%, 70.4%]) of the respondents reported clinical levels of depression, anxiety, and/or stress. Moreover, 22.5% (95% C.I. = [18.2%, 27.2%]) of the respondents were showing signs of psychosis risk. Subjective feelings of loneliness, but not social network size, were associated with increased psychiatric symptoms. To mitigate the potential epidemic of mental illness in the near future, there is an urgent need to prepare clinicians, caregivers and stakeholders to focus on loneliness.
Keywords: COVID-19, Global mental health, Loneliness, Depression, Anxiety, Psychosis
1. Introduction
The Corona Virus Disease 2019 (COVID-19), first started in China in December 2019, has spread across the globe within a few months and was declared a pandemic on March 11th, 2020. Many mental health professionals and scholars predict that the pandemic will have profound and long-lasting impact on mental health worldwide (Holmes et al., 2020). Even prior to the current pandemic, mental illness was a global public health issue. According to the 2013 Global Burden of Diseases study, psychological disorders were the fifth leading cause of disability worldwide (Salomon et al., 2015). Anxiety disorders and major depressive disorder each affected over 250 million people, and acute schizophrenia carried the highest disability weight of all diseases (Murray et al., 2015; Vos et al., 2015). Based on past observations of surges of psychiatric disorders and deaths by suicide following large-scale, life-threatening epidemics—for example, SARS in 2003 (Cheung et al., 2008; Mak et al., 2009), the 2014–2016 Ebola epidemic (Jalloh et al., 2018), and the 1918–19 influenza pandemic (Mamelund, 2010; Wasserman, 1992)—and the unprecedented scale of the COVID-19 pandemic, the extraordinary societal burden of mental illness is likely to grow further and rapidly in the near future. Many expect a significant increase in the incidence of posttraumatic stress disorder (PTSD), depression, anxiety, substance use, suicide and other mental disorders, post-COVID among the survivors, their caregivers, and healthcare workers (Holmes et al., 2020). Indeed, preliminary results from China and Italy confirm the high prevalence of PTSD, anxiety, depression, and perceived stress among the survivors of COVID-19 and healthcare workers (Bo et al., 2020; Rossi et al., 2020).
The mental health impact of COVID-19 will not be limited to those who are directly confronting (or have confronted) the disease. To contain the spread of the virus, nearly every country has implemented unprecedented levels and scales of quarantine, physical distancing, and even community lockdown. Although effective in flattening the epidemic curve (Matrajt and Leung, 2020), these public health strategies severely disrupt daily social life and limit interpersonal interactions with adverse consequences of social disconnection and loneliness, which play a central role in poor physical and mental health outcomes (Cacioppo et al., 2015). Loneliness has been linked to premature death from stroke and cardiovascular diseases (Valtorta et al., 2016), altered expression of genes involved in inflammation and antiviral response (Cole et al., 2015), as well as increased depression, generalized anxiety disorder, panic disorder, suicide risk and psychosis (Badcock et al., 2020; Beutel et al., 2017). With the prolonged social distancing related to COVID-19, the general public will soon experience a surge in physical and mental illness. Indeed, emerging data from China suggest increased incidence of mental illness among the general population following the COVID-19 epidemic (Gao et al., 2020; Wang et al., 2020). Preliminary data also support the association between increased loneliness and greater depression (Killgore et al., 2020), although this relationship may be moderated by other psychological factors (Shrira et al., 2020). Further studies are needed to confirm the role of loneliness in mental health during COVID-19 with important factors likely impacting wellbeing controlled, and extend the investigation from depression and anxiety to other mental health concerns such as substance use and symptoms indicative of more severe disorders (e.g., psychosis).
The present study examined wellbeing of the general public following prolonged social distancing during the COVID-19 pandemic, and the role of loneliness and social network. We selected one of the first regions affected by COVID-19 with strictly enforced quarantine and social distancing protocols since late January 2020—Hong Kong. Hong Kong is a Special Administration Region of China separated by a border with the mainland. In the first week of January, when the outbreak in Wuhan, China was first reported, Hong Kong started implementing rigorous preventive measures including quarantine, isolation, and social distancing, along with other hygiene practices such as wearing face masks. Despite its geographical proximity to China and the large number of visitors from China, Hong Kong has achieved a relatively flat epidemic curve and, as of June 7th, 2020, only four COVID-related deaths (Government of the Hong Kong Special Administrative Region, 2020). The rapid and comprehensive response of the community is credited as the major reason for the success in containing the outbreak (Cowling et al., 2020). However, this early rapid response also means that the community has been living in prolonged social isolation since January 2020. We conducted an online survey of Hong Kong residents between March 31st and May 30th, 2020 to assess the physical and mental wellbeing after the city had implemented widespread social distancing for two months. We expected to observe high rates of common psychiatric symptoms (depression, anxiety, stress) as well as symptoms indicating emergence of severe mental illnesses (psychosis risk). Furthermore, we expected that high levels of loneliness would be observed and would significantly explain health and mental health status, even after controlling for other key factors likely impacting wellbeing.
2. Methods
2.1. Participants
Respondents of this online survey were adults (age 18 or above), regardless of ethnic backgrounds and nationalities, currently residing in Hong Kong. A total of 555 unique visitors viewed the survey overview page in the period from March 31st, 2020 to May 30th, 2020, out of which 461 were eligible for the survey by answering 18 or above for age and selecting “yes” or “part of the time” for the question of Hong Kong residence. Of the eligible participants, 432 (93.7%) completed at least the demographics section and 347 (75.3%) completed the entire survey. Only respondents completed at least the demographics section (N = 432) were included in the analyses below. These respondents on average completed 87.6% (median = 100%; SD = 27.5%) of the survey.
2.2. Procedure
The survey was available in two languages (traditional Chinese and English) and was run on the Qualtrics online platform (Provo, UT). Links to the survey were circulated on social media, local online forums or websites, and via words of mouth to reach the target population of Hong Kong residents. The survey was anonymous as no identifying information (e.g., name, date of birth, contact information, IP address) was asked or recorded. The median time respondents spent on the survey was 10 min 33 s. This study received exempt determination from the University of Michigan Institutional Review Board (IRB# HUM00179454).
2.3. Measures
The survey consisted of 145 questions assessing participants’ demographics, general health, mental health, loneliness, and social network. The demographics and general health questions used in this survey (English version) can be found in Supplementary Information 1. Items related to mental health, loneliness, and social network can be found in prior publications (detailed below).
For mental health, the 21-item version of the Depression Anxiety Stress Scales (DASS-21) (Lovibond and Lovibond, 1995a; Taouk Moussa et al., 2001) was used to assess depression, anxiety, and stress levels. Scores for Depression, Anxiety, and Stress were calculated for each individual and classified into severity levels (normal, mild, moderate, severe, or extremely severe) according to the published norms (Lovibond and Lovibond, 1995b). The 16-item version of the Prodromal Questionnaire (PQ-16) (Ising et al., 2012) was used to screen for psychosis risk symptoms. For each individual, Total Score (i.e., number of items endorsed) and Distress Score (sum of distress related to endorsed items) were computed. A Total Score of 6 or higher was considered screened positive for psychosis risk syndrome (Ising et al., 2012). The UCLA Loneliness Scale (Russell, 1996) was used to assess the respondent's perceived loneliness. The Social Network Index (SNI) (Cohen, 1997) was used to measure diversity (i.e., number of social roles) and size (number of people with whom the respondent has regular contact) of social network.
2.4. Statistical analysis
Respondents’ demographics, general health, and mental health (DASS-21 and PQ-16 scores), loneliness (UCLA total score), and social network (SNI diversity and size scores) were examined with descriptive statistics.
