Abstract
Background
Self-medication with antibiotics (SMA) is a global problem. This extends to medication of under-fives by their parents. In particular, there is currently insufficient information for this problem.
Purpose
To determine the proportion and factors associated with medication of under-fives with antibiotics by their parents.
Materials and Methods
A cross-sectional study among parents/caregivers of under-fives in 30 hamlets/streets of Bagamoyo District Council, in Tanzania was conducted between July and August, 2019. Respondents were the under-fives’ parents/caregivers aged at least 18 years selected from households using probability proportional to a size cluster-sampling method. Respondents were required to report whether or not the under-fives had been unwell within the past 12 months and to describe the type or specific name of any medicine administered to their child. We used descriptive and analytical procedures to analyze the data.
Results
The study included 730 parents/caregivers of under-fives. Their mean age was 32.2 (SD=7.4) years. The majority 668 (91.5%) were biological mothers and 574 (78.6%) having completed primary education. The proportion of parental SMA to under-fives was 47.7% (95% CI=43.7, 51.8). Knowledge on the appropriate use of antibiotics among parents was low. The most commonly used antibiotic was amoxicillin, 181 (62.0%). Independent factors associated with parental SMA to under-fives were average household income, distance to the nearest health facility, knowledge about use of antibiotics and the parent/caregiver’s awareness of prescription-only medicines (POMs).
Conclusion
Since the prevalence of SMA by parents to under-fives in Bagamoyo District is high, there is a need for health systems to enhance those measures that would control the sale of antibiotics without prescriptions. In addition, more than half of all study participants have a minimal understanding of the use of antibiotics and are unaware of POMs. Findings indicate a need to have routine continuous health education at the community level about the use of antibiotics.
Keywords: antibiotics, parent, self-medication, under-fives, Tanzania
Introduction
Self-medication with antibiotics (SMA) to treat self-diagnosed disorders or symptoms, or the intermittent or continued use of prescribed antibiotics for chronic or recurrent disease or symptoms, is not appropriate.1,2 Although general reasons for self-medicating are diverse, in some sub-Saharan African countries, reasons for SMA mostly include health system challenges such as the unavailability of qualified personnel and deficiencies in diagnostic capability. At the individual level, motives for SMA include lack of time, money and perceptions of illness being too minor to seek medical attention.3–5
The main consequences of SMA are the emergence of multi-drug resistant pathogens, treatment failure, wastage of medical resources and drug dependency.6–9 Globally, and more specifically in less developed countries like Tanzania, antimicrobial resistance is of significant public health importance.10,11 In Tanzania, antibiotics are prescription-only medicines (POMs).12 However, their availability and ease of accessibility in drug stores without prescriptions promote a higher incidence of SMA.13 The available literature indicates that, since under-fives are more susceptible to the common respiratory and urinary tract infections, and diarrhoeal diseases than adults, it is more likely that the under-fives will be given antibiotics than other medications.14
There have reports of SMA to under-fives in some sub-Saharan counties like Cameroon and Namibia; with prevalence ranging between 50% and 60%.3,15 Chipwaza et al found that parents in most rural Tanzanian communities practice self-medication of under-fives.16 For example, almost 60% of heads of households from a rural area in Kilimanjaro Region in Northeastern Tanzania, reported self-medication with antibiotics.17 Furthermore, a recent study from the same region reported close to 30% of parents administered antibiotics to their under-fives from leftover supplies or without prescription.18
Evidence has accumulated concerning SMA in different sub-Saharan African countries and for different populations.3,17,19,20 Among those studies addressing antibiotic self-medication, few have covered parents self-medicating their under-fives. Since children are at an increased risk of succumbing to infectious diseases because of their relatively less developed immune systems,21 they are more prone to SMA. Hence the aim of this study was to determine the proportion of parents that self-medicate their children under-five with antibiotics and to determine those factors associated with this practice in Bagamoyo District, Tanzania. Based on the results of this study, we determined that there is a need to introduce measures to educate parents/caregivers in SMA and the use of antibiotics without prescription with the aim of reducing the prevalence of this practice.
Materials and Methods
Study Design and Setting
We conducted a cross-sectional study between July and August, 2019 in Bagamoyo District. The district is semi-urban and one of nine districts comprising Pwani Region in Tanzania. It borders the Indian Ocean and has 11 wards, 8 villages and 174 hamlets. The district has 19 government health facilities and 6 private health facilities. It has 99 registered Accredited Drug Dispensing Outlet shops and 6 pharmacies.
