Abstract
Background:
Existing evidence suggest that cannabis may impair driving and is the most prevalent drug identified in drivers. Males exhibit an excess risk for driving under the influence of drugs or alcohol compared to females. We assessed sex differences in the association between the reason for cannabis use (medical, recreational, or both) and driving under the influence of cannabis (DUIC).
Methods:
A sample of 17,405 past 12-month cannabis users (18+ years old) were analyzed from the 2016–17 National Survey on Drug Use and Health. Multivariable logistic regression was used to assess the interaction of sex and reason for cannabis use on DUIC using predicted probabilities.
Results:
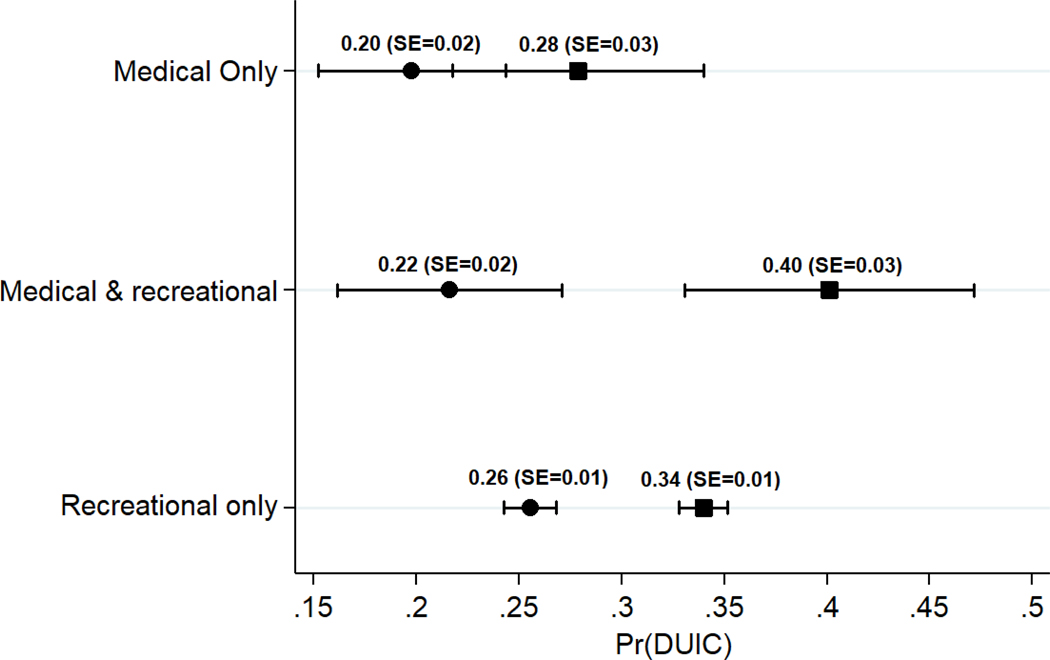
Among cannabis users in the sample, 88.1% used for recreational reasons, 7.8% used for medical reasons, and 4.1% used for medical and recreational reasons. The probability of DUIC was as low as 20% among female medical only users, and as high as 40% among male combined medical and recreational users. Females showed more similar probabilities of DUIC across reasons of use (range 20% to 25%s) than males (range 28% to 40%). The difference in the probability of DUIC between combined medical and recreational users and recreational only users was significantly greater among males than among females (Δ0.1, p<0.05).
Conclusions:
The observed effects of sex and reasons for cannabis use on DUIC suggests a need for targeted educational interventions, particularly among males reporting combined medical and recreational marijuana use.
Keywords: Marijuana, Cannabis, Driving under the Influence, Recreational Cannabis, Medical, Cannabis, Sex
1. Introduction
In the United States (US), cannabis is the most prevalent drug identified in drivers arrested and involved in motor vehicle crashes (MVCs) (Brady & Li, 2014; DuPont et al., 2018; Kelley-Baker et al., 2017; Logan et al., 2014). From 2007 to 2014, the prevalence of night-time drivers testing positive for tetrahydrocannabinol (THC), a psychoactive component of cannabis, increased by 48% (Berning et al., 2015). The most devastating consequence of DUIC is MVC-associated injuries and fatalities. Systematic reviews indicate MVC risk associated with DUIC ranges from no association to twice the risk of a MVC (Asbridge et al., 2012; Hostiuc et al., 2018; Li et al., 2012; Rogeberg & Elvik, 2016).
DUIC is a prevalent behavior in the US. Johnson and White (1989) found that approximately 50% of a sample of young adults in the US reported DUIC, and Davis et. al. (2016) found that approximately 44% of cannabis users in Washington state and Colorado reported past 12-month DUIC (Davis et al., 2016; Johnson & White, 1989). In a study among cannabis users across 50 US states, Cuttler and colleagues found that more than 50% of cannabis users reported DUIC within one-hour of using cannabis (Cuttler, Sexton, & Mischley, 2018). Moreover, approximately 24% of cannabis users in Colorado and Washington state reported DUIC within one-hour of use on at least 5 occasions in the past month (Davis et al., 2016). A Traffic Safety Culture Index (TSCI) report indicated that approximately 5% of drivers reported driving within one hour of using cannabis (Arnold & Tefft, 2016). Recommended lengths of time between cannabis use and driving have ranged from 3–8 hours (Armentano, 2013; Fischer et al., 2013, 2014; Neavyn et al., 2014; Ramaekers et al., 2006).
Cannabis use may cause psychological and physiological impairments including, disorientation, lack of concentration, poor judgement, motor coordination problems, slowed reaction time, lane weaving, sedation, and changes in perception, thought formation, or mood (Asbridge et al., 2012; Couper & Logan, 2004; Downey et al., 2012; Hartman & Huestis, 2013). Nonetheless, some cannabis users perceive DUIC as safe, less dangerous than driving under the influence of alcohol or other illicit drugs, or only perceive cannabis as causing slight impairment (Cuttler et al., 2018; Lenné, Fry, Dietze, & Rumbold, 2001; Terry & Wright, 2005). Furthermore, some individuals may be aware of adverse effects and still feel that MVC risk is not increased (Aitken et al., 2000). Cuttler and colleagues found that approximately 30% of users who believed that cannabis impairs driving drove within one-hour of cannabis use (Cuttler et al., 2018). In addition, DUIC has been associated with reduced speed and increased headway between cars, which may be an attempt to compensate for impairment and allow additional time to react to changes in the driving environment (Anderson, Rizzo, Block, Pearlson, & O’Leary, 2010; Hartman et al., 2016; Lenné et al., 2010; Ronen et al., 2010); however, these factors do not negate the potential of cannabis to impair driving and decrease highway safety. Furthermore, the effects of cannabis can be influenced by frequency of use, age of initiation, and co-use with other substances. For instance, infrequent users have been shown to experience greater impairment than users who have a tolerance for cannabis (Chow et al., 2019; Desrosiers et al., 2015). Moreover, Dahlgren and colleagues (2020) determined that even without acute intoxication, chronic, heavy recreational cannabis users had decreased driving performance compared to healthy controls, including increased accidents, speed, lateral movement, and decreased rule–following. In addition, those who initiated cannabis use before the age of 16 had worse driving performance than those who initiated cannabis use after 16 years of age (Dahlgren et al., 2020). Moreover, cannabis use with other substances may have synergistic effects that increase impairment (Downey et al., 2012; Hartman et al., 2015; Ramaekers, Robbe, & O’Hanlon, 2000).