To understand the relationship of loneliness and social network to health and mental health, hierarchical regression analyses were conducted. This model comparison approach allows us to examine whether loneliness and/or social network can explain health and mental health above and beyond other demographic, psychological, and socio-political factors that likely have influence on one's wellbeing. These include age, sex, exposure to domestic abuse, and worries about COVID-19. Given the current political context of Hong Kong where the residents had already been exposed to prolonged societal unrest and distress, we also considered the level of participation in the protest as a potentially influential factor. Therefore, in Step 1 of the hierarchical regression analyses, age, sex (two dummy coded variables: female, and no response to question of sex), frequency of domestic violence/abuse, level of concern about COVID-19, and level of participation in the protests were entered as predictors into the reduced model. In Step 2, Stepwise method was used to add loneliness (UCLA total score) and social network (SNI diversity and size) measures as predictors into the full model. The dependent variables included: 1) self-report overall health; 2) numbers of days (over the past 30 days) in which physical health was not good; 3) numbers of days in which mental health was not good; 4) number of days in which poor physical or mental health affected usual activities; 5) number of days in which pain affected usual activities; 6) number of days in which the respondent felt worried, anxious, or tense; 7) DASS-21 Depression; 8) DASS-21 Anxiety; 9) DASS-21 Stress; 10) PQ-16 Total Score; and 11) PQ-16 Distress Score.
Since level of participation in the Hong Kong protests was not a significant predictor when included in any of the reduced or full models, and that nearly 20% of the respondents had a missing value on the item (they chose not to answer the question), we removed this variable from the regression analyses to increase the sample size. The results of the regression analyses with or without this variable were virtually identical. We only report the results without this predictor variable below.
3. Results
Because some respondents did not complete all the questions, the percentages reported below were calculated using the number of respondents completed the corresponding section as the denominator.
3.1. Demographics
Summary of the 432 respondents who completed the demographics section is presented in Table 1 . Respondents’ mean age was 33.4 years (SD = 10.6), and the majority (56.9%) identified as female. Most of the respondents completed the survey in Chinese (88.4%) and resided full-time in Hong Kong (96.5%). The respondents were highly educated, with 70.8% having a college degree or higher level of education. Most of them were living with others (91.0%), never married (63.0%), and employed (64.8%). Only 4.6% were healthcare workers. 5.1% endorsed having been exposed to domestic violence or abuse in the past week. Most of the respondents (73.1%) have participated in the anti-government and pro-democracy protests since June 2019.
Table 1.
Participant demographics (N = 432).
| Range | mean (SD) | |
|---|---|---|
| Age (years) | 18 – 70 | 33.4 (10.6) |
| N | % | |
| Survey language | ||
| Chinese | 382 | 88.4% |
| English | 50 | 11.6% |
| Sex | ||
| Female | 246 | 56.9% |
| Male | 164 | 38.0% |
| Other | 1 | 0.2% |
| Prefer not to answer | 21 | 4.9% |
| Residency in Hong Kong | ||
| Full-time | 417 | 96.5% |
| Part-time | 15 | 3.5% |
| Education level | ||
| Primary/elementary school or below | 1 | 0.2% |
| Junior high | 11 | 2.5% |
| High school | 72 | 16.7% |
| Associate degree | 42 | 9.7% |
| Bachelor's degree | 238 | 55.1% |
| Postgraduate degree | 68 | 15.7% |
| Marital status | ||
| Never married | 272 | 63.0% |
| Married | 143 | 33.1% |
| Cohabiting | 8 | 1.9% |
| Separated | 1 | 0.2% |
| Divorced | 7 | 1.6% |
| Widowed | 1 | 0.2% |
| Living status | ||
| Living with others | 393 | 91.0% |
| Living alone | 39 | 9.0% |
| Employment status | ||
| Employed | 280 | 64.8% |
| Full-time student | 81 | 18.8% |
| Homemaker | 25 | 5.8% |
| Unemployed | 46 | 10.6% |
| Healthcare worker | ||
| Yes | 20 | 4.6% |
| No | 412 | 95.4% |
| Frequency of domestic violence experienced in past week | ||
| Never | 410 | 94.9% |
| Once | 20 | 1.9% |
| A few times | 2 | 3.0% |
| Every day | 1 | 0.2% |
| Participation in Hong Kong protests | ||
| Never | 33 | 7.6% |
| Rarely | 73 | 16.9% |
| Sometimes | 131 | 30.3% |
| Often | 112 | 25.9% |
| Prefer not to answer | 83 | 19.2% |
| In Hong Kong during SARS outbreak 2003 | ||
| Full-time | 385 | 89.1% |
| Part of the time | 12 | 2.8% |
| No | 35 | 8.1% |
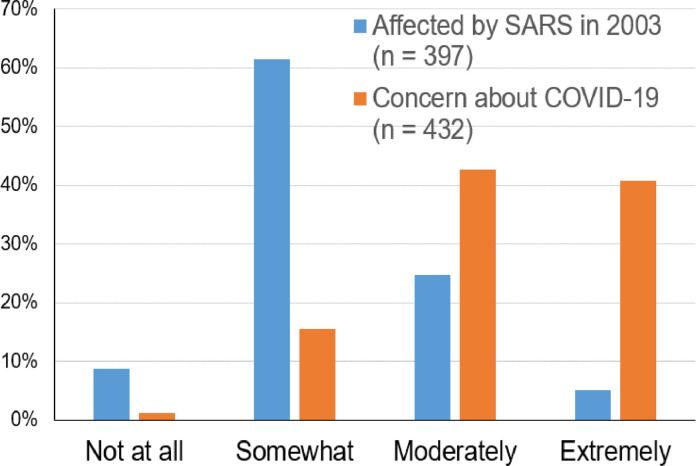
Most (n = 397; 91.9%) of the respondents experienced the 2003 SARS outbreak as they resided exclusively (n = 385) or partially (n = 12) in Hong Kong during that time. Among these respondents, 29.7% reported that they were moderately or extremely affected by the outbreak at the time. Comparatively, concern about the current COVID-19 epidemic was much higher, with 360 (83.3%) of the 432 respondents expressing moderate or extreme concern (Fig. 1 ).
Fig. 1.
Impact of the 2003 SARS outbreak and level of concern about COVID-19.
3.2. General health
392 respondents completed the general health section. For self-perceived overall health, rated on a 1–5 scale (representing “Excellent,” “Very good,” “Good,” “Fair,” and “Poor”), most respondents (71.4%) reported “Good” or better (median = 3.0, mean = 2.9, SD = 0.97). About a third (34.9%) endorsed one or more of the following types of illnesses in the past 30 days: head cold or chest cold (14.0%); gastrointestinal illness with vomiting or diarrhea (16.3%); flu, pneumonia, or ear infections (9.7%); an ongoing or chronic medical condition (6.9%). Only 3.8% were in mandatory or self-quarantine related to COVID-19 (median duration = 14 days). None were in inpatient hospital care.
Few (9.9%) of the 389 respondents were cigarette smokers (mean = 0.68 packs/day, SD = 0.36) or alcohol drinkers (19.1%; mean = 3.6 drinks/week, SD = 4.2). However, among those who smoke or drink, many endorsed having been smoking (41.0%) or drinking (28.0%) more than usual in the past 30 days.
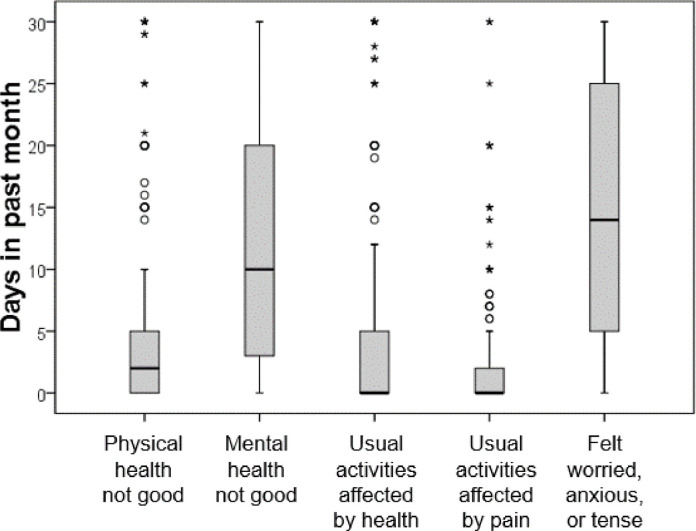
The number of days in which various health-related problems occurred over the past 30 days are summarized in Fig. 2 . Overall, the respondents reported more days affected by mental health issues than by physical health issues.
Fig. 2.
