Highlights
-
•
No data are available to the distress of infertile couples during COVID-19.
-
•
Stop performing ART treatments during COVID-19 contributed to increase anxiety.
-
•
The psychological impact was more severe for women than for men.
-
•
Psychological impact of COVID-19 in infertility couple should not be underestimated.
Keywords: Anxiety, COVID-19, Distress, Infertility, Pandemic, Psychological impact
Abstract
Objective(s)
to evaluate the impact of the COVID-19 pandemic on infertile couples’ emotions, anxiety and future plans.
Study design
An observational study was perfomed by Italian ART centers and online forums. In this study, infertile couples candidate to ART and whose treatment was blocked due to the COVID-19 lockdown were enrolled through an online survey. The psychological impact of COVID-19 was measured by Impact of Event Scale-Revised (IES-R) and by a short form of the Spielberger State-Trait Anxiety Inventory (STAI); Self-perceived anxiety related either to pregnancy safety and to economic crisis measured by VAS scale.
Results
627 patients completed the survey. The COVID-19 lock-down had a moderate/severe psychological impact on infertile patients (mean IES-R score 36.4 ± 16.6). The mean STAI score was 49.8 ± 15.3, with an overall incidence of STAI > 36 of 71 %. The mean VAS scale for anxiety perception was 45.3 ± 15.3. Women were more emotionally distressed, anxious and depressed than men (36.8 ± 16.4 vs 31.0 ± 18.4 for IES-R, respectively; p = 0.03). Notwithstanding the uncertainty about pregnancy safety, 64.6 % of respondents chose to maintain their reproductive programme. Economic crisis induced 11.5 % of the surveyed patients to give up their ART program. Respondents who had at least one relative affected by COVID-19 had a significantly higher IES-R score and anxiety VAS, but not higher STAI scores, than patients belonging to unaffected families.
Conclusion(s)
COVID-19 pandemic itself and the recommendation to stop ART program generated higher distress levels in infertile couples. The psychological impact of COVID-19 pandemic in infertility patients should not be underestimated, and a specific psychological support should be planned.
Introduction
The disease caused by coronavirus (SARS-CoV-2) was named Coronavirus Disease 19 (COVID-19) by World Health Organization, who classified COVID-19 as pandemic, global public health emergency [1]. COVID-19 was first reported in Wuhan (China) in December 2019 and was suddenly followed by an outbreak across Hubei Province and other parts of the country [1,2]. The first two cases of COVID-19 in Italy were confirmed in January 2020 in Chinese tourists, and the first case of secondary transmission occurred in Codogno, close to Milan, in February [3].
The SARS-Cov-2 is a novel beta coronavirus: enveloped, non-segmented, positive-sense RNA virus to the Coronaviridae family and to the Nidovirales order, broadly spread in humans and other mammals. COVID-19 is characterized by a high infectivity and multiple possible transmission routes, among which respiratory droplet transmission is the most common, as indicated by the typical respiratory symptoms [[4], [5], [6]].
COVID-19 caused in Italy several clusters of patients with pneumonia and severe acute respiratory syndrome and was sometimes associated with unfavourable outcome. Lockdown measures adopted to limit the spread of COVID-19 pandemic all over the world imposed a challenge to psychological resilience. An online survey conducted in China on 1210 respondents showed that 53.8 % rated the psychological impact of the outbreak as moderate or severe and 28.8 % reported moderate to severe anxiety symptoms [7].
Nowadays, concern is rising on the impact of COVID-19 on pregnancy and on the possible vertical transmission; most available data suggest that the clinical course of the infection in pregnancy is similar to that in non-pregnant patients [8]. The risk of an increased incidence of preterm birth with occasional unfavourable perinatal COVID-19 disease was reported, but most series showed reassuring neonatal outcomes [9].During the current COVID-19, the most important Reproductive Medicine Societies advised to stop the start of new Assisted Reproductive Treatments (ART) in order to avoid the strain on healthcare system. For some patients the indefinite postponement of ART could lead to a to an irremediable worsening of reproductive prognosis.
