Abstract
Background:
To examine the association between childhood trauma and work functioning, and to elucidate to what extent this association can be accounted for by depression and/or anxiety.
Methods:
Data of 1,649 working participants were derived from the Netherlands Study of Depression and Anxiety (NESDA, n = 2,981). Childhood trauma (emotional neglect, psychological, physical, and sexual abuse before age 16) was assessed with a structured interview and work functioning, in terms of absenteeism and presenteeism, with the Health and Labor Questionnaire Short Form (SF-HLQ) and the World Health Organization Disability Assessment Schedule II (WHODAS-II), respectively. Depressive and/or anxiety disorders were assessed with the Composite Interview Diagnostic Instrument (CIDI). Mediation analyses were conducted.
Results:
At baseline, 44.8% reported to have experienced childhood trauma. Workers with the highest childhood trauma level showed significantly (p < 0.001) more absenteeism as well as more presenteeism. Mediation analyses revealed that indirect effects between the childhood trauma index and both work indices were significantly mediated by current depressive disorder (p = 0.023 and p < 0.001, respectively) and current comorbid depression-anxiety (p = 0.020 and p < 0.001, respectively), with the latter accounting for the largest effects (P M = 0.23 and P M = 0.29, respectively). No significant mediating role in this relationship was found for current anxiety disorder and remitted depressive and/or anxiety disorder.
Conclusions:
Persons with childhood trauma have significantly reduced work functioning in terms of absenteeism and presenteeism. This seems to be largely accounted for by current depressive disorders and current comorbid depression-anxiety.
Keywords: Absenteeism, anxiety, childhood trauma, depression, presenteeism
Introduction
Attendance and performance at work are not only dependent on competence and knowledge; but a multitude of health-related, personal, and work-related factors also play an important role. Work loss and suboptimal work performance are not only a burden for the individuals themselves, but also for their colleagues and employers, their families and wider environment, and for society in general since both increase employer and healthcare costs [1,2]. Some well-known examples of sick-leave predictors are psychosomatic complaints, being unmarried, and low job control [3,4]. Another important factor that may influence absenteeism and presenteeism (i.e., missing work due to illness and going to work despite illness, respectively) is experiences with childhood trauma, but systematic studies on this topic are scarce. Possible, because the interval between cause and effect may be (very) long, this contributing factor may easily be overlooked. On top of that, the traumatic childhood events that eventually led to work impairment are usually not shared, out of shame, secrecy, and social taboo. Using data from the adverse childhood experiences study, Anda et al. [5] reported that individuals with a (self-reported) history of childhood emotional, physical, and/or sexual abuse were more likely to report problems with work absenteeism in adulthood. A more recent study also found evidence of an increased risk of permanent work disability at 55 years in persons with childhood adversity [6]. It has been reported on more often that in persons with adverse childhood experiences more school absenteeism or overall poorer school performance was observed [7,8]. To the best of our knowledge, however, the association between childhood trauma and presenteeism has as yet not been investigated.
How childhood trauma exactly results in absenteeism and presenteeism many years later has not been examined. However, it seems logical to assume that this can partly be accounted for by the large impact such early adverse events have on a person’s (developing) mental health. The WHO World Mental Health Surveys found strong associations between childhood adversities and overall adult psychopathology [9]. Individuals reporting childhood trauma are about twice more likely to develop a depression and/or an anxiety disorder later in life [10]. Literature reviews and meta-analyses have demonstrated that childhood trauma is associated with a range of psychological problems and psychiatric disorders, among which are depressive and anxiety disorders. Chen et al. [11] came to the conclusion that a history of sexual abuse correlates with an increased risk of a lifetime diagnosis of (one of) these disorders, which conclusion was confirmed in a recent umbrella review by Hailes et al. [12]. Furthermore, there is evidence of a relationship between nonsexual child maltreatment (i.e., physical abuse, emotional abuse, and/or neglect) and depressive and anxiety disorders [13]. The effects of childhood trauma are not just limited to an increased initial vulnerability, but can also have a major impact on the clinical course of the two disorders, which notably is more serious, often chronic, and prognostically unfavorable course of the disease [14–16].
Mental-health problems, especially anxiety and/or depressive episodes, have consistently been linked to worse short- and long-term absenteeism and presenteeism outcomes among working people [1,2,17–22]. The large-scale Netherlands Study of Depression and Anxiety (NESDA) discerned that current depressive disorders were associated with a sevenfold higher risk of long-term work absence and a fivefold higher risk of impaired work performance, whereas current anxiety disorders increased these odds with around a factor two [23], which numbers were later confirmed by Hendriks et al. [24] in their longitudinal study.
The purpose of the present study is to gain more insight into the association between childhood trauma and work functioning in terms of absenteeism as well as presenteeism, and to elucidate to what extent any associations can be accounted for by a depression and/or anxiety disorder. The results were obtained in an extensive sample of the Dutch working population participating in the NESDA study [25].
