Abstract
Introduction
Young adults have high combustible cigarette and e-cigarette use rates, and low utilization of evidence-based smoking cessation strategies compared to older adults. It is unknown whether young adults who try to quit smoking without assistance, with evidence-based strategies, or with e-cigarettes, are equally successful compared to older adults.
Aims and Methods
This analysis used a population-based sample from the Population Assessment of Tobacco and Health study of young adult (aged 18–24, n = 745) and older adult (aged 25–64, n = 2057) established cigarette smokers at Wave 1 (2013–2014) who reported having made a quit attempt at Wave 2 (2014–2015). Cessation strategies were: behavioral therapy, pharmacotherapy, product substitution, 2+ strategies, and unassisted. Logistic regression estimated associations between cessation strategy and short-term cessation status at Wave 2 (quit, no quit); multinomial logistic regression predicted long-term cessation patterns at Waves 2 and 3 (sustained quit, temporary quit, delayed quit, no quit).
Results
No cessation strategy (ref: unassisted) significantly predicted short-term cessation. No cessation strategy (ref: unassisted) significantly predicted long-term cessation patterns for young adults. Substitution with e-cigarettes predicted short-term cessation for older daily smokers of ≥5 cigarettes/day (adjusted odds ratio [AOR]: 1.70; 95% confidence interval: 1.08, 2.67) but did not predict long-term cessation patterns.
Conclusions
Despite differences in cessation strategy use between young and older adult smokers, strategy effectiveness largely did not differ by age group. No strategy examined, including e-cigarettes, was significantly associated with successful cessation for young adults. More work is needed to identify effective interventions that help young adult smokers quit.
Implications
(1) Neither behavioral support, pharmacotherapy, nor product substitution was associated with short-term cessation for young or older adults compared to quitting unassisted. (2) Neither behavioral support, pharmacotherapy, nor product substitution was associated with longer-term cessation for young or older adults compared to quitting unassisted. (3) Substitution with e-cigarettes predicted short-term cessation for older daily smokers of ≥5 cigarettes/day but was not associated with longer-term cessation.
Introduction
Young adulthood is a key transition time for tobacco use, during which many young adults who have experimented with tobacco either stop or develop longer-term addiction.1 Early tobacco cessation has been found to reduce the risk of death from tobacco-related disease and extend life expectancy compared to continued smoking.2–4 Many young adult smokers are interested in quitting smoking and make quit attempts5; however young adult smokers who try to quit are less likely to use evidence-based cessation strategies than their older adult counterparts and are more likely to try to quit unassisted.6–10 A recent study found that young adults frequently reported using e-cigarettes for their most recent quit attempt (26.3% used e-cigarettes vs. 6.3% nicotine replacement therapy).10
There is evidence that smoking cessation interventions are equally efficacious for young adults and the general adult population.11 However, although nicotine replacement therapy and the prescription drugs varenicline and bupropion have been demonstrated effective in clinical trials,12,13 evidence of their effectiveness in real-world settings is mixed. Some studies have demonstrated pharmacotherapy in the absence of behavioral counseling to be effective14 while others have found it only effective in combination with behavioral counseling.15 Only a few studies have looked at cessation patterns longitudinally,16,17 including a recent study reporting that effects of pharmacotherapy aids varied by product and by time point for evaluating abstinence.18 Much of this work has studied adults in the United Kingdom, Canada, and France,14,15,18 and often occurred before e-cigarettes were popular.
Since the emergence of e-cigarettes, several clinical trials and observational studies has assessed their effectiveness for smoking cessation, also with mixed findings.19–21 A recent comprehensive report from the National Academies of Sciences, Engineering, and Medicine concluded that there was limited evidence that e-cigarettes are effective smoking cessation aids.22 Since that report, a clinical trial in England reported that, coupled with 4 weekly counseling sessions, e-cigarettes were more effective than nicotine replacement therapy at 12-month abstinence.21
E-cigarettes vary in nicotine concentration, power, flavor, and patterns of use, and almost all smokers who use e-cigarettes to quit do not receive formal cessation counseling. Examining whether e-cigarettes predict cessation outside of trials is critical to understanding their real-world impact. Two recent studies examined cessation using the first two waves of the Population Assessment of Tobacco and Health (PATH) study. Benmarhnia and colleagues found that use of pharmaceutical aids did not predict persistent (≥30 day) cigarette abstinence at Wave 2.23 They also found that cigarette cessation attempts using e-cigarettes were associated with abstinence, but not with reduction in cigarette consumption for the non-abstinent.23 Berry and colleagues reported that transition to daily e-cigarette use at Wave 2 was associated with cigarette cessation and reduction in cigarettes smoked per day,24 although this study did not isolate individuals who used e-cigarettes intentionally for a quit attempt.
To our knowledge, no observational studies of cessation strategy use have looked specifically at young adults, and some previous studies omitted them.15,21 Given the differences between young adult and older adult smokers, the high rate of e-cigarette use among young adults,25 and the importance of cessation in young adulthood, longitudinal, population studies of young adult quit attempts in the United States are needed.
This study used three waves of the PATH study (2013–2016) to assess the effectiveness of behavioral support, pharmacotherapy, and product substitution on short- and longer-term patterns of cessation and compared effectiveness for young adults and older adults.
Materials and Methods
Participants and Procedures
We used a population-based sample of young adults (age 18–24) and older adults (age 25–64) who were established smokers at Wave 1 of the PATH study and were surveyed at Wave 2 (2014–2015), and a subsample who were surveyed at Wave 3 (2015–2016).26 The PATH study was administered via in-home computer-assisted interviews and over-sampled young adults, tobacco users, and African Americans. Details on the administration of the PATH study have been published elsewhere.27 The present study used the PATH Study’s Public-Use Files and was certified exempt by the University of California, San Francisco’s Institutional Review Board.
Measures
Cigarette Use and Cessation Outcomes
An individual was labeled a current established smoker at each wave if they had smoked more than 100 cigarettes in their lifetime and currently smoked every day or some days at the time of survey administration. This study is limited to current established smokers at Wave 1.