The emotional reaction to infertility is conditioned by personality, health perception, cognitive appraisal and social support [10]. Currently, there is poor knowledge on the psychological health of infertile couples during the COVID-19 outbreak, and no data are available about Italian population, the first in Europe to be involved by the disease. The current study was aimed to investigate some psychological aspects of infertile couples waiting for ART in order to better understand their level of psychological distress and anxiety during the COVID-19 lockdown.
Materials and methods
This observational study was planned to assess the extent of the emotional impact of COVID-19 pandemic on infertile patients, assessing the effect of uncertainty about pregnancy safety and of economic crisis on their reproductive plans. The study was approved by the regional ethical committee on April 16, 2020 (protocol n. 111/2020).
A previously validated survey with 40 questions was published using the SurveyMonkey platform (https://it.surveymonkey.com/r/SPNTPB5) and was administered to infertility patients waiting for Intrauterine Insemination (IUI) or In Vitro Fertilization (IVF) in three public Italian ART Units, sited in Catanzaro, Naples and Turin. Patients were invited by a standardized email, in which it was exposed the aim of the survey. Patient emails were retrieved from the lists available to the three centers, in particular from the waiting lists registers. All three centers collected the mailing list and the addresses were uploaded to the “surveymonkey” site server, so that the emails were automatically sent to all the addresses simultaneously. At least one email was sent for each invited couple, and when available, both the female and male partners were contacted. The automatic system sent a second email if the questionnaire was not completed five days after the first invitation.
The survey weblink was also published on six online forums frequented by infertile patients scheduled for ART cycles in other Italian ART Centres, who were free to join it.
Data were collected anonymously; they included demographic characteristics of the respondents such as age, sex, city of residence and duration of infertility. Respondents were also asked if themselves or any of their relatives, colleagues or friends had been affected by the COVID-19 infection or have died for it.
Validated questionnaires were used to assess the psychological impact.
Psychological impact questionnaire
The psychological impact of COVID-19 was measured using the Italian version of the Impact of Event Scale-Revised (IES-R), a 22-item questionnaire (Table 1 ) assessing subjective distress caused by traumatic events [11]. Respondents were asked to indicate how much they were distressed or bothered during the past seven days by this specific stressful life event. To cope with the specific aims of this study, the perception of the stressful event was expanded to the last 30 days (instead of 7), a time period more appropriate to capture the mood of patients throughout the lockdown. The IES-R provided a total score (ranging from 0 to 88) composed of three subscores, respectively measuring the Intrusion, Avoidance and Hyperarousal subscales. Each item was rated on a 5-point scale ranging from 0 ("not at all") to 4 ("extremely"). The higher the score, the higher the psychological impact. The psychological impact according to the total IES-R score was categorized as normal (0–23), mild (24–32), moderate (33–36), and severe (>37) [11].
Table 1.
IES-R questions.
| Questions: |
|
Anxiety questionnaire
Anxiety was measured using the Italian version of the 6-item short form of the Spielberger State-Trait Anxiety Inventory scale (STAI) and the visual analogue scale for anxiety (VAS).
STAI is a self-administered test designed to assess levels of state anxiety by using quantitative adjectives scored by a Likert-scale. Respondents were asked to state if they “never”, “sometimes”, “often” or “almost always” felt “calm”, “tense and restless”, “sad”, “relaxed”, “happy” or “worried” during their last 30 days. Accordingly, patients were scored on a scale (20–80) where higher scores were associated with higher anxiety levels. A STAI score of 34–36 was considered normal [12].
Patients were also asked about the will to continue the reproductive program and about the self-perceived anxiety (a) when thinking of getting pregnant during the COVID-19 pandemic, given the unknown effects of the virus on the fetus, and (b) when considering the economic effects of the COVID-19 pandemic; the Visual Analogue Scale (VAS) was used to answer [13].
Statistical calculation
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) v. 19.0 (IBM Inc), showing data as mean plus/minus SD or as percentage. Descriptive statistics were calculated for sociodemographic characteristics. The questionnaire scores were expressed as mean plus/minus SD, and after assessing the normal distribution of data, they were analyzed using the T-test or the One-way ANOVA; they were also analysed subgrouping patients according to sex, length of infertility, city of provenience, experience of infection of the respondent or of his/her relatives. Univariate comparison of dichotomous data was performed using the Chi-square test with continuity correction.
A two-sided P value lower than 0.05 was considered significant.
