The COVID-19 outbreak has caused a high mortality, with millions of people affected worldwide. COVID-19 infection has been reported to cause respiratory, enteric, hepatic, and neurological and neuropsychiatric complications with varied clinical severity.1 The prophylactic and treatment measures used for this disease varies by countries, and the World Health Organization (WHO) has also suggested other strategies to avoid the spread and management of COVID-19.2 The etiology of COVID-19 is still mostly unknown. Therefore, identifying the mechanisms that promote viral transmission and disease infection is critical in order to overcome this pandemic situation.3 Furthermoreuntil, Mnow there are no vaccines or therapeutic drugs available for COVID-19. Multiple drugs that may provide non-specific action, namely antiviral drugs (eg, remdesivir) and antimalarial drugs (eg, chloroquine and hydroxychloroquine), are being clinically screened for treatment of COVID-19 patients. Systemic complications related to COVID-19 infection are being treated with therapeutic drugs such as corticosteroid (dexamethasone) or biological agents (antibodies) against the cytokine storm (interleukins: IL-1 and IL-6, and TNF-α). Kinase inhibitors are also being tried.4 Until the development of vaccines and better therapeutics, there is an urgent need for strategies to control respiratory infection and to boost immune functions for patients suffering from COVID-19.5,6
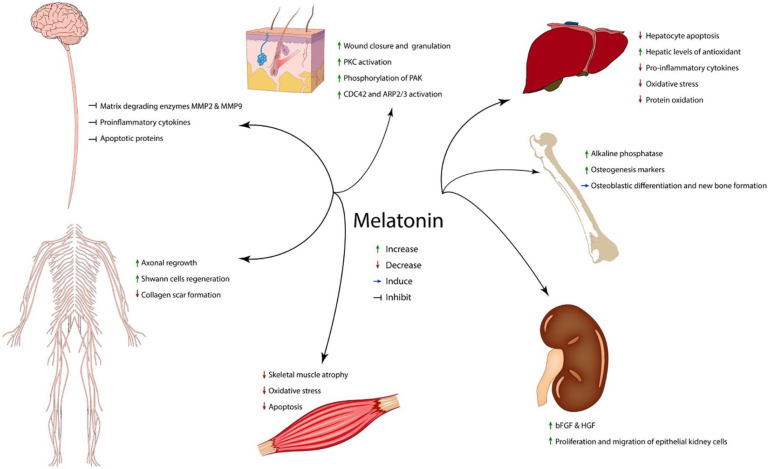
L-tryptophan (Trp), an essential amino acid, is the precursor of the neurotransmitter serotonin (5-hydroxytryptamine, 5-HT), which promotes a sense of well-being and “happiness”, and plays a role in preventing mood disorders. Dietary fatty acids affecting the pro-inflammatory cytokines have been suggested to affect the metabolic fate of Trp. Tryptophan and its metabolites including melatonin have the capacity to improve the immune system and reduce inflammation in various conditions.7-9 Here, we discuss the potential of using tryptophan and its metabolites including melatonin to boost the immune system in fighting COVID-19 infection (see Figure 1).
Figure 1.
Tryptophan and its possible actions.
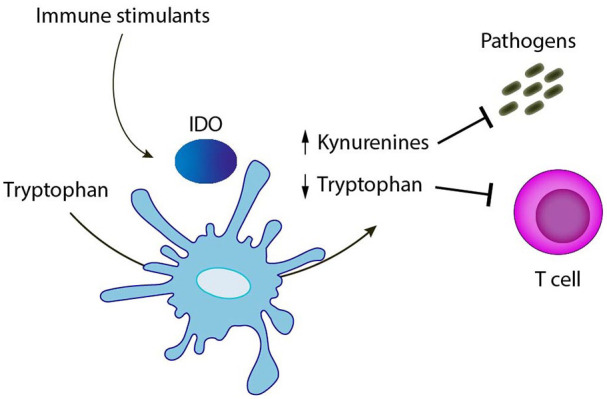
A recent study by Gardinassi et al,3 revealed a high involvement of inflammatory networks and increased expression of genes involved in tryptophan metabolism in COVID19 patients. There is a definite involvement of interleukin-6 (IL-6) in the immune response in COVID-1910 and IL-6 is thought to affect tryptophan catabolism in other pathophysiological conditions.11-13 Similarly, another study suggested a link between immunosuppressive therapy with tocilizumab and tryptophan metabolism in COVID-19 patients.14 This possibility indicates that tryptophan-rich sources could be beneficial for COVID-19 subjects.15 Despite enormous efforts to develop a COVID-19 vaccine, an effective and safe will, vaccine will likely not be available before 2021, which further demonstrates the need to develop quickly alternative solutions that are effective and known to be safe. Increasing evidence from several studies show that tryptophan and its metabolites including melatonin can reduce inflammatory reactions and enhance the immune system.7-9 There may also be a possibility that serotonin levels are altered in COVID-19 patients because of mental stress, which suggest a role for Trp in treatment. Trp is the precursor for melatonin (sleep hormone), which was reported to exert beneficial effects on the immune system through various physiological means16 (see Figure 2—adapted from Khan et al).17
Figure 2.