Study Population
Eligible study participants were the parents or caregivers of under-five year old children in the selected households. Respondents were either the biological mother or father to the under-five or when not present, any person aged at least 18 years that had been responsible for the child and their daily care, protection and support for a period of at least two years leading up to the study. After the interview, we were able to establish whether or not the person was the parent or a caregiver.
Sample Size and Sampling Procedure
The participant pool comprised 738 individuals. This sample size was calculated based on the formula: n = Z2p(1-p)/E2, where Z corresponds to the critical value of the normal distribution for a 95% confidence level,22 p is a 60% estimate of the population practicing SMA16 and 5% for E, an estimated margin of error around p. We also adjusted for possible sampling errors within the clusters by the design effect of 2.
We used a two-stage cluster sampling method to select eligible study participant. The 174 clusters comprised hamlets or streets in semi-urban or urban settings. In the first stage of the study, we randomly selected 30 clusters from the list. In the second stage, we included all households with under-fives within the selected clusters. Using these lists of households, we applied systematic sampling to select 27 households. In case a household had more than one under-five, we randomly selected only one of the under-fives. This process provided the highest number of study participants with compensation for the approximately 10% of eligible respondents in households unavailable at the time of conducting interviews and for those participants who would not consent to being interviewed.
Data Collection Instruments
Data were collected using structured interviews with both closed and open-ended questions. These included questions on demographics, self-medication practices and interviewees’ knowledge of antibiotic use. The interview tool was initially prepared in English and then translated into Kiswahili, the language common to everyone in Tanzania. We pre-tested the interview-form among 30 parents or caregiver in one of the streets that were not earmarked for inclusion in the study: this provided for improvements to the clarity and comprehension thus enhancing the validity of this tool. The interview included three sections: section one comprised questions on the socio-demographic characteristics of the parent or caregiver of the child. The second section included structured and semi-structured questions about each under-five’s recent illnesses and use of antibiotics. The third section included questions about knowledge of the use of antibiotics and consisted mainly or responses requiring a “yes,” “no,” or “I don’t know.” Research assistants were four trained registered nurses experienced in health-related research.
Measures
The study dependent variable was the parental antibiotic medication to the under-five age group children. Each parent/caregiver was asked whether or not their child had been unwell during the 12 months prior to the survey, the type or names of the medication if applicable and the source(s) of the medicines. If antibiotics were mentioned or implied, the parent or caregiver was shown examples of antibiotics commonly used to treat under-five age children in order to identify the medication, and the parent/caregiver would confirm the medication name and how it had been administered. Parents/caregivers were asked 10 questions to assess their knowledge on the use of antibiotics. Of the other questions, two covered drug identification, two related to the use of antibiotics, three covered knowledge of possible side effects and three questions reported on drug resistance. We did not use a standard tool for assessing knowledge; nevertheless, we were able to benchmark the knowledge questions with other studies, to consider the study population, and to consult with a pharmacist and a pediatrician so as to enhance the quality of the assessment section.
Data Processing and Analysis
During data processing, to derive a composite knowledge score, a respondent scored two points for each correct answer and zero for other responses. A knowledge scale variable had possible values ranging between 0 and 20; 0 implying no knowledge at all. A respondent’s level of knowledge was categorized as low when the score was below an average of seven points, average with score between seven and 13 and high when scoring above 13 points. The reliability of responses was assessed based on Cronbach’s alpha score and overall found to be moderate (reliability, α=0.64).
The main data analyses were both descriptive and analytical. We used frequencies for descriptive analysis and cross-tabulations in the bivariate analyses where the dependent variable was SMA practice. We applied Poisson regression analysis with robust adjustment to control for possible SMA dependency within the clusters when assessing independent predictors of parental SMA practice. This analysis was because of a high proportion of antibiotics administration to under-fives.23 The outcomes in the multivariable analyses were prevalence ratios that we used to quantify the magnitude and direction of the association with a 5% level of significance.
Ethical Considerations
The Muhimbili University of Health and Allied Sciences Institutional Review Board approved the protocol with reference number DA.287/298/01A/. Participation in the study was on a voluntary basis and we assured each study participant of the strict anonymity and confidentiality of all stages of the study. Each potential study participant signed a consent form or provided a thump print if unable to write.