Results
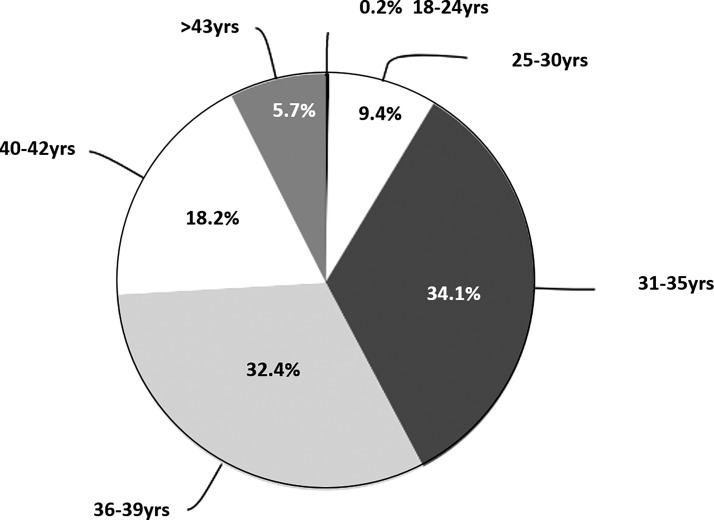
During the study period, 825 patients were recruited by email invitation by the three promoting Centers and other 671 joined the survey online via ART forums. A total number of 627 patients (498 recluted directly, 173 via forum link) agreed to complete the survey (response rate 41.9 %). Among respondents, 588 (93.8 %) were woman, and 66.5 % were aged 31–39 (Fig. 1). Four hundred and eight respondents (65.2 %) lived in Southern Italy, 37 (5.9 %) in Central Italy and 181 (28.9 %) in Northern Italy, with one patient not reporting her living place.
Fig. 1.
Age distributions of respondents. Patients were distributed in 6 classes according to their age (18-24, 25-30, 31-35, 36-39, 40-42 and over 43 years old), with most of respondents aged 31-39 years.
Most respondents had infertility history longer than 2 years (477 patients, 76.1 %), whereas 28 had <1 year infertility (4.5 %). Only 2 out of 627 of the patients (0.3 %) had been infected by COVID-19, but 55 had at least one infected relative (8.8 %), and 39 (6.2 %) had experienced the loss of one relative, friend or colleague due to COVID-19. As expected, 72.7 % and 59 % of those with at least one relative or friend infected and/or dead, respectively, came from Northern Italy, where the outbreak was more severe.
The COVID-19 pandemic had a moderate/severe psychological impact on infertile patients, with a mean IES-R score of 36.4 ± 16.6. More than half of the respondents (64 %) rated the psychological impact as severe; on the average, women appeared to be more emotionally distressed, anxious and depressed than men (36.8 ± 16.4 vs 31.0 ± 18.4, respectively; p = 0.03).
The mean STAI questionnaire score was 49.8 ± 15.3, with 71 % overall incidence of STAI > 36. Within women, the mean score was 51.2 ± 14.6, with 72.2 % overall incidence of STAI > 36; within men the mean score was 45 ± 11.6, 61.1 % having STAI > 36.
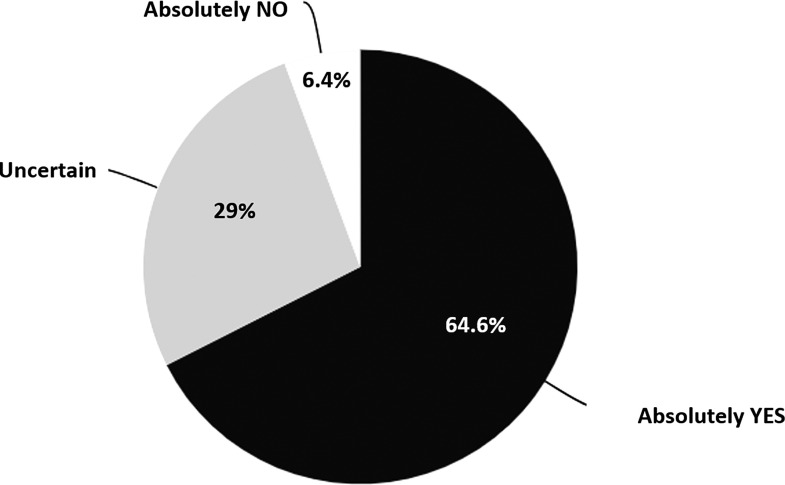
The mean score of VAS-anxiety regarding the idea of getting pregnant during COVID-19 pandemic despite the unknown effects on the fetus was 45.5 ± 30.6 for women, with 54.5 % overall incidence of score >50; within men it was 42.2 ± 30.5, with 38.5 % overall incidence of score >50. Therefore, despite the uncertainty about pregnancy safety, 64.6 % of respondents expressed the will to maintain their reproductive programme, 29 % declared to be uncertain, and only 6.4 % preferred to postpone any attempt (Fig. 2 ).