Methods
Participants
We extracted our baseline data from NESDA, an ongoing Dutch longitudinal multisite cohort study for which 2,981 adults (aged 18–65 years) were recruited between 2004 and 2007. NESDA recruited from three different settings: the general population, primary care, and specialized mental healthcare and is designed to have a control group without a depressive or anxiety disorder. Participants with depressive and anxiety disorders were recruited in all three of these settings and thereby cover the entire range of mood psychopathology including both persons with and without treatment needs and experiences, whereas healthy individuals were only recruited in the general population and the general practices. The baseline assessments included a structured diagnostic psychiatric interview, after which all participants were monitored to investigate the course and consequences of depressive and anxiety disorders. Candidates not fluent in Dutch and those with a primary clinical diagnosis of psychotic, obsessive–compulsive, bipolar, post-traumatic stress or severe substance use disorder were excluded. The research protocol was approved by the ethics committees of the participating universities and written informed consent was obtained from all participants. For further details on NESDA, see Penninx et al. [25].
In the present study, we describe and analyze the data of the 1,873 participants that had a paid job and worked at least 8 h a week at baseline, thereby excluding the 1,108 participants who were not employed or employed for less than 8 h a week.
Measurements
Work functioning
Work functioning was conceptualized as absenteeism and presenteeism, with absenteeism being assessed with the validated Health and Labor Questionnaire Short Form (SF-HLQ) [26,27]. Consistent with Plaisier et al. [23], absenteeism was computed by dividing the number of absent days from work during the past 6 months because of health problems by the number of actual work days per week. This variable did not meet normality assumptions and was therefore categorized into three categories: no absenteeism, short-term absenteeism (≤2 weeks), and long-term absenteeism (>2 weeks). This classification also enabled us to make a distinction between absence from work most probably due to self-limiting conditions such as common colds, and work absenteeism, where more chronic conditions were likely to be involved.
Presenteeism was assessed with the validated World Health Organization Disability Assessment Schedule II (WHODAS-II) [28,29]. This 36-item instrument gauges health and disability and provides a work-functioning profile across six activity domains. For our study, we restricted ourselves to the four items of the work-activities domain: Difficulties in (a) day-to-day work, (b) doing most important work tasks well, (c) getting all work done, and (d) getting work done as quickly as needed. The respondents rated the items on a 5-point scale, ranging from 1 (None) to 5 (Extreme/Cannot do). The summated work domain scale has a range from 4 to 20, with higher scores reflecting a higher level of disability.
Childhood trauma
Childhood trauma was assessed retrospectively using the Childhood Trauma Interview (CTI), a structured interview for adults in the age range of 18–64 years first described in the Netherlands Mental Health Survey and Incidence Study (NEMESIS).
During their baseline assessment, all participants were asked whether they had experienced any kind of emotional neglect and/or psychological, physical, or sexual abuse before the age of 16. The definition of emotional neglect was lack of parental attention or support and ignorance of the participant’s problems and experiences as a child. Psychological abuse was defined as verbal abuse, undeserved punishment, subordination to siblings, and being emotionally blackmailed. Physical abuse was specified as being kicked or hit with hands or an object, being beaten up, or being physically abused in any other way, while sexual abuse was delineated as being sexually approached against one’s will in terms of being touched or made to touch someone in a sexual way. Participants answered “Yes” or “No” to each of the four forms of childhood trauma and were asked to give an indication of the frequency of the incidents on a 5-point scale (Once, Sometimes, Regularly, Often, and Very often). As was done in earlier studies [30,31], a cumulative childhood trauma index with sum scores from 0 to 8 was composed, where higher scores were indicative of more types and more incidents of adverse childhood trauma. The interrater reliability of the CTI is 0.73 to 1.0 [32] and according to Spinhoven et al. [33] there is a convergent correlation with the Childhood Trauma Questionnaire (CTQ) for trauma severity (r = 0.57–0.61). Data from the CTI was collected at wave 1 (baseline) and from the CTQ at wave 4 of the NESDA study (4 years after baseline).
Depressive and/or anxiety disorder
Our participants were screened for depressive and/or anxiety disorders at baseline by trained clinical staff using the validated Composite Interview Diagnostic Instrument (CIDI version 2.1) [34] that assesses the presence of major depressive disorder, dysthymic disorder, generalized anxiety disorder, panic disorder, agoraphobia, and/or social phobia. We took into account current (6-month recency) depressive, anxiety, and comorbid depressive-anxiety disorder, and remitted depressive and/or anxiety disorder (lifetime but not 6-month recency). The widely used CIDI classifies diagnoses according to DSM-IV criteria and has good overall reliability and validity [35].
Covariates
Because we specifically sought to describe the association between childhood trauma and work functioning, and the role of depressive and/or anxiety disorders in this relationship, we limited the number of potentially confounding covariates to sex, age, education (in years attained), the number of working hours per week, and the number of somatic conditions. The latter conditions were assessed with the chronic diseases interview, a 21-item face-to-face interview instrument that was designed for NESDA and provides a sum of self-reported heart disease, diabetes, stroke, cancer, high blood pressure, allergies, intestinal disorders, liver disease, epilepsy, chronic lung problems, injuries, and arthritis. In addition, participants could mention up to five chronic diseases that were not (yet) included in the list [25]. Given the skewed distribution of this variable, it was dichotomized into (0) No somatic condition and (1) At least one somatic condition.