Number of days (over the past 30 days) in which health problems occurred. A) Physical health was not good: mean = 4.8 days (SD = 6.9). B) Mental health was not good: mean = 11.6 days (SD = 10.0); C) Usual activities were affected due to health problems: mean = 3.9 days (SD = 7.2); D) Usual activities were affected due to pain: mean = 1.9 (SD = 4.5); and E) Feeling worried, anxious, or tense: mean = 14.1 days (SD = 10.8).
3.3. Mental health
3.3.1. Depression, anxiety, and stress
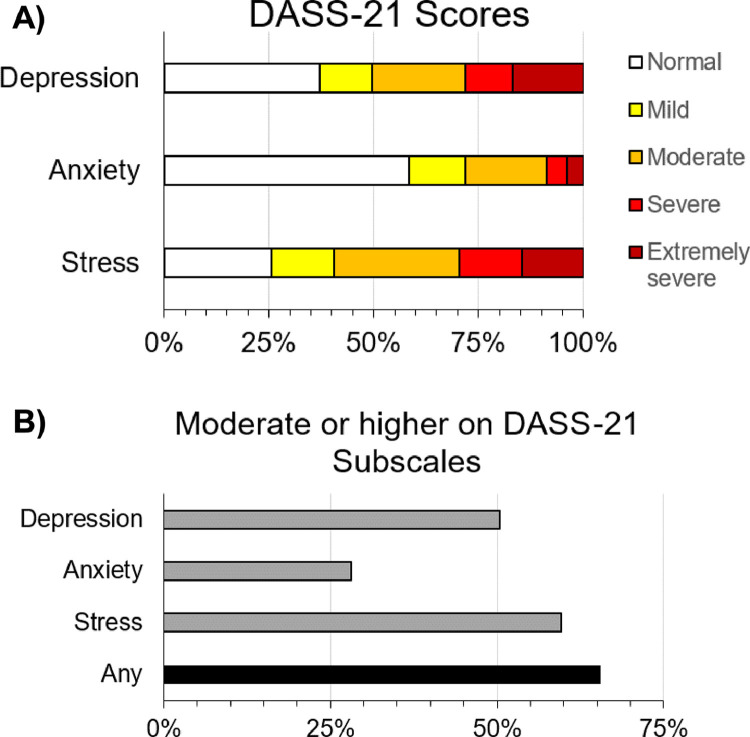
381 respondents completed the DASS-21. The mean subscale scores were 15.10 (SD = 10.97) for Depression; 9.46 (SD = 7.97) for Anxiety; 16.01 (SD = 9.53) for Stress. Based on the cutoff scores provided by Lovibond and Lovibond (1995a), 50.4% (95% C.I. = [45.3%, 55.5%]), 28.1% (95% C.I. = [23.6%, 32.9%]), and 59.6% (95% C.I. = [54.5%, 64.6%]) scored at the moderate or above levels for Depression, Anxiety, and Stress, respectively. Additionally, 65.6% (95% C.I. = [60.6%, 70.4%]) of the respondents scored moderate or higher on one or more of the three subscales. Detailed distributions of the responses are displayed in Fig. 3 .
Fig. 3.
Levels of depression, anxiety, and stress among 381 respondents. A) Percentages of respondents scoring at different severity levels of Depression, Anxiety, and Stress on the DASS-21. B) Percentages of respondents scoring moderate to extremely severe on each and any of the three areas on the DASS-21.
3.3.2. Psychosis risk symptoms
347 respondents completed the PQ-16, who on average endorsed 3.53 items (median = 3.0, SD = 3.24, range = 0 – 14) and reported a mean distress score of 3.78 (median = 2.0, SD = 5.09, range = 0 – 30). Using the cutoff number of endorsed items of 6 or more as the criterion (Ising et al., 2012), 22.5% (95% C.I. = [18.2%, 27.2%]) of this sample screened positive for ultra-high risk syndrome using the PQ-16.
3.4. Loneliness and social network
3.4.1. Loneliness
367 respondents completed the UCLA Loneliness Scale. The mean score was 49.7 (median = 50.0; SD = 10.5), more than one standard deviation above the published norms obtained from samples of college students and nurses in North America (Russell, 1996).
3.4.2. Social network diversity and size
356 respondents completed the Social Network Index, reporting a mean number of social roles of 4.9 (median = 5.0, SD = 1.8, range = 1 – 11). The mean number of people with whom the respondents have regular contact (i.e., at least once every 2 weeks) was 14.3 (median = 10.0, SD = 15.6, range = 0 – 118).
3.5. Predictors of health and mental health status
The model statistics of the hierarchical regression analyses are summarized in Table 2 ; coefficients statistics are presented in Supplementary Information 2 (Table S1). Briefly, even after controlling for the effects of key variables that could impact health and mental health (age, sex, domestic violence exposure, and level of concern about COVID-19), loneliness significantly explained variance (R2-change ranging from 1.3% to 29.2%) in all of the health and mental health measures (except the number of days in which usual activities were affected by pain). This amount was even higher for models using scores of validated scales of psychiatric symptoms (i.e., DASS and PQ16) as the dependent variable, with R2-change ranging from 12.3% to 29.2%. Social network diversity and size did not significantly explain any of the health and mental health measures.
Table 2.
Prediction of Health and Mental Health Status.
| Dependent variable | Model statistics |
Change statistics |
||||||
|---|---|---|---|---|---|---|---|---|
| df | R2 (95% C.I.) | F | P | R2 change (95% C.I.) | F change | df | p | |
| Single-item health/mental health measures | ||||||||
| Self-report general health | 6, 357 | 12.4% (6.2% – 18.6%) | 8.44 | <0.0001 | 5.2% (0.8% - 9.6%) | 21.09 | 1, 357 | <0.0001 |
| Days physical health not good | 6, 357 | 13.0% (6.7% – 19.4%) | 8.86 | <0.0001 | 5.8% (1.1% – 10.5%) | 23.83 | 1, 357 | <0.0001 |
| Days mental health not good | 6, 357 | 18.0% (11.0% – 25.0%) | 13.02 | <0.0001 | 9.4% (3.7% – 15.1%) | 40.74 | 1, 357 | <0.0001 |
| Days usual activities affected by health | 6, 357 | 9.1% (3.6% – 14.6%) | 5.96 | <0.0001 | 1.3% (−1.0% – 3.6%) | 5.23 | 1, 357 | .023 |
| Days feeling worries, anxious, or tense | 6, 357 | 18.1% (11.1% – 25.1%) | 13.13 | <0.0001 | 4.9% (0.6% – 9.2%) | 21.17 | 1, 357 | <0.0001 |
| Validated scales of psychiatric symptoms | ||||||||
| DASS Depression | 6, 357 | 38.9% (31.2% – 46.6%) | 37.88 | <0.0001 | 29.2% (21.3% – 37.1%) | 170.41 | 1, 357 | <0.0001 |
| DASS Anxiety | 6, 357 | 26.0% (18.4% – 33.6%) | 20.95 | <0.0001 | 13.5% (7.0% – 20.0%) | 64.99 | 1, 357 | <0.0001 |
| DASS Stress | 6, 357 | 29.4% (21.7% – 37.1%) | 24.80 | <0.0001 | 17.3% (10.2% – 24.4%) | 87.44 | 1, 357 | <0.0001 |
| PQ-16 Total Score | 6, 340 | 22.6% (15.0% – 30.2%) | 16.54 | <0.0001 | 13.1% (6.5% – 19.7%) | 57.60 | 1, 340 | <0.0001 |
| PQ-16 Distress Score | 6, 340 | 23.3% (15.7% – 30.9%) | 17.20 | <0.0001 | 12.3% (5.8% – 18.8%) | 54.62 | 1, 340 | <0.0001 |
Note. All predictive models included 6 predictive variables: age, sex (two dummy coded variables: female, and no response to the question of sex), frequency of domestic abuse/violence, level of concern about COVID-19, and UCLA loneliness score. Change statistics were relative to the reduced model, which contained only 5 predictive variables (i.e., all variables except UCLA loneliness score).