Fig. 2.
Respondents willing to start ART cycle. Despite the lack of data on pregnancy safety during COVID-19, 64.6 % of patients want to maintain their reproductive programme, while 6.4 % prefer to postpone any attempt, waiting for more evidence.
Regarding the idea of getting pregnant during the economic crisis linked to COVID-19 pandemic, the mean VAS-anxiety score was 35.8 ± 28.8 for women, with 39 % overall incidence of score >50; within men it was 28.4 ± 35.1, with 21.6 % overall incidence of score >50. Overall, economic issues discouraged ART attempts just in 11.5 % of surveyed patients, whereas in most of them, they did not influence reproductive program.
As expected, respondents who had at least one relative affected by COVID-19 showed significantly higher IES-R score (42.5 ± 16.6 vs. 35.8 ± 16.5; p = 0.004) and anxiety VAS (59.3 ± 27.8 vs. 43.9 ± 30.5; p = 0.001), but comparable STAI scores vs. patients with no affected relatives. The death of a relative, friend or colleague did not statistically increase any of the IES-R, STAI or VAS score for anxiety. No sub-analysis was possible among patients who were personally infected by the virus, given their small number.
No significant differences were observed in the sub-analysis for Italian region, with comparable results in Northern and Southern Italy for IES-R (37.2 ± 17.2 vs. 34.7 ± 15.9, respectively; p = 0.14), STAI (48.2 ± 18.3 vs. 47.7 ± 17.2, respectively; p = 0.15) and VAS score for anxiety (45.1 ± 28.4 versus 45.3 ± 31.0, respectively; p = 0.24).
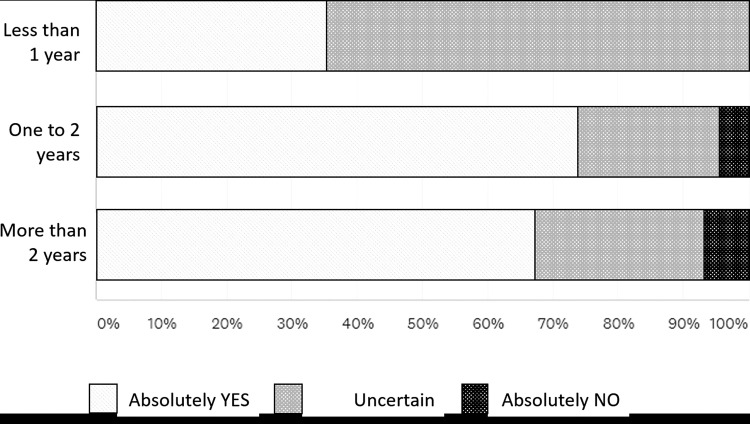
Differently, infertility duration inversely affected the percentage of patients with uncertain will to start ART treatment without evidence of safety, as it was 64.3 %, 21.8 % and 26.2 %, respectively, in patients infertile from less than 1 year, from 1 to 2 years and from more than 2 years (Fig. 3 ).
Fig. 3.
Length of infertility and willing to start ART cycle. Respondents with longer history of infertility are more willing to take the risks of getting pregnant during COVID-19 pandemic than infertile patients since less than 1 year.
Discussion
Principal findings
COVID-19 pandemic was a sudden event with relevant emotional consequences, able to aggravate the psychological status of infertile patients, particularly on women with advanced reproductive age or diminished ovarian reserve [14].
Moreover, 11 % of patients considered themselves suddently unable to start their family project for financial problems caused by COVID-19.