Patterns of cannabis use, psychosocial factors, and environmental factors have been associated with DUIC. Perceived dangerousness of driving after smoking cannabis has been associated with a lower frequency of driving after smoking cannabis (Aston et al., 2016). Cannabis users who drove within one hour of cannabis use tended to be of younger age, have higher education, use cannabis more frequently, use higher quantities of cannabis, initiate cannabis use at younger ages, and perceive DUIC as safe (Cuttler et al., 2018). Among a sample of young adults, frequency of cannabis use was associated with DUIC (Whitehill et al., 2018). In another study, risk factors for DUIC among cannabis users included being male and having less than a high school education (Walsh & Mann, 1999). Furthermore, DUIC has been associated with population size of a community (i.e. lower population size increased risk of DUIC), cannabis-related problems, polysubstance use, and being a passenger in a car with a person under the influence of alcohol (Alvarez et al., 2007). Moreover, risky driving behaviors have been associated with a risk-taking personality or sensation seeking (Donovan et al., 1983; Jonah, 1990; Macdonald & Mann, 1996). Similarly, Richer and Bergeron (2009) found that impulsitivity and sensation seeking were predictors of DUIC. Correspondingly, Dahlgren and colleagues (2020) found that impulsivity influenced driving performance among sober recreational cannabis users. Additionally, DUIC was associated with risky driving and negative emotional driving (Richer & Bergeron, 2009).
Cannabis users are diverse. Not only are there differences in the strains of cannabis, routes of administration, and dosage of cannabis, but the reasons for use and factors associated with reasons for use differ among cannabis users. Cannabis users may engage in medical use, recreational use, or combined medical and recreational use. Zaller and colleagues (2015) found that medical cannabis use was associated with being male, White, college educated, and covered by health insurance while Ryan-Ibara and colleagues (2015) found that prevalence was highest among White adults and younger adults. Nonetheless, medical cannabis is used by many different types of people. Ryan-Ibara and colleagues (2015) determined that the prevalence of medical cannabis use was similar regardless of gender, education, or region. Furthermore common conditions associated with medical cannabis use included pain, insomnia, and anxiety (Reinarman et al., 2011; Zaller et al., 2015). Individuals who reported any medical cannabis use were more likely to report a higher prevalence of medical conditions compared to recreational cannabis users based on analyses by Wall and colleagues (2019). Similarly, Lin and colleagues (2016) found that medical users had poorer health compared to recreational users. In addition, a significantly larger proportion of medical cannabis users reported daily cannabis use compared to recreational users. Nevertheless, medical cannabis users were less likely to report alcohol use disorder or use of other drugs compared to recreational users (Lin et al., 2016), and medical users were less likely to report anxiety, alcohol use disorder, or opioid use disorder compared to combined medical and recreational cannabis users (Wall et al., 2019). Additionally, another study found that men were more likely to report recreational cannabis use compared to women, and women were more likely to report medical cannabis use compared to men (Cuttler et al., 2016).
Additional research is necessary to better understand the driving behaviors of this heterogeneous population of cannabis users based on the reasons of use. Cuttler and colleagues (2018) found that there were no significant differences between medical, recreational, and combined medical and recreational cannabis users regarding the beliefs of the safety of DUIC, DUIC within one hour of use, and DUIC-related incidents. However, sex differences of these associations have not been explored, particularly when data has shown that males are more likely to drive under the influence than females (Jewett et al., 2015; Lipari et al., 2016). Previous research has not thoroughly examined sex differences in the effects of reasons for cannabis use on self-reported DUIC, based on our knowledge.
The goal of these analyses was to assess sex differences in the association between reason for cannabis use and DUIC in a representative US sample using self-reported data on past 12-month cannabis use and DUIC. We hypothesized that (1) regardless of reason for cannabis use, males would have a higher probability of DUIC than females; (2) regardless of sex, the probability of DUIC would be greatest among recreational only users and lowest among medical only users; (3) the probability of DUIC would be greatest among male recreational only users than among individuals in the other sex-reason groups; and (4) the largest sex differences in the probability of DUIC would be observed when comparing medical only users and recreational only users.
2. Methods
2.1. Participants
Data were obtained from the 2016–2017 National Survey on Drug Use and Health (NSDUH; CBHSQ, 2018a; CBHSQ, 2018b). This annual, cross-sectional survey uses a multistage, state-based probability sampling design to collect data concerning substance use and mental health from a representative US sample. The NSDUH includes civilian, non-institutionalized individuals living in the US, 12 years of age or older. Our analyses included past 12-month cannabis users, 18 years or older, with data on DUIC and reasons for cannabis use (n=17,405).
2.2. Measures
The dependent variable was past 12-month DUIC. Respondents were asked “During the past 12 months, have you driven a vehicle while you were under the influence of marijuana?” DUIC was categorized as a binary variable (yes; no). The independent variable, the reason for cannabis use, was derived from two questions: (1) “Earlier, you reported using marijuana in the past year. Was any of your marijuana use in the past 12 months recommended by a doctor or other health care professional?” and (2) “Was all of your marijuana use in the past 12 months recommended by a doctor or other health care professional?” Cannabis use was defined as medical use only (all use was recommended by a health professional), recreational use only (no use was recommended by a health professional), and combined medical and recreational use (some use was recommended by a health professional).
Covariates included sociodemographic factors, substance use factors, and thrill seeking. Sociodemographic covariates included sex (male; female), age (18–25; 26–34; 35–49; 50+), race/ethnicity (non-Hispanic White; non-Hispanic Black; Hispanic; non-Hispanic other), education (less than high school; high school graduate; some college/associate degree; college graduate or higher), household income (less than $20,000; $20,000-$49,999; $50,000-$74,999; $75,000 or higher), and residence in a state with a medical marijuana law (MML, yes; no). Respondents rated overall health as excellent, very good, good, or fair/poor. Substance use covariates included past 12-month other drug use (yes; no) and past 30-day alcohol use (no alcohol use; alcohol use, no binge drinking; binge drinking, no heavy alcohol use; heavy alcohol use; CBHSQ, 2018b). Other drugs included cocaine, hallucinogens, heroin, inhalants, methamphetamine, and misuse of psychotherapeutics (prescription pain relievers, sedatives, stimulants, and tranquilizers). Covariates associated with cannabis use included risk perception of using cannabis once or twice a week (no/slight risk; moderate/great risk), age of first use (continuous), and past 12-month frequency of cannabis use (continuous; number of days used out of the past 365 days). Thrill-seeking was derived from the question “How often do you get a real kick out of doing things that are a little dangerous?” (never recoded as no; seldomsometimes/always recoded as yes).