4. Discussion
The findings of this survey paint a very disconcerting picture of the mental health status among people in Hong Kong during the COVID-19 pandemic. Although many respondents reported overall good physical health and few days in the past month in which they were affected by physical health or pain issues, they suffered mental health issues frequently in that they experienced poor mental health or feeling worried, anxious or tense, on average, in more than one-third of the time over the past month. Their responses to validated scales of psychiatric symptoms suggest that almost two-thirds (65.6%) reported clinical levels of depression, anxiety, and/or stress. Population-wide incidence and prevalence of psychiatric disorders prior to COVID-19 have been tracked by the large community-based studies of mental health (Lam et al., 2015; Lee et al., 2011); weighted prevalence was estimated at 13.3% for any past-week for any psychiatric condition, with mixed anxiety and depressive disorder being the most frequent diagnoses. Therefore, our results from the current survey indicate a significant increase in the risk for mental illness in the general population.
Yet more concerning is the high rate (22.5%) of elevated risk for a psychotic disorder observed in this study. Previous studies using the same measure found only 4.0% of help-seeking young people in North America screened positive for psychosis-risk (Ising et al., 2012). A prior population-based household survey for mental disorders estimated a lifetime prevalence of all psychotic disorders to be approximately 2.5% among the Chinese adult population in Hong Kong (Chang et al., 2017); this estimate is similar to the prevalence reported globally, suggesting that the elevated psychosis risk found in this study was not due to a higher “baseline” psychosis risk among Hong Kong people.
This is a population with low rates of smoking (9.9%) or drinking alcohol on a regularly basis (19.1%). While the smoking rate in this sample was similar to that reported in the 2015 census (10.5%) (Census and Statistics Department, 2018), the drinking rate was much higher than the 11.1% reported in the Population Health Survey 2014/15 (Centre for Health Protection, 2017). Among those who smoke or drink alcohol regularly, many reported having been smoking (41%) or drinking (28%) more heavily in the past month. Taken together, these findings indicate that the societal impact of the COVID-19 in Hong Kong extends beyond the illness itself and well into the future, with sharp increases in the risk for depression, anxiety, stress, psychosis, and substance use.
In addition to psychiatric symptoms, level of loneliness was very high in this Hong Kong sample: it was one standard deviation elevated compared with samples of similar education attainment (college students and nurses) in North America (Russell, 1996). Furthermore, loneliness significantly explained physical and mental health across measures, even after accounting for the effects of other important variables (age, sex, domestic abuse/violence frequency, and level of concern for COVID-19). The only health measure not significantly explained by loneliness was the number of days affected by pain, likely due to the very low frequency of pain in this sample. Whilst the prevalence of psychological distress found in this sample during the pandemic is daunting, our finding that loneliness is playing a central role may give us a handle to address this public health emergency at a societal level. To mitigate the potential epidemic of mental illness in the near future, there is an urgent need to prepare clinicians, caregivers and stakeholders to focus on loneliness. Reducing loneliness could result in reduction of mental illness across all diagnostic categories. Our finding that social network size (number of social roles, and number of people in the social network) failed to explain any of the health and mental health measures suggests that it is the quality rather than quantity of interpersonal relationships that matters. Therefore, interventions that can strengthen social connectedness (e.g., training in communication and social skills, consistent group activities) may exert larger impact than focusing only on increasing the amount of social encounters. Furthermore, interventions need to be implemented at a broad societal level rather than for a small fraction of the population. Creative solutions, including those leveraging technology, are likely needed to help achieve this goal. It is important to remember that individuals with pre-existing psychiatric conditions or those who were already marginalized in society are likely to be impacted even more by the social distancing protocols introduced to reduce the transmission rate of the virus and economic aftermath of the pandemic (Tsai and Wilson, 2020; Yao et al., 2020), and we must deploy more resources and social capital to address the mental health needs of people disproportionately affected by the pandemic.
The COVID-19 pandemic unfolded against the backdrop of a political crisis and civil unrest in Hong Kong, sparked by a controversial legislation in March 2019. Mass anti-government protests broke out in June 2019 and have since strengthened into a widespread, ongoing pro-democracy movement (Reuters, 2020), which has been assailed by an unprecedented level of violent crackdown (Amnesty International, 2019; TIME, 2019) and persecution by the authorities (Pang, 2020). This sociopolitical context must be considered when interpreting the findings of this study. The city was already embattled with a mental health crisis before the pandemic. A study conducted in late 2019, just before the COVID-19 epidemic in Hong Kong, showed high rates of probable posttraumatic stress (12.8%) and depression (11.2%) among the residents, especially the younger (age 18–35) cohort who show higher level of support for the protests (Ni et al., 2020). The pandemic further deteriorated people's mental health, not only through prolonged social distancing, but also economic decline (Lam, 2020a), surge of unemployment rate (Lam, 2020b), and public mistrust of the government (Marlow and Hong, 2020; Radio Television Hong Kong, 2020). Therefore, the alarming COVID-19 related mental health status found in this study was likely amplified by ongoing societal problems, some of which are in common with other countries and some are unique to Hong Kong.
This study has several limitations. The sample was relatively young and highly educated, unlikely to be fully representative of the Hong Kong population. This was a cross-sectional study and lacked longitudinal data to track changes in mental health over time during the pandemic. However, the rates of psychiatric symptoms founded in this study were higher than the estimates reported in a study of a representative sample conducted in December 2019 (Ni et al., 2020), just before the first confirmed case of COVID-19 was reported. This provides some preliminary evidence for the adverse consequences of COVID-19 on mental health across broad domains including psychosis. Additionally, although level of participation in the Hong Kong protests was not a significant predictor of mental health status in the regression analyses, it should be noted that a non-trivial proportion of the respondents (~20%) chose not to answer this question. It is possible that respondents who participated frequently in the protests were more likely to skip this question because they were worried about political or legal repercussions. However, it is also possible that those who never or rarely participated in the protests tended to skip this question because of social desirability (the protests are widely supported by people in Hong Kong). It is unclear whether the data of this question were missing at random or not. In so far as we could test from the available data, we could only conclude that level of participation in the Hong Kong protests did not predict health/mental health status. This may be because the political crisis and social unrest affected everyone negatively regardless of one's political orientation. Obviously, this result applies only to this sample at this given point in time. The political situation has significantly worsened since our survey, so it is possible that the impact of participation in political protests has changed as well. Finally, the survey data were collected mostly in April 2020; it is unknown how mental health outcome would be impacted by the lifting of social distancing protocols worldwide, potentially followed by a second- or even third-wave of the pandemic. Close monitoring of the mental health impact of this pandemic is warranted.
To conclude, this study investigated the mental health status of ordinary citizens and the impact of loneliness in a city that was one of the first regions that practiced population-wide social distancing during the COVID-19 pandemic. The results indicate a dire situation with respect to mental health, with highly elevated rates of significant psychiatric symptoms including depression, anxiety, stress, and signs of psychosis risk. Subjective feelings of loneliness, but not social network size, significantly explained these increased psychiatric symptoms above and beyond other demographic factors. These findings together suggest that there will likely be an epidemic of mental illness in the near future, and preparing clinicians, caregivers and stakeholders to focus on alleviating loneliness would be one effective way to mitigate this impending public health crisis.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Ivy F. Tso: Project administration, Resources, Investigation, Data curation, Formal analysis, Visualization, Writing - original draft. Sohee Park: Conceptualization, Methodology, Writing - review & editing.
Declaration of Competing Interest
The authors declare no conflicts of interest pertinent to this study.
Acknowledgments
The authors thank the respondents for donating their valuable time to complete this survey.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113423.
Appendix. Supplementary materials
References
- Amnesty International, 2019. Hong Kong: arbitrary arrests, brutal beatings and torture in police detention revealed. https://www.amnesty.org/en/latest/news/2019/09/hong-kong-arbitrary-arrests-brutal-beatings-and-torture-in-police-detention-revealed/.
- Badcock J.C., Adery L.H., Park S. Loneliness in psychosis: a practical review and critique for clinicians. Clin. Psychol. Sci. Pract. 2020 doi: 10.1111/cpsp.12345. [DOI] [Google Scholar]
- Beutel M.E., Klein E.M., Brähler E., Reiner I., Jünger C., Michal M., Wiltink J., Wild P.S., Münzel T., Lackner K.J., Tibubos A.N. Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry. 2017;17:97. doi: 10.1186/s12888-017-1262-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bo H.-.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.-.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020;103:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S., Grippo A.J., London S., Goossens L., Cacioppo J.T. Loneliness: clinical Import and Interventions. Perspect. Psychol. Sci. 2015;10:238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census and Statistics Department, 2018. Thematic Household Survey Report No. 64. Hong Kong. https://www.statistics.gov.hk/pub/B11302642018XXXXB0100.pdf.