Results of the study in the context of what is know
The high number of infected subjects and the relatively high mortality in Northern Italy obliged authorities to impose restrictive measures to the entire nation for more than 2 months in order to contain the spread of the infection. Italian government ordered the suspension of non-urgent medical care and elective procedures, such as ART, in order to avoid any possible access to Intensive Care Units (ICU) due to ART complications, allowing to perform only urgent procedures, such as fertility preservation for cancer patients. Similar recommendations were also issued by American Society for Reproductive Medicine (ASRM), that recommended to suspend all embryo transfers, whether fresh or frozen [15].
Isolation, social distancing and radical changes in daily life might have increased the risk of depression among vulnerable subjects, such as infertile patients. A study published by the Engage Minds Hub Research Group (Catholic University of Milan) claimed that at least one third of the Italian population will suffer in the near future from a psychological state defined “alert state”: these people will act in an inappropriate way in relation to the healthcare system because of the fear of COVID-19 [16]. To date, while some interesting data are available on pregnant women reactions and perception to the pandemic [17], nobody investigated the intensity of the “alert state” in infertile patients. In our opinion it is of paramount importance to assess the psychological impact of the COVID-19 outbreak on infertile population.
Our survey, the largest published on the topic up to now, clearly demonstrated that the COVID-19 pandemic had a moderate/severe psychological impact on Italian infertile patients, with an overall incidence of 75 % and 71 % of IES-R and STAI scores. Although the low response rate of the male partners, according to our results women can be presumed to be more emotionally distressed, anxious and depressed than men; this was also suggested by the rate of respondents, significantly higher for women, since often the subjects who are most emotionally involved participate with more interest in the interviews. Almost 40 % of surveyed women and 21 % of men reported high anxiety (assessed as VAS for anxiety >50) related to the idea of having a pregnancy during the COVID-19 pandemic because of the largely unknown effects on the fetus [6,18,19]. However, despite the uncertainty about pregnancy safety, 64.6 % of the respondents chose to maintain their reproductive program.
The impact of economic issues on the decision of changing reproductive programs was limited, as only 11 % of the couples declared to be so worried about economic situation to give up. However, considering that 498 out of 627 (79.4 %) of the respondents were in the waiting list of a public ART Unit, where treatments are almost completely reimbursed, an overall proportion of 11 % of patients who considered themselves suddently unable to start their family project for financial problems can be considered a significant impact.
Research and clinical implication
As expected, in our study, having at least one relative affected by COVID-19 infection had a significant impact in originating higher IES-R score and anxiety; the death of a relative, friend or colleague, on the contrary, did not apparently increase any of the questionnaires, possibly because of the smaller number of observations. Interestingly, there was no significant difference in any score between Northern areas, more severely affected by the epidemic, and Southern regions. This could suggest that infertility per se is associated with psychological consequences that are poorly affected by external events unless these events involve the more intimate family life. Moreover the percentage of uncertainty about pregnancy safety, was significantly higher among patients whose infertility duration was shorter, while patients with more than 1 year of infertility were more likely to take the risk and start to achieve pregnancy. This aspect may be included in the evaluations regarding how to re-start our programs, since many Centers are now evaluating the possibility to modify their waiting lists to give preference to couples with advanced maternal age or those close to the cut-off age decided by the Regions to access healthcare reimbursed by the National Health System.
Strengths and limitations of the study
Although this is the largest investigation published on the topic up to now, there are two main limitations of this study. First we cannot exclude a selection bias: patients with the most definite opinions joined the survey, those with more uncertain ideas skipped it; as a consequence, we cannot be sure that what observed is an accurate picture of the world of Italian infertile couples.
In particular, we must recognize that the objective of verifying the impact of COVID-19 on a national scale may have been limited by the considerable different incidence of SARS-CoV-2 infection in the various Italian regions. A seroprevalence study reports a cumulative COVID-19 incidence of about 10 % in women at the first trimester of pregnancy in S. Anna Hospital, Turin, one of the centers involved in the present study [20]: in this center, the rate of adhesion was higher (87.3 %, n.83/95). The reduced response rates in the centers of Southern Italy can be caused by a lower diffusion of COVID-19 in this region: the couples experienced the emergency with a different awareness that may have conditioned their willingness to submit to the questionnaire. While the adhesion rate may have been influenced by the perception of the spread of COVID-19 by specific region, we believe that the psychologic impact related to the suspension of ART treatments was common for all patients. Therefore, we believe that our analysis remains realistic.