Results
Description of Study Participants
Total participants for the study were 730 pairs of parents/caregivers and under-five age children (98.9% participation rate). The mean age of respondents was 32.2 (SD=7.4) years. The youngest and oldest parent/caregivers were 21 and 65 years old, respectively. The majority, 668 (91.5%), were the biological mothers of the children; 574 (78.6%) of the parents/caregivers had completed primary education. Almost half, 358 (49.0%), of the study participants perceived their household income level as average (Table 1).
Table 1.
Background Characteristics of Study Participants (n=730)
| Characteristics | Number (%) |
|---|---|
| Respondent’s relationship to the child | |
| Mother | 668 (91.5) |
| Guardian | 62 (8.5) |
| Respondent’s age (years); mean (SD) | 32.2 (SD = 7.4) |
| 21–30 | 296 (40.5) |
| 31–40 41–65 |
328 (44.9) 106 (14.5) |
| Respondent’s highest education level | |
| Primary | 574 (78.6) |
| Secondary and above | 156 (24.4) |
| Main source of income | |
| Agriculture | 381 (52.2) |
| Others | 349 (47.8) |
| Perceived household income level | |
| Low | 258 (35.3) |
| Average | 358 (49.0) |
| High | 114 (15.6) |
| Sex of the child | |
| Boys | 23 (3.2) |
| Girls | 707 (96.8) |
| Age of under-five (months); mean (SD) | 22.1 (SD=2.1) |
| 1–11 | 149 (20.4) |
| 12–23 | 184 (25.2) |
| 24–59 | 397 (54.4) |
Prevalence of Parent/Caregiver Antibiotic Administration to Under-Fives
Among all study participants, 612 (83.8%) parents/caregivers reported their under-fives had been unwell at least once during the 12 months prior to the interviews. Of these, 502 (82.0%) were given antibiotics. The prevalence of parental/caregiver SMA to under-fives was 292 (47.7%) (95% CI=43.7, 51.8). The main source of antibiotics was drug stores, 291 (99.7%).
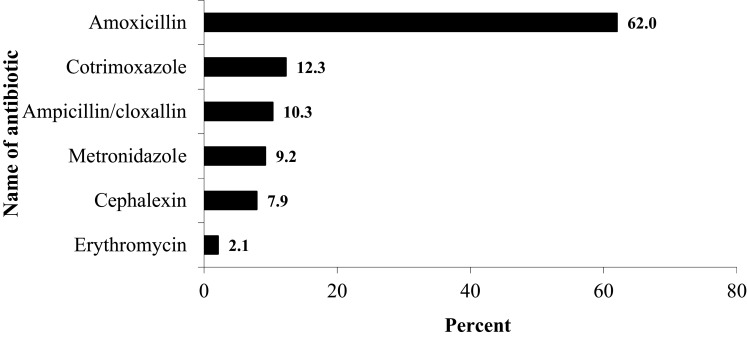
In Figure 1, we present the proportion of parents/caregivers reporting antibiotic use to medicate their under-fives. Common antibiotics used for medicating under-fives were amoxicillin, 181 (62.0%), cotrimoxazole 36 (12.3%) and ampicillin/cloxacillin 30 (10.3%). The main reported illnesses in which parents/caregivers medicated the under-fives with antibiotics were cough 235 (80.5%), fever 153 (52.4%), cold 124 (42.5%), diarrhoea 33 (11.3%) and headache 20 (6.8%).
Figure 1.
Proportion of parents/caregivers reporting different antibiotics used to self-medicate under-fives.
Knowledge About Antibiotics
We assessed knowledge of the general use and misuse of antibiotics. Out of the maximum 20 points allocated to “knowledge,” the average score was 6.9 (SD=2.7) points. Parents/caregivers with a low knowledge of antibiotics comprised 274 (54.6%). Almost a quarter, 119 (23.7%), of study participants confirmed that they had used antibiotics for treating a previous similar condition without medical consultation. Furthermore, 207 (41.2%) believed that they could always self-administer antibiotics at home before considering going to the health facility; 165 (32.9%) reported that they had stopped taking a full course of the antibiotic if their symptoms had improved, and 114 (22.7%) responded that their use of antibiotics without medical consultation could potentially lead to drug resistance.