- Centre for Health Protection, 2017. Report of Population Health Survey 2014/15. https://www.chp.gov.hk/files/pdf/dh_phs_2014_15_full_report_eng.pdf.
- Chang W.C., Wong C.S.M., Chen E.Y.H., Lam L.C.W., Chan W.C., Ng R.M.K., Hung S.F., Cheung E.F.C., Sham P.C., Chiu H.F.K., Lam M., Lee E.H.M., Chiang T.P., Chan L.K., Lau G.K.W., Lee A.T.C., Leung G.T.Y., Leung J.S.Y., Lau J.T.F., van Os J., Lewis G., Bebbington P. Lifetime prevalence and correlates of schizophrenia-spectrum, affective, and other non-affective psychotic disorders in the Chinese adult population. Schizophr. Bull. 2017;43:1280–1290. doi: 10.1093/schbul/sbx056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung Y.T., Chau P.H., Yip P.S.F. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23:1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social Ties and Susceptibility to the Common Cold. JAMA J. Am. Med. Assoc. 1997;277:1940. doi: 10.1001/jama.1997.03540480040036. [DOI] [PubMed] [Google Scholar]
- Cole S.W., Capitanio J.P., Chun K., Arevalo J.M.G., Ma J., Cacioppo J.T. Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proc. Natl. Acad. Sci. 2015;112:15142–15147. doi: 10.1073/pnas.1514249112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling B.J., Ali S.T., Ng T.W.Y., Tsang T.K., Li J.C.M., Fong M.W., Liao Q., Kwan M.Y., Lee S.L., Chiu S.S., Wu J.T., Wu P., Leung G.M. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Heal. 2020;5:e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of the Hong Kong Special Administrative Region, 2020. Coronavirus Disease (COVID-19) in HK [WWW Document]. URLhttps://www.coronavirus.gov.hk/eng/index.html(accessed 6.7.20).
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ising H.K., Veling W., Loewy R.L., Rietveld M.W., Rietdijk J., Dragt S., Klaassen R.M.C., Nieman D.H., Wunderink L., Linszen D.H., Van Der Gaag M. The validity of the 16-item version of the prodromal questionnaire (PQ-16) to screen for ultra high risk of developing psychosis in the general help-seeking population. Schizophr. Bull. 2012;38:1288–1296. doi: 10.1093/schbul/sbs068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalloh M.F., Li W., Bunnell R.E., Ethier K.A., O'Leary A., Hageman K.M., Sengeh P., Jalloh M.B., Morgan O., Hersey S., Marston B.J., Dafae F., Redd J.T. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob. Heal. 2018;3 doi: 10.1136/bmjgh-2017-000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Letter to the Editor. Loneliness : a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam, E., 2020a. Pandemic and Politics Push Hong Kong's Economy Into Record Slump [WWW Document]. Bloomberg. URLhttps://www.bloomberg.com/news/articles/2020-05-04/hong-kong-set-for-deeper-economic-slump-as-companies-shed-jobs(accessed 6.7.20).
- Lam, E., 2020b. Hong Kong's Unemployment Rate Rises to Highest Since 2009 [WWW Document]. Bloomberg.URLhttps://www.bloomberg.com/news/articles/2020-05-19/hong-kong-s-unemployment-rate-rises-to-highest-since-2009(accessed 6.7.20).
- Lam L.C.-W., Wong C.S.-M., Wang M.-.J., Chan W.-.C., Chen E.Y.-H., Ng R.M.-K., Hung S.-.F., Cheung E.F.-C., Sham P.-.C., Chiu H.F.-K., Lam M., Chang W.-.C., Lee E.H.-M., Chiang T.-.P., Lau J.T.-F., van Os J., Lewis G., Bebbington P. Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: the Hong Kong Mental Morbidity Survey (HKMMS) Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:1379–1388. doi: 10.1007/s00127-015-1014-5. [DOI] [PubMed] [Google Scholar]
- Lee S., Ma Y.L., Tsang A. A community study of generalized anxiety disorder with vs. without health anxiety in Hong Kong. J. Anxiety Disord. 2011;25:376–380. doi: 10.1016/j.janxdis.2010.10.012. [DOI] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. 2 Ed. Psychology Foundation; Sydney, Australia: 1995. Manual For the Depression Anxiety & Stress Scales. [Google Scholar]
- Mak I.W.C., Chu C.M., Pan P.C., Yiu M.G.C., Chan V.L. Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry. 2009;31:318–326. doi: 10.1016/j.genhosppsych.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamelund S. Historical Influenza Pandemics: Lessons Learned. Copenhagen; Denmark: 2010. The Impact of Influenza on Mental Health in Norway, 1872-1929. [Google Scholar]
- Marlow, I., Hong, J., 2020. Hong Kong Police Arrest Protesters for Violating Social Distancing Guidelines [WWW Document]. Time. URLhttps://time.com/5835103/hong-kong-protesters-coronavirus-restrictions/(accessed 6.7.20).
- Matrajt L., Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg. Infect. Dis. 2020;26 doi: 10.3201/eid2608.201093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray C.J.L., Barber R.M., Foreman K.J., Ozgoren A.A., Abd-Allah F., Abera S.F., Aboyans V., Abraham J.P., Abubakar I., Abu-Raddad L.J., Abu-Rmeileh N.M., Achoki T., Ackerman I.N., Ademi Z., Adou A.K., Adsuar J.C., Afshin A., Agardh E.E., Alam S.S., Alasfoor D., Albittar M.I., Alegretti M.A., Alemu Z.A., Alfonso-Cristancho R., Alhabib S., Ali R., Alla F., Allebeck P., Almazroa M.A., Alsharif U., Alvarez E., Alvis-Guzman N., Amare A.T., Ameh E.A., Amini H., Ammar W., Anderson H.R., Anderson B.O., Antonio C.A.T., Anwari P., Arnlöv J., Arsenijevic V.S.A., Artaman A., Asghar R.J., Assadi R., Atkins L.S., Avila M.A., Awuah B., Bachman V.F., Badawi A., Bahit M.C., Balakrishnan K., Banerjee A., Barker-Collo S.L., Barquera S., Barregard L., Barrero L.H., Basu A., Basu S., Basulaiman M.O., Beardsley J., Bedi N., Beghi E., Bekele T., Bell M.L., Benjet C., Bennett D.A., Bensenor I.M., Benzian H., Bernabé E., Bertozzi-Villa A., Beyene T.J., Bhala N., Bhalla A., Bhutta Z.A., Bienhoff K., Bikbov B., Biryukov S., Blore J.D., Blosser C.D., Blyth F.M., Bohensky M.A., Bolliger I.W., Başara B.B., Bornstein N.M., Bose D., Boufous S., Bourne R.R.A., Boyers L.N., Brainin M., Brayne C.E., Brazinova A., Breitborde N.J.K., Brenner H., Briggs A.D., Brooks P.M., Brown J.C., Brugha T.S., Buchbinder R., Buckle G.C., Budke C.M., Bulchis A., Bulloch A.G., Campos-Nonato I.R., Carabin H., Carapetis J.R., Cárdenas R., Carpenter D.O., Caso V., Castañeda-Orjuela C.A., Castro R.E., Catalá-López F., Cavalleri F., Çavlin A., Chadha V.K., Chang J.C., Charlson F.J., Chen H., Chen W., Chiang P.P., Chimed-Ochir O., Chowdhury R., Christensen H., Christophi C.A., Cirillo M., Coates M.M., Coffeng L.E., Coggeshall M.S., Colistro V., Colquhoun S.M., Cooke G.S., Cooper C., Cooper L.T., Coppola L.M., Cortinovis M., Criqui M.H., Crump J.A., Cuevas-Nasu L., Danawi H., Dandona L., Dandona R., Dansereau E., Dargan P.I., Davey G., Davis A., Davitoiu D.V., Dayama A., De Leo