Second, 93.8 % of our study population were women, and we can not compare their emotional status with that of their male counterparts.
Conclusion
In our study the need to stop performing ART treatments during the COVID-19 pandemic contributed to increase emotional distress and anxiety in infertile couples. The strong psychological impact was severe expecially for women, for couples with longer infertility history, and for those whose family hade an infected member. Nevertheless, approximately two thirds of patients waiting for ART expressed the will to proceed with their treatment, even if no conclusive data on the safety of the COVID-19 infection across conception and during pregnancy are available yet. Overall, we can state that the psychological consequences of COVID-19 pandemic on infertile patients should not be underestimated, and a specific psychological support should be planned.
Financial support
No specific funding was received for this study.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salute.gov.it [Internet]. Italia: Ministero della salute; c2020 [cited 2020 Apr 25]. Covid-19 - Situazione in Italia. Available from: http://www.salute.gov.it/portale/nuovocoronavirus.
- 4.Wang W., Xu Y., Gao R. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carosso A., Cosma S., Borella F. Pre-labor anorectal swab for SARS-CoV-2 in COVID-19 patients: is it time to think about it? Eur J Obstet Gynecol Reprod Biol. 2020;249:98–99. doi: 10.1016/j.ejogrb.2020.04.023. Apr 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong L., Tian J., He S. Possible Vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323(18):1846–1848. doi: 10.1001/jama.2020.4621. Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C., Pan R., Wan X. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. March 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Breslin N., Baptiste C., Gyamfi-Bannerman C. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. 2020;2(2) doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yan J., Guo J., Fan C. Coronavirus disease 2019 (COVID-19) in pregnant women: a report based on 116 cases. Am J ObstetGynecol. 2020 doi: 10.1016/j.ajog.2020.04.014. Apr 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel A., Sharma P.S.V.N., Kumar P., Binu V.S. Illness cognitions, anxiety, and depression in men and women undergoing fertility treatments: a dyadic approach. J Hum Reprod Sci. 2018;11:180–189. doi: 10.4103/jhrs.JHRS_119_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Creamer M., Bell R., Failla S. Psychometric properties of the impact of event scale-revised. Behav Res Ther. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 12.Marteau T.M., Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI) Br J Clin Psychol. 1992;31:301–306. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 13.Williams V.S., Morlock R.J., Feltner D. Psychometric evaluation of a visual analog scale for the assessment of anxiety. Health Qual Life Outcomes. 2010;8:57. doi: 10.1186/1477-7525-8-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turocy J.M., Robles A., Hercz D., D’Alton M., Forman E.J., Williams Z. The emotional impact of the ASRM guidelines on fertility patients during the COVID-19 pandemic. Fertil Steril. 2020 Apr 14. [Google Scholar]
- 15.American Society for Reproductive Medicine. Patient Management and Clinical Recommendations during the Coronavirus (COVID-19) Pandemic. Available at https://www.asrm.org/news-and-publications/covid-19/statements/patient-management-and-clinical-recommendations-during-the-coronavirus-covid-19-pandemic. (Accessed on 27 March 2020).
- 16.L’Angiocola P.D. Monti M. COVID-19: the critical balance between appropriate governmental restrictions and expected economic, psychological and social consequences in Italy. Are we goin in the right direction? Acta Biomed. 2020;91(2):35–38. doi: 10.23750/abm.v91i2.9575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saccone G., Florio A., Aiello F., Venturella R., De Angelis M.C., Locci M. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol. 2020;223(2):293–295. doi: 10.1016/j.ajog.2020.05.003. Aug. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen H., Guo J., Wang C. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fan C., Lei D., Fang C. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa226. March 17; ciaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cosma S., Borella F., Carosso A. The "scar" of a pandemic: cumulative incidence of COVID-19 during the first trimester of pregnancy. J Med Virol. 2020 doi: 10.1002/jmv.26267. Jul 7. [DOI] [PMC free article] [PubMed] [Google Scholar]