Abstract
Introduction
Despite greater smoking prevalence among sexual minority (SM) individuals relative to non-SM individuals, minimal research has examined whether SM smokers have differential success at quitting, and no prior treatment studies have examined differences within SM subgroups. There is also limited knowledge of the psychosocial characteristics of treatment-seeking SM smokers, which could inform targeted treatments. To address these gaps, we compared treatment outcomes and baseline characteristics for SM and non-SM smokers and for bisexual versus lesbian or gay smokers in a large randomized controlled trial of two web-based cessation treatments.
Methods
Trial participants completed a survey to assess baseline characteristics, including self-identification as either SM (n = 253; lesbian or gay, n = 122; bisexual, n = 131) or non-SM (n = 2384). The primary cessation outcome was complete-case, self-reported 30-day abstinence at 12 months after randomization.
Results
Cessation outcomes did not differ significantly for SM versus non-SM smokers (24% vs. 25%, adjusted OR = 0.91, 95% CI = 0.65 to 1.28) or across SM subgroups (24% for bisexual vs. 23% for lesbian or gay, adjusted OR = 1.01, 95% CI = 0.51 to 2.00), and there were no interactions with treatment group assignment. At baseline, SM smokers differed from non-SM smokers on most demographics, were more likely to screen positive for all mental health conditions assessed, and had greater exposure to other smokers in the home.
Conclusions
Substantial differences in baseline characteristics of SM versus non-SM smokers and bisexual versus lesbian or gay smokers did not translate into differential treatment outcomes. Nonetheless, SM smokers’ willingness or ability to quit smoking could be enhanced by taking their unique psychosocial profile into account when designing targeted interventions.
Implications
The findings of this study, which included the largest sample of SM smokers in a prospective intervention trial to date, support those of a small extant body of literature showing no differences in treatment-assisted cessation outcomes between SM and non-SM smokers. Regardless of their quit rates relative to non-SM smokers, SM smokers’ willingness or ability to quit smoking could potentially be enhanced by taking their unique psychosocial profile into account in intervention design, including their younger age, lower socioeconomic status, greater likelihood of being racial or ethnic minorities, and greater prevalence of mental health symptoms.
Introduction
Being a member of a sexual minority (SM) group—that is, identifying with a sexual orientation other than heterosexual or straight—is associated with higher likelihood of ever and current cigarette smoking as well as greater use of other nicotine and tobacco products, such as electronic nicotine delivery systems.1–5 Although it is clear that some of these differences in use reflect higher rates of initiation among SM adolescents and young adults relative to their heterosexual peers,6,7 it is less clear whether differential success rates for quit attempts may also play a role. Elucidating the reasons that the current prevalence of tobacco use is 1.5–2 times higher in the SM population than in the non-SM population,1,3,8 including the possibility that quitting may be more difficult, is critical to formulating plans to address tobacco-related health disparities experienced by SM adults, such as higher all-cause and cancer-related mortality.9 Knowledge of how SM tobacco users differ from non-SM users on characteristics that could inform targeted, culturally competent intervention approaches is also an important but neglected area of inquiry, as SM smokers consistently indicate a preference for targeted treatments over nontargeted treatments.10–13
Only three studies have examined differences in cessation outcomes or psychosocial characteristics of treatment-seeking smokers who identify as SM versus non-SM. All three studies were secondary analyses of clinical trials, and two of the three focused on a broad group of sexual and gender minority (SGM) smokers, including not only those who identify with a sexual orientation other than heterosexual or straight, but also those whose gender identity does not match sex assigned at birth. In the first trial, which focused only on men, there were no significant differences in end-of-treatment quit rates between heterosexual men and gay or bisexual men in response to a combined behavioral and pharmacologic treatment.14 Likewise, in the second trial, which was a pooled analysis of extended pharmacotherapy and group cessation counseling, the SGM participants did not differ from the non-SGM participants on quit rates at any follow-up point through 2 years after randomization.15 Finally, there were no significant differences in treatment outcomes for SGM versus non-SGM young adults in a trial of a Facebook-delivered intervention, either at end of treatment or at 12-month follow-up.16 Given the size of the SM or SGM samples in these studies (ie, ranging from n = 54 to n = 136), statistical power to detect modest differences in quit rates was low. Larger studies are needed to be more confident that the lack of differences is not attributable to small sample sizes alone.
These same three trials are also the only published studies examining differences in the psychosocial characteristics of treatment-seeking smokers who identify as SM or SGM versus nonminority smokers. The first study found that male smokers who identified as gay or bisexual were younger and of higher socioeconomic status than heterosexual male smokers but did not differ on other demographics, smoking, or psychological and mental health characteristics.14 The second trial found that SGM smokers only differed from non-SGM smokers in terms of younger age and higher scores on one indicator of motivation to quit, whereas they did not differ on socioeconomic status, mood states, perceived stress, heaviness of smoking, or severity of nicotine dependence.15 The final trial focused exclusively on young adults and examined only differences in smoking-related characteristics at baseline, finding no differences between SGM and non-SGM participants.16 Thus, with the possible exception of younger age, there is little consistency in the findings of the existing literature on differences between SM and non-SM smokers in a treatment context, which is partly a function of the small number of published studies on this topic and partly a function of the limited set of baseline characteristics on which groups have been compared. A more comprehensive evaluation of differences in the profiles of SM and non-SM smokers could aid in the design of targeted interventions that take the characteristics of the population into account—a central tenet of user-centered design.17
To the best of our knowledge, no treatment studies to date have evaluated differences between smokers who identify as bisexual and those who identify as lesbian or gay. This may be because the sample size of SM or SGM participants in the three previous treatment studies14–16 ranged from 54 to 136, meaning that comparisons of SM or SGM subgroups would have low statistical power. Outside of the cessation treatment context, there is evidence that bisexual smokers may differ on several characteristics that are predictive of cessation. One population study found lower severity of nicotine dependence among bisexual women relative to lesbian and heterosexual women,5 which may suggest less difficulty quitting. On the other hand, adults who identify as bisexual tend to be younger and less likely than either heterosexual or lesbian or gay adults to have a college degree, and they may be more likely to be unemployed, living in poverty, lack health insurance and/or a health care provider, have poor mental health, and report prior-year suicidal ideation.4,18 Given that low socioeconomic status, poor access to health care (including medications and other support for quitting), and mental health conditions are associated with difficulty quitting,19–21 it is possible that bisexual smokers are at greater risk of poor cessation outcomes than lesbian or gay smokers.