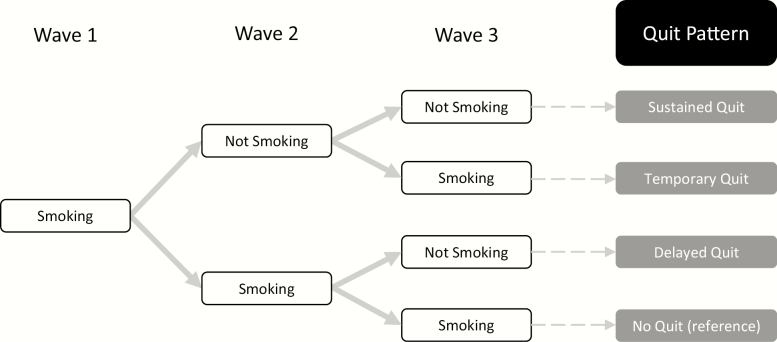
At Waves 2 and 3, an individual was defined as having quit if they were not a current established smoker at that wave. We combined current established smoking status at Waves 2 and 3 to identify four cessation patterns over time: sustained quit (Wave 2 not smoking, Wave 3 not smoking), temporary quit (Wave 2 not smoking, Wave 3 smoking), delayed quit (Wave 2 smoking, Wave 3 not smoking), and a reference category of no quit (Wave 2 smoking, Wave 3 smoking) (see Figure 1).
Figure 1.
Cessation patterns at Waves 2 and 3 were defined using current established smoking status at each wave. If an individual was not a current established smoker at either wave they were designated as having “quit.” At Wave 2, each participant reported having made a cessation attempt between Waves 1 and 2.
Cigarette Cessation Strategies
We identified respondents in Wave 2 as having made a quit attempt if they answered one or more, did not know, or refused to answer the question “In total, how many times in the past 12 months have you tried to quit [PRODUCT(s)] completely?” and had stopped smoking or using tobacco for 1 day or longer because they were trying to quit. In Wave 2, individuals who had made a quit attempt were asked about the strategies they used the last time they tried to quit. We grouped cessation strategies into four categories: behavioral support, pharmacotherapy (including nicotine replacement therapy and prescription drugs), product substitution (complete or incomplete switching to another tobacco product), and unassisted quitting (see Table A1, available at Nicotine and Tobacco Research online for definitions). Due to a limited number of responses, quit attempts using non-cigarette combustible tobacco products, smokeless tobacco, and hookah, were combined with e-cigarettes for primary analyses. We defined respondents as making an unassisted quit attempt if they did not use behavioral support, pharmacotherapy, or product substitution during their last quit attempt.
Our primary predictor had five categories: behavioral support alone, pharmacotherapy alone, product substitution alone, two or more strategies, and unassisted (reference category). Given previous findings that behavioral support and pharmacotherapy are more effective together than alone,15 a second version of this variable separated behavioral support and pharmacotherapy together from other combinations of two or more strategies. To isolate e-cigarette use, a third version divided substitution into substitution using e-cigarettes (including in combination with another product) and substitution using a tobacco product other than e-cigarettes.
The PATH study asked about e-cigarette cessation attempts and other tobacco cessation attempts separately at Wave 2. Established smokers at Wave 1 with no other established use at Wave 1 or 2 were asked exclusively about cessation strategies the last time they tried to quit cigarette smoking. Established users of cigarettes and e-cigarettes at Wave 1 or 2 were asked about cessation strategies the last time they tried to quit each product separately. If a respondent used two or more non-e-cigarette tobacco products, they were asked about cessation strategies the last time they tried to quit tobacco use overall and asked separately about the last time they tried to quit e-cigarettes. For this subset of poly-tobacco users, we cannot isolate their last cigarette cessation attempt. Because of this survey design complexity, we examined the most recent cessation attempt for each respondent, regardless of what tobacco product(s) they were asked about. Thus, our study describes tobacco cessation strategies of cigarette smokers. We conducted a robustness check with cigarette-only smokers to test the validity of these estimates.
Covariates
All covariates were measured at Wave 1. To account for nicotine dependence, which has been negatively associated with cessation,28,29 we included a binary indicator of whether an individual was a light or intermittent smoker. We also included an indicator of whether an individual was a poly-tobacco user (established use of any non-cigarette tobacco product in addition to cigarette use) which has been associated with nicotine dependence30 and with choice of cessation strategy.10Current established use of non-cigarette tobacco products was defined as whether a respondent had ever used a non-cigarette tobacco product fairly regularly and currently used that product every day or some days. A respondent was coded as a light or intermittent smoker if they were a non-daily smoker or were a daily smoker and smoked on average 5 cigarettes or fewer/day (ref: daily smoker and >5 cigarettes/day).31–35 Previous research has demonstrated that previous quit attempts are a marker of motivation to quit, but multiple failed attempts could also signify difficulties in quitting permanently and relapse to smoking.36,37 We included the number of quit attempts reported in the last 12 months, right censored with a maximum of 52 attempts. We included a binary measure indicating whether the respondent lived with anyone who used tobacco.
Demographic and socioeconomic measures included: sex, race, and ethnicity (Non-Hispanic White, Non-Hispanic African American or Black, and other race); education (less than high school education and high school education or equivalent and above); lesbian, gay, bisexual, or other non-heterosexual sexual identity; and financial instability (unable to pay important bills on time in the past 30 days because of shortage of money).
There were 3121 individuals who were current established cigarette smokers at Wave 1, reported making a quit attempt at Wave 2, and were under the age 65. We removed 68 cases because of missing data on one or more cessation strategy and 251 because of missing data on one or more covariate. The final sample included 2802 individuals. There were no significant differences in cessation status at Wave 2 or cessation strategy choice between the study sample and those with one or more missing covariate (results not shown).
Analysis
We estimated short (Wave 2)- and longer (Waves 2 and 3)-term cessation for young adult and older adult current established smokers at Wave 1 who reported having made one or more quit attempts at Wave 2.