Statistical analyses
Sample characteristics are presented as means with standard deviations or numbers with percentages. Baseline characteristics were compared across the childhood trauma indices using analyses of variance for continuous variables and Pearson’s chi-squared tests for categorical variables.
We subsequently tested depressive and anxiety disorder more specifically as potential contributors to the childhood-trauma and work-functioning associations to see whether they would at least partially explain why adverse early-life events lead to work impairment later in life. To do so, we applied a single model to each outcome measure with four mediators (current depressive disorder, current anxiety disorder, current comorbid depression-anxiety, and remitted depressive and/or anxiety disorder). Because of the dichotomous nature of the mediators, we used probit regression for the mediating models. In the outcome model we applied ordinal probit regression for absenteeism (three categories) and linear regression for presenteeism. Mediation was investigated by directly testing the significance of the indirect effect of the independent variable (IV) on the dependent variable (DV) through the mediator (M), quantified as the product of the effects of the IV on M (a) and the effect of M on DV (b), partialling out the effects of the IV. The 95% percentile-based confidence intervals (CIs) were computed using bootstrap with 1,000 samples. As unstandardized coefficients in probit and linear models are on different scales, all effects were expressed as standardized effects [36]. All models were adjusted for sex, age, education, number of working hours, and the presence of somatic conditions.
Descriptive analyses were conducted in SPPS version 26.0 (SPSS Inc, Chicago, IL) and mediation analyses using R. Statistical significance was set at p < .05.
Results
Baseline sample and outcome characteristics
Of the 1,873 working participants, 223 individuals (11.9%) were excluded due to missing data on work functioning and one additional person due to incompletion of the childhood trauma questionnaire, leaving 1,649 subjects (n = 584 male and n = 1,065 female) for analysis.
Table 1 shows the baseline demographic and clinical characteristics of the study sample according to childhood trauma level. The mean age of the participants was 40.7 years, 64.6% were women, and the mean years of attained education was 13 years. Childhood trauma was reported by 44.8 and 22.4% reported a remitted depressive and/or anxiety disorder, 13.6% a current depressive disorder, 19.0% a current anxiety disorder, 20.5% a current comorbid depressive-anxiety disorder, and 24.4% neither a current nor a remitted depressive or anxiety disorder. Of the study population, 47.4% had not been absent from work in the last 6 months, while 31.0% reported 0–2 weeks, and 21.6% more than 2 weeks of absenteeism. Significant differences were found between workers without childhood trauma, those with a childhood trauma index between 1 and 4 (mild), and those with scores between 5 and 8 (serious) regarding sex (p < 0.001), age (p = 0.002), educational level (p < 0.001), somatic health (p = 0.004), number of working hours (p = 0.023), and psychiatric status (p < 0.001). As for absenteeism (p < 0.001) and presenteeism (p < 0.001), those workers reporting the highest childhood trauma scored higher on these outcome measures. Of the workers who had not experienced any childhood trauma, 55% reported no absenteeism, which was 39.8% for those having experienced mild childhood trauma scores and 32.3% for those with high childhood trauma scores. Within the nontrauma group, short-term absenteeism was reported by 27.7%, within the mild trauma group 36.1%, and within the severe trauma group 31.7%. When looking at the long-term absenteeism reports, we noted even more pronounced increases: 17.3, 24.2, and 35.9%, respectively. Mean disability scores went from 7.64 in workers without childhood trauma, to 9.45 and 9.98 in workers with mild and higher childhood trauma scores, respectively.
Table 1.
Baseline demographic and clinical characteristics according to childhood trauma scores at baseline (n = 1,649).
| Childhood trauma score | Total | ||||
|---|---|---|---|---|---|
| 0 | 1–4 | 5–8 | p value* | ||
| Socio-demographics | |||||
| Gender (N, % female) | 543 (59.6) | 401 (70.2) | 121 (72.5) | <.001 | 1065 (64.6) |
| Age in years (mean, SD) | 39.93 (12.2) | 41.38 (11.1) | 42.95 (10.9) | .002 | 40.74 (11.7) |
| Education in years (mean, SD) | 12.77 (3.2) | 12.85 (3.3) | 11.76 (3.2) | <.001 | 12.70 (3.2) |
| Number of working hours (mean, SD) | 31.64 (10.8) | 30.36 (10.3) | 29.78 (10.6) | .023 | 31.01 (10.6) |
| Somatic health | |||||
| % with at least one chronic condition | 422 (46.3) | 295 (51.7) | 99 (59.3) | .004 | 816 (49.5) |
| Work functioning | |||||
| Absenteeism (N, %) | <.001 | ||||
| No absenteeism | 501 (55.0) | 227 (39.8) | 54 (32.3) | 782 (47.4%) | |
| Short-term absenteeism (≤ 2 weeks) | 252 (27.7) | 206 (36.1) | 53 (31.7) | 511 (31.0) | |
| Long-term absenteeism (> 2 weeks) | 158 (17.3) | 138 (24.2) | 60 (35.9) | 356 (21.6) | |
| Disability (4–20), mean (SD) | 7.64 (4.2) | 9.45 (4.5) | 9.98 (4.6) | <.001 | 8.50 (4.4) |
| Psychiatric status (N, %) | <.001 | ||||
| No depressive or anxiety disorder | 311 (34.1) | 78 (13.7) | 14 (8.4) | 403 (24.4) | |
| Remitted depressive and/or anxiety disorder | 202 (22.2) | 136 (23.8) | 32 (19.2) | 370 (22.4) | |
| Current depressive disorder | 105 (11.5) | 92 (16.1) | 27 (16.2) | 224 (13.6) | |
| Current anxiety disorder | 168 (18.4) | 108 (18.9) | 38 (22.8) | 314 (19.0) | |
| Current comorbid depressive-anxiety disorder | 125 (13.7) | 157 (27.5) | 56 (33.5) | 338 (20.5) | |
Abbreviations: CTI, Childhood Trauma Index; SD, standard deviation; %, within CTI score.