In sum, minimal research has focused on the treatment outcomes and psychosocial characteristics of SM smokers, and no studies have examined differences within SM subgroups. To address these knowledge gaps and inform SM-focused tobacco control efforts, we conducted a secondary analysis of data from a randomized controlled trial of two web-delivered interventions for smoking cessation,22 comparing treatment outcomes as well as baseline characteristics of SM and non-SM smokers to determine the extent to which SM smokers may (1) have more difficulty quitting, and (2) differ in their psychosocial profiles, which may be useful for informing targeted treatment efforts regardless of whether there are differences in cessation outcomes. We also explored differences in cessation outcomes and baseline characteristics within the SM group based on whether they identified as lesbian or gay versus bisexual, as previous evidence indicates that bisexual adults may differ from lesbian or gay adults on several characteristics that predict cessation outcomes. Finally, we also explored differences in self-reported utilization of cessation medications as a secondary outcome. Both web programs encouraged participants to consider using pharmacotherapy to support their quit attempt, but medications were not provided through the study and, based on prior literature showing differences in health care access,4 may not be equally accessible to SM smokers.
Methods
Participants
Participants (n = 2637) enrolled in a randomized controlled trial evaluating the effectiveness of two web-delivered smoking cessation interventions.22 Of the 2637 participants, 253 reported on the baseline survey (see Measures section for a detailed description) that they identified as lesbian, gay, or bisexual (ie, SM), and the remaining 2384 identified as heterosexual or straight (non-SM). To be eligible, participants had to (1) be aged 18 or older; (2) smoke at least 5 cigarettes/day for the last 12 months; (3) be motivated to quit in the next 30 days; (4) reside in the United States; (5) be able to read in English; (6) have Internet and E-mail access; (7) never have used Smokefree.gov, the control condition, or the experimental acceptance and commitment therapy web intervention via participation in a previous study by the research team; (8) not currently be enrolled in any cessation interventions; (9) not have another household member participating; and (10) be willing to be randomized and complete all study procedures.
Procedures
A comprehensive description of study procedures is provided in the report of the main study outcome.22 Briefly, participants were recruited for the trial via diversified online (eg, Facebook, Google and Craigslist advertisements, an online survey panel, organic search engine results) and offline methods (earned traditional media, family and friend referrals, mailings to Kaiser Permanente Washington health plan members) between March 2014 and August 2015. Targeted recruitment strategies were used to meet the objective of reaching 25% representation of racial/ethnic minorities.23 There was no targeting of recruitment on the basis of SM status. Recruitment methods that yielded the highest number of SM trial participants were Facebook advertisements (n = 84), online survey panel (n = 69), and free Internet methods such as Craigslist (n = 56); these findings are consistent with the top three recruitment methods for the overall trial.23 Despite Facebook advertisements having the highest overall yield of enrolled SM participants, they also produced the lowest proportion of participants from that source identifying as SM (7%), whereas free Internet methods (15%) and survey panel (13%) had the highest.23
Interested potential participants were linked to a recruitment web page for additional details about the study. Those who remained interested after learning more about the study completed an online eligibility survey. Eligible individuals were sent a link via E-mail to enter the study Web site, which prompted them to provide informed consent and complete a baseline survey and contact form. When these tasks were completed, participants were enrolled and randomized to receive one of two web-based cessation interventions: one grounded in acceptance and commitment therapy and the other in the standard care treatment model (the National Cancer Institute’s Smokefree.gov Web site). Participants had access to their assigned intervention for 12 months following randomization. In addition to the web program, participants received up to four intervention text messages per day for 28 days. The treatment content of the messages differed by arm, but in both arms the intended functions of the messages were to push key intervention content out to users as well as encouraging them to use their assigned web program.
Outcome assessments were administered at 3, 6, and 12 months after randomization via a multimodal survey protocol. The first modality offered was a web-based survey, followed by telephone, mail, and postcard-only options sequentially as needed until a response was received or the protocol was completed and the participant was classified as a nonresponder. Participants were compensated $25 for completing each survey, with a $10 bonus for responding within 24 hours to any E-mailed survey link. Because the entire study was conducted remotely, procedures to prevent fraudulent activity were implemented (eg, CAPTCHA authentication, monitoring of duplicate and non-US IP addresses, contacting participants by phone if unusual response patterns were detected). All study procedures were reviewed and approved by the Fred Hutchinson Cancer Research Center Institutional Review Board. The trial was registered on ClinicalTrials.gov (National Clinical Trial no. 1166334).
Measures
Baseline Demographics, Including Sexual Orientation
The baseline survey covered demographics such as age, gender (male vs. female), race (American Indian or Alaska Native, Asian, black or African American, Native Hawaiian or Other Pacific Islander, white, or Other; categorized for analysis into white vs. nonwhite), ethnicity (yes or no to being Hispanic or Latino), relationship status (yes or no to being in a long-term, committed relationship, regardless of whether married or not), education (highest level achieved; categorized for analysis into high school or lower vs. greater than high school), income, and sexual orientation. Low income was defined as household annual income less than or equal to US $20 000. The survey question assessing sexual orientation asked, “Do you consider yourself to be: (a) heterosexual or straight, (b) gay or lesbian, (c) bisexual?”
Smoking
The Fagerström Test for Nicotine Dependence24 was included as a measure of nicotine dependence severity. The Commitment to Quitting Smoking Scale25 and the Avoidance and Inflexibility Scale26 were administered to assess commitment to achieving abstinence and smoking-specific experiential avoidance (ie, efforts to avoid aversive internal states, like negative affect, by smoking), respectively, which were the theory-based targets of the novel acceptance and commitment therapy intervention being evaluated. The survey also included questions about current electronic cigarette use (ie, “How often do you currently [within the last 30 days] use any kind of e-cigarettes?” with response options ranging from “not at all” to “at least daily”; responses categorized for analysis into a binary indicator of any use in the prior 30 days) and number of quit attempts in the past 12 months. There were three questions related to the density of smokers in the immediate social environment—that is, number of close friends who smoke, number of adults in the home who smoke, and whether or not they live with a partner who smokes.