Analysis 1: Cessation Status at Wave 2
Our first two models used logistic regression to estimate the association between cessation strategy (ref: unassisted quit attempt) and quit status at Wave 2. The second model introduced an interaction term between cessation strategy and age group to isolate associations for young adults. From the interaction model, we calculated the odds ratio and confidence interval (CI) for the association between each cessation strategy and quit status for young adults using the lincom command in Stata. Analyses were conducted using the 2802 respondents who had no missing data for any of the Wave 1 covariates, Wave 2 cessation strategy variables, and smoking status at either Wave (young adults [YA]: 745; older adults [OA]: 2057).
Analysis 2: Cessation Patterns at Waves 2 and 3
Our third model used multinomial logistic regression to estimate the association between cessation strategy and four cessation patterns at Waves 2 and 3 (sustained quit, temporary quit, delayed quit vs. no quit). Our fourth model introduced an interaction term between cessation strategy and age group. Lincom calculations were repeated. Analyses were conducted using the 2502 respondents with no missing data in predictors or outcomes at Waves 1, 2, and 3 (YA: 662; OA: 1840).
All models controlled for age group, demographic and socioeconomic characteristics, cigarette and other tobacco use, dependence, and number of past-year quit attempts at Wave 1.
Robustness Checks and Supplemental Analyses
As a robustness check, we replicated models 1 and 3 with established users of only cigarettes at Wave 1. This check (1) provided a clean set of models where the cessation strategy reports referred to cigarette cessation specifically and (2) helped to identify whether any observed differences in strategy use by age were driven by differences in poly-tobacco use prevalence between age groups. Sample size constraints prevented us from reporting cigarette-only smoker results for age interaction models.
We re-estimated models 1 and 3 using (1) a six-category cessation strategy variable with combined behavioral support and pharmacotherapy and then (2) using a cessation strategy variable that separated substitution with and without e-cigarettes. Because strategies might have different effects for light and heavy smokers,38 we re-estimated models 1 and 3 including an interaction term between smoking intensity cessation strategy, using the product substitution variable that separated e-cigarettes. We stratified the Wave 2 analysis by age. Sample size constraints prevented us from stratifying the Wave 2 and 3 analysis by age.
Data cleaning and analyses were conducted using Stata 14. Descriptive statistics were calculated for the Wave 2 sample and weighted using Wave 2 respondent-level sample weights (provided by the PATH study). Statistical tests for Wave 2 cessation status (Wave 2 and 3 cessation patterns) were weighted with Wave 2 (Wave 3 “all wave”) replicate weights using the brr Stata command for balanced repeated replication.
Results
Sample Description (Table 1)
Table 1.
PATH Study Descriptive Statistics for US Young and Older Adults Who Reported a Quit Attempt at Wave 2
| Young adults (18–24) (n = 745) | Older adults (25–64) (n = 2057) | All Adults (18–64) (n = 2802) | |
|---|---|---|---|
| Weighted% | Weighted% | Weighted% | |
| Outcomes a | |||
| Cessation (Wave 2) | 23.67 | 20.02 | 20.69 |
| Cessation (Wave 3) | 24.43 | 21.87 | 22.35 |
| Cessation Patterns (Waves 2 and 3)b | |||
| Sustained quit | 13.24 | 12.10 | 12.31 |
| Temporary quit | 11.12 | 7.06 | 7.82 |
| Delayed quit | 11.19 | 9.77 | 10.03 |
| No quit | 64.46 | 71.07 | 69.84 |
| Cessation strategies (Wave 2) | |||
| Behavioral support alone | 1.95 | 2.40 | 2.32 |
| Pharmacotherapy alone | 2.75 | 15.10 | 12.83 |
| Product substitution alone | 26.88 | 21.06 | 22.13 |
| With e-cigarettes | 22.63 | 18.99 | 19.66 |
| Without e-cigarettes | 4.25 | 2.07 | 2.47 |
| 2+ strategies | 6.02 | 10.13 | 9.38 |
| Behavioral + pharma | 2.47 | 1.37 | 2.26 |
| Unassisted | 62.39 | 51.31 | 53.35 |
| Covariates (Wave 1) | |||
| Female (ref: male) | 43.58 | 46.42 | 45.90 |
| Race/ethnicity | |||
| NH White (reference) | 76.69 | 75.63 | 75.82 |
| NH Black or Afr. Am. | 11.74 | 16.09 | 15.29 |
| Other race/ethnicity | 11.57 | 8.28 | 8.88 |
| LGB+ (ref: heterosexual) | 13.16 | 6.77 | 7.95 |
| Unable to pay bills | 26.99 | 30.82 | 30.12 |
| Education, high school+ | 84.70 | 87.16 | 86.71 |
| Uses non-cigarette tobacco | 39.33 | 22.32 | 25.45 |
| Lives with tobacco user | 67.40 | 51.55 | 54.46 |
| Light or intermittent smoker | 46.84 | 32.61 | 35.22 |
| Mean | Mean | Mean | |
| # of quit attempts | 2.34 | 2.34 | 2.34 |
NH = Non-Hispanic; OA = older adults; YA = young adults; LGB = lesbian, gay, bisexual.
aWeighted percentages report the percent of respondents who had quit at Wave 2 (of all Wave 1 smokers who made a quit attempt at Wave 2), who had quit at Wave 3, and who had each cessation pattern across Waves 2 and 3.
bReported for Wave 1 smokers who made a quit attempt at Wave 2 with Wave 3 follow-up, n = 2502 (YA: 662; OA: 1840).
A total of 23.67% of young adult and 20.02% of older adult Wave 1 smokers were not smoking at Wave 2 and 24.43% of young adult and 21.87% of older adult Wave 1 smokers were not smoking at Wave 3. Of the 2502 smokers with observations at all waves, 12.31% were classified as sustained quitting (YA: 13.24%; OA: 12.1%), 7.82% as temporary quitting (YA: 11.12%; OA: 7.06%), 10.03% as delayed quitting (YA: 11.19%; OA: 9.77%), and the remaining 69.84% reported smoking at both waves (YA: 64.46%; OA: 71.07%).