Factors Associated with Parental/Caregiver Administration of Antibiotics to Under-Fives
In Table 2, we present the prevalence of parental/caregiver administration of antibiotics to under-fives by selected characteristics of the parent/caregiver and of the under-five. In this analysis, one of the factors associated with parents/caregivers medicating under-fives with antibiotics was the age of the parent/caregiver, χ2(L) (1, 502),=26.8, p<0.01. The proportion of parents/caregivers medicating under-fives with antibiotics decreased significantly with increasing age. Similarly, the proportion of parents/caregivers medicating under-fives with antibiotics decreased significantly with an increase in the perceived level of income of the household, χ2(L) (1, 502), = 5.4, p=0.02. Furthermore, significantly more parents/caregivers, 160 (66.7%), who lived closer to their nearest health facility medicated their under-fives with antibiotics than their counterparts, 132 (50.4), χ2 (1, 502)=13.65, p<0.01. Parents/caregivers who self-medicated their under-fives with antibiotics had a significantly lower knowledge score related to the use of antibiotics compared to their counterparts (t(df=501)=3.107, p=0.01). In addition, the proportion of parents/caregivers unaware of prescription-only medication (POM) who -medicated under-fives with antibiotics was significantly higher, 205 (68.1%) than those aware of the policy, χ2 (1, 502)=30.52, p<0.01.
Table 2.
Bivariate Analysis of Factors Associated with Parental Antibiotics Self‐medication
| Characteristic | Parental Antibiotics Self-Medication | χ2, p-value | |
|---|---|---|---|
| Yes, Number (%) | No, Number (%) | ||
| Respondent’s age (years) | 26.8; < 0.001a | ||
| 21–30 | 164 (72.9) | 61 (27.1) | |
| 31–40 | 97 (45.5) | 116 (54.5) | |
| 41–65 | 31 (48.4) | 33 (51.6) | |
| Respondent’s education | 0.24; 0.628 | ||
| Primary | 248 (58.6) | 175 (41.4) | |
| Secondary and above | 44 (55.7) | 35 (44.3) | |
| Perceived household income level | 5.4; < 0.001a | ||
| Low | 104 (71.7) | 41 (28.3) | |
| Average | 144 (50.2) | 143 (49.8) | |
| High | 44 (62.9) | 26 (37.1) | |
| Distance to nearest health facility | 13.65; < 0.001 | ||
| About 30 minutes | 160 (66.7) | 80 (33.3) | |
| More than 30 minutes | 132 (50.4) | 130 (49.6) | |
| Age of under-five (months) | 2.02; 0.155 | ||
| 1–11 | 55 (55.0) | 45 (45.0) | |
| 12–23 | 65 (53.2) | 58 (46.8) | |
| 24–59 | 171 (61.5) | 107 (38.5) | |
| Respondent keeps antibiotics | 3.0; 0.084 | ||
| Yes | 56 (66.7) | 28 (33.3) | |
| No | 236 (56.5) | 182 (43.5) | |
| Mean antibiotic knowledge (SD) | 6.6 (SD=2.5) | 7.4 (SD=2.8) | 3.107; 0.01b |
| Awareness of prescription-only medication | 30.52, <0.01 | ||
| Aware | 87 (42.8) | 114 (57.2) | |
| Not aware | 205 (68.1) | 96 (31.9) | |
Notes: aBased on Ordinal Chi-square test. bBased on independent t-test
Factors Associated with Parents Self-Medicating Under-Fives with Antibiotics
In Table 3, we present the prevalence ratios of SMA to under-fives. Independent factors associated with parental antibiotic self-medication include average household income, distance to the nearest health facility, knowledge about the use of antibiotics and a parent’s/caregiver’s awareness of POMs. Parents/caregivers of under-fives walking more than 30 minutes to the nearest health facility had a significantly (20%) higher prevalence ratio for self-medicating under-fives with antibiotics compared to those living close to the health facility (aPR: 1.2; 95% CI: 1.1, 1.4). In addition, the parents/caregivers of under-fives who were unaware of POMs policy had a significantly (20%) higher prevalence ratio for -medicating under-fives with antibiotics compared to those aware of the policy (aPR: 1.2; 95% CI: 1.1, 1.3).
Table 3.