2.3. Data Analysis
Chi-square tests of independence, two sample t-tests, and bivariate logistic regression models were performed to assess differences in cannabis users by DUIC status. Multivariable logistic regression models were conducted to estimate the predicted probabilities of DUIC by sex and reasons for cannabis use, while holding constant the effect of potential confounders.These analyses helped determine whether an interaction effect was present in the natural metric of the dependent variable using predicted probabilities (Agresti, 2013; Long, 1997; Long & Freese, 2014; Mize, 2019). Differences in the marginal effects (first order differences) and the equality of differences in the marginal effects (second differences or interaction effects) across subgroups of interest were tested by comparing predicted probabilities from the multivariable logistic regression models as recommended by Mize (2019) for non-linear dependent variables. Significance levels were set at p<0.05. Estimates were weighted to control for the NSDUH’s multistage, stratified sampling design. Descriptive statistics were performed in SAS ® software, version 9.4 (SAS Institute, Cary NC), and multivariable logistic regression were conducted using Stata 13 (StataCorpLP, College Station, TX).
3. Results
3.1. Descriptive Summary
Table 1 shows the descriptive summary for all variables included in the analyses. Among cannabis users, 88.1% used for recreational only reasons (males: 88.2% vs. females: 88.1%), 7.8% used for medical only reasons (males: 7.7% vs. females: 7.9%), and 4.1% used for combined medical and recreational reasons (males: 4.2% vs. females: 3.9%). Approximately one-third (33.2%) of cannabis users reported DUIC; 24.8% of females and 33.8% of males reported DUIC. Among adults who reported DUIC, 86.8% were recreational only users, 7.3% were medical only users, and 5.9% were combined recreational and medical reasons. The predicted probabilities of DUIC by sex and reason for cannabis use from the multivariable logistic regression model are shown in Figure 1. These predicted probabilities were used to determine the first differences and second differences between sex and across reasons for cannabis use within sex shown in Table 2 and Table 3.
Table 1.
Sociodemographic and substance use characteristics of past 12-month cannabis users stratified by driving under the influence of cannabis (DUIC) status (n=17,405)
| Characteristics | Overall n =17,405 % (95% CI) | No DUIC n=11,627 % (95% CI) | DUIC n=5,778 % (95% CI) | p-value | OR (95% CI) § |
|---|---|---|---|---|---|
| Reason for cannabis use | 0.0001 | ||||
| Medical only | 7.8 (7.0,8.5) | 8.0 (6.9,9.1) | 7.3 (5.9,8.6) | ref. | |
| Recreational only | 88.1 (87.3, 89.0) | 88.7 (87.6,89.9) | 86.8 (85.2,88.5) | 1.08 (0.82,1.41) | |
| Medical and recreational | 4.1 (3.6,4.6) | 3.3 (2.8,3.8) | 5.9 (4.8,7.0) | 1.97 (1.41,2.77) | |
| Sex | <0.0001 | ||||
| Female | 41.8 (40.7,42.9) | 44.9 (43.3,46.5) | 34.6 (33.0,36.2) | ref. | |
| Male | 58.2 (57.1, 59.3) | 55.1 (53.5,56.7) | 65.4 (63.8,67.0) | 1.54 (1.39,1.71) | |
| Age | <0.0001 | ||||
| 18–25 | 32.1 (31.1,33.2) | 29.3 (27.8,30.7) | 38.9 (37.2,40.6) | ref. | |
| 26–34 | 24.8 (23.9,25.7) | 24.7 (23.6, 25.8) | 25.1(23.4,26.9) | 0.77(0.68,0.86) | |
| 35–49 | 21.9 (21.1,22.8) | 22.6 (21.4,23.8) | 20.4 (19.1, 21.8) | 0.68 (0.59,0.78) | |
| 50+ | 21.1 (19.7, 22.5) | 23.5 (21.8,25.2) | 15.5 (13.5,17.6) | 0.50 (0.41,0.60) | |
| Race/Ethnicity | 0.0061 | ||||
| Non-Hispanic Whites | 65.9 (64.7,67.1) | 64.8 (63.4,66.2) | 68.6 (66.5,70.7) | ref. | |
| Non-Hispanic Blacks | 14.0 (13.2,14.8) | 14.5 (13.5, 15.4) | 13.0 (11.6,14.4) | 0.85 (0.73,0.99) | |
| Hispanics | 13.4 (12.4,14.3) | 13.7 (12.4, 15.0) | 12.6 (11.5,13.7) | 0.87(0.73,1.03) | |
| Non-Hispanic “Other” | 6.7 (5.9, 7.5) | 7.1 (6.1, 8.0) | 5.8 (5.0,6.6) | 0.78 (0.66,0.91) | |
| Education | <0.0001 | ||||
| Less than high school | 11.0 (10.2,11.7) | 11.4 (10.6, 12.2) | 10.0 (8.7,11.3) | ref. | |
| High school graduate | 24.8 (23.9,25.7) | 24.7 (23.6, 25.7) | 25.2 (23.6,26.8) | 1.17 (0.98,1.39) | |
| Some college/associate degree | 37.3 (36.0,38.6) | 35.4 (33.9,39.9) | 41.7 (39.5, 43.8) | 1.34 (1.13,1.60) | |
| College graduate or higher | 26.9 (25.5, 28.4) | 28.5 (26.9,30.1) | 23.2 (21.0, 25.3) | 0.93 (0.78,1.10) | |
| Household Income | 0.0005 | ||||
| Less than $20,000 | 22.8 (21.7,23.8) | 23.6 (22.4, 24.9) | 20.8 (19.2, 22.3) | ref. | |
| $20,000 - $49,999 | 30.1 (29.1,31.1) | 30.0 (28.9, 31.0) | 30.5 (29.0, 32.0) | 1.16 (1.04, 1.29) | |
| $50,000 - $74,999 | 14.1 (13.4,14.8) | 13.3 (12.6, 14.0) | 15.8(14.2, 17.5) | 1.35 (1.15,1.60) | |
| $75,000+ | 33.0 (31.7,34.3) | 33.1 (31.7, 34.4) | 32.9 (30.9, 35.0) | 1.13(1.00,1.28) | |
| Self-Rated Health* | <0.0001 | ||||
| Excellent | 19.6 (18.7,20.4) | 20.7 (19.6, 21.7) | 17.0 (15.7, 18.4) | ref. | |
| Very Good | 38.0 (37.0,39.1) | 36.7 (35.3, 38.0) | 41.1 (39.8, 42.5) | 1.36 (1.21,1.53) | |