Mental Health
The baseline survey included both mental health screeners and an item to assess self-reported mental health conditions,20,27 which included options for anxiety disorder, depression disorder, bipolar disorder, schizophrenia, alcohol abuse, drug abuse, or none of the above. Mental health screeners covered depression (Center for Epidemiological Studies Depression Scale 28; positive screen is ≥16), generalized anxiety (Generalized Anxiety Disorder-729; positive screen is ≥10), panic disorder (Autonomic Nervous System Questionnaire30), post-traumatic stress disorder (PTSD Checklist31; positive screen is ≥14), social anxiety (Mini Social Phobia Inventory32; positive screen is ≥6), and at-risk drinking (Alcohol Use Disorders Identification Test-Concise).33 Heavy drinking on the Alcohol Use Disorders Identification Test-Concise was defined as drinking four or more (for women) or five or more (for men) drinks on a typical drinking day.34 On the Autonomic Nervous System Questionnaire, a positive screen for panic disorder required (1) indication of a panic attack in the past month, and (2) at least one attack in the past month occurring in a situation in which they were not in danger or not the center of attention.30
Cessation Outcomes
Cessation was assessed via participant self-report of time since last cigarette (not even a puff). The primary cessation outcome for the trial was 30-day point prevalence abstinence (PPA) at 12 months using complete-case analysis. As a sensitivity analysis, we also examined 30-day PPA at 12-month follow-up assuming that all missing responses were indicative of smoking (ie, missing = smoking). As this was a large population-based cessation trial with no face-to-face contact, where demand characteristics are minimal and biochemical confirmation is not feasible because of sample size,35 we did not biochemically verify self-reported abstinence.
Cessation Medication Utilization
The 12-month outcome survey assessed utilization of pharmacotherapy that was suggested in the web programs, but not provided by the study. The survey question covered the period since randomization and asked whether participants had used any of the following medications: nicotine gum, nicotine patch, Chantix, Zyban, none, or other. Given that the study only enrolled participants who resided in the United States, we limited our definition of cessation medication utilization to US Food and Drug Administration-approved medications (ie, nicotine replacement therapy, bupropion, and varenicline).
Statistical Analysis
Comparison of baseline characteristics was conducted using chi-squared tests for categorical variables and t tests for continuous variables. Adjusted logistic regression and negative binomial models were used to evaluate differences in cessation outcomes and pharmacotherapy utilization by SM status. Models included terms for treatment group assignment and baseline factors used in stratified randomization (ie, gender, high school or less education, and smoking ≥21 cigarettes/day) and considered treatment by SM status interactions. Interaction terms that were not significant were dropped from the final models. Baseline demographic and smoking variables were included in the models as covariates if they differed by diagnostic group and were associated with the cessation outcome. Owing to the post hoc, exploratory nature of the analyses, we did not control for multiple testing. All tests used a two-sided significance level of p < .05. Analyses were conducting using R, v. 3.4.236 and R package “MASS”.37
Results
Baseline Characteristics
As shown in Table 1, compared with non-SM smokers, SM smokers were younger, lower-income, and more likely to be racial and ethnic minorities. There was a higher proportion of men in the SM group than in the non-SM group. SM participants had higher rates of every self-reported and screened mental health condition, including anxiety disorders, mood disorders, serious mental illnesses (bipolar disorder and schizophrenia), heavy drinking, and substance use disorders. They did not differ significantly from non-SM smokers on nicotine dependence, heaviness of smoking, use of electronic cigarettes, or quit attempts in the past 12 months. They also did not differ on the psychological processes targeted by acceptance and commitment therapy —that is, commitment to quitting and smoking-specific experiential avoidance. They did report a higher number of adults in the home who smoked.
Table 1.
Baseline Characteristics of Participants, by Sexual Minority Status
| Total (n = 2637) | Non-SM (n = 2384) | SM (n = 253) | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age, mean (SD) | 46.2 (13.4) | 47.0 (13.1) | 38.3 (12.8) | <.001 |
| Male | 546 (21%) | 468 (20%) | 78 (31%) | <.001 |
| White | 1914 (73%) | 1764 (74%) | 150 (59%) | <.001 |
| Hispanic | 222 (8%) | 186 (8%) | 36 (14%) | <.001 |
| In a long-term committed relationship | 1639 (62%) | 1486 (62%) | 153 (60%) | .609 |
| Working | 1381 (52%) | 1250 (52%) | 131 (52%) | .895 |
| HS or less education | 735 (28%) | 677 (28%) | 58 (23%) | .076 |
| Low income | 737 (28%) | 640 (27%) | 97 (38%) | <.001 |
| Mental health | ||||