Multivariable Poisson Regression Analysis of Factors on Parental Self-Medication
| Predictor | PR (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| Respondent’s age (years) | ||
| 21–30 | 1.3 (1.2, 1.4) | 0.9 (0.8, 1.1) |
| 31–40 | 1.3 (1.1, 1.5) | 1.2 (1.0, 1.4) |
| 41–65 | Reference | Reference |
| Perceived household income level | ||
| Low | Reference | Reference |
| Average | 1.2 (1.1, 1.4) | 1.2 (1.0, 1.4) |
| High | 1.1 (1.0, 1.3) | 0.9 (0.8, 1.1) |
| Distance to nearest health facility | ||
| About 30 minutes | Reference | Reference |
| More than 30 minutes | 1.2 (1.1, 1.3) | 1.2 (1.1, 1.4) |
| Age of under-five (months) | ||
| 1–11 | Reference | Reference |
| 12–23 24–59 |
1.1 (1.0, 1.2) 1.1 (1.0, 1.2) |
1.0 (0.9, 1.1) 1.0 (0.9, 1.1) |
| Respondent keeps antibiotics | ||
| Yes | 1.1 (1.0, 1.2) | 1.0 (0.9, 1.1) |
| No | Reference | Reference |
| Mean antibiotic knowledge (SD) | 0.9 (0.98, 0.99) | 1.02 (1.0, 1.04) |
| Awareness of POMs | ||
| Aware | Reference | Reference |
| Not aware | 1.3 (1.2, 1.4) | 1.2 (1.1, 1.3) |
Abbreviations: PR, prevalence ratio; CI, confidence interval; POMs, prescription-only medicines.
Discussion
The study aimed to determine the proportion of parents -medicating under-fives with antibiotics and the factors associated with this practice. In an effort to reduce the antimicrobial resistance through control of the overuse and/or misuse of antibiotics, it is important to establish and quantify the extent of antibiotic self-medication and associated factors in the general population including those caring for under-five aged children. Treatment by use of antibiotics, especially of under-fives, is common.24 In this study, the use of antibiotics occurred with more than 80% of under-fives, whether by prescription or not. Globally, more than 80% of children are prescribed for antimicrobials.25
The reported prevalence of self-medication among adults in some parts of Tanzania is around 70%.26 Since this prevalence may be homogenous and found also in other parts of the country, and since parents practicing self-medication are more likely to self-medicate their children with antibiotics,27,28 it is not surprising that in this study parental SMA was almost 50%. In Uganda, SMA of infants was almost 45%.29 These data fit the general finding that antimicrobial self-medication among the general population of developing countries is high.30
Almost all parents/caregivers mentioned drug stores as the main source of antibiotics used when medicating their under-fives. Possible policy implications of this practice include finding the best mechanisms of reinforcing the Tanzania Food, Drugs and Cosmetics Act of 2003.31 This Act has a legal backing prohibiting pharmaceutical dealers from selling POMs. Nevertheless, SMA practices persist: among possible reasons for parents/caregivers self-medicating antibiotics to under-fives could be their inability to obtain prescriptions from authorized physicians due to long distances to their nearest health-care facilities and a lack of appropriate and adequate knowledge about the use of antibiotics.32
As in many developing countries, over-prescribing of antibiotics in some parts of Tanzania may be a factor in SMA.33 Reasons for the over-prescription of antibiotics include prescription incompetence, diagnostic uncertainty, easily available and accessible antibiotics and the unavailability of treatment guidelines.34 Although knowledge of antibiotics is high among community pharmacists this group appears to be a main source for mishandling POMs.35
In this study, the most common antimicrobials used were amoxicillin, cotrimoxazole and ampicillin/cloxacillin. Several studies in sub-Saharan Africa, including Tanzania, have previously reported the use of amoxicillin for self-medicating under-fives.17,36-38 Reasons for the widespread use of amoxicillin could be historical and also relate to its affordability.39 Also among children, sometimes amoxicillin flavored with banana, orange, strawberry, and fruit can form the basis for its attractiveness. Nevertheless, patients on ampicillin or amoxicillin medications, whether prescribed or not, are at an increased risk of their infections developing antimicrobial resistance.40,41
In this study, parental SMA to under-fives was independent and significantly linked to households of median income, increased distance from a health facility, and both a lower knowledge about the use of antibiotics and awareness about POMs. Parents or caregivers of under-fives from households with high incomes are more likely to seek health-care services, and consequently more likely to obtain the correct prescription and medications. Economic status may, therefore, explain the mechanism for elevated risk of parental SMA to under-fives.42 The relationship between the lower level of knowledge about antibiotic use and parental/caregiver SMA to under-fives is straightforward.43 When a patient or a treatment-supporter has the correct knowledge relating to a treatment plan and type of medication, the patient is more likely to improve or to be cured.