Young adults were substantially less likely to use pharmacotherapy compared to older adults, and both groups used product substitution, largely with e-cigarettes, most often. A total of 62.39% of young adult smokers tried to quit unassisted compared to 51.31% of older adult smokers. Young adult smokers had higher rates of poly-tobacco use, living with a tobacco user, and light or intermittent smoking. Young and older adults reported, on average, the same number of past-12-month quit attempts.
Analysis 1: Wave 2 Cessation Status
Table 2 reports regression results for Wave 2 cessation status. None of the cessation strategies significantly predicted Wave 2 cessation. There was no significant association between age group and Wave 2 cessation, suggesting that after adjusting for differences between age groups and confounders, young adult and older adult smokers were just as likely to have successfully quit in the short term (Table 2, “Model 1”). Furthermore, interaction terms between cessation strategies and age group were not significant (Table 2, “Model 2”), suggesting no difference in the association between cessation strategy use and cessation success for young and older adults.
Table 2.
Cessation Status at Wave 2 (2014–2015) of the PATH Study for US Young and Older Adult Smokers Who Reported a Quit Attempt at Wave 2 (n = 2802) by Cessation Strategy
| Weighted%a | Model 1 | Model 2 | |||
|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | ||
| Outcome: quit at Wave 2 | |||||
| Cessation strategies | |||||
| Unassisted | 21.2 | reference | reference | ||
| Behavioral support alone | 18.25 | 0.89 | [0.38, 2.08] | 0.66 | [0.22, 2.00] |
| Pharmacotherapy alone | 16.31 | 0.81 | [0.56, 1.18] | 0.84 | [0.57, 1.23] |
| Product substitution alone | 23.26 | 1.21 | [0.91, 1.61] | 1.35 | [0.97, 1.90] |
| 2+ strategies | 18.27 | 0.91 | [0.63, 1.33] | 1.04 | [0.69, 1.59] |
| Strategies*age interaction | |||||
| Behavioral support alone*age | 3.57 | [0.53, 23.87] | |||
| Pharmacotherapy alone*age | 1.04 | [0.33, 3.34] | |||
| Product substitution alone*age | 0.60 | [0.36, 1.02] | |||
| 2+ strategies*age | 0.33 | [0.09, 1.14] | |||
| Covariates | |||||
| Female | 1.02 | [0.82, 1.27] | 1.02 | [0.81, 1.27] | |
| LGB+ | 0.78 | [0.51, 1.19] | 0.78 | [0.51, 1.20] | |
| Race/ethnicity | |||||
| NH Black or Afr. Am. | 0.56* | [0.40, 0.77] | 0.56* | [0.41, 0.78] | |
| Other race/ethnicity | 0.86 | [0.59, 1.26] | 0.85 | [0.58, 1.24] | |
| Unable to pay bills | 0.76* | [0.61, 0.94] | 0.75* | [0.60, 0.94] | |
| Education, high school+ | 1.79* | [1.21, 2.66] | 1.76* | [1.19, 2.61] | |
| Uses non-cigarette tobacco | 1.03 | [0.80, 1.33] | 1.03 | [0.80, 1.34] | |
| Lives with tobacco user | 0.85 | [0.67, 1.09] | 0.85 | [0.66, 1.08] | |
| Light or intermittent smoker | 2.02* | [1.61, 2.53] | 2.02* | [1.61, 2.55] | |
| # quit attempts | 0.99 | [0.95, 1.04] | 0.99 | [0.95, 1.04] | |
| Young adult | 1.11 | [0.85, 1.45] | 1.30 | [0.94, 1.80] | |
| Constant | 0.15 | [0.09, 0.24] | 0.15 | [0.09, 0.23] | |
| N | 2802 | 2802 | |||
| F statistic | 6.69 | 4.99 | |||
CI = confidence interval; NH = Non-Hispanic.
aWeighted percentages report the percentage of respondents from each quit attempt category who had quit at Wave 2.
*p < .05.
Analysis 2: Wave 2 and 3 Cessation Patterns
Table 3 reports regression results for Wave 2 and 3 cessation patterns. Consistent with findings from Analysis 1, none of the cessation strategies significantly predicted cessation patterns after adjustment. Young adults were significantly more likely to report temporary quitting than not quitting, compared to older adults (Table 3, “Model 3”); age group did not predict any other cessation pattern.
Table 3.