p value based on chi-square statistics for categorical variables and analyses of variances for continuous variables (one-way ANOVA).
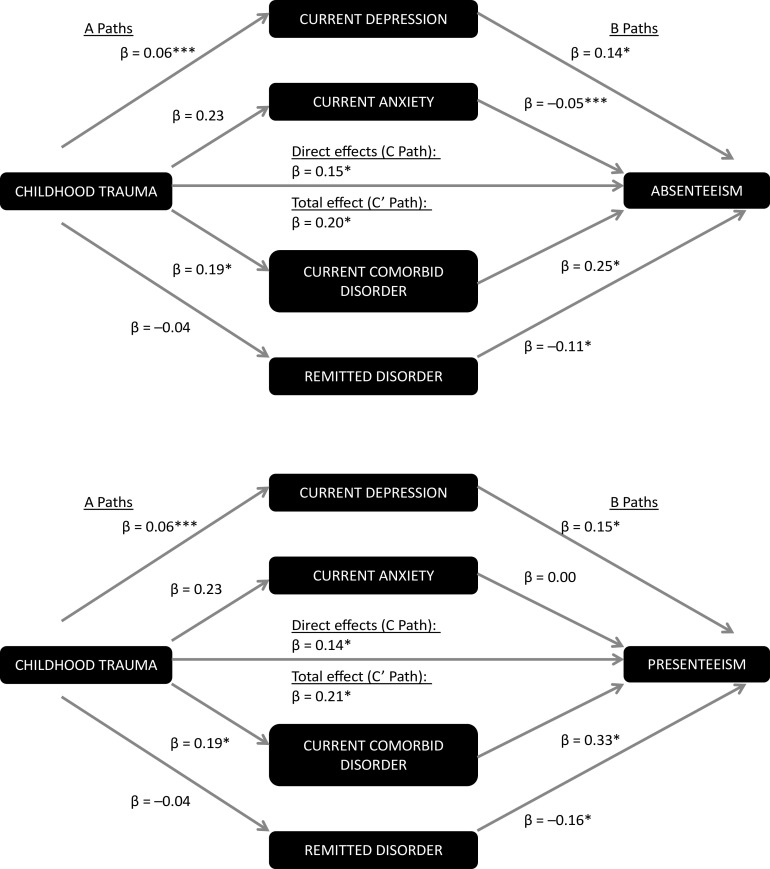
Mediation by psychopathology
Table 2 and Figure 1 display the main results of the mediation analyses in which childhood trauma and current and remitted depressive and/or anxiety disorders were entered with absenteeism and presenteeism as the dependent variables. After correction for age, gender, education, number of working hours, and somatic conditions, there is an overall significant, direct effect of the childhood trauma index on both work-functioning indices (p < 0.001). The significant indirect effects of current depression and current comorbid depression-anxiety indicate that these factors partially explain the association between the childhood trauma index and both absenteeism (p = 0.023 and p < 0.001, respectively) and presenteeism (p = 0.020 and p < 0.001, respectively). Current depressive disorder accounted for only a small fraction of the total effect on absenteeism (P M = 0.04 [indirect effect/total effect]), while the role of current comorbid depression-anxiety was larger (P M = 0.23). We found similar results for presenteeism: current depressive disorder: P M = 0.05; current comorbid depression-anxiety: P M = 0.29. Apparently, current anxiety disorder and remitted anxiety and/or depression play no significant mediating role in the childhood-trauma/work-functioning association.
Table 2.