Limitations
This study has some potential biases. One, the responses from parents/caregivers were subject to their ability to recall their use of antibiotics in the most recent occasion within the past 12 months. A twelve-month period was set as an optimum duration for a parent/caregiver to remember when under-five was most recently unwell. In addition, by having a range of common medicines for under-fives, parents/caregivers would correctly remember at least the medications they used when the child was ill. Nevertheless, there is a possibility that some of the respondents were unable to remember exactly whether they used antibiotics or not and the type of the antibiotics. This recall bias might have underestimated our parameters. Two, although we used trained nurses to collect data, there was a possibility that some parents/caregivers knew these nurses, thus, giving socially desirable responses. However, before and during data collection these nurses were intensively trained on interviewing techniques including the way they should present themselves so as to minimize information bias.
Conclusions
We conclude that the prevalence of parental SMA to under-fives is high. More than half of the parents have low knowledge relating to the use of antibiotics. We recommend that health systems improve the measures available to community members to control SMA, including augmenting communication and education campaigns directed against the use of antibiotics without prescription and making the general public more aware of the consequences of SMA. In addition, regulatory bodies should consider strengthening control of the sale of antibiotics.
Acknowledgments
We thank all the parents and caregivers of the under-fives for consenting to participate in this study. This work was edited by Dr Eric James of Rockville, Maryland, USA.
Abbreviations
aPR, adjusted prevalence ratio; CI, confidence interval; POMs, prescription-only medicines; SD, standard deviation; SM, self-medication.
Data Sharing Statement
Data may be available for sharing upon request from the first author bbongole@ihi.or.tz.
Disclosure
The authors declare that they have no competing interests to disclose in this work.
References
- 1.Brata C, Fisher C, Marjadi B, Schneider CR, Clifford RM. Factors influencing the current practice of self-medication consultations in Eastern Indonesian community pharmacies: a qualitative study. BMC Health Serv Res. 2016;16:179. doi: 10.1186/s12913-016-1425-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alhomoud F, Aljamea Z, Almahasnah R, Alkhalifah K, Basalelah L, Alhomoud FK. Self-medication and self-prescription with antibiotics in the Middle East do they really happen? A systematic review of the prevalence, possible reasons, and outcomes. Int J Infect Dis. 2017;57:3–12. doi: 10.1016/j.ijid.2017.01.014 [DOI] [PubMed] [Google Scholar]
- 3.Kamati M, Godman B, Kibuule D. Prevalence of self-medication for acute respiratory infections in young children in Namibia: findings and implications. J Res Pharm Pract. 2019;8(4):220–224. doi: 10.4103/jrpp.JRPP_19_121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams PCM, Isaacs D, Berkley JA. Antimicrobial resistance among children in sub-Saharan Africa. Lancet Infect Dis. 2018;18(2):e33e44. doi: 10.1016/S1473-3099(17)30467-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Hawy RM, Ashmawy MI, Kamal MM, et al. Studying the knowledge, attitude and practice of antibiotic misuse among Alexandria population. Eur J Hosp Pharm. 2017;24(6):349–354. doi: 10.1136/ejhpharm-2016-001032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sridhar SB, Shariff A, Dallah L, Anas D, Ayman M, Rao PG. Assessment of nature, reasons, and consequences of self-medication practice among general population of Ras Al-Khaimah, UAE. Int J Appl Basic Med Res. 2018;8(1):3–8. doi: 10.4103/ijabmr.IJABMR_46_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lei X, Jiang H, Liu C, Ferrier A, Mugavin J. Self-medication practice and associated factors among residents in Wuhan, China. Int J Environ Res Public Health. 2018;15(1):68. doi: 10.3390/ijerph15010068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohseni M, Azami-Aghdash S, Gareh Sheyklo S, et al. Prevalence and reasons of self-medication in pregnant women: a systematic review and meta-analysis. Int J Community Based Nurs Midwifery. 2018;6(4):272–284. [PMC free article] [PubMed] [Google Scholar]