D., Degenhardt L., Del Pozo-Cruz B., Dellavalle R.P., Deribe K., Derrett S., Des Jarlais D.C., Dessalegn M., Dharmaratne S.D., Dherani M.K., Diaz-Torné C., Dicker D., Ding E.L., Dokova K., Dorsey E.R., Driscoll T.R., Duan L., Duber H.C., Ebel B.E., Edmond K.M., Elshrek Y.M., Endres M., Ermakov S.P., Erskine H.E., Eshrati B., Esteghamati A., Estep K., Faraon E.J.A., Farzadfar F., Fay D.F., Feigin V.L., Felson D.T., Fereshtehnejad S.M., Fernandes J.G., Ferrari A.J., Fitzmaurice C., Flaxman A.D., Fleming T.D., Foigt N., Forouzanfar M.H., Fowkes F.G.R., Paleo U.F., Franklin R.C., Fürst T., Gabbe B., Gaffikin L., Gankpé F.G., Geleijnse J.M., Gessner B.D., Gething P., Gibney K.B., Giroud M., Giussani G., Dantes H.G., Gona P., González-Medina D., Gosselin R.A., Gotay C.C., Goto A., Gouda H.N., Graetz N., Gugnani H.C., Gupta Rahul, Gupta Rajeev, Gutiérrez R.A., Haagsma J., Hafezi-Nejad N., Hagan H., Halasa Y.A., Hamadeh R.R., Hamavid H., Hammami M., Hancock J., Hankey G.J., Hansen G.M., Hao Y., Harb H.L., Haro J.M., Havmoeller R., Hay S.I., Hay R.J., Heredia-Pi I.B., Heuton K.R., Heydarpour P., Higashi H., Hijar M., Hoek H.W., Hoffman H.J., Hosgood H.D., Hossain M., Hotez P.J., Hoy D.G., Hsairi M., Hu G., Huang C., Huang J.J., Husseini A., Huynh C., Iannarone M.L., Iburg K.M., Innos K., Inoue M., Islami F., Jacobsen K.H., Jarvis D.L., Jassal S.K., Jee S.H., Jeemon P., Jensen P.N., Jha V., Jiang G., Jiang Y., Jonas J.B., Juel K., Kan H., Karch A., Karema C.K., Karimkhani C., Karthikeyan G., Kassebaum N.J., Kaul A., Kawakami N., Kazanjan K., Kemp A.H., Kengne A.P., Keren A., Khader Y.S., Khalifa S.E.A., Khan E.A., Khan G., Khang Y.H., Kieling C., Kim D., Kim S., Kim Y., Kinfu Y., Kinge J.M., Kivipelto M., Knibbs L.D., Knudsen A.K., Kokubo Y., Kosen S., Krishnaswami S., Defo B.K., Bicer B.K., Kuipers E.J., Kulkarni C., Kulkarni V.S., Kumar G.A., Kyu H.H., Lai T., Lalloo R., Lallukka T., Lam H., Lan Q., Lansingh V.C., Larsson A., Lawrynowicz A.E.B., Leasher J.L., Leigh J., Leung R., Levitz C.E., Li B., Li Yichong, Li Yongmei, Lim S.S., Lind M., Lipshultz S.E., Liu S., Liu Y., Lloyd B.K., Lofgren K.T., Logroscino G., Looker K.J., Lortet-Tieulent J., Lotufo P.A., Lozano R., Lucas R.M., Lunevicius R., Lyons R.A., Ma S., Macintyre M.F., Mackay M.T., Majdan M., Malekzadeh R., Marcenes W., Margolis D.J., Margono C., Marzan M.B., Masci J.R., Mashal M.T., Matzopoulos R., Mayosi B.M., Mazorodze T.T., McGill N.W., McGrath J.J., McKee M., McLain A., Meaney P.A., Medina C., Mehndiratta M.M., Mekonnen W., Melaku Y.A., Meltzer M., Memish Z.A., Mensah G.A., Meretoja A., Mhimbira F.A., Micha R., Miller T.R., Mills E.J., Mitchell P.B., Mock C.N., Ibrahim N.M., Mohammad K.A., Mokdad A.H., Mola G.L.D., Monasta L., Hernandez J.C.M., Montico M., Montine T.J., Mooney M.D., Moore A.R., Moradi-Lakeh M., Moran A.E., Mori R., Moschandreas J., Moturi W.N., Moyer M.L., Mozaffarian D., Msemburi W.T., Mueller U.O., Mukaigawara M., Mullany E.C., Murdoch M.E., Murray J., Murthy K.S., Naghavi M., Naheed A., Naidoo K.S., Naldi L., Nand D., Nangia V., Narayan K.M.V., Nejjari C., Neupane S.P., Newton C.R., Ng M., Ngalesoni F.N., Nguyen G., Nisar M.I., Nolte S., Norheim O.F., Norman R.E., Norrving B., Nyakarahuka L., Oh I.H., Ohkubo T., Ohno S.L., Olusanya B.O., Opio J.N., Ortblad K., Ortiz A., Pain A.W., Pandian J.D., Panelo C.I.A., Papachristou C., Park E.K., Park J.H., Patten S.B., Patton G.C., Paul V.K., Pavlin B.I., Pearce N., Pereira D.M., Perez-Padilla R., Perez-Ruiz F., Perico N., Pervaiz A., Pesudovs K., Peterson C.B., Petzold M., Phillips M.R., Phillips B.K., Phillips D.E., Piel F.B., Plass D., Poenaru D., Polinder S., Pope D., Popova S., Poulton R.G., Pourmalek F., Prabhakaran D., Prasad N.M., Pullan R.L., Qato D.M., Quistberg D.A., Rafay A., Rahimi K., Rahman S.U., Raju M., Rana S.M., Razavi H., Reddy K.S., Refaat A., Remuzzi G., Resnikoff S., Ribeiro A.L., Richardson L., Richardus J.H., Roberts D.A., Rojas-Rueda D., Ronfani L., Roth G.A., Rothenbacher D., Rothstein D.H., Rowley J.T., Roy N., Ruhago G.M., Saeedi M.Y., Saha S., Sahraian M.A., Sampson U.K.A., Sanabria J.R., Sandar L., Santos I.S., Satpathy M., Sawhney M., Scarborough P., Schneider I.J., Schöttker B., Schumacher A.E., Schwebel D.C., Scott J.G., Seedat S., Sepanlou S.G., Serina P.T., Servan-Mori E.E., Shackelford K.A., Shaheen A., Shahraz S., Levy T.S., Shangguan S., She J., Sheikhbahaei S., Shi P., Shibuya K., Shinohara Y., Shiri R., Shishani K., Shiue I., Shrime M.G., Sigfusdottir I.D., Silberberg D.H., Simard E.P., Sindi S., Singh A., Singh J.A., Singh L., Skirbekk V., Slepak E.L., Sliwa K., Soneji S., Søreide K., Soshnikov S., Sposato L.A., Sreeramareddy C.T., Stanaway J.D., Stathopoulou V., Stein D.J., Stein M.B., Steiner C., Steiner T.J., Stevens A., Stewart A., Stovner L.J., Stroumpoulis K., Sunguya B.F., Swaminathan S., Swaroop M., Sykes B.L., Tabb K.M., Takahashi K., Tandon N., Tanne D., Tanner M., Tavakkoli M., Taylor H.R., Te Ao B.J., Tediosi F., Temesgen A.M., Templin T., Ten Have M., Tenkorang E.Y., Terkawi A.S., Thomson B., Thorne-Lyman A.L., Thrift A.G., Thurston G.D., Tillmann T., Tonelli M., Topouzis F., Toyoshima H., Traebert J., Tran B.X., Trillini M., Truelsen T., Tsilimbaris M., Tuzcu E.M., Uchendu U.S., Ukwaja K.N., Undurraga E.A., Uzun S.B., Van Brakel W.H., Van De Vijver S., Van Gool C.H., Van Os J., Vasankari T.J., Venketasubramanian N., Violante F.S., Vlassov V.V., Vollset S.E., Wagner G.R., Wagner J., Waller S.G., Wan X., Wang H., Wang J., Wang L., Warouw T.S., Weichenthal S., Weiderpass E., Weintraub R.G., Wenzhi W., Werdecker A., Westerman R., Whiteford H.A., Wilkinson J.D., Williams T.N., Wolfe C.D., Wolock T.M., Woolf A.D., Wulf S., Wurtz B., Xu G., Yan L.L., Yano Y., Ye P., Yentür G.K., Yip P., Yonemoto N., Yoon S.J., Younis M.Z., Yu C., Zaki M.E., Zhao Y., Zheng Y., Zonies D., Zou X., Salomon J.A., Lopez A.D., Vos T. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–2191. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni M.Y., Yao X.I., Leung K.S.M., Yau C., Leung C.M.C., Lun P., Flores F.P., Chang W.C., Cowling B.J., Leung G.M. Depression and post-traumatic stress during major social unrest in Hong Kong: a 10-year prospective cohort study. Lancet. 2020;395:273–284. doi: 10.1016/S0140-6736(19)33160-5. [DOI] [PubMed] [Google Scholar]
- Pang, J., 2020. Hong Kong police detain veteran democracy activists in raids [WWW Document]. Reuters. URL https://www.reuters.com/article/us-hongkong-protests-arrests/hong-kong-police-detain-veteran-democracy-activists-in-raids-idUSKBN2200AI (accessed 6.7.20).