Explained variance of depression and anxiety in the relationship between childhood trauma index (IV) and work functioning (DV) in the working population (N = 1,649).
| Dependent variable (DV) | Independent variable (IV) | Mediating variable (M) | Effect of IV on M (a) | Effect of M on DV (b) | Direct effect of IV on DV (c) | Indirect effect (or mediation) = a × b | Total effect = indirect + direct effect | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| a (95% CI) | p value | b (95% CI) | p value | c (95% CI) | p value | a × b | p value | c′ = Σa × b + c (95% CI) | p value | |||
| Absenteeism | Childhood Trauma index (CTI 0–8) | Current anxiety only (0/1) | 0.225 (−0.027 to 0.078) | 0.340 | −0.054 (−0.106 to −0.001) | 0.045 | 0.146 (0.092–0.200) | <0.001 | −0.001 (−0.004 to 0.002) | 0.389 | 0.204 (0.151–0.257) | <0.001 |
| Current Depression only (0/1) | 0.064 (0.012–0.116) | 0.016 | 0.139 (0.087–0.190) | <0.001 | 0.009 (0.001–0.017) | 0.023 | ||||||
| Current comorbid depression-anxiety (0/1) | 0.190 (0.139–0.241) | <0.001 | 0.245 (0.192–0.298) | <0.001 | 0.046 (0.031–0.062) | <0.001 | ||||||
| Remitted anxiety and/or depression (0/1) | −0.035 (−0.083to 0.013) | 0.154 | −0.107 (−0.160 to 0.054) | <0.001 | 0.004 (−0.002 to 0.009) | 0.182 | ||||||
| Presenteeism | Childhood Trauma index (CTI 0–8) | Current anxiety only (0/1) | 0.225 (−0.027to 0.078) | 0.340 | 0.002 (−0.043to 0.047) | 0.939 | 0.137 (0.089–0.185) | <0.001 | 0.000 (−0.001 to 0.001) | 0.939 | 0.214 (0.164–0.264) | <0.001 |
| Current depression only (0/1) | 0.064 (0.012–0.116) | 0.016 | 0.153 (0.101–0.204) | <0.001 | 0.010 (0.002–0.018) | 0.020 | ||||||
| Current comorbid depression-anxiety (0/1) | 0.190 (0.139–0.241) | <0.001 | 0.326 (0.278–0.373) | <0.001 | 0.062 (0.043–0.081) | <0.001 | ||||||
| Remitted anxiety and/or depression (0/1) | −0.035 (−0.083 to 0.013) | 0.154 | −0.159 (−0.201 to 0.117) | <0.001 | 0.006 (−0.002 to 0.013) | 0.155 | ||||||
The childhood trauma score was considered a continuous variable. Models corrected for age, gender, education, number of working hours, and somatic conditions.
Abbreviations: CI, confidence interval.
Figure 1.
Mediation model for childhood trauma on absenteeism and presenteeism through depressive and anxiety disorder. Note: β = standardized effects; *p < 0.001, **p < 0.01, ***p < 0.05; all models corrected for age, gender, education, somatic conditions, and number of working hours.
Discussion
This study expands upon prior literature, examining the relationship between childhood trauma and work absenteeism and presenteeism, and investigating contributing factors in a large cohort (NESDA) of the Dutch working population. Almost half (44.7%) of our participants reported having experienced some form of childhood trauma and we found a strong, significant relationship between exposure to early-life adversity and reduced work functioning, both in terms of absenteeism and presenteeism. Associations were most pronounced for long-term absenteeism, where we observed a marked increase proportional to childhood trauma level. We are the first to show that persons with childhood trauma have more presenteeism at the workplace and that the associations between childhood trauma and absenteeism and presenteeism were slightly but significantly accounted for by a current depressive disorder, while the role of current comorbid depression-anxiety in this relationship was more pronounced, explaining one quarter of the total effect in absenteeism as well as in presenteeism. A large part of the total effect remains unexplained, which means that the relationship between childhood trauma and reduced work functioning in adulthood goes beyond psychopathology. We, for instance, found no significant mediating role of current anxiety disorder and remitted depressive and/or anxiety disorder. The differences in the roles of current anxiety, depressive disorder, and comorbid disorder in this relationship are perhaps explained by differences in their course. Hovens et al. [15] showed that childhood trauma was associated with an elevated risk of the persistence of depression or a comorbid disorder, while this was not the case for the 2-year course of anxiety disorders. In our previous study [37] we found that childhood trauma was associated with chronicity of anxiety symptoms and occurrence of social phobia, but not with the persistence of panic disorder at 2-year follow-up. Moreover, depressive disorders usually have a more continuous and more persistent nature, with a higher risk of (long-term) work disability, whereas anxiety disorders tend to be more episodic. In addition, when people experience anxiety, they may still (prefer to) go to work because the workplace and work activities might distract them from their avoidance behaviors.
As to the methodological strengths of our study, we can point to the large representative cohort of working adults we were able to investigate. We, moreover, used validated, structured diagnostic interviews and well-defined clinical outcome measures (standardized self-report questionnaires), as well as a known mediation model to determine the role of depression and/or anxiety on work absenteeism and presenteeism.