- 9.Shafie M, Eyasu M, Muzeyin K, Worku Y, Martín-Aragón S. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One. 2018;13(3):e0194122. doi: 10.1371/journal.pone.0194122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chokshi A, Sifri Z, Cennimo D, Horng H. Global contributors to antibiotic resistance. J Glob Infect Dis. 2019;11(1):36–42. doi: 10.4103/jgid.jgid_110_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control. 2017;6:47. doi: 10.1186/s13756-017-0208-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tanzania Food, Drugs and Cosmetics Act 2003. Sale and administration of drugs subject to prescription by appropriate practitioners. 2003; Cap 74 (1):60. [Google Scholar]
- 13.Aslam A, Gajdács M, Zin CS, Binti Abd Rahman NS, Ahmed SI, Jamshed SQ. Public awareness and practices towards self-medication with antibiotics among the Malaysian population. A development of questionnaire and pilot-testing. Antibiotics. 2020;9(2):97. doi: 10.3390/antibiotics9020097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal S, Yewale VN, Dharmapalan D. Antibiotics use and misuse in children: A knowledge, attitude and practice survey of parents in India. J Clin Diagn Res. 2015;9(11):SC21SC4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ekambi EG, Ebongue CO, Penda IC, Nga EN, Mpondo EM, Moukoko CE. Knowledge, practices and attitudes on antibiotics use in Cameroon: self-medication and prescription survey among children, adolescents and adults in private pharmacies. PLoS One. 2019;14(2):e0212875. doi: 10.1371/journal.pone.0212875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chipwaza B, Mugasa JP, Mayumana I, Amuri M, Makungu C, Gwakisa PS. Self-medication with anti-malarials is a common practice in rural communities of Kilosa district in Tanzania despite the reported decline of malaria. Malar J. 2014;13:252. doi: 10.1186/1475-2875-13-252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horumpende PG, Said SH, Mazuguni FS, et al. Prevalence, determinants and knowledge of antibacterial self-medication: a cross sectional study in North-eastern Tanzania. PLoS One. 2018;13(10):e0206623. doi: 10.1371/journal.pone.0206623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ngocho JS, Horumpende PG, de Jonge MI, Mmbaga BT. Inappropriate treatment of community-acquired pneumonia among children under five years of age in Tanzania. Int J Infect Dis. 2020;93:56–61. doi: 10.1016/j.ijid.2020.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Torres NF, Solomon VP, Middleton LE. Patterns of self-medication with antibiotics in Maputo City: a qualitative study. Antimicrob Resist Infect Control. 2019;8:161. doi: 10.1186/s13756-019-0618-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ouedraogo AS, Jean Pierre H, Bañuls AL, Ouédraogo R, Godreuil S. Emergence and spread of antibiotic resistance in West Africa: contributing factors and threat assessment. Med Sante Trop. 2017;27(2):147–154. doi: 10.1684/mst.2017.0678 [DOI] [PubMed] [Google Scholar]
- 21.Christopher A, Mshana SE, Kidenya BR, Hokororo A, Morona D. Bacteremia and resistant gram-negative pathogens among under-fives in Tanzania. Ital J Pediatr. 2013;39:27. doi: 10.1186/1824-7288-39-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kish L. Survey Sampling. N.Y: John Wiley & Sons; 1965. [Google Scholar]
- 23.Martinez BAF, Leotti VB, Silva GSE, Nunes LN, Machado G, Corbellini LG. Odds ratio or prevalence ratio? An overview of reported statistical methods and appropriateness of interpretations in cross-sectional studies with dichotomous outcomes in veterinary medicine. Front Vet Sci. 2017;4:193. doi: 10.3389/fvets.2017.00193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rogawski ET, Platts-Mills JA, Seidman JC, et al. Use of antibiotics in children younger than two years in eight countries: a prospective cohort study. Bull World Health Organ. 2017;95(1):49–61. doi: 10.2471/BLT.16.176123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Versporten A, Bielicki J, Drapier N, Sharland M, Goossens H, on behalf of the ARPEC project group. The worldwide antibiotic resistance and prescribing in European children (ARPEC) point prevalence survey: developing hospital-quality indicators of antibiotic prescribing for children. J Antimicrob Chemother. 2016;71(4):1106–1117. doi: 10.1093/jac/dkv418 [DOI] [PubMed] [Google Scholar]