- Radio Television Hong Kong, 2020. Hundreds of medical workers walk off in protest [WWW Document]. URLhttps://news.rthk.hk/rthk/en/component/k2/1506328-20200203.htm(accessed 6.7.20).
- Reuters, 2020. Timeline: key dates in Hong Kong's anti-government protests [WWW Document]. URL https://www.reuters.com/article/us-hongkong-protests-timeline/timeline-key-dates-in-hong-kongs-anti-government-protests-idUSKBN23608O(accessed 6.7.20).
- Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., Rossi A. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. open. 2020;3 doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D. UCLA loneliness scale (version 3): reliability,validity, and factor structure. J. Pers. Assess. 1996;66:20–40. doi: 10.1207/s15327752jpa6601. [DOI] [PubMed] [Google Scholar]
- Salomon J.A., Haagsma J.A., Davis A., de Noordhout C.M., Polinder S., Havelaar A.H., Cassini A., Devleesschauwer B., Kretzschmar M., Speybroeck N., Murray C.J.L., Vos T. Disability weights for the global burden of disease 2013 study. Lancet Glob. Heal. 2015;3:e712–e723. doi: 10.1016/S2214-109X(15)00069-8. [DOI] [PubMed] [Google Scholar]
- Shrira A., Hoffman Y., Bodner E., Palgi Y. COVID-19 related loneliness and psychiatric symptoms among older adults: the buffering role of subjective age. Am. J. Geriatr. Psychiatry. 2020 doi: 10.1016/j.jagp.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taouk Moussa, M., Lovibond, P.F., Laube, R., 2001. Psychometric properties of a chinese version of the 21-item depression anxiety stress scales (DASS21). Sydney, Australia. http://www2.psy.unsw.edu.au/dass/Chinese/Chinese&20DASS21&20Paper.pdf.
- TIME, 2019. Hong Kong Police Storm University Campus Occupied by Protesters as Courts Overturn Mask Ban [WWW Document]. URLhttps://time.com/5731365/hong-kong-polytechnic-university-siege/(accessed 6.7.20).
- Tsai J., Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Heal. 2020;5:e186–e187. doi: 10.1016/S2468-2667(20)30053-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtorta N.K., Kanaan M., Gilbody S., Ronzi S., Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102:1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vos T., Barber R.M., Bell B., Bertozzi-Villa A., Biryukov S., Bolliger I., Charlson F., Davis A., Degenhardt L., Dicker D., Duan L., Erskine H., Feigin V.L., Ferrari A.J., Fitzmaurice C., Fleming T., Graetz N., Guinovart C., Haagsma J., Hansen G.M., Hanson S.W., Heuton K.R., Higashi H., Kassebaum N., Kyu H., Laurie E., Liang X., Lofgren K., Lozano R., MacIntyre M.F., Moradi-Lakeh M., Naghavi M., Nguyen G., Odell S., Ortblad K., Roberts D.A., Roth G.A., Sandar L., Serina P.T., Stanaway J.D., Steiner C., Thomas B., Vollset S.E., Whiteford H., Wolock T.M., Ye P., Zhou M., Ãvila M.A., Aasvang G.M., Abbafati C., Ozgoren A.A., Abd-Allah F., Aziz M.I.A., Abera S.F., Aboyans V., Abraham J.P., Abraham B., Abubakar I., Abu-Raddad L.J., Abu-Rmeileh N.M., Aburto T.C., Achoki T., Ackerman I.N., Adelekan A., Ademi Z., Adou A.K., Adsuar J.C., Arnlov J., Agardh E.E., Al Khabouri M.J., Alam S.S., Alasfoor D., Albittar M.I., Alegretti M.A., Aleman A.V., Alemu Z.A., Alfonso-Cristancho R., Alhabib S., Ali R., Alla F., Allebeck P., Allen P.J., AlMazroa M.A., Alsharif U., Alvarez E., Alvis-Guzman N., Ameli O., Amini H., Ammar W., Anderson B.O., Anderson H.R., Antonio C.A.T., Anwari P., Apfel H., Arsenijevic V.S.A., Artaman A., Asghar R.J., Assadi R., Atkins L.S., Atkinson C., Badawi A., Bahit M.C., Bakfalouni T., Balakrishnan K., Balalla S., Banerjee A., Barker-Collo S.L., Barquera S., Barregard L., Barrero L.H., Basu S., Basu A., Baxter A., Beardsley J., Bedi N., Beghi E., Bekele T., Bell M.L., Benjet C., Bennett D.A., Bensenor I.M., Benzian H., Bernabe E., Beyene T.J., Bhala N., Bhalla A., Bhutta Z., Bienhoff K., Bikbov B., Abdulhak A.Bin, Blore J.D., Blyth F.M., Bohensky M.A., Basara B.B., Borges G., Bornstein N.M., Bose D., Boufous S., Bourne R.R., Boyers L.N., Brainin M., Brauer M., Brayne C.E., Brazinova A., Breitborde N.J., Brenner H., Briggs A.D., Brooks P.M., Brown J., Brugha T.S., Buchbinder R., Buckle G.C., Bukhman G., Bulloch A.G., Burch M., Burnett R., Cardenas R., Cabral N.L., Nonato I.R.C., Campuzano J.C., Carapetis J.R., Carpenter D.O., Caso V., Castaneda-Orjuela C.A., Catala-Lopez F., Chadha V.K., Chang J.-.C., Chen H., Chen W., Chiang P.P., Chimed-Ochir O., Chowdhury R., Christensen H., Christophi C.A., Chugh S.S., Cirillo M., Coggeshall M., Cohen A., Colistro V., Colquhoun S.M., Contreras A.G., Cooper L.T., Cooper C., Cooperrider K., Coresh J., Cortinovis M., Criqui M.H., Crump J.A., Cuevas-Nasu L., Dandona R., Dandona L., Dansereau E., Dantes H.G., Dargan P.I., Davey G., Davitoiu D.V., Dayama A., De la Cruz-Gongora V., de la Vega S.F., De Leo D., del Pozo-Cruz B., Dellavalle R.P., Deribe K., Derrett S., Des Jarlais D.C., Dessalegn M., DeVeber G.A., Dharmaratne S.D., Diaz-Torne C., Ding E.L., Dokova K., Dorsey E.R., Driscoll T.R., Duber H., Durrani A.M., Edmond K.M., Ellenbogen R.G., Endres M., Ermakov S.P., Eshrati B., Esteghamati A., Estep K., Fahimi S., Farzadfar F., Fay D.F., Felson D.T., Fereshtehnejad S.