When interpreting the results of our study, some caution is warranted. Importantly, we exclusively relied on retrospective self-reports of childhood trauma, which may give rise to memory bias. However, several studies concluded that this bias was too small to challenge the findings [38–40]. The CTI assessed type and frequency of the trauma and not duration and severity of the abuse. These latter objective characteristics are important predictors of psychopathology, as were more subjective characteristics (e.g., negative reactions to disclosure and feelings of guilt) [41]. We have to bear in mind that retrospective reports of childhood trauma identify other groups of individuals than prospective reports. We used an interview, and not a questionnaire, to assess a broad childhood trauma index, and not subtypes, which strengthens the concordance between retrospective and prospective measures [42]. However, we have to take into account that not including subtypes of childhood trauma can also limit the results, since the test–retest reliability and agreement of retrospective self-reports on childhood abuse seems to be partly dependent on the type of childhood abuse. Wielaard et al. [43] found that the answer consistency on emotional neglect is significantly influenced by depression diagnosis and depression severity at baseline, but not the other types of childhood abuse. Moreover, patients with potential mental disorders more frequently reported severe and very severe childhood adversities than patients without a probable mental disorder [44]. Also, given the long-time lapse between the adverse childhood events and our assessment of work functioning, we were not able to consider other potentially contributing factors in the period prior to the NESDA baseline wave, such as social and (work-related) environmental factors, or past and/or current medical/psychological treatments. We also should be very cautious with the concepts of mediation and mediators since we cannot assume a causal relationship between childhood trauma and the dependent variables we investigated on account of the cross-sectional nature of our approach. As a final remark we need to mention the exclusion of 223 individuals (11.9%) due to missing data on the independent or dependent variables.
Our findings have important clinical implications because they shed new light on the pathway from childhood trauma to adult work functioning. With many spending half of their waking hours at the workplace, employees ought to be supported by a proactive and effective management and offered preventive interventions, including the early recognition of reduced work quality, early support, and easily accessible and affordable treatment for any psychiatric disorder. Moreover, mental ill health is underreported in the sick-leave records because it often remains undetected or is dominated by or hidden behind somatic symptoms. Occupational coaches and medical staff need to take into account this potential vulnerability and the psychological origins of current symptoms and act accordingly when estimating the disability duration, potential replacement income and referral policy. Arguably these professionals are often not aware of the trauma the worker has experienced growing up because they do not have access to such sensitive information, but they could play a major role in the detection and recovery process by offering timely screening for psychopathology (e.g., depression and comorbidity) using widely-used and validated screening instruments. Ultimately, as a society, we have an important mission: to break the taboo around childhood maltreatment and mental-health problems and make help more accessible and readily available at as early a stage as possible.
Conclusion
We have shown that childhood trauma is directly associated with reduced work functioning in adult life, both in terms of absenteeism and presenteeism. The relationship is partly mediated by a current depressive and/or comorbid depressive-anxiety disorder. Apart from these psychopathology-related factors, there are indubitably other mechanisms that warrant attention since they may also play a part in the observed association. Childhood trauma is common and can have (delayed and prolonged) disruptive effects on workers’ physical and mental health and well-being. Adverse early-life experiences then merit serious attention from the business community and labor leaders, but far preferably, at an earlier stage from General Practitioners, mental-health services, and policy-makers at the government level.
Acknowledgments and Financial Support
The infrastructure for the NESDA study (www.nesda.nl) has been funded through the Geestkracht programme of the Netherlands Organization for Health Research and Development (Zon-Mw, grant number 10-000-1002) and by participating universities and mental health care organizations (Amsterdam University Medical Centers (location VUmc), GGZ in Geest, Leiden University Medical Center, University Medical Center Groningen, University of Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Rob Giel Onderzoekscentrum). This project was partly funded by project number 5739 (bequest Cassiers) of the University of Antwerp.
Conflicts of Interest
Prof. Dr. Penninx has received—nonrelated—research funding from Jansen Research and Boehringer Ingelheim. Maud De Venter reports personal fees from Bequest Cassiers, during the conduct of the study. The authors Bernet Elzinga, Filip Van Den Eede, Kristien Wouters, Guido Van Hal, Dick Veltman, and Bernard Sabbe declare none.
Data Availability Statement
The data that support the findings of this study are property of the NESDA consortium, represented by the NESDA principal investigator (PI) prof. Dr. B. W. J. H. Penninx. The total NESDA dataset is available on the internal NESDA website. Restrictions apply to the availability of these data, which were used under license for this study (collaboration agreement between the University of Antwerp and the NESDA consortium).