| Current depression symptoms (CES-D) | 1470 (56%), n = 2622 | 1302 (55%), n = 2370 | 168 (67%), n = 252 | <.001 |
| Current anxiety symptoms (GAD-7) | 903 (34%), n = 2623 | 788 (33%), n = 2373 | 115 (46%), n = 250 | <.001 |
| Current panic disorder symptoms (ANSQ) | 1145 (48%), n = 2364 | 1006 (47%), n = 2129 | 139 (59%), n = 235 | <.001 |
| Current PTSD symptoms (PCL-6) | 1383 (53%), n = 2628 | 1224 (51%), n = 2377 | 159 (63%), n = 251 | <.001 |
| Current social anxiety symptoms (mini-SPIN) | 797 (30%), n = 2630 | 704 (30%), n = 2377 | 93 (37%), n = 253 | .023 |
| Heavy drinker (on AUDIT-C) | 282 (11%), n = 2573 | 236 (10%), n = 2325 | 46 (19%), n = 248 | <.001 |
| Self-reported depression | 711 (27%) | 623 (26%) | 88 (35%) | .004 |
| Self-reported anxiety | 667 (25%) | 577 (24%) | 90 (36%) | <.001 |
| Self-reported bipolar disorder or schizophrenia | 227 (9%) | 178 (7%) | 49 (19%) | <.001 |
| Self-reported alcohol or drug abuse | 157 (6%) | 123 (5%) | 34 (13%) | <.001 |
| Self-reported no mental health conditions | 1566 (59%) | 1444 (61%) | 122 (48%) | <.001 |
| Smoking behavior | ||||
| FTND score, mean (SD) | 5.6 (2.2) | 5.6 (2.2) | 5.5 (2.3) | .297 |
| Smokes >1 pack per day | 873 (33%) | 803 (34%) | 70 (28%) | .063 |
| Used e-cigarettes at least once in past month | 909 (34%) | 819 (34%) | 90 (36%) | .750 |
| Quit attempts in past 12 mo, mean (SD) | 1.7 (5.0), n = 2511 | 1.7 (5.1), n = 2277 | 1.5 (3.3), n = 234 | .564 |
| Commitment to quitting (CQS) | 4.0 (0.8), n = 2628 | 4.0 (0.8), n = 2375 | 4.0 (0.8), n = 253 | .708 |
| Acceptance of physical triggers (AIS) | 3.0 (0.5), n = 2603 | 3.0 (0.5), n = 2352 | 2.9 (0.5), n = 251 | .176 |
| Friend and partner smoking | ||||
| Close friends who smoke, mean (SD) | 2.2 (1.6) | 2.2 (1.6) | 2.4 (1.6) | .084 |
| Adults in home who smoke, mean (SD) | 1.5 (0.8) | 1.4 (0.8) | 1.6 (0.9) | .019 |
| Live with partner who smokes | 780 (30%) | 694 (29%) | 86 (34%) | .122 |
p values based on chi-squared tests for categorical variables and t tests for continuous variables.
AIS = Avoidance and Inflexibility Scale; ANSQ = Autonomic Nervous System Questionnaire; AUDIT-C = Alcohol Use Disorders Identification Test-Concise; CES-D = Center for Epidemiological Studies Depression Scale; CQS = Commitment to Quitting Scale; e-cigarette = electronic cigarette; FTND = Fagerström Test for Nicotine Dependence; GAD-7 = Generalized Anxiety Disorder-7; HS = high school; Mini-SPIN = Mini Social Phobia Inventory; PCL-6 = PTSD Checklist; PTSD = post-traumatic stress disorder; SM = sexual minority.
As shown in Table 2, compared with smokers who identified as lesbian or gay, those who identified as bisexual were younger, more likely to be in a long-term committed relationship, and more likely to be women. They had lower severity of nicotine dependence but reported a higher number of adults in the home who smoked and were more than twice as likely to live with a partner who smoked (47% vs. 20%, p < .01). They did not differ on race/ethnicity, any indicators of socioeconomic status (employment, education, income), electronic cigarette use, recent quit attempts, or any mental health conditions or symptoms.
Table 2.
Baseline Characteristics of Lesbian or Gay Versus Bisexual Participant
| Lesbian or gay (n = 122) | Bisexual (n = 131) | p | |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) | 42.5 (13.6) | 34.3 (10.6) | <.001 |
| Male | 56 (46%) | 22 (17%) | <.001 |
| White | 75 (61%) | 75 (57%) | .579 |
| Hispanic | 14 (11%) | 22 (17%) | .303 |
| In a long-term committed relationship | 65 (53%) | 88 (67%) | .033 |
| Working | 68 (56%) | 63 (48%) | .276 |
| HS or less education | 31 (25%) | 27 (21%) | .449 |
| Low income | 43 (35%) | 54 (41%) | .340 |
| Mental health | |||
| Current depression symptoms (CES-D) | 75 (62%) | 93 (71%) | .167 |
| Current anxiety symptoms (GAD-7) | 54 (45%) | 61 (47%) | .768 |
| Current panic disorder symptoms (ANSQ) | 66 (58%) | 73 (60%) | .805 |
| Current PTSD symptoms (PCL-6) | 75 (62%) | 84 (65%) | .763 |
| Current social anxiety symptoms (mini-SPIN) | 40 (33%) | 53 (40%) | .257 |
| Heavy drinker (AUDIT-C) | 22 (18%) | 24 (19%) | >0.99 |
| Self-reported depression | 43 (35%) | 45 (34%) | .986 |
| Self-reported anxiety | 38 (31%) | 52 (40%) | .198 |
| Self-reported bipolar disorder or schizophrenia | 22 (18%) | 27 (21%) | .719 |
| Self-reported alcohol or drug abuse | 14 (11%) | 20 (15%) | .485 |
| Self-reported no mental health conditions | 65 (53%) | 57 (44%) | .153 |
| Smoking behavior | |||
| FTND score, mean (SD) | 5.8 (2.3) | 5.2 (2.2) | .030 |
| Smokes >1 pack per day | 41 (34%) | 29 (22%) | .058 |
| Used e-cigarettes at least once in past month | 45 (37%) | 45 (34%) | .772 |
| Quit attempts in past 12 mo, mean (SD) | 1.5 (3.3), n = 111 | 1.6 (3.2), n = 123 | .877 |
| Commitment to quitting | 4.0 (0.8) | 3.9 (0.8) | .422 |
| Acceptance of physical triggers | 2.9 (0.5), n = 121 | 2.9 (0.5), n = 130 | .763 |
| Friend and partner smoking | |||
| Close friends who smoke, mean (SD) | 2.2 (1.6) | 2.5 (1.5) | .184 |
| Number of adults in home who smoke, mean (SD) | 1.4 (0.8) | 1.8 (1.0) | <.001 |
| Living with partner who smokes | 25 (20%) | 61 (47%) | <.001 |
p values based on chi-squared tests for categorical variables and t tests for continuous variables.