Melatonin and its possible actions (adopted from Khan et al(12)).17
In conclusion, even though Trp and its metabolites are known to be beneficial in improving the function of the immune system, the impact of Trp and its metabolites against severity of COVID-19 is still circumstantial and still needs to be demonstrated experimentally and clinically and to understand their role in personalized nutrition thus precision health to combat COVID-19.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Gilles J Guillemin  https://orcid.org/0000-0001-8105-4470
https://orcid.org/0000-0001-8105-4470
References
- 1. Hasöksüz M, Kiliç S, Saraç F. Coronaviruses and SARS-COV-2. Turk J Med Sci. 2020;50:549-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tobaiqy M, Qashqary M, Al-Dahery S, et al. Therapeutic management of COVID-19 patients: a systematic review. Infection Prevention in Practice. 2020;2(3):100061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gardinassi LG, Souza COS, Sales-Campos H, Fonseca SG. Immune and metabolic signatures of COVID-19 revealed by transcriptomics data reuse. Front Immunol. 2020;11:1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Iannaccone G, Scacciavillani R, Del Buono MG, et al. Weathering the cytokine storm in COVID-19: therapeutic implications. Cardiorenal Med. 2020. doi: 10.1159/000509483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dowd JB, Andriano L, Brazel DM, et al. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci USA. 2020;117(8):9696-9698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yao H, Lu X, Chen Q, et al. Patient-derived mutations impact pathogenicity of SARS-CoV-2. MedRxiv. 2020; 20060160. [Google Scholar]
- 7. Achtyes E, Keaton SA, Smart LA, et al. Inflammation and kynurenine pathway dysregulation in post-partum women with severe and suicidal depression. Brain Behav Immun. 2020;83:239-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dehhaghi M, Kazemi Shariat Panahi H, Guillemin GJ. Microorganisms, tryptophan metabolism, and kynurenine pathway: a complex interconnected loop influencing human health status. Int J Tryptophan Res. 2019;12:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garcez ML, Jacobs KR, Guillemin GJ. Microbiota alterations in Alzheimer’s disease: involvement of the kynurenine pathway and inflammation. Neurotox Res. 2019;36(2): 424-436. [DOI] [PubMed] [Google Scholar]
- 10. Thomas T, Stefanoni D, Reisz JA, et al. COVID-19 infection alters kynurenine and fatty acid metabolism, correlating with IL-6 levels and renal status. JCI Insight. 2020;19:140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mondanelli G, Albini E, Pallotta MT, et al. The proteasome inhibitor bortezomib controls indoleamine 2,3-dioxygenase 1 breakdown and restores immune regulation in autoimmune diabetes. Front Immunol. 2017;8:428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Orabona C, Mondanelli G, Pallotta MT, et al. Deficiency of immunoregulatory indoleamine 2,3-dioxygenase 1 in juvenile diabetes. JCI Insight. 2018;3(6):e96244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Orabona C, Pallotta MT, Volpi C, et al. SOCS3 drives proteasomal degradation of indoleamine 2,3-dioxygenase (IDO) and antagonizes IDO-dependent tolerogenesis. Proc Natl Acad Sci USA. 2008;105(52):20828-20833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Belladonna ML, Orabona C. Potential benefits of tryptophan metabolism to the efficacy of tocilizumab in COVID-19. Front Pharmacol. 2020:11:959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shader RI. COVID-19, interferons, and depression: a commentary. Psychiat Res. 2020;291:113198. [DOI] [PubMed] [Google Scholar]
- 16. Carrillo-Vico A, Lardone PJ, Alvarez-Sánchez N, Rodríguez-Rodríguez A, Guerrero JM. Melatonin: buffering the immune system. Int J Mol Sci. 2013;14(4):8638-8683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khan SU, Khan MU, Riaz H, et al. Effects of nutritional supplements and dietary interventions on cardiovascular outcomes: an umbrella review and evidence map. Ann Intern Med. 2019;171(3):190-198. [DOI] [PMC free article] [PubMed] [Google Scholar]