Cessation Patterns at Wave 2 (2014–2015) and Wave 3 (2015–2016) of the PATH Study for US Young and Older Adult Smokers Who Reported a Quit Attempt at Wave 2 (n = 2502) by Cessation Strategy
| Weighted%a | Model 3b | Model 4b | |||
|---|---|---|---|---|---|
| RRR | 95% CI | RRR | 95% CI | ||
| Ref: no quit | |||||
| Cessation strategies | |||||
| Unassisted | 68.90 | ||||
| Behavioral support alone | 81.30 | ||||
| Pharmacotherapy alone | 74.12 | ||||
| Product substitution alone | 69.00 | ||||
| 2+ strategies | 68.91 | ||||
| Outcome 1: sustained quit | |||||
| Cessation strategies | |||||
| Unassisted | 13.30 | reference | reference | ||
| Behavioral support alone | 11.83 | 0.98 | [0.34, 2.80] | 0.65 | [0.18, 2.33] |
| Pharmacotherapy alone | 8.57 | 0.69 | [0.40, 1.19] | 0.70 | [0.40, 1.23] |
| Product substitution alone | 12.31 | 0.99 | [0.68, 1.43] | 1.10 | [0.70, 1.74] |
| 2+ strategies | 12.99 | 1.09 | [0.64, 1.87] | 1.22 | [0.68, 2.19] |
| Strategies*age interaction | |||||
| Behavioral support alone*age | 4.81 | [0.34, 67.84] | |||
| Pharmacotherapy alone*age | 1.22 | [0.22, 6.91] | |||
| Product substitution alone*age | 0.60 | [0.26, 1.38] | |||
| 2+ strategies*age | 0.32 | [0.04, 2.71] | |||
| Covariates | |||||
| Female | 1.05 | [0.80, 1.36] | 1.04 | [0.80, 1.36] | |
| LGB+ | 0.73 | [0.44, 1.22] | 0.73 | [0.44, 1.22] | |
| Race/ethnicity | |||||
| NH Black or Afr. Am. | 0.49* | [0.31, 0.80] | 0.50* | [0.31, 0.80] | |
| Other race/ethnicity | 1.00 | [0.57, 1.76] | 1.00 | [0.56, 1.77] | |
| Unable to pay bills | 0.59* | [0.43, 0.81] | 0.59* | [0.43, 0.81] | |
| Education, high school+ | 1.65 | [0.97, 2.78] | 1.62 | [0.95, 2.74] | |
| Uses non-cigarette tobacco | 1.19 | [0.88, 1.61] | 1.20 | [0.89, 1.62] | |
| Lives with tobacco user | 0.68* | [0.52, 0.89] | 0.67* | [0.51, 0.89] | |
| Light or intermittent smoker | 2.53* | [1.93, 3.32] | 2.53* | [1.92, 3.34] | |
| # quit attempts | 0.97 | [0.92, 1.03] | 0.97 | [0.93, 1.03] | |
| Young adult | 1.06 | [0.73, 1.55] | 1.22 | [0.78, 1.92] | |
| Constant | 0.12 | [0.07, 0.23] | 0.12 | [0.07, 0.23] | |
| Outcome 2: temporary quit | |||||
| Cessation strategies | |||||
| Unassisted | 7.61 | reference | reference | ||
| Behavioral support alone | 2.61c | 0.33 | [0.04, 2.60] | 0.33 | [0.02, 5.06] |
| Pharmacotherapy alone | 6.51 | 0.95 | [0.58, 1.58] | 1.04 | [0.61, 1.77] |
| Product substitution alone | 10.09 | 1.35 | [0.94, 1.95] | 1.67* | [1.07, 2.59] |
| 2+ strategies | 5.82 | 0.81 | [0.39, 1.70] | 1.02 | [0.47, 2.20] |
| Strategies*age interaction | |||||
| Behavioral support alone*age | 1.33 | [0.03, 51.08] | |||
| Pharmacotherapy alone*age | 0.76 | [0.09, 6.28] | |||
| Product substitution alone*age | 0.47* | [0.22, 0.99] | |||
| 2+ strategies*age | 0.17 | [0.02, 1.97] | |||
| Covariates | |||||
| Female | 0.98 | [0.66, 1.45] | 0.97 | [0.65, 1.43] | |
| LGB+ | 0.92 | [0.45, 1.87] | 0.91 | [0.45, 1.87] | |
| Race/ethnicity | |||||
| NH Black or Afr. Am. | 0.55* | [0.35, 0.87] | 0.55* | [0.35, 0.88] | |
| Other race/ethnicity | 0.60 | [0.33, 1.09] | 0.59 | [0.32, 1.08] | |
| Unable to pay bills | 1.09 | [0.81, 1.47] | 1.10 | [0.81, 1.49] | |
| Education, high school+ | 2.01* | [1.06, 3.80] | 1.97* | [1.04, 3.73] | |
| Uses non-cigarette tobacco | 1.04 | [0.69, 1.58] | 1.04 | [0.69, 1.57] | |
| Lives with tobacco user | 1.02 | [0.69, 1.52] | 1.01 | [0.68, 1.50] | |
| Light or intermittent smoker | 1.72* | [1.19, 2.50] | 1.72* | [1.18, 2.50] | |
| # quit attempts | 1.02 | [0.98, 1.07] | 1.02 | [0.98, 1.06] | |
| Young adult | 1.59* | [1.13, 2.23] | 2.14* | [1.35, 3.37] | |
| Constant | 0.04 | [0.02, 0.09] | 0.04 | [0.02, 0.09] | |
| Outcome 3: delayed quit | |||||
| Cessation strategies | |||||
| Unassisted | 10.18 | reference | reference | ||
| Behavioral support alone | 4.26c | 0.41 | [0.06, 2.79] | 0.33 | [0.03, 4.37] |
| Pharmacotherapy alone | 10.80 | 1.20 | [0.72, 2.00] | 1.26 | [0.75, 2.12] |
| Product substitution alone | 8.60 | 0.82 | [0.54, 1.25] | 0.89 | [0.55, 1.44] |
| 2+ strategies | 12.27 | 1.28 | [0.76, 2.16] | 1.08 | [0.60, 1.96] |
| Strategies*age interaction | |||||
| Behavioral support alone*age | 2.89 | [0.07, 118.98] | |||
| Pharmacotherapy alone*age | 0.13 | [0.01, 1.91] | |||
| Product substitution alone*age | 0.69 | [0.32, 1.52] | |||
| 2+ strategies*age | 2.28 | [0.55, 9.52] | |||
| Covariates | |||||
| Female | 0.99 | [0.72, 1.35] | 0.99 | [0.72, 1.36] | |
| LGB+ | 1.21 | [0.72, 2.02] | 1.20 | [0.72, 1.99] | |
| Race/ethnicity | |||||
| NH Black or Afr. Am. | 0.47* | [0.29, 0.75] | 0.47* | [0.30, 0.75] | |
| Other race/ethnicity | 0.75 | [0.40, 1.39] | 0.76 | [0.41, 1.41] | |
| Unable to pay bills | 0.85 | [0.59, 1.22] | 0.84 | [0.59, 1.20] | |
| Education, high school+ | 1.86* | [1.11, 3.11] | 1.88* | [1.12, 3.17] | |
| Uses non-cigarette tobacco | 1.37 | [0.96, 1.97] | 1.38 | [0.96, 1.99] | |
| Lives with tobacco user | 0.74 | [0.54, 1.00] | 0.73 | [0.54, 1.00] | |
| Light or intermittent smoker | 2.51* | [1.81, 3.49] | 2.48* | [1.78, 3.45] | |
| # quit attempts | 0.98 | [0.95, 1.01] | 0.98 | [0.95, 1.01] | |
| Young adult | 1.13 | [0.79, 1.63] | 1.16 | [0.75, 1.80] | |
| Constant | 0.08 | [0.04, 0.13] | 0.07 | [0.04, 0.13] | |
| N | 2502 | 2502 | |||
| F statistic | 4.82 | 3.74 | |||
CI = confidence interval; NH = Non-Hispanic.