References
- [1].Buist-Bouwman MA, De Graaf R, Vollebergh WAM, Ormel J. Comorbidity of physical and mental disorders and the effect on work-loss days. Acta Psychiatr Scand. 2005;111:436–443.doi: 10.1111/j.1600-0447.2005.00513.x. [DOI] [PubMed] [Google Scholar]
- [2].De Graaf R, Tuithof M, Van Dorsselaer S, Ten Have M. Comparing the effects on work performance of mental and physical disorders. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1873–1883.doi: 10.1007/s00127-012-0496-7. [DOI] [PubMed] [Google Scholar]
- [3].Duijts SFA, Kant IJ, Landeweerd JA, Swaen GMH. Prediction of sickness absence: development of a screening instrument. Occup Environ Med. 2006;63:564–569.doi: 10.1136/oem.2005.024521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Duijts SFA, Kant IJ, Swaen GMH, van den Brandt PA, Zeegers MPA. A meta-analysis of observational studies identifies predictors of sickness absence. J Clin Epidemiol. 2007;60:1105–1115.doi: 10.1016/j.jclinepi.2007.04.008. [DOI] [PubMed] [Google Scholar]
- [5].Anda RF, Fleisher VI, Felitti VJ, Edwards VJ, Whitfield CL, Dube SR, et al. Childhood abuse, household dysfunction, and indicators of impaired adult worker performance. Perm J. 2004;8:30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Fahy AE, Stansfeld SA, Smuk M, Lain D, Horst M, Vickerstaff S, et al. Longitudinal associations of experiences of adversity and socioeconomic disadvantage during childhood with labour force participation and exit in later adulthood. Soc Sci Med. 2017;183:80–7. doi: 10.1016/j.socscimed.2017.04.023. [DOI] [PubMed] [Google Scholar]
- [7].Stempel H, Cox-Martin M, Bronsert M, Dickinson LM, Allison MA. Chronic school absenteeism and the role of adverse childhood experiences. Acad Pediatr. 2017;17:837–843.doi: 10.1016/j.acap.2017.09.013. [DOI] [PubMed] [Google Scholar]
- [8].Crouch E, Radcliff E, Hung P, Bennett K. Challenges to school success and the role of adverse childhood experiences. Acad Pediatr. 2019;19:899–907.doi: 10.1016/j.acap.2019.08.006. [DOI] [PubMed] [Google Scholar]
- [9].Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br J Psychiatry. 2010;197:378–385.doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].De Venter M, Demyttenaere K, Bruffaerts R. The relationship between adverse childhood experiences and mental health in adulthood. A systematic literature review. Tijdschr Psychiatr. 2013;55:259–268. [PubMed] [Google Scholar]
- [11].Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, et al. Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clin Proc. 2010;85:618–629.doi: 10.4065/mcp.2009.0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hailes HP, Yu R, Danese A, Fazel S. Long-term outcomes of childhood sexual abuse: an umbrella review. Lancet Psychiatry. 2019;6:830–839.doi: 10.1016/S2215-0366(19)30286-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9:e1001349doi: 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hovens JGFM, Giltay EJ, Wiersma JE, Spinhoven P, Penninx BWJH, Zitman FG. Impact of childhood life events and trauma on the course of depressive and anxiety disorders. Acta Psychiatr Scand. 2012;126:198–207.doi: 10.1111/j.1600-0447.2011.01828.x. [DOI] [PubMed] [Google Scholar]
- [15].Hovens JGFM, Giltay EJ, Van Hemert AM, Penninx BWJH. Emotional scars: impact of childhood trauma on the development of depressive and anxiety disorders later in life. Tijdschr Psychiatr. 2017;59:286–296. [PubMed] [Google Scholar]
- [16].Hendriks SM, Spijker J, Licht CMM, Beekman ATF, Penninx BWJH. Two-year course of anxiety disorders: different across disorders or dimensions? Acta Psychiatr Scand. 2013;128:212–221.doi: 10.1111/acps.12024. [DOI] [PubMed] [Google Scholar]
- [17].Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;109:38–46.doi: 10.1111/j.1600-0047.2004.00329.x. [DOI] [PubMed] [Google Scholar]
- [18].Alonso J, Petukhova M, Vilagut G, Chatterji S, Heeringa S, Üstün TB, et al. Days out of role due to common physical and mental conditions: results from the WHO World Mental Health surveys. Mol Psychiatry. 2011;16:1234–1246.doi: 10.1038/mp.2010.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Bokma WA, Batelaan NM, Balkom AJLM, Penninx BWJH. Impact of anxiety and/or depressive disorders and chronic somatic diseases on disability and work impairment. J Psychosom Res. 2017;94:10–6. doi: 10.1016/j.jpsychores.2017.01.004. [DOI] [PubMed] [Google Scholar]
- [20].Dewa CS, Lin E. Chronic physical illness, psychiatric disorder and disability in the workplace. Soc Sci Med. 2000;51:41–50.doi: 10.1016/S0277-9536(99)00431-1. [DOI] [PubMed] [Google Scholar]
- [21].Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychol Med. 1997;27:861–873.doi: 10.1201/b15265. [DOI] [PubMed] [Google Scholar]
- [22].Laitinen-Krispijn S, Bijl RV. Mental disorders and employee sickness absence: the NEMESIS study. Soc Psychiatry Psychiatr Epidemiol. 2000;35:71–77. [DOI] [PubMed] [Google Scholar]
- [23].Plaisier I, Beekman ATF, Graaf R, Smit JH, Dyck R, Penninx BWJH. Work functioning in persons with depressive and anxiety disorders: the role of specific psychopathological characteristics. J Affect Disord. 2010;125:198–206. doi: 10.1016/j.jad.2010.01.072. [DOI] [PubMed] [Google Scholar]