| Good | 29.2 (28.3,30.2) | 28.7 (27.5, 30.0) | 30.3 (28.6, 32.1) | 1.28 (1.11,1.47) | |
| Fair/Poor | 13.2 (12.3,14.1) | 13.9 (12.8, 15.0) | 11.5 (10.3, 12.6) | 1.00 (0.85,1.18) | |
| Past 12-month Other Drug Use | <0.0001 | ||||
| No | 65.9 (64.8,67.0) | 72.6 (71.4, 73.8) | 50.2 (48.1, 52.4) | ref. | |
| Yes | 34.1 (33.0,35.2) | 27.4 (26.2, 28.6) | 49.8 (47.6, 51.9) | 2.63 (2.36,2.93) | |
| Past 30-day Alcohol Use | <0.0001 | ||||
| No | 21.2 (20.2,22.1) | 22.3 (21.1, 23.5) | 18.6 (17.2, 19.9) | ref. | |
| Alcohol use | 24.6 (23.6,25.6) | 25.8 (24.6, 27.0) | 21.9 (20.1, 23.7) | 1.02 (0.87,1.19) | |
| Binge drinking | 35.5 (34.6,36.5) | 34.9 (33.6, 36.2) | 37.0 (35.2, 38.8) | 1.27 (1.11,1.45) | |
| Heavy alcohol use | 18.7 (17.8,19.6) | 17.0 (15.9, 18.1) | 22.5 (21.0, 24.1) | 1.59 (1.39,1.83) | |
| Live in a state with a medical marijuana law | 0.0278 | ||||
| No | 36.1 (34.9,37.2) | 35.3 (33.8, 36.8) | 37.9 (36.1, 39.7) | ref. | |
| Yes | 63.9 (62.8, 65.1) | 64.7 (63.2, 66.2) | 62.1 (60.3, 63.9) | 0.89 (0.80,0.99) | |
| Cannabis risk perception* (n=8479) | <0.0001 | ||||
| No/Slight risk | 88.4 (87.5,89.3) | 86.0 (85.0, 87.0) | 94.0 (92.9, 95.0) | ref. | |
| Moderate/Great risk | 11.6 (10.7,12.5) | 14.0 (13.0, 15.0) | 6.0 (5.0, 7.1) | 0.39 (0.33,0.48) | |
| Thrill seeking* | <0.0001 | ||||
| No | 27.6 (26.4,28.8) | 31.4 (29.9, 32.8) | 18.9 (17.4, 20.6) | ref. | |
| Yes | 72.4 (71.2,73.6) | 68.6 (67.2, 70.1) | 81.0 (79.3, 82.5) | 1.96 (1.74,2.20) | |
| Age of first cannabis use (years), Mean (95% CI) | 17.1 (16.9, 17.3) | 17.7 (17.5,17.9) | 15.7 (15.6,15.9) | <0.0001 | 0.90 (0.89,0.92) |
| Frequency of cannabis use (days), Mean (95% CI) | 126.1 (123.5,128.6) | 91.4 (88.1,94.7) | 206.7 (201.6,211.9) | <0.0001 | 1.01 (1.01,1.01) |
| Survey Year | 0.8555 | ||||
| 2016 | 47.9 (46.6,49.1) | 47.8 (46.3, 49.3) | 48.0 (45.8, 50.3) | ref. | |
| 2017 | 52.1 (50.9,53.4) | 52.2 (50.7, 53.7) | 52.0 (49.7, 54.2) | 0.99 (0.89,1.10) | |
Missingness: self-rated health,n=3; cannabis risk perception, n=39; thrill seeking, n=37
Bivariate models were adjusted for survey year.
Figure 1. Probability of driving under the influence of cannabis (DUIC) by sex and reason for cannabis use.
Pr(DUIC)= Probability of driving under the influence of cannabis
SE=Standard Error
Table 2.
Probability of driving under the influence of cannabis (DUIC) by sex and reason for cannabis use: marginal effects of sex and differeces in effects of sex across reasons for cannabis use.
| Effect of sex | First differences (SE) | Second differences§ (SE) | |
|---|---|---|---|
| a. Males vs. Females, among medical only users | 0.28 – 0.20 = 0.08 (0.04)* | a vs. b | 0.08 – 0.18= −0.10 (0.06) |
| b. Males vs. Females, among combined medical & recreational users | 0.40 – 0.22 = 0.18 (0.04)** | b vs. c | 0.18 – 0.08= 0.10 (0.04)* |
| c. Males vs. Females, among recreational only users | 0.33 – 0.25 = 0.08 (0.01)** | a vs. c | 0.08 – 0.08= ~0.01 (0.04) |
The “ second differences” column presents the sex differences (first differences) across reasons of use (second differences).
p<0.05;
p<0.01.
Note: This model was adjused for age, race/ethnicity, education, household income, self-rated health, past 12-month other drug use, past 30-day alcohol use, residence in a state with a medical marijuana law, cannabis risk perception, thrill seeking, age of first cannabis use, frequency of cannabis use, survey year.
Table 3.
Probability of driving under the influence of cannabis (DUIC) by reason for cannabis use and sex: marginal effects of reasons for cannabis use and differeces in effects of reasons for cannabis use across sex.
| Effect of reason for cannabis use | First differences (SE) | Second differences (SE)§ | |
|---|---|---|---|
| a. Medical only vs. Recreational only among males | 0.28 – 0.34 = − 0.06 (0.03) | a vs. b | −0.06 – (− 0.06)= 0.01(0.04) |
| b. Medical only vs. Recreational only among females | 0.20 – 0.26 = −0.06 (0.02) * | ||
| c. Medical only vs. Combined medical & recreational among males | 0.28 – 40 = −0.12 (0.05)* | c vs. d | −0.12 – (−0.02)= 0.1 (0.06) |
| d. Medical only vs. Combined medical & recreational among females | 0.20 – 0.22 = −0.02 (0.04) | ||
| e. Combined medical & recreational vs. Recreational only among males | 0.40 – 0.34 = 0.06 (0.04) | e vs. f | 0.06 – (−0.04)= 0.1(0.04)* |
| f. Combined medical & recreational vs. Recreational only among females | 0.22 – 0.26 = −0.04 (0.03) | ||
The second differences” column presents the differences in the reasons for use (first differences) across sex (second differences).
p<0.05;
p<0.01, two-tailed test.
Note: This model was adjused for age, race/ethnicity, education, household income, self-rated health, past 12-month other drug use, past 30-day alcohol use, residence in a state with a medical marijuana law, cannabis risk perception, thrill seeking, age of first cannabis use, frequency of cannabis use, survey year.