aWeighted percentages report the percentage of respondents from each quit attempt category who had the specific cessation outcome (eg of respondents who reported trying to quit unassisted, 68.9% had not quit at either wave).
bEstimates from multinomial logistic regression with four-category outcome variable. Reference group: no quit at both Waves 2 and 3.
cEstimates unstable due to limited sample size.
*p < .05.
The interaction between age and substitution (Table 3, “Model 3”) was significant; for older adults, using product substitution predicted temporary quitting compared to not quitting at either wave (Table 3, “Model 3”). Lincom calculations revealed no significant association between substitution and temporary quitting for young adults. Young adults who tried to quit unassisted, however, were more likely to report temporary quitting compared to older adults who tried to quit unassisted.
Covariates
Light or intermittent smoking positively predicted all cessation outcomes: Wave 2 cessation, sustained quitting, temporary quitting, and delayed quitting. Respondents who lived with a tobacco user were less likely to have sustained quitting than those who did not. Neither poly-tobacco use nor the number of quit attempts was associated with cessation. African American respondents were consistently less likely to have quit. Inability to pay bills and education status also negatively predicted quitting (Tables 2 and 3).
Robustness Checks and Supplemental Analyses
Results of robustness checks and supplemental analyses are available in the Supplemental Material, available at Nicotine and Tobacco Research online.
Cigarette-Only Smokers (Tables A2 and A3, Available at Nicotine and Tobacco Research Online)
The results using cigarette-only smokers were largely consistent with the full-sample models. Of note, cigarette-only smokers who used product substitution to try to quit were less likely to be delayed quitters compared to not quitting at all (relative risk ratio [RRR]: 0.56, 95% CI: 0.33, 0.94).
Behavioral Support and Pharmacotherapy (Tables A4 and A5, Available at Nicotine and Tobacco Research Online)
We found no significant association between combined behavioral support and pharmacotherapy and either Wave 2 cessation status (AOR: 0.61; 95% CI: 0.23, 1.61) or Wave 2 and 3 cessation patterns (sustained quitting – RRR: 0.58, 95% CI: 0.21, 1.56; temporary quitting – RRR: 0.44, 95% CI: 0.44, 2.11; delayed quitting – RRR: 0.42, 95% CI: 0.12, 1.43).
Substitution With E-cigarettes (Tables A4 and A5, Available at Nicotine and Tobacco Research Online)
We found no significant association between substitution with e-cigarettes and either Wave 2 cessation status (AOR: 1.25; 95% CI: .91, 1.72) or Wave 2 and 3 cessation patterns (sustained quitting – RRR: 1.02, 95% CI: 0.69, 1.51; temporary quitting – RRR: 1.35, 95% CI: 0.91, 2.01; delayed quitting – RRR: 0.83, 95% CI: 0.53, 1.31).
Light and Intermittent Smokers (Tables A6 and A7, Available at Nicotine and Tobacco Research Online)
E-cigarette substitution predicted Wave 2 cessation for regular or heavy smokers (AOR: 1.52; 95% CI: 1.04, 2.23) but not for light or intermittent smokers; estimating this model on young adult and older adult subsamples revealed a significant relationship only for older adults (AOR: 1.70; 95% CI: 1.08, 2.67, n = 2057) and not for young adults (AOR: 0.94, 0.51, 1.73). In the longer-term models, e-cigarette substitution positively predicted temporary quitting for regular or heavy smokers (RRR: 1.61, 95% CI: 1.01, 2.56), but not sustained or delayed quitting.
Discussion
We used three waves of the PATH study data to investigate cessation strategy effectiveness in the real world for young and older adult established cigarette smokers who had tried to quit smoking. Across four model specifications that adjusted for other tobacco use, nicotine dependence, past quit attempts, and socioeconomic characteristics, we found consistent evidence that cessation strategy use was not significantly associated with short- and longer-term cessation, with one exception. Product substitution was positively associated with temporary quitting for older adults.
In line with previous research suggesting similar efficacy of smoking cessation interventions for young adults and the general population,11 we found few differences in cessation patterns for young adult and older adult smokers who tried to quit. Despite differences in the profile of young and older adult smokers, we found that among smokers who tried to quit, young adults were just as likely to have successfully quit in the short term as older adults and young adults were more likely than older adults to have made a temporary quit, compared to no cessation in either wave. Unfortunately, our analyses also showed that most cessation strategies used in the real world were no more effective than unassisted quitting, which is also consistent with previous research. Moreover, and conflicting with prior studies,15 we found that combined pharmacotherapy and behavioral counseling was no more effective than unassisted quitting either.
Compared to other population-based studies, which have found past-year quit rates of around 7.4% (based on the National Health Interview Survey),39 the quit rates of more than 20% seem high. However, it should be noted that our sample is limited to participants who had made a serious quit attempt in the past year, which only about 50% of the smokers in the general population do,39 which is likely the reason we observe higher success.