- 26.Mwita S, Meja O, Katabalo D, Richard C. Magnitude and factors associated with anti-malarial self-medication practice among residents of Kasulu Town Council, Kigoma-Tanzania. Afr Health Sci. 2019;19(3):2457–2461. doi: 10.4314/ahs.v19i3.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paredes JL, Navarro R, Riveros M, et al. Parental antibiotic use in urban and peri-urban health care centers in Lima: a cross-sectional study of knowledge, attitudes, and practices. Clin Med Insights Pediatr. 2019;13:1179556519869338. doi: 10.1177/1179556519869338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu M, Zhao G, Stålsby Lundborg C, Zhu Y, Zhao Q, Xu B. Knowledge, attitudes, and practices of parents in rural China on the use of antibiotics in children: a cross-sectional study. BMC Infect Dis. 2014;14:112. doi: 10.1186/1471-2334-14-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ocan M, Aono M, Bukirwa C, et al. Medicine use practices in management of symptoms of acute upper respiratory tract infections in children (≤12 years) in Kampala city, Uganda. BMC Public Health. 2017;17(1):732. doi: 10.1186/s12889-017-4770-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ocan M, Obuku EA, Bwanga F, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health. 2015;15:742. doi: 10.1186/s12889-015-2109-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Tanzania Food and Drugs Authority (TFDA). The Tanzania food, drugs and cosmetics act. 2003;2003:1–89. [Google Scholar]
- 32.Bosley H, Henshall C, Appleton JV, Jackson D. A systematic review to explore influences on parental attitudes towards antibiotic prescribing in children. J Clin Nurs. 2018;27(56):892–905. doi: 10.1111/jocn.14073 [DOI] [PubMed] [Google Scholar]
- 33.Gwimile JJ, Shekalaghe SA, Kapanda GN, Kisanga ER. Antibiotic prescribing practice in management of cough and/or diarrhoea in Moshi Municipality, Northern Tanzania: cross-sectional descriptive study. Pan Afr Med J. 2012. 12 103. [PMC free article] [PubMed] [Google Scholar]
- 34.Keitel K, Kilowoko M, Kyungu E, Genton B, D’Acremont V. Performance of prediction rules and guidelines in detecting serious bacterial infections among Tanzanian febrile children. BMC Infect Dis. 2019;19(1):769. doi: 10.1186/s12879-019-4371-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gajdács M, Paulik E, Szabó A. Knowledge, attitude and practice of community pharmacists regarding antibiotic use and infectious diseases: a cross-sectional survey in Hungary (KAPPhA-HU). Antibiotics. 2020;9(2):41. doi: 10.3390/antibiotics9020041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ateshim Y, Bereket B, Major F, et al. Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional survey. BMC Public Health. 2019;19(1):726. doi: 10.1186/s12889-019-7020-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nepal G, Bhatta S. Self-medication with antibiotics in WHO Southeast Asian region: A systematic review. Cureus. 2018;10(4):e2428. doi: 10.7759/cureus.2428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kibuule D, Kagoya HR, Godman B. Antibiotic use in acute respiratory infections in under-fives in Uganda: findings and implications. Expert Rev Anti Infect Ther. 2016;14(9):863–872. doi: 10.1080/14787210.2016.1206468. [DOI] [PubMed] [Google Scholar]
- 39.Khuluza F, Haefele-Abah C. The availability, prices and affordability of essential medicines in Malawi: A cross-sectional study. PLoS One. 2019;14(2:e0212125. doi: 10.1371/journal.pone.0212125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nhung NT, Chansiripornchai N, Carrique-Mas JJ. Antimicrobial resistance in bacterial poultry pathogens: A review. Front Vet Sci. 2017;4:126. doi: 10.3389/fvets.2017.00126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bernabé KJ, Langendorf C, Ford N, Ronat JB, Murphy RA. Antimicrobial resistance in West Africa: a systematic review and meta-analysis. Int J Antimicrob Agents. 2017;50(5):629–639. doi: 10.1016/j.ijantimicag.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 42.Chang J, Wang Q, Fang Y. Socioeconomic differences in self-medication among middle-aged and older people: data from the China health and retirement longitudinal study. BMJ Open. 2017;7(12):e017306. doi: 10.1136/bmjopen-2017-017306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mboya EA, Sanga LA, Ngocho JS. Irrational use of antibiotics in the Moshi Municipality Northern Tanzania: a cross sectional study. Pan Afr Med J. 2018;31:165. doi: 10.11604/pamj.2018.31.165.15991 [DOI] [PMC free article] [PubMed] [Google Scholar]