-.M., Fernandes J.G., Ferri C.P., Flaxman A., Foigt N., Foreman K.J., Fowkes F.G.R., Franklin R.C., Furst T., Futran N.D., Gabbe B.J., Gankpe F.G., Garcia-Guerra F.A., Geleijnse J.M., Gessner B.D., Gibney K.B., Gillum R.F., Ginawi I.A., Giroud M., Giussani G., Goenka S., Goginashvili K., Gona P., de Cosio T.G., Gosselin R.A., Gotay C.C., Goto A., Gouda H.N., Guerrant R., Gugnani H.C., Gunnell D., Gupta Rajeev, Gupta Rahul, Gutierrez R.A., Hafezi-Nejad N., Hagan H., Halasa Y., Hamadeh R.R., Hamavid H., Hammami M., Hankey G.J., Hao Y., Harb H.L., Haro J.M., Havmoeller R., Hay R.J., Hay S., Hedayati M.T., Pi I.B.H., Heydarpour P., Hijar M., Hoek H.W., Hoffman H.J., Hornberger J.C., Hosgood H.D., Hossain M., Hotez P.J., Hoy D.G., Hsairi M., Hu H., Hu G., Huang J.J., Huang C., Huiart L., Husseini A., Iannarone M., Iburg K.M., Innos K., Inoue M., Jacobsen K.H., Jassal S.K., Jeemon P., Jensen P.N., Jha V., Jiang G., Jiang Y., Jonas J.B., Joseph J., Juel K., Kan H., Karch A., Karimkhani C., Karthikeyan G., Katz R., Kaul A., Kawakami N., Kazi D.S., Kemp A.H., Kengne A.P., Khader Y.S., Khalifa S.E.A., Khan E.A., Khan G., Khang Y.-.H., Khonelidze I., Kieling C., Kim D., Kim S., Kimokoti R.W., Kinfu Y., Kinge J.M., Kissela B.M., Kivipelto M., Knibbs L., Knudsen A.K., Kokubo Y., Kosen S., Kramer A., Kravchenko M., Krishnamurthi R.V., Krishnaswami S., Defo B.K., Bicer B.K., Kuipers E.J., Kulkarni V.S., Kumar K., Kumar G.A., Kwan G.F., Lai T., Lalloo R., Lam H., Lan Q., Lansingh V.C., Larson H., Larsson A., Lawrynowicz A.E., Leasher J.L., Lee J.-.T., Leigh J., Leung R., Levi M., Li B., Li Yichong, Li Yongmei, Liang J., Lim S., Lin H.-.H., Lind M., Lindsay M.P., Lipshultz S.E., Liu S., Lloyd B.K., Ohno S.L., Logroscino G., Looker K.J., Lopez A.D., Lopez-Olmedo N., Lortet-Tieulent J., Lotufo P.A., Low N., Lucas R.M., Lunevicius R., Lyons R.A., Ma J., Ma S., Mackay M.T., Majdan M., Malekzadeh R., Mapoma C.C., Marcenes W., March L.M., Margono C., Marks G.B., Marzan M.B., Masci J.R., Mason-Jones A.J., Matzopoulos R.G., Mayosi B.M., Mazorodze T.T., McGill N.W., McGrath J.J., McKee M., McLain A., McMahon B.J., Meaney P.A., Mehndiratta M.M., Mejia-Rodriguez F., Mekonnen W., Melaku Y.A., Meltzer M., Memish Z.A., Mensah G., Meretoja A., Mhimbira F.A., Micha R., Miller T.R., Mills E.J., Mitchell P.B., Mock C.N., Moffitt T.E., Ibrahim N.M., Mohammad K.A., Mokdad A.H., Mola G.L., Monasta L., Montico M., Montine T.J., Moore A.R., Moran A.E., Morawska L., Mori R., Moschandreas J., Moturi W.N., Moyer M., Mozaffarian D., Mueller U.O., Mukaigawara M., Murdoch M.E., Murray J., Murthy K.S., Naghavi P., Nahas Z., Naheed A., Naidoo K.S., Naldi L., Nand D., Nangia V., Narayan K.M.V., Nash D., Nejjari C., Neupane S.P., Newman L.M., Newton C.R., Ng M., Ngalesoni F.N., Nhung N.T., Nisar M.I., Nolte S., Norheim O.F., Norman R.E., Norrving B., Nyakarahuka L., Oh I.H., Ohkubo T., Omer S.B., Opio J.N., Ortiz A., Pandian J.D., Panelo C.I.A., Papachristou C., Park E.-.K., Parry C.D., Caicedo A.J.P., Patten S.B., Paul V.K., Pavlin B.I., Pearce N., Pedraza L.S., Pellegrini C.A., Pereira D.M., Perez-Ruiz F.P., Perico N., Pervaiz A., Pesudovs K., Peterson C.B., Petzold M., Phillips M.R., Phillips D., Phillips B., Piel F.B., Plass D., Poenaru D., Polanczyk G.V., Polinder S., Pope C.A., Popova S., Poulton R.G., Pourmalek F., Prabhakaran D., Prasad N.M., Qato D., Quistberg D.A., Rafay A., Rahimi K., Rahimi-Movaghar V., Rahman S.ur, Raju M., Rakovac I., Rana S.M., Razavi H., Refaat A., Rehm J., Remuzzi G., Resnikoff S., Ribeiro A.L., Riccio P.M., Richardson L., Richardus J.H., Riederer A.M., Robinson M., Roca A., Rodriguez A., Rojas-Rueda D., Ronfani L., Rothenbacher D., Roy N., Ruhago G.M., Sabin N., Sacco R.L., Ksoreide K., Saha S., Sahathevan R., Sahraian M.A., Sampson U., Sanabria J.R., Sanchez-Riera L., Santos I.S., Satpathy M., Saunders J.E., Sawhney M., Saylan M.I., Scarborough P., Schoettker B., Schneider I.J., Schwebel D.C., Scott J.G., Seedat S., Sepanlou S.G., Serdar B., Servan-Mori E.E., Shackelford K., Shaheen A., Shahraz S., Levy T.S., Shangguan S., She J., Sheikhbahaei S., Shepard D.S., Shi P., Shibuya K., Shinohara Y., Shiri R., Shishani K., Shiue I., Shrime M.G., Sigfusdottir I.D., Silberberg D.H., Simard E.P., Sindi S., Singh J.A., Singh L., Skirbekk V., Sliwa K., Soljak M., Soneji S., Soshnikov S.S., Speyer P., Sposato L.A., Sreeramareddy C.T., Stoeckl H., Stathopoulou V.K., Steckling N., Stein M.B., Stein D.J., Steiner T.J., Stewart A., Stork E., Stovner L.J., Stroumpoulis K., Sturua L., Sunguya B.F., Swaroop M., Sykes B.L., Tabb K.M., Takahashi K., Tan F., Tandon N., Tanne D., Tanner M., Tavakkoli M., Taylor H.R., Te Ao B.J., Temesgen A.M., Have M.Ten, Tenkorang E.Y., Terkawi A.S., Theadom A.M., Thomas E., Thorne-Lyman A.L., Thrift A.G., Tleyjeh I.M., Tonelli M., Topouzis F., Towbin J.A., Toyoshima H., Traebert J., Tran B.X., Trasande L., Trillini M., Truelsen T., Trujillo U., Tsilimbaris M., Tuzcu E.M., Ukwaja K.N., Undurraga E.A., Uzun S.B., van Brakel W.H., van de Vijver S., Dingenen R.Van, van Gool C.H., Varakin Y.Y., Vasankari T.J., Vavilala M.S., Veerman L.J., Velasquez-Melendez G., Venketasubramanian N., Vijayakumar L., Villalpando S., Violante F.S., Vlassov V.V., Waller S., Wallin M.T., Wan X., Wang L., Wang J., Wang Y., Warouw T.S., Weichenthal S., Weiderpass E., Weintraub R.G., Werdecker A., Wessells K.R.R., Westerman R., Wilkinson J.D., Williams H.C., Williams T.N., Woldeyohannes S.M., Wolfe C.D.A, Wong J.Q., Wong H., Woolf A.D., Wright J.L., Wurtz B., Xu G., Yang G., Yano Y., Yenesew M.A., Yentur G.K., Yip P., Yonemoto N., Yoon S.-.J., Younis M., Yu C., Kim K.Y., Zaki M.E.S., Zhang Y., Zhao Z., Zhao Y., Zhu J., Zonies D., Zunt J.R., Salomon J.A., Murray C.J. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman I.M. The impact of epidemic, war, prohibition and media on suicide: United States, 1910-1920. Suicide Life Threat Behav. 1992;22:240‐254. [PubMed] [Google Scholar]
- Yao H., Chen J.-.H., Xu Y.-.F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.