- [24].Hendriks SM, Spijker J, Licht CMM, Hardeveld F, Graaf R, Batelaan NM, et al. Long-term work disability and absenteeism in anxiety and depressive disorders. J Affect Disord. 2015;178:121–30. doi: 10.1016/j.jad.2015.03.004. [DOI] [PubMed] [Google Scholar]
- [25].Penninx BWJH, Beekman ATF, Smit JH, Zitman FG, Nolen WA, Spinhoven P, et al. The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int J Methods Psychiatr Res. 2008;17:121–140.doi: 10.1002/mpr.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hakkaart-Van Roijen L. Manual Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiC-P). Rotterdam, The Netherlands: Institute for Medical Technology Assessment Erasmus University Rotterdam, 2007. [Google Scholar]
- [27].Bouwmans C, Jong KD, Timman R, Zijlstra-Vlasveld M, Feltz-Cornelis C, Tan SS, et al. Feasibility, reliability and validity of a questionnaire on healthcare consumption and productivity loss in patients with a psychiatric disorder (TiC-P). BMC Health Serv Res. 2013;13:217. doi: 10.1186/1472-6963-13-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].World Health Organization. Disability Assessment Schedule II. Geneva, Switzerland: WHO, 2000. [Google Scholar]
- [29].Chwastiak LA, Von Korff M. Disability in depression and back pain: evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003;56:507–514. [DOI] [PubMed] [Google Scholar]
- [30].Hovens JGFM, Wiersma JE, Giltay EJ, Oppen P, Spinhoven P, Penninx BWJH, et al. Childhood life events and childhood trauma in adult patients with depressive, anxiety and comorbid disorders vs. controls. Acta Psychiatr Scand. 2010;122:66–74. doi: 10.1111/j.1600-0447.2009.01491.x. [DOI] [PubMed] [Google Scholar]
- [31].Wiersma JE, Hovens JGFM, Van Oppen P, Giltay EJ, Van Schaik DJF, Beekman ATF, et al. The importance of childhood trauma and childhood life events for chronicity of depression in adults. J Clin Psychiatry. 2009;70:983–989.doi: 10.4088/JCP.08m04521. [DOI] [PubMed] [Google Scholar]
- [32].Fink LA, Bernstein D, Handelsman L, Foote J, Lovejoy M. Initial reliability and validity of the childhood trauma interview: a new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry. 1995;152:1329–1335. [DOI] [PubMed] [Google Scholar]
- [33].Spinhoven P, Penninx BW, Hickendorff M, van Hemert AM, Bernstein DP, Elzinga BM. Childhood Trauma Questionnaire: factor structure, measurement invariance, and validity across emotional disorders. Psychol Assess. 2014;26:717–729.doi: 10.1037/pas0000002. [DOI] [PubMed] [Google Scholar]
- [34].World Health Organization. Composite International Diagnostic Interview (CIDI): version 2.1. Geneva, Switzerland: World Health Organization, 1997. [Google Scholar]
- [35].Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28:57–84. [DOI] [PubMed] [Google Scholar]
- [36].MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- [37].De Venter M, Van Den Eede F, Pattyn T, Wouters K, Veltman DJ, BWJH P, et al. Impact of childhood trauma on course of panic disorder: contribution of clinical and personality characteristics. Acta Psychiatr Scand. 2017;135:554–563.doi: 10.1111/acps.12726. [DOI] [PubMed] [Google Scholar]
- [38].Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatr. 2004;45:260–273. [DOI] [PubMed] [Google Scholar]
- [39].Hardt J, Sidor A, Bracko M, Egle UT. Reliability of retrospective assessments of childhood experiences in Germany. J Nerv Ment Dis. 2006;194:676–683. [DOI] [PubMed] [Google Scholar]
- [40].Hardt J, Vellaisamy P, Schoon I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychol Rep. 2010;107:425–440. [DOI] [PubMed] [Google Scholar]
- [41].Lange A, Beurs E, Dolan C, Lachnit T, Sjollema S, Hanewald G. Long-term effects of childhood sexual abuse: objective and subjective characteristics of the abuse and psychopathology in later life. J Nervous Mental Dis. 1999;187:150–8. doi: 10.1097/00005053-199903000-00004. [DOI] [PubMed] [Google Scholar]
- [42].JR B, Reuben A, Newbury JB, Danese A. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76:584–593.doi: 10.1001/jamapsychiatry.2019.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Wielaard I, Stek ML, Comijs HC, Rhebergen D. Reliability of retrospective reports on childhood abuse and its determinants in older adults during a 6-year follow-up. J Psychiatr Res. 2018;105:9–16.doi: 10.1016/j.jpsychires.2018.08.009. [DOI] [PubMed] [Google Scholar]
- [44].Haüser W, Hoffmann E-M, Wolfe F, Worthing AB, Stahl N, Rothenberg R, et al. Self-reported childhood maltreatment, lifelong traumatic events and mental disorders in fibromyalgia syndrome: a comparison of US and German outpatients. Clin Exp Rheumatol. 2015;33(1 Suppl 88): S86–92. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are property of the NESDA consortium, represented by the NESDA principal investigator (PI) prof. Dr. B. W. J. H. Penninx. The total NESDA dataset is available on the internal NESDA website. Restrictions apply to the availability of these data, which were used under license for this study (collaboration agreement between the University of Antwerp and the NESDA consortium).