3.2. Effect of Sex
Males showed higher probabilities of DUIC than females across all reasons for use based on marginal differences (first differences; Table 2). The marginal effects encapsulated the effect of the independent variables in terms of the model’s predicted probabilites (Mize 2019). Males who reported medical only use had a significantly higher probability of DUIC (0.28) than females who also reported medical only use (0.20; Δ = 0.08; p<0.05). Moreover, males who reported recreational only use had a significantly higher probability of DUIC (0.34) than females who reported recreational only use (0.26; Δ = 0.08; p<0.01). Compared to female combined medical and recreational users (0.22), male combined medical and recreational users had a significantly higher probability of DUIC (0.40; Δ = 0.18; p<0.01).
To test for the interaction between sex and reason for cannabis use, second differences were calculated to test the equality of multiple effects (Mize 2019). When considering the effect of sex on the relationship between reason for cannabis use and DUIC [second differences (interaction effects); Table 2], the sex gap in the probability of DUIC was significantly greater for adults who reported combined medical and recreational cannabis use than for adults who used cannabis recreationally only (Δ0.1, p<0.05). Therefore, DUIC probabilities between males and females who reported recreational only cannabis use were more similar than DUIC probabilities between males and females who reported combined medical and recreational cannabis use.
3.3. Effect of Reason for Cannabis Use
Males who used cannabis for combined medical and recreational reasons had a significantly higher probability of DUIC than males who used it for medical only reasons (Δ = 0.12; p<0.05; Table 3 first differences or marginal effects). In addition, female recreational only cannabis users had a significantly higher probability of DUIC than females who used it for medical only reasons (Δ = 0.06; p<0.05).
When examining whether differences in the probability of DUIC across reasons for cannabis use differed among males and females, our results revealed that the difference in the probability of DUIC between combined medical and recreational users and recreational only users was significantly greater among males than among females (Δ = 0.1; p<0.05). No other significant differences across reasons for cannabis use were identified among males and females.
4. Discussion
With regards to our first hypothesis, we found that males had significantly higher probabilities of DUIC compared to females in the corresponding reason for cannabis use group. Our second hypothesis was partially supported. Among females, recreational only users showed the greatest probability of DUIC. However, among males combined medical and recreational users showed the greatest probability of DUIC. Thus, our third hypothesis was not supported; combined medical and recreational male users showed the greatest probability of DUIC. Finally, our fourth hypothesis was partially supported. Among females, the largest significant difference in the probability of DUIC was observed between recreational only users and medical only users. However, among males the largest significant difference in the probability of DUIC was found between combined medical and recreational users and recreational only users. A test of the sex*reason for use interaction revealed that the difference in the probability of DUIC between combined medical and recreational users and recreational only users was significantly greater among males than among females. While prior research has not found differences in regards to driving practices and reasons for cannabis use (Cuttler et al., 2018), our findings suggest that sex differences should be considered when assessing this association.
Regardless of the reason for cannabis use, males had higher probabilities of DUIC compared to females. These findings were consistent with previous studies. Among respondents 16 years or older in the US, males reported higher rates of driving under the influence of illicit drugs and driving under the influence of both alcohol and illicit drugs in the past year compared to females (Lipari et al., 2016). A study sponsored by the AAA Foundation for Traffic Safety determined that, among drivers, males were more likely to report the use of alcohol and cannabis compared to females. Moreover, males were more likely to report DUIC within one hour of use (Arnold & Tefft, 2016). There is substantial evidence in the literature that males are more likely to drive under the influence than females.
Nonetheless, differences in the effect of sex across reasons for cannabis use were observed. Males who reported combined medical and recreational cannabis use had substantially higher probabilities of DUIC. Combined medical and recreational users may experience better health than medical only cannabis users, but experience poorer health compared to recreational only users (Wall et al., 2019). In comparison to medical cannabis use, combined medical and recreational users may use cannabis recreationally for non-medical reasons (i.e. to feel pleasure, to have fun, or to fit in with peers), without a doctor’s recommendation to treat medical conditions or to substitute cannabis for another medication, or both (Salazar et al., 2019). Even after a recommendation for medical cannabis from a physician, cannabis users may not receive appropriate information about behaviors such as DUIC after using cannabis (Haug et al., 2016; Linares et al., 2016). There are accepted standards to guide practices regarding the use of medications and substances such as tobacco and alcohol; however, there are no globally accepted standards that can help cannabis users make informed decisions about their actions after cannabis use (National Academies of Sciences, Engineering, and Medicine, 2017). Efforts to increase harm reduction, including educational campaigns and evidence-based education through medical providers and dispensary staff may be necessary to ensure the safety of this high risk group on the highway. Furthermore, additional research is necessary to understand the reasons for combined medical and recreational cannabis use as well as its consequences, including DUIC.
Among females, those who reported recreational only use had a greater probability of DUIC than medical only users. The excess probability of DUIC among females who reported recreational only use compared to medical only users is consistent with research documenting the increased rates of traffic accidents among cannabis users who exhibited increasing risk taking behavior and use drugs recreationally (Neavyn et al., 2014). Furthermore, recreational cannabis use has been associated with polysubstance use (Lin et al., 2016), which may increase impairment and involvement in riskier behaviors such as DUIC.
At the same time, the lower probabilities of DUIC observed among female medical only users, warrants further investigation, particularly with regards to the factors preventing and protecting female medical cannabis users from DUIC. Among medical cannabis users with chronic pain, higher levels of pain have been associated with a decreased likelihood of DUIC (Bonar et al., 2019). In this regard, Lin and colleagues found that medical cannabis users were more likely to have poorer health compared to recreational users (Lin et al., 2016). Similarly, Wall and colleagues (2019) determined that medical only users had a lower physical quality of life and higher prevalence of medical conditions (i.e. pain interference, arthritis, nerve peoblems, insomnia, cancer, diabetes, and human immunodeficiency virus) compared to recreational only users. However, medical only users reported a lower prevalence of psychiatric disorders compared to those who reported any recreational cannabis use (Wall et al., 2019). Therefore, increased probability of DUIC among females with recreational cannabis use compared to medical only users may be due to other heath related factors not assessed in this study. Although we adjusted for self-rated health status in our models, the potential of residual confounding exists as this variable does not reflect potential disabilities that may prevent or reduce driving.
In addition, Salazar and colleagues (2019) found that medical only users had unique characteristics compared to recreational only users and combined medical and recreational users. A larger proportion of medical only users reported “other” employment, which included being student, retired, stay at home parent, or unable to work (Salazar et al., 2019). These individuals may drive less than those those who are employed, resulting in a lower probability of DUIC. In the same study, medical only users tended to intiate use at a later age and use a vaporizer as the primary route of administration (Salazar et al., 2019). Refraining from combustible cannabis and cannabis use during adolescence have been recommended to reduce cannabis associated risks (Fischer et al., 2017). Furthermore, medical only users reported using higher percentages of THC and had more knowledge about the THC content of products used (Salazar et al., 2019). Therefore, being aware of the contents of cannabis products used may aid in the decision-making process to drive under the influence, resulting in decreased DUIC when high levels of THC are used.