In our analyses, 26.88% of young adults reported using another tobacco product for their last cessation attempt, but product substitution did not predict cessation, regardless of smoking intensity. Product substitution was negatively associated with delayed quitting for cigarette-only smokers and positively predicted temporary quitting for older adult smokers. Examining e-cigarette effectiveness by smoking intensity, we found that substitution with e-cigarettes was associated with temporary quitting for older adult smokers of more than 5 cigarettes a day. Together, our findings suggest that product substitution is not effective for long-term smoking cessation and, for cigarette-only smokers, use of e-cigarettes might suppress longer-term cessation outcomes, which is consistent with the bulk of previous research on the utility of e-cigarettes for smoking cessation.20
We found e-cigarettes to be associated with short-term cessation only for one subgroup of the sample, whereas the study most similar to ours found using e-cigarettes to quit positively predicted Wave 2 abstinence.23 Different choices of outcome (30-day abstinence vs. smoking status), use of propensity score matching, and inclusion of adults over 64 might explain differences in findings. Our addition of Wave 3 suggests that any effectiveness of e-cigarettes for smoking cessation may be short-lived.
We found that light or intermittent smoking was positively associated with short- and longer-term cessation, consistent with previous research.40 In addition to smoking intensity, the most consistent finding across models was the predictive power of demographic and socioeconomic characteristics on cessation status. African American respondents were less likely to be successful, adjusting for nicotine dependence and cessation strategy. This finding is consistent with previous work that has found African American smokers to have similarly high quit intentions and quit attempts but less likelihood of success than their white counterparts.41 Income insecurity and lower education were also associated with less cessation success. The fact that race and socioeconomic status consistently predicted cessation success while the use of cessation aids did not, presents a significant challenge to health equity that needs to be addressed in cessation treatment.
Limitations
There are several limitations to this study. Due to data limitations, we could only investigate the most recent quit attempt, could not investigate patterns of quit attempts and strategies, and could not identify how smoking behavior changed immediately following a cessation attempt. We were not able to determine how nicotine replacement therapy, prescription drugs, and substituted products were used and whether unobserved patterns of use or e-cigarette device type can help explain our findings.42,43 Relatedly, the behavioral therapy measure includes many types of treatment (counseling, quit lines, web-based programs) and we are unable to determine the relative effectiveness of those programs in this study. Moreover, text-messaging smoking cessation programs, which have good evidence of efficacy44 and smoking apps, for which there is nascent and promising evidence45 were not explicitly mentioned in the assessment instrument. Finally, due to limited sample size, we were unable to differentiate between types of pharmacotherapy, although previous work has found that the effectiveness of pharmacotherapy varied across products.15,18,46 Small sample size yielded large CIs for estimates of behavioral support and age interaction terms; although the relative risk ratio is large, we cannot conclude there is a significant age interaction effect. Sample size limitations also required our e-cigarette substitution measure to include individuals who used e-cigarettes in combination with other tobacco products to try to quit.
Conclusion
This study evaluated predictors of cessation success for young adults using a large, nationally representative longitudinal dataset of tobacco use. We were particularly interested in whether young adult smokers, who have less short-term intention to quit, lower nicotine dependence, and more unassisted quit attempts compared to older adults,10 were more or less successful than older adults once they decided to make a quit attempt. We found that, although young adult and older adult smokers had different patterns of cessation strategy use, there were few differential effects of those strategies on cessation by age group, and none of the strategies examined were significantly associated with successful cessation for young adults at the population level. One key finding is that e-cigarettes were found to neither assist nor deter quitting among young adults, although they had temporary benefit for older adult regular and heavy daily smokers. More work is needed to identify effective interventions that help young adult smokers quit before they become lifelong users.
Supplementary Material
Acknowledgments
This work was conducted while SLW was a postdoctoral fellow at the University of California, San Francisco.
Funding
National Cancer Institute (T32CA113710-11), The California Tobacco-Related Disease Research Program (TRDRP 25FT-0009), The US National Institutes of Health and Food and Drug Administration (P50CA180890), Dorothy Rice Center for Health Economics.
Declaration of Interests
None declared.
References
- 1. Villanti AC, Niaura RS, Abrams DB, Mermelstein R. Preventing smoking progression in young adults: the concept of prevescalation. Prev Sci. 2019;20(3):377–384. doi:10.1007/s11121-018-0880-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ. 2004;328(7455):1519. doi:10.1136/bmj.38142.554479.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-Century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. [DOI] [PubMed] [Google Scholar]
- 4. Pirie K, Peto R, Reeves GK, Green J, Beral V; Million Women Study Collaborators The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. 2013;381(9861):133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Diemert LM, Bondy SJ, Brown KS, Manske S. Young adult smoking cessation: predictors of quit attempts and abstinence. Am J Public Health. 2013;103(3):449–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCarthy M, Siahpush M, Shaikh RA, Sikora Kessler A, Tibbits M. Social disparities in unaided quit attempts among daily current and former smokers: results from the 2010–2011 tobacco use supplement to the current population survey. Nicotine Tob Res. 2016;18(8):1705–1710. [DOI] [PubMed] [Google Scholar]
- 7. Solberg LI, Asche SE, Boyle R, McCarty MC, Thoele MJ. Smoking and cessation behaviors among young adults of various educational backgrounds. Am J Public Health. 2007;97(8):1421–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Curry SJ, Sporer AK, Pugach O, Campbell RT, Emery S. Use of tobacco cessation treatments among young adult smokers: 2005 National Health Interview Survey. Am J Public Health. 2007;97(8):1464–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hughes JR, Cohen B, Callas PW. Treatment seeking for smoking cessation among young adults. J Subst Abuse Treat. 2009;37(2):211–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Watkins SL, Thrul J, Max W, Ling P. Cold Turkey and Hot Vapes? A national study of young adult cigarette cessation strategies. Nicotine Tob Res. 2018;1–9. doi:10.1093/ntr/nty270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Suls JM, Luger TM, Curry SJ, Mermelstein RJ, Sporer AK, An LC. Efficacy of smoking-cessation interventions for young adults: a meta-analysis. Am J Prev Med. 2012;42(6):655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel Liaisons and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35(2):158–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview of reviews. 2013;( 5):CD009329. doi:10.1002/14651858.CD009329.pub2 [DOI] [PMC free article] [PubMed]