ANSQ = Autonomic Nervous System Questionnaire; AUDIT-C = Alcohol Use Disorders Identification Test-Concise; CES-D = Center for Epidemiological Studies Depression Scale; e-cigarette = electronic cigarette; FTND = Fagerström Test for Nicotine Dependence; GAD-7 = Generalized Anxiety Disorder-7; HS = high school; Mini-SPIN = Mini Social Phobia Inventory; PCL-6 = PTSD Checklist; PTSD = post-traumatic stress disorder.
Cessation Outcomes
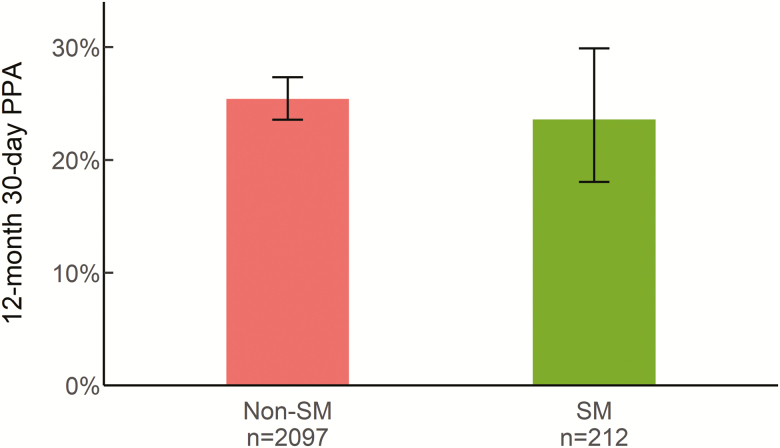
Data retention rates at 12 months were similar between SM (84%) and non-SM (88%) smokers (p = .13). On the primary cessation outcome of self-reported, 30-day PPA at 12 months after randomization, the quit rates for SM smokers (23.6%) versus non-SM smokers (25.4%) were not significantly different (adjusted OR = 0.91, 95% CI = 0.65 to 1.28, p = .58; see Figure 1). In a sensitivity analysis, the missing = smoking outcomes yielded a similar conclusion: quit rates for SM smokers (19.8%) did not significantly differ from non-SM smokers (22.4%; adjusted OR = 0.86, 95% CI = 0.62 to 1.20, p = .39). Both of these analyses controlled for treatment arm (which was not associated with outcome, as reported previously22), three stratification factors, white race, self-reported depression, self-reported anxiety, self-reported no mental health conditions, and number of adults in the home who smoke. The treatment group by SM status interaction was not significant in any of the models evaluating cessation outcomes, so the interaction term was dropped.
Figure 1.
Complete-case, 30-day point prevalence abstinence (PPA) at 12 months with 95% confidence intervals, by sexual minority (SM) status.
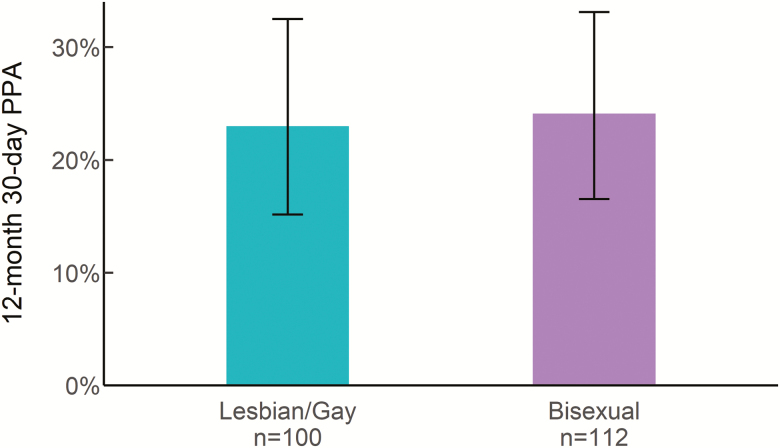
Quit rates for participants who identified as bisexual versus lesbian or gay did not significantly differ either in the primary, complete-case analysis (24.1% for bisexual vs. 23.0% for lesbian or gay, adjusted OR = 1.01, 95% CI = 0.51 to 2.00, p = .98; see Figure 2) or in the sensitivity analysis using the missing = smoking imputation (20.6% for bisexual vs. 18.9% for lesbian or gay, adjusted OR = 1.02, 95% CI = 0.52 to 1.97, p = .96). Both of these analyses controlled for treatment arm, three stratification factors, white race, self-reported depression, self-reported anxiety, self-reported no mental health conditions, and number of adults in the home who smoke.
Figure 2.
Complete-case, 30-day point prevalence abstinence (PPA) at 12 months with 95% confidence intervals, by sexual minority subgroup.
We also explored differences between SM and non-SM smokers (see Supplementary Table 1), and between lesbian or gay and bisexual smokers (see Supplementary Table 2), at the earlier 3- and 6-month follow-ups. All of these results were consistent with the 12-month outcomes, showing no significant differences in quit rates or data retention rates. Finally, we conducted exploratory subgroup analyses to assess whether cessation differences between SM and non-SM smokers may differ by gender. Among women, the 30-day PPA rates at 12 months for SM versus non-SM smokers were very similar in both complete-case (24.5% vs. 25.1%, adjusted OR = 0.98, 95% CI = 0.66 to 1.45) and missing = smoking (21.7% vs. 22.4%, adjusted OR = 0.95, 95% CI = 0.65 to 1.39) analyses. Among men, quit rates were numerically lower for SM versus non-SM smokers in both complete-case (21.1% vs. 26.7%, adjusted OR = 0.75, 95% CI = 0.37 to 1.50) and missing = smoking (15.4% vs. 22.0%, adjusted OR = 0.69, 95% CI = 0.35 to 1.34) analyses.
Use of Cessation Pharmacotherapy
Compared with non-SM participants, SM participants had a similar likelihood of self-reporting use of any type of cessation pharmacotherapy (35.1% vs. 40.0%, adjusted OR = 1.01, 95% CI = 0.73 to 1.39, p = .945). Some differences within classes of medications were noted. After controlling for age and hazardous drinking, SM smokers were significantly more likely than non-SM smokers to use varenicline and/or bupropion (13.7% vs. 12.6%, adjusted OR = 1.58, 95% CI = 1.02 to 2.45, p = .04). Self-reported nicotine replacement therapy use was lower in SM versus non-SM smokers (22.9% vs. 31.1%), although this difference was not statistically significant when controlling for age, positive screen for generalized anxiety disorder, no self-reported mental health conditions, and number of adults in the home who smoke (adjusted OR = 0.73, 95% CI = 0.51 to 1.04, p = .08).