Limitations of our analyses should be noted. First, data was self-reported; self-reported data is vulnerable to recall and social desirability biases. However, past 12-month self-reported data were used for the analyses. Recall bias may be reduced in the analyses due to the short time period of self-reproted data. In addition, the NSDUH used computer assisted interviewing methods to increase privacy and accurate reporting for sensitive topics such as substance use. Misclassification of the reason for cannabis use may be present due to the assessment of medical cannabis use. Medical cannabis use was defined as use recommended by a doctor or other health care professional. A definition of “health care provider” was not specified, and the type of health professional (e.g. registered vs. non-registered) who recommended any type of cannabis product is unknown. Third, the NSDUH does not capture information on driving status. Some adults may not drive. Fourth, a dichotomous measure of DUIC may have a lower sensitivity than a continuous DUIC measure such as frequency of DUIC. Fifth, impairment while driving was unknown. Impairment can be influenced by several factors, including the potency of cannabis, quantity used, frequency of use, route of administration, type of preparation, co-use with other substances, and tolerance. Sixth, residual confounding may be present. For example, the analyses did not include information on the frequency or quantity of other substances used. Lastly, estimates of DUIC may be underestimated, as those who were killed in MVCs were not included in the NSDUH.
Despite these limitations, we were able to assess DUIC among cannabis users using NSDUH data, which represents one of the few reliable sources of self-reported DUIC behaviors at the national level. Beginning with the 2016 NSDUH, respondents were asked specifically about DUIC. Self-reported DUIC may provide an improved estimate of those who drive under the influence of cannabis as the collection of blood samples have some limitations. For instance, DUIC has been assessed by identifying THC and its metabolites in biological samples; however, these products may be detectable for a month or more of abstinence (Rogeberg & Elvik, 2016). Furthermore, DUIC has been associated with other substance use, which may influence impairment (Downey et al., 2012; Hartman et al., 2015; Ramaekers et al., 2000); cannabis use with other substances complicate the relationship between cannabis use and DUIC. Self-report of DUIC may reduce some of these challenges. Moreover, we examined the interaction between sex and reason for cannabis use on DUIC among cannabis users. Although, it has been well established that males have a higher rate of driving under the influence than females, it is critical to assess nuances in cannabis use within and between the sexes.
5. Conclusions
Our findings provide evidence of an independent and combined effect of sex and reason for cannabis use on the probability of DUIC. Observed sex and reason for use differences suggests a need for targeted educational interventions to decrease DUIC, especially among males who reported combined medical and recreational use and females who reported recreational cannabis use. To decrease DUIC and consequences associated with DUIC, education, surveillance, improved characterization of cannabis products, instruments to rapidly detect cannabis associated impairment, and monitoring of psychoactive cannabinoids may be needed to increase highway safety.
Highlights.
Approximately one-third of adult cannabis users reported DUIC.
Male combined medical and recreational cannabis users had the highest probability of DUIC.
Female medical only users had the lowest probability of DUIC.
The largest sex gap in DUIC was found among combined medical and recreational users.
Targeted educational interventions are needed to prevent DUIC.
Acknowledgments
Role of Funding Source: This work was supported by a National Institute on Drug Abuse (NIDA) T32 training grant (T32DA035167) and a NIDA Mentored Research Scientist Development Award (K01DA046715) from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding sources did not have a role in the study design, collection, analysis and interpretation of data, writing of the report, and decision to submit the article for publication.
Footnotes
Author Disclosures
Conflicts of Interest: No conflicts declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agresti A (2013). Categorical Data Analysis. Hoboken, NJ: Wiley. [Google Scholar]
- Aitken C, Kerger M, & Crofts N. (2000). Drivers Who Use Illicit Drugs: behaviour and perceived risks. Drugs: Education, Prevention and Policy, 7(1), 39–50. 10.1080/dep.7.1.39.50 [DOI] [Google Scholar]
- Alvarez FJ, Fierro I, & Del Río MC (2007). Cannabis and driving: Results from a general population survey. Forensic Science International, 170(2–3), 111–116. 10.1016/j.forsciint.2007.03.024 [DOI] [PubMed] [Google Scholar]
- Anderson BM, Rizzo M, Block RI, Pearlson GD, & O’Leary DS (2010). Sex Differences in the Effects of Marijuana on Simulated Driving Performance. Journal of Psychoactive Drugs, 42(1), 19–30. 10.1080/02791072.2010.10399782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armentano P. (2013). Cannabis and psychomotor performance: A rational review of the evidence and implications for public policy: Cannabis and psychomotor performance. Drug Testing and Analysis, 5(1), 52–56. 10.1002/dta.1404 [DOI] [PubMed] [Google Scholar]
- Arnold L, & Tefft B. (2016, May 12). Driving Under the Influence of Alcohol and Marijuana: Beliefs and Behaviors, United States, 2013–2015. AAA Foundation; https://aaafoundation.org/driving-influence-alcohol-marijuana-beliefs-behaviors-united-states-2013-2015/ [Google Scholar]
- Asbridge M, Hayden JA, & Cartwright JL (2012). Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ, 344(feb09 2), e536–e536. 10.1136/bmj.e536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aston ER, Merrill JE, McCarthy DM, & Metrik J. (2016). Risk Factors for Driving After and During Marijuana Use. Journal of Studies on Alcohol and Drugs, 77(2), 309–316. 10.15288/jsad.2016.77.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berning A, Compton R, & Wochinger K. (2015). Results of the 2013–2014 National Roadside Survey of Alcohol and Drug Use by Drivers (Traffic Safety Facts Research Note DOT HS 812 118). National Highway Safety Administration; https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/812118-roadside_survey_2014.pdf [Google Scholar]