- 14. West R, Zhou X. Is nicotine replacement therapy for smoking cessation effective in the “real world”? Findings from a prospective multinational cohort study. Thorax. 2007;62(11):998–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kotz D, Brown J, West R. ‘Real-world’ effectiveness of smoking cessation treatments: a population study. Addiction. 2014;109(3):491–499. [DOI] [PubMed] [Google Scholar]
- 16. Pierce JP, Gilpin EA. Impact of over-the-counter sales on effectiveness of pharmaceutical aids for smoking cessation. JAMA. 2002;288(10):1260–1264. [DOI] [PubMed] [Google Scholar]
- 17. Heckman BW, Cummings KM, Kasza KA, et al. Effectiveness of switching smoking-cessation medications following relapse. Am J Prev Med. 2017;53(2):e63–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chaiton M, Diemert LM, Bondy SJ, et al. Real-world effectiveness of pharmaceutical smoking cessation aids: time-varying effects. Nicotine Tob Res. 2018;1–6. doi:10.1093/ntr/nty194 [DOI] [PubMed] [Google Scholar]
- 19. Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016;(9):CD010216. doi:10.1002/14651858.CD010216.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4(2):116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hajek P, Waller AP, Przulj D, et al. A randomized trial of E-cigarettes versus nicotine-replacement therapy. N Engl J Med. 2019;380(7):629–637. doi:10.1056/NEJMoa1808779 [DOI] [PubMed] [Google Scholar]
- 22. Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems. In: Stratton K, Kwan LY, Eaton DL, eds. Public Health Consequences of E-Cigarettes. Washington, DC: The National Academic Press; 2018. doi:10.17226/24952 [Google Scholar]
- 23. Benmarhnia T, Pierce JP, Leas E, et al. Can E-cigarettes and pharmaceutical aids increase smoking cessation and reduce cigarette consumption? Findings from a nationally representative cohort of American smokers. Am J Epidemiol. 2018;187(11):2397–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Berry KM, Reynolds LM, Collins JM, et al. E-cigarette initiation and associated changes in smoking cessation and reduction: the Population Assessment of Tobacco and Health Study, 2013–2015. Tob Control. 2018;28(1):42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vallone DM, Bennett M, Xiao H, Pitzer L, Hair EC. Prevalence and correlates of JUUL use among a national sample of youth and young adults. Tob Control. 2019;28(6):603–609. [DOI] [PubMed] [Google Scholar]
- 26. United States Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse, United States Department of Health and Human Services, Food and Drug Administration. Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]. 28 September 2018. doi:10.3886/ICPSR36498.v8 [Google Scholar]
- 27. Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017;26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control. 1997;6(suppl 2):S57–S62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. 2004;6(suppl 3):363–369. [DOI] [PubMed] [Google Scholar]
- 30. Sung H, Wang Y, Yao T, Lightwood J, Max W. Polytobacco use and nicotine dependence symptoms among US adults, 2012–2014. Nicotine Tob Res. 2018;20(1):88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Levy DE, Biener L, Rigotti NA. The natural history of light smokers: a population-based cohort study. Nicotine Tob Res. 2009;11(2):156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shiffman S, Kassel JD, Paty J, Gnys M, Zettler-Segal M. Smoking typology profiles of chippers and regular smokers. J Subst Abuse. 1994;6(1):21–35. [DOI] [PubMed] [Google Scholar]
- 33. Brauer LH, Hatsukami D, Hanson K, Shiffman S. Smoking topography in tobacco chippers and dependent smokers. Addict Behav. 1996;21(2):233–238. [DOI] [PubMed] [Google Scholar]
- 34. Trinidad DR, Pérez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine Tob Res. 2009;11(2):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jiang N, Gonzalez M, Ling PM, Glantz SA. Relationship of smokefree laws and alcohol use with light and intermittent smoking and quit attempts among US adults and alcohol users. PloS one 10(10):e0137023 2015;10(10):1–17. doi:10.1371/journal.pone.0137023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhou X, Nonnemaker J, Sherrill B, Gilsenan AW, Coste F, West R. Addictive behaviors attempts to quit smoking and relapse: factors associated with success or failure from the ATTEMPT cohort study. Addict Behav. 2009;34(4):365–373. [DOI] [PubMed] [Google Scholar]
- 37. Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ Open. 2016;6(6):e011045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schane RE, Prochaska JJ, Glantz SA. Counseling nondaily smokers about secondhand smoke as a cessation message: a pilot randomized trial. Nicotine Tob Res. 2013;15(2):334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults—United States, 2016. Morb Mortal Wkly Rep. 2018;67(2):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ussher M, Kakar G, Hajek P, West R. Dependence and motivation to stop smoking as predictors of success of a quit attempt among smokers seeking help to quit. Addict Behav. 2016;53:175–180. [DOI] [PubMed] [Google Scholar]
- 41. Kulak JA, Cornelius ME, Fong GT, Giovino GA. Differences in quit attempts and cigarette smoking abstinence between whites and African Americans in the United States: literature review and results from the international tobacco control US survey. Nicotine Tob Res. 2016;18(suppl 1):S79–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Zhang B, Cohen JE, Bondy SJ, Selby P. Duration of nicotine replacement therapy use and smoking cessation: a population-based longitudinal study. Am J Epidemiol. 2015;181(7):513–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Siahpush M, Shaikh RA, McCarthy M, Sikora Kessler A, Tibbits M, Singh GK. Association between duration of use of pharmacotherapy and smoking cessation: findings from a national survey. BMJ Open. 2015;5(1):e006229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Whittaker R, McRobbie H, Bullen C, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2016;4(4):CD006611. doi:10.1002/14651858.CD006611.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vilardaga R, Casellas-Pujol E, McClernon JF, Garrison KA. Mobile applications for the treatment of tobacco use and dependence. Curr Addict Rep. 2019;6(2):86–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kotz D, Brown J, West R. Prospective cohort study of the effectiveness of varenicline versus nicotine replacement therapy for smoking cessation in the “real world”. BMC Public Health. 2014;14:1163. doi:10.1186/1471-2458-14-1163 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.