Relative to gay or lesbian participants, bisexual participants had a similar likelihood of using any pharmacotherapy for cessation (32.4% for bisexual vs. 38.1% for gay or lesbian, adjusted OR = 0.97, 95% CI = 0.49 to 1.89, p = .919). Reported use of varenicline and/or bupropion was lower in bisexual versus gay or lesbian smokers (10.2% vs. 17.5%), but this difference was not statistically significant when controlling for age (adjusted OR = 0.66, 95% CI = 0.27 to 1.66, p = .380). Bisexual and gay or lesbian smokers had a similar likelihood of using nicotine replacement therapy (23.1% vs. 22.7%, adjusted OR = 1.01, 95% CI = 0.50 to 2.05, p = .984).
Discussion
To inform SM-focused tobacco control efforts, the aims of this study were to (1) compare treatment outcomes and pharmacotherapy utilization for SM and non-SM smokers to determine whether SM smokers may experience more difficulty quitting or accessing medications to support quitting, and (2) explore differences in psychosocial characteristics of SM versus non-SM smokers that may have implications for the design of targeted interventions for SM smokers. We found that SM smokers did not differ from non-SM smokers on cessation outcomes or overall use of cessation pharmacotherapy, nor were there differential quit rates within the SM subgroups of bisexual versus lesbian or gay smokers. However, SM smokers differed from non-SM smokers on most demographics, had higher prevalence of all mental health symptoms or conditions, and had greater exposure to household smoking. Bisexual smokers were more likely than lesbian or gay smokers to be younger, female, and in a long-term relationship, were less nicotine dependent, and had greater exposure to household and partner smoking, but were similar in all other respects.
The finding of no differences between SM and non-SM smokers on cessation outcomes for treatment that is not targeted for SM or SGM smokers is the fourth demonstration of such,14–16 in the largest sample to date of SM smokers. Given that this similarity in treatment outcomes has now been replicated across diverse samples and forms of treatment, the key question at this point may be less about whether overall differences exist between SM and non-SM groups and more about whether variability exists within SGM subgroups. Our exploratory subgroup analyses by gender suggested that there was more of a signal for SM-related differences in cessation outcomes among men than among women, and the magnitude of the difference was a clinically meaningful one (ie, an absolute difference of six to seven percentage points).38 This finding warrants further evaluation, particularly as other work has demonstrated that gender may moderate the relationship between SM status and tobacco use.5,6
Although commonly combined for analytic purposes (often due to sample size issues) SGM smokers are not a homogeneous group. For example, when broken down by subgroup, tobacco use prevalence rates are often higher among people who identify as bisexual than people who identify as lesbian or gay.2,5 Consequently, we conducted the first exploration of differences between bisexual and lesbian or gay smokers in terms of baseline characteristics and cessation outcomes and found several differences at baseline, but not on cessation. We note, however, that within these SM subgroups the confidence intervals for the complete-case point estimates of abstinence are wide (see Figures 1 and 2) because of the smaller sample size of the subgroups identifying as bisexual (n = 100; 30-day PPA at 12 months = 24.1%; 95% CI = 16.5 to 33.1%) and lesbian or gay (n = 112; 30-day PPA at 12 months = 23.0%; 95% CI = 15.2% to 32.5%). Owing to sample size limitations and lack of data on nonbinary gender identities, we could not test interactions between sexual orientation, gender identity, and age in relation to baseline characteristics or treatment outcomes. Such analyses could be informative given that prior work has shown differences in tobacco and nicotine product use between SGM and non-SGM individuals vary by gender identity and age.39,40
The finding of very similar quit rates among SM and non-SM participants is somewhat surprising given the nature of the baseline differences observed. On the basis of the findings that SM smokers were more likely to be low income and racial/ethnic minorities; reported substantially worse mental health on numerous indicators, which is consistent with the minority stress model41; and had greater exposure to smokers in their households, we would have predicted a markedly lower quit rate in the SM group as these characteristics are associated with lower quit rates in general population samples of smokers.19,20,42,43 We cannot determine why these poor prognostic factors were not associated with lower quit rates, but there may be buffering factors that were not measured in this study among SM smokers that offset the negative impacts of these characteristics on quitting. The presence of buffering factors may also explain the finding that, similar to past studies,14–16 there were no differences in any smoking-related variables between SM smokers and non-SM smokers at baseline, including heaviness of smoking and severity of nicotine dependence. Evaluating potential stress-buffering or protective factors that may affect smoking cessation among SM smokers, including both intrapersonal (eg, resilience) and interpersonal (eg, social support) factors, will help to better understand and address tobacco-related health disparities in this group.
The finding that quit rates did not differ by SM status does not negate the possibility that cessation outcomes could be improved for SM smokers by targeting treatment to address the unique characteristics and treatment needs of SM smokers. In addition, this type of targeting can increase receptivity to the treatment. Willingness to engage with treatment is just as important as its potential effectiveness, and evidence suggests that SM smokers have a preference for culturally targeted treatments over nontargeted treatments.10–13
Our findings provide additional evidence of younger age among treatment-seeking SM smokers14,15 and are in line with the broader finding that SGM-identified individuals in the general population are younger, on average, than non-SGM individuals, possibly due to increasing social acceptability and greater willingness to identify as SGM among younger cohorts.18,44 The finding that SM smokers—who were nearly a decade younger than non-SM smokers (mean age = 38.3 vs. 47.0)—benefit similarly from web-based cessation treatment bodes well for this intervention modality as a means of intervening early to prevent tobacco-related health disparities among SM adults. Quitting prior to the age of 40 years is associated with an almost complete reversal of the mortality risks of smoking (ie, a 9-year regain of life expectancy).45 Also promising was the finding that the proportion of smokers using pharmacotherapy to aid cessation was similar across groups and consistent with population estimates of 35%–45% of quit attempters using a medication.46 This suggests that SM smokers making a quit attempt via a web-based intervention are (1) at least equally receptive to combining behavioral treatment with a medication, and (2) similarly able to access evidence-based pharmacotherapy that can improve cessation success.