- Bonar EE, Cranford JA, Arterberry BJ, Walton MA, Bohnert KM, & Ilgen MA (2019). Driving under the influence of cannabis among medical cannabis patients with chronic pain. Drug and Alcohol Dependence, 195, 193–197. 10.1016/j.drugalcdep.2018.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady JE, & Li G. (2014). Trends in alcohol and other drugs detected in fatally injured drivers in the United States, 1999–2010. Am J Epidemiol, 179(6), 692–699. 10.1093/aje/kwt327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CBHSQ. (2018). 2017 National Survey on Drug Use and Health Final Analytic File Codebook. Substance Abuse and Mental Health Services Administration; http://samhda.s3-us-gov-west-1.amazonaws.com/s3fs-public/field-uploads-protected/studies/NSDUH-2017/NSDUH-2017-datasets/NSDUH-2017-DS0001/NSDUH-2017-DS0001-info/NSDUH-2017-DS0001-info-codebook.pdf [PubMed] [Google Scholar]
- CBHSQ. (2018). 2016 National Survey on Drug Use and Health: Public Use File Codebook. Substance Abuse and Mental Health Services Administration; https://samhda.s3-us-gov-west-1.amazonaws.com/s3fs-public/field-uploads-protected/studies/NSDUH-2016/NSDUH-2016-datasets/NSDUH-2016-DS0001/NSDUH-2016-DS0001-info/NSDUH-2016-DS0001-info-codebook.pdf [Google Scholar]
- Chow RM, Marascalchi B, Abrams WB, Peiris NA, Odonkor CA, & Cohen SP (2019). Driving Under the Influence of Cannabis: A Framework for Future Policy. Anesthesia & Analgesia, 128(6), 1300–1308. 10.1213/ANE.0000000000003575 [DOI] [PubMed] [Google Scholar]
- Couper FJ, & Logan BK (2004). Drugs and Human Performance Fact Sheets. National Highway Traffic Safety Administration; https://one.nhtsa.gov/About-NHTSA/Traffic-Techs/current/Drugs-and-Human-Performance-Fact-Sheets [Google Scholar]
- Cuttler C, Mischley LK, & Sexton M. (2016). Sex Differences in Cannabis Use and Effects: A Cross-Sectional Survey of Cannabis Users. Cannabis Cannabinoid Res, 1(1), 166–175. 10.1089/can.2016.0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuttler C, Sexton M, & Mischley L. (2018). Driving Under the Influence of Cannabis: An Examination of Driving Beliefs and Practices of Medical and Recreational Cannabis Users across the United States. Cannabis, 1(2), 1–13. 10.26828/cannabis.2018.02.001 [DOI] [Google Scholar]
- Dahlgren MK, Sagar KA, Smith RT, Lambros AM, Kuppe MK, & Gruber SA (2020). Recreational cannabis use impairs driving performance in the absence of acute intoxication. Drug and Alcohol Dependence, 107771. 10.1016/j.drugalcdep.2019.107771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis KC, Allen J, Duke J, Nonnemaker J, Bradfield B, Farrelly MC, Shafer P, & Novak S. (2016). Correlates of Marijuana Drugged Driving and Openness to Driving While High: Evidence from Colorado and Washington. PLOS ONE, 11(1), e0146853. 10.1371/journal.pone.0146853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desrosiers NA, Ramaekers JG, Chauchard E, Gorelick DA, & Huestis MA (2015). Smoked Cannabis’ Psychomotor and Neurocognitive Effects in Occasional and Frequent Smokers. Journal of Analytical Toxicology, 39(4), 251–261. 10.1093/jat/bkv012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan DM, Marlatt GA, & Salzberg PM (1983). Drinking behavior, personality factors and high-risk driving. A review and theoretical formulation. Journal of Studies on Alcohol, 44(3), 395–428. [DOI] [PubMed] [Google Scholar]
- Downey LA., King R., Papafotiou K., Swann P., Ogden E., Boorman M., & Stough C. (2012). Detecting impairment associated with cannabis with and without alcohol on the Standardized Field Sobriety Tests. Psychopharmacology, 224(4), 581–589. 10.1007/s00213-012-2787-9 [DOI] [PubMed] [Google Scholar]
- DuPont RL, Holmes HM, Talphins SK, & Walsh JM (2018). Marijuana-Impaired Driving In Contemporary Health Issues on Marijuana (pp. 183–218). Oxford University Press. [Google Scholar]
- Fischer B, Dawe M, McGuire F, Shuper PA, Capler R, Bilsker D, Jones W, Taylor B, Rudzinski K, & Rehm J. (2013). Feasibility and impact of brief interventions for frequent cannabis users in Canada. Journal of Substance Abuse Treatment, 44(1), 132–138. 10.1016/j.jsat.2012.03.006 [DOI] [PubMed] [Google Scholar]
- Fischer B, Ivsins A, Rehm J, Webster C, Rudzinski K, Rodopoulos J, & Patra J. (2014). Factors Associated with High-Frequency Cannabis Use and Driving among a Multisite Sample of University Students in Ontario. Canadian Journal of Criminology and Criminal Justice, 56(2), 185–200. 10.3138/cjccj.2014.ES03 [DOI] [Google Scholar]
- Fischer B, Russell C, Sabioni P, van den Brink W, Le Foll B, Hall W, Rehm J, & Room R. (2017). Lower-Risk Cannabis Use Guidelines: A Comprehensive Update of Evidence and Recommendations. American Journal of Public Health, 107(8), e1–e12. 10.2105/AJPH.2017.303818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman RL, & Huestis MA (2013). Cannabis Effects on Driving Skills. Clinical Chemistry, 59(3), 478–492. 10.1373/clinchem.2012.194381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman RL, Brown TL, Milavetz G, Spurgin A, Pierce RS, Gorelick DA, Gaffney G, & Huestis MA (2015). Cannabis effects on driving lateral control with and without alcohol. Drug and Alcohol Dependence, 154, 25–37. 10.1016/j.drugalcdep.2015.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman RL, Brown TL, Milavetz G, Spurgin A, Pierce RS, Gorelick DA, Gaffney G, & Huestis MA (2016). Cannabis effects on driving longitudinal control with and without alcohol: Cannabis’ effects on longitudinal driving control with/without alcohol. Journal of Applied Toxicology, 36(11), 1418–1429. 10.1002/jat.3295 [DOI] [PubMed] [Google Scholar]
- Haug NA, Kieschnick D, Sottile JE, Babson KA, Vandrey R, & Bonn-Miller MO (2016). Training and Practices of Cannabis Dispensary Staff. Cannabis and Cannabinoid Research, 1(1), 244–251. 10.1089/can.2016.0024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostiuc S, Moldoveanu A, Negoi I, & Drima E. (2018). The Association of Unfavorable Traffic Events and Cannabis Usage: A Meta-Analysis. Frontiers in Pharmacology, 9, 99 10.3389/fphar.2018.00099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewett A, Shults RA, Banerjee T, & Bergen G. (2015). Alcohol-Impaired Driving Among Adults - United States, 2012. MMWR. Morbidity and Mortality Weekly Report, 64(30), 814–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson V, & White HR (1989). An investigation of factors related to intoxicated driving behaviors among youth. Journal of Studies on Alcohol, 50(4), 320–330. [DOI] [PubMed] [Google Scholar]
- Jonah BA. (1990). Age differences in risky driving. Health Education Research, 5(2), 139–149. 10.1093/her/5.2.139 [DOI] [Google Scholar]