Several limitations of this study should be noted. First, the study assessments did not inquire about gender minority identities (eg, transgender, nonbinary), so we were unable to include gender minority status in the analyses. Second, the baseline survey question on sexual orientation assessed sexual identity using a limited set of descriptors (ie, heterosexual or straight, gay or lesbian, or bisexual) and excluded other potential indicators of sexual orientation, such as same-sex sexual behavior or sexual attraction. Although these limited descriptors of sexual identity are consistent with the manner in which these data have been historically collected and analyzed in the context of nicotine and tobacco research, it is worth noting that there are ongoing generational shifts in self-description of sexual identity, with younger cohorts being more likely to use alternative terms like “queer,” “pansexual,” or “asexual.” 47 And although the extant published studies on quit rates among SM or SGM smokers also use sexual identity to define SM status,14–16our findings may not be comparable to future studies that use a broader definition of the construct. In addition, generalizability is limited by the fact that (1) the participants included in this secondary analysis are a convenience sample of treatment-seeking smokers in the United States who were willing to enroll in a clinical trial and use an online cessation program, and (2) participants who identified as bisexual were predominantly (83%) women, likely due to in part to women’s greater likelihood of identifying as bisexual relative to men.6 As a consequence, it is unclear how generalizable the findings are to bisexual men. Finally, cessation outcomes were limited to self-report, with no biochemical verification. Although this design was consistent with prevailing recommendations for population-level intervention studies with no face-to-face contact at the time the study was conducted,35 self-reported quit rates may overestimate the true rate of smoking abstinence.
Despite these limitations, this is the largest sample to date of SM participants in a trial of nontargeted treatment and the first evaluation of differences between smokers who identify as bisexual versus lesbian or gay. Our findings suggested that the substantial differences in baseline characteristics of SM versus non-SM smokers and bisexual versus lesbian or gay smokers did not translate into differential treatment outcomes. Future intervention work should consider differences among both SM and gender minority subgroups and evaluate whether targeting treatment to address their unique characteristics and treatment needs could boost quit rates and/or increase uptake of effective cessation interventions.
Funding
This work was supported by a grant from the National Cancer Institute at the National Institutes of Health (grant number R01CA166646 to JBB). JLH’s writing of the manuscript was supported by a grant from the Fred Hutchinson Cancer Research Center (to JLH). The funding sources had no role in the study design; collection, analysis, and interpretation of the data; the writing of this report; or the decision to submit this manuscript for publication.
Declaration of Interests
JLH has received research support from Pfizer. JBB has served as a consultant for GlaxoSmithKline and serves on the advisory board of Chrono Therapeutics. None of the other authors have financial conflicts to disclose.
Supplementary Material
Acknowledgments
The authors would like to thank Katrina Akioka for her assistance on this project. We are also indebted to the volunteer participants for their involvement in the study.
References
- 1. Hoffman L, Delahanty J, Johnson SE, Zhao X. Sexual and gender minority cigarette smoking disparities: an analysis of 2016 Behavioral Risk Factor Surveillance System data. Prev Med. 2018;113:109–115. [DOI] [PubMed] [Google Scholar]
- 2. Emory K, Kim Y, Buchting F, Vera L, Huang J, Emery SL. Intragroup variance in lesbian, Gay, and bisexual tobacco use behaviors: evidence that subgroups matter, notably bisexual women. Nicotine Tob Res. 2016;18(6):1494–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. King BA, Dube SR, Tynan MA. Current tobacco use among adults in the United States: findings from the National Adult Tobacco Survey. Am J Public Health. 2012;102(11):e93–e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shahab L, Brown J, Hagger-Johnson G, et al. Sexual orientation identity and tobacco and hazardous alcohol use: findings from a cross-sectional English population survey. BMJ Open. 2017;7(10):e015058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wheldon CW, Kaufman AR, Kasza KA, Moser RP. Tobacco use among adults by sexual orientation: findings from the Population Assessment of Tobacco and Health study. LGBT Health. 2018;5(1):33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Corliss HL, Wadler BM, Jun HJ, et al. Sexual-orientation disparities in cigarette smoking in a longitudinal cohort study of adolescents. Nicotine Tob Res. 2013;15(1):213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ganz O, Johnson AL, Cohn AM, et al. Tobacco harm perceptions and use among sexual and gender minorities: findings from a national sample of young adults in the United States. Addict Behav. 2018;81:104–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lehavot K, Rillamas-Sun E, Weitlauf J, et al. Mortality in postmenopausal women by sexual orientation and veteran status. Gerontologist. 2016;56 (suppl 1):S150–S162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ramo DE, Meacham M, Thrul J, Belohlavek A, Sarkar U, Humfleet G. Exploring identities and preferences for intervention among LGBTQ+ young adult smokers through online focus groups. J Adolesc Health. 2019;64(3):390–397. [DOI] [PubMed] [Google Scholar]
- 11. Bruce Baskerville N, Wong K, Shuh A, et al. A qualitative study of tobacco interventions for LGBTQ+ youth and young adults: overarching themes and key learnings. BMC Public Health. 2018;18(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Matthews AK, Cesario J, Ruiz R, Ross N, King A. A qualitative study of the barriers to and facilitators of smoking cessation among lesbian, gay, bisexual, and transgender smokers who are interested in quitting. LGBT Health. 2017;4(1):24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bryant L, Damarin AK, Marshall Z. Tobacco control recommendations identified by LGBT Atlantans in a community-based participatory research project. Prog Community Health Partnersh. 2014;8(3):269–279. [DOI] [PubMed] [Google Scholar]
- 14. Covey LS, Weissman J, LoDuca C, Duan N. A comparison of abstinence outcomes among gay/bisexual and heterosexual male smokers in an intensive, non-tailored smoking cessation study. Nicotine Tob Res. 2009;11(11):1374–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grady ES, Humfleet GL, Delucchi KL, Reus VI, Muñoz RF, Hall SM. Smoking cessation outcomes among sexual and gender minority and nonminority smokers in extended smoking treatments. Nicotine Tob Res. 2014;16(9):1207–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vogel EA, Thrul J, Humfleet GL, Delucchi KL, Ramo DE. Smoking cessation intervention trial outcomes for sexual and gender minority young adults. Health Psychol. 2019;38(1):12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. LeRouge C, Ma J, Sneha S, Tolle K. User profiles and personas in the design and development of consumer health technologies. Int J Med Inform. 2013;82(11):e251–e268. [DOI] [PubMed] [Google Scholar]
- 18. Pew Research Center. A Survey of LGBT Americans: Attitudes, Experiences, and Values in Changing Times. Washington, DC: Author; 2013. [Google Scholar]
- 19. Hiscock R, Murray S, Brose LS, et al. Behavioural therapy for smoking cessation: the effectiveness of different intervention types for disadvantaged and affluent smokers. Addict Behav. 2013;38(11):2787–2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tedeschi GJ, Cummins SE, Anderson CM, Anthenelli RM, Zhuang YL, Zhu SH. Smokers with self-reported mental health conditions: a case for screening in the context of tobacco cessation services. PLoS One. 2016;11(7):e0159127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Finney Rutten LJ, Wanke K, Augustson E. Systems and individual factors associated with smoking status: evidence from HINTS. Am J Health Behav. 2005;29(4):302–310. [DOI] [PubMed] [Google Scholar]
- 22. Bricker JB, Mull KE, McClure JB, Watson NL, Heffner JL. Improving quit rates of web-delivered interventions for smoking cessation: full-scale randomized trial of WebQuit.org versus Smokefree.gov. Addiction. 2018;113(5):914–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Watson NL, Mull KE, Heffner JL, McClure JB, Bricker JB. Participant recruitment and retention in remote eHealth intervention trials: methods and lessons learned from a large randomized controlled trial of two web-based smoking interventions. J Med Internet Res. 2018;20(8):e10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 25. Kahler CW, Lachance HR, Strong DR, Ramsey SE, Monti PM, Brown RA. The commitment to quitting smoking scale: initial validation in a smoking cessation trial for heavy social drinkers. Addict Behav. 2007;32(10):2420–2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gifford EV, Kohlenberg BS, Hayes SC, et al. Acceptance-based treatment for smoking cessation. Behav Ther. 2004;35(6):689–705. [Google Scholar]
- 27. North American Quitline Consortium. The Minimal Data Set for Evaluating Quitlines. Phoenix, AZ;2012. [Google Scholar]
- 28. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 29. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. [DOI] [PubMed] [Google Scholar]
- 30. Stein MB, Roy-Byrne PP, McQuaid JR, et al. Development of a brief diagnostic screen for panic disorder in primary care. Psychosom Med. 1999;61(3):359–364. [DOI] [PubMed] [Google Scholar]
- 31. Lang AJ, Stein MB. An abbreviated PTSD checklist for use as a screening instrument in primary care. Behav Res Ther. 2005;43(5):585–594. [DOI] [PubMed] [Google Scholar]
- 32. Connor KM, Kobak KA, Churchill LE, Katzelnick D, Davidson JR. Mini-SPIN: a brief screening assessment for generalized social anxiety disorder. Depress Anxiety. 2001;14(2):137–140. [DOI] [PubMed] [Google Scholar]
- 33. Babor TF, de la Fuente JR, Saunders J, Grant M.. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Health Care. Geneva: World Health Organization; 1992. [Google Scholar]
- 34. Sanchez-Craig M, Wilkinson DA, Davila R. Empirically based guidelines for moderate drinking: 1-year results from three studies with problem drinkers. Am J Public Health. 1995;85(6):823–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4(2):149–159. [DOI] [PubMed] [Google Scholar]
- 36. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing 2017. https://www.R-project.org/. Accessed March 26, 2019.
- 37. Venables WN, Ripley BD.. Modern Applied Statistics With S. 4th ed. New York, NY: Springer; 2002. [Google Scholar]
- 38. West R. The clinical significance of “small” effects of smoking cessation treatments. Addiction. 2007;102(4):506–509. [DOI] [PubMed] [Google Scholar]
- 39. McCabe SE, Matthews AK, Lee JGL, Veliz P, Hughes TL, Boyd CJ. Tobacco use and sexual orientation in a national cross-sectional study: age, race/ethnicity, and sexual identity-attraction differences. Am J Prev Med. 2018;54(6):736–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kidd JD, Dolezal C, Bockting WO. The relationship between tobacco use and legal document gender-marker change, hormone use, and gender-affirming surgery in a United States sample of trans-feminine and trans-masculine individuals: implications for cardiovascular health. LGBT Health. 2018;5(7):401–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Meyer IH, Frost DM. Minority stress and the health of sexual minorities. In: Patterson CJ, D’Augelli AR, eds. Handbook of Psychology and Sexual Orientation. New York, NY: Oxford University Press; 2013:252–266. [Google Scholar]
- 42. Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence. Clinical Practice Guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2000. [Google Scholar]
- 43. Trinidad DR, Pérez-Stable EJ, White MM, Emery SL, Messer K. A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. Am J Public Health. 2011;101(4):699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cahill S, Geffen S, Vance A, Wang T, Barrera J.. Equality and Equity: Advancing LGBT Community in Massachusetts. Boston, MA: Boston Indicators and The Fenway Institute; 2018. [Google Scholar]
- 45. Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328(7455):1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kasza KA, Cummings KM, Carpenter MJ, Cornelius ME, Hyland AJ, Fong GT. Use of stop-smoking medications in the United States before and after the introduction of varenicline. Addiction. 2015;110(2):346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kahn E, Johnson A, Lee M, Miranda L.. LGBTQ Youth Report. Washington, D.C.: Human Rights Campaign Foundation Public Education and Research Program; 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.