- Kelley-Baker T, Berning A, Ramirez A, Lacey J, Carr K, Waehrer G, & Compton R. (2017). 2013–2014 National Roadside Study of Alcohol and Drug Use by Drivers: Drug Results (Report No. DOT HS 812 411). National Highway Traffic Safety Administration; https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/documents/13013-nrs_drug_092917_v6_tag.pdf [Google Scholar]
- Lenné MG, Fry CLM, Dietze P, Rumbold G. (2001). Attitudes and Experiences of People Who Use Cannabis and Drive: Implications for drugs and driving legislation in Victoria, Australia. Drugs: Education, Prevention and Policy, 8(4), 307–313. 10.1080/09687630110048061 [DOI] [Google Scholar]
- Lenné MG, Dietze PM, Triggs TJ, Walmsley S, Murphy B, & Redman JR (2010). The effects of cannabis and alcohol on simulated arterial driving: Influences of driving experience and task demand. Accident Analysis & Prevention, 42(3), 859–866. 10.1016/j.aap.2009.04.021 [DOI] [PubMed] [Google Scholar]
- Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, & Li G. (2012). Marijuana Use and Motor Vehicle Crashes. Epidemiologic Reviews, 34(1), 65–72. 10.1093/epirev/mxr017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin LA, Ilgen MA, Jannausch M, & Bohnert KM (2016). Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addictive Behaviors, 61, 99–103. 10.1016/j.addbeh.2016.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares R, Choi-Nurvitadhi J, Cooper S, Ham Y, Ishmael JE, & Zweber A. (2016). Personnel training and patient education in medical marijuana dispensaries in Oregon. Journal of the American Pharmacists Association, 56(3), 270–273.e2. 10.1016/j.japh.2015.12.015 [DOI] [PubMed] [Google Scholar]
- Lipari RN, Hughes A, & Bose J. (2016). Driving Under the Influence of Alcohol and Illicit Drugs (The CBHSQ Report) Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; https://www.samhsa.gov/data/sites/default/files/report_2688/ShortReport-2688.html [PubMed] [Google Scholar]
- Logan BK, Mohr ALA, & Talpins SK (2014). Detection and Prevalence of Drug Use in Arrested Drivers Using the Dräger Drug Test 5000 and Affiniton DrugWipe Oral Fluid Drug Screening Devices. Journal of Analytical Toxicology, 38(7), 444–450. 10.1093/jat/bku050 [DOI] [PubMed] [Google Scholar]
- Long SJ (1997). Regression Models for Categorical and Limited Dependent Variables. Thosand Oaks, CA: Sage. [Google Scholar]
- Long SJ., & Freese J. (2014). Regression Models for Categorical Dependent Variables Using Stata, Third Edition College Station, TX: Stata Press. [Google Scholar]
- Macdonald S, & Mann RE (1996). Distinguishing causes and correlates of drinking and driving. Contemporary Drug Problems, 23(2), 259–290. 10.1177/009145099602300206 [DOI] [Google Scholar]
- Mennes CE, Ben Abdallah A, & Cottler LB (2009). The reliability of self-reported cannabis abuse, dependence and withdrawal symptoms: Multisite study of differences between general population and treatment groups. Addictive Behaviors, 34(2), 223–226. 10.1016/j.addbeh.2008.10.003 [DOI] [PubMed] [Google Scholar]
- Mize T. (2019). Best Practices for Estimating, Interpreting, and Presenting Nonlinear Interaction Effects. Sociological Science, 6, 81–117. 10.15195/v6.a4 [DOI] [Google Scholar]
- Neavyn MJ, Blohm E, Babu KM, & Bird SB (2014). Medical Marijuana and Driving: a Review. Journal of Medical Toxicology, 10(3), 269–279. 10.1007/s13181-014-0393-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers JG, Moeller MR, van Ruitenbeek P, Theunissen EL, Schneider E, & Kauert G. (2006). Cognition and motor control as a function of Δ9-THC concentration in serum and oral fluid: Limits of impairment. Drug and Alcohol Dependence, 85(2), 114–122. 10.1016/j.drugalcdep.2006.03.015 [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Robbe HWJ, & O’Hanlon JF (2000). Marijuana, alcohol and actual driving performance. Human Psychopharmacology, 15(7), 551–558. [DOI] [PubMed] [Google Scholar]
- Reinarman C, Nunberg H, Lanthier F, & Heddleston T. (2011). Who are medical marijuana patients? Population characteristics from nine California assessment clinics. Journal of Psychoactive Drugs, 43(2), 128–135. 10.1080/02791072.2011.587700 [DOI] [PubMed] [Google Scholar]
- Richer I, & Bergeron J. (2009). Driving under the influence of cannabis: Links with dangerous driving, psychological predictors, and accident involvement. Accident Analysis & Prevention, 41(2), 299–307. 10.1016/j.aap.2008.12.004 [DOI] [PubMed] [Google Scholar]
- Rogeberg O, & Elvik R. (2016). The effects of cannabis intoxication on motor vehicle collision revisited and revised: Cannabis and motor vehicle collision risk. Addiction, 111(8), 1348–1359. 10.1111/add.13347 [DOI] [PubMed] [Google Scholar]
- Ronen A, Chassidim HS, Gershon P, Parmet Y, Rabinovich A, Bar-Hamburger R, Cassuto Y, & Shinar D. (2010). The effect of alcohol, THC and their combination on perceived effects, willingness to drive and performance of driving and non-driving tasks. Accident Analysis & Prevention, 42(6), 1855–1865. 10.1016/j.aap.2010.05.006 [DOI] [PubMed] [Google Scholar]
- Salazar CA., Tomko RL., Akbar SA., Squeglia LM., & McClure EA. (2019). Medical Cannabis Use among Adults in the Southeastern United States. Cannabis (Research Society on Marijuana), 2(1), 53–65. [PMC free article] [PubMed] [Google Scholar]
- Terry P, & Wright KA (2005). Self-reported driving behaviour and attitudes towards driving under the influence of cannabis among three different user groups in England. Addictive Behaviors, 30(3), 619–626. 10.1016/j.addbeh.2004.08.007 [DOI] [PubMed] [Google Scholar]
- Wall MM, Liu J, Hasin DS, Blanco C, & Olfson M. (2019). Use of marijuana exclusively for medical purposes. Drug and Alcohol Dependence, 195, 13–15. 10.1016/j.drugalcdep.2018.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh GW, & Mann RE (1999). On the high road: driving under the influence of cannabis in Ontario. Canadian Journal of Public Health = Revue Canadienne De Sante Publique, 90(4), 260–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehill JM, Rodriguez-Monguio R, Doucette M, & Flom E. (2018). Driving and riding under the influence of recent marijuana use: Risk factors among a racially diverse sample of young adults. Journal of Ethnicity in Substance Abuse, 1–19. 10.1080/15332640.2018.1425951 [DOI] [PubMed] [Google Scholar]
- Zaller N, Topletz A, Frater S, Yates G, & Lally M. (2015). Profiles of Medicinal Cannabis Patients Attending Compassion Centers in Rhode Island. Journal of Psychoactive Drugs, 47(1), 18–23. 10.1080/02791072.2014.999901 [DOI] [PubMed] [Google Scholar]