Abstract
Background
Black women are more likely to be diagnosed with later stage breast cancer compared to white women due to biological or access to care factors. Therefore, our objective was to identify whether racial/ethnic differences in patient experiences with healthcare are associated with stage at diagnosis.
Methods
We used the SEER registry data linked with patient surveys from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) completed prior to the diagnosis date. We examined responses about various aspects of their care such as the ability to get needed care, and to get care quickly. We used multivariable linear regression to examine racial/ ethnic differences in patient experiences, and a multivariable ordinal logistic regression to determine the association between patient experiences and earlier stage at diagnosis.
Results
Of the 10,144 patients, 80.7% were non-Hispanic white, 7.6% black, 7.1% Hispanic, and 4.6% Asian. After controlling for potential confounders, black patients had significantly lower mean scores for getting care quickly (β = −2.78), getting needed care (β = −2.26), getting needed prescription drugs (β = −3.83), and lower ratings of their health care (β = −2.33) compared to white patients. More importantly, we found that black patients who reported a 1-unit increase in rating of their experiences with customer service (OR 1.04, 95% CI 1.01–1.06) and the ability to get care quickly (OR 1.03, 1.01–1.05) had higher odds of earlier stage breast cancer.
Conclusion
Racial/ethnic minorities reported poorer patient experiences with care preceding a diagnosis of breast cancer. Better ratings among black patients were associated with earlier stage at diagnosis.
Keywords: Breast cancer, Consumer Assessment of Healthcare and Providers (CAHPS), Health care disparities, Patient experiences, Cancer stage
Introduction
Black and Hispanic women have a 2.5 and 1.5 times greater odds, respectively, of presenting with advanced disease as compared to non-Hispanic white women [1] and are more likely to die from the disease [2, 3]. Late stage at diagnosis is thought to relate to both biologically more aggressive hormone receptor-negative or triple-negative disease in black and Hispanic women [1, 4], and poorer access to mammography screening [5]. Disparities in cancer mortality result in part from differences in the receipt of effective evidence-based cancer treatment [3, 6]. The process of receiving appropriate cancer treatment is complex and fraught with many administrative barriers that can lead to racial/ethnic disparities in timely receipt of cancer treatment [7, 8]. Due to these complexities, the Institute of Medicine (IOM) and the National Cancer Institute (NCI) have released several reports that emphasize the importance of cancer treatment that focuses on the needs of patients and the use of patient-reported measures to evaluate the quality of care that they receive [9–11]. Thus, the racial/ethnic disparities in late stage at diagnosis and treatment emphasize the importance of high-quality medical care prior to the time of a breast cancer diagnosis.
Medical conditions that require routine treatment and follow-up are best managed in health care systems where the patients’ needs are a top priority [12–15]. One way to measure the quality of care that patients receive, which acknowledges a patient-centered care focus, is to ask them to rate aspects of their health care. Excellent experiences with access to needed medical care and care that is wellcoordinated among providers and delivered by physicians who communicate well with patients are associated with reduced inequities in care [16, 17], better health outcomes [18–20], and lower medical costs [19, 21, 22].
Racial/ethnic disparities in reporting excellent experiences with aspects of their healthcare are striking among patients with chronic diseases. For instance, Black and Hispanic patients with chronic conditions (e.g., hypertension, diabetes) are less likely to report excellent provider communication and care coordination among specialist providers as compared to non-Hispanic white patients [23, 24]. Among colorectal cancer patients, patient experiences have been linked to adherence to guideline survivorship care among colorectal cancer patients [25]. Thus, patient experiences such as the inability to get care quickly and get needed care may lead to delays in adherence to screening and breast cancer treatment resulting in later stage at diagnosis.
However, less is known about the patient experiences of breast cancer patients prior to their primary diagnosis and treatment and whether their experiences with care are associated with a later stage at diagnosis. Therefore, the purpose of this study was to identify racial/ethnic differences in patient experiences with medical care and to determine the association between their medical care experiences and stage at diagnosis.
Methods
Data source
We used the National Cancer Institute’s Surveillance, Epidemiology and End Results (SEER) program data linked to the Centers for Medicare and Medicaid Services (CMS) Medicare enrollment data, administrative claims, and the Consumer Assessment of Healthcare Providers and Systems (CAHPS) patient experience survey [26]. The SEER-CAHPS linked database is described in detail elsewhere [26]. Briefly, the SEER cancer registry data are available to identify cancer diagnosis, socioeconomic, demographic, prognostic, and initial treatment factors. The SEER cancer registry program collects and maintains patient demographic (date of birth, race/ethnicity, sex, marital status), tumor and clinical prognostic information (e.g., date of diagnosis, tumor stage (clinical and pathologic) and size, cell differentiation, axillary lymph node involvement, receptor-status, histology), and treatment information (surgery, radiation) on all individuals diagnosed with cancer while residing in participating cancer registry areas. The data also contain neighborhood-level socioeconomic information. We used data from the SEER registry-CAHPS Survey linked data to identify racial/ethnic differences in patient experiences with the delivery of their healthcare and interactions with their providers. The CAHPS survey was developed to assess patient experiences with health care providers and the care that patients received as a way to measure the quality of care. CMS has surveyed a nationally representative random sample of Medicare beneficiaries annually since 1998 on a wide variety of measures of perceived quality and access to care. The average response rate for Medicare patients is 71% [26].
Study cohort
We conducted a retrospective cohort analysis of women ≥ 65 years old diagnosed with breast cancer from 1997 to 2011 who completed a CAHPS survey on experiences with medical care at any time prior to the date of diagnosis. We excluded patients that were missing race/ethnicity data and since patients under the age of 65 years old may be eligible for Medicare if they are disabled or if they have end-stage renal disease we excluded them from the analysis since they do not represent the general Medicare population. For the patients who completed multiple surveys, the survey closest to the date of the first breast cancer diagnosis was analyzed.
Race/ethnicity
We developed a mutually exclusive variable by defining race/ethnicity identified in SEER with the following categories: Non-Hispanic white, Non-Hispanic black, Hispanic, Non-Hispanic Asian, and other. If a patient was categorized as being of Hispanic ethnicity in either SEER, Medicare or CAHPS datasets then the patient was considered to be Hispanic. We then used the self-reported race variable from CAHPS to categorize a patient’s race. If race was missing, we used the race variable from the SEER registry and then Medicare. 'Other' race was excluded from the analyses due to small sample size (n = 17).
Patient experiences with components of their healthcare
Five composite measures from CAHPS survey responses were utilized to assess patient experiences with: (1) customer service, (2) physician communication, (3) getting care quickly, (4) getting needed care, and (5) getting needed prescription drugs [27]. Each composite measure consisted of individual questions that ask patients how often (never, sometimes, usually, always) they experienced each of the following when needed: for ‘customer service’ (1) information from customer service, (2) were treated with respect; for ‘physician communication’ (1) doctors explained things in a way that they understood, (2) listened to their needs, (3) showed respect during their interaction, and (4) spent enough time with them; for ‘getting care quickly’ (1) got needed are right away and (2) got appointments when needed; for ‘getting needed care’ (1) got an appointment with specialist when needed, (2) got care, tests, and treatment when needed, (3) seen a personal doctor/nurse, and (4) had delays while waiting for approval; for ‘getting needed prescription drugs’ (1) got medicine prescribed by doctor, (2) filled prescription at local pharmacy easily, and (3) filled prescription by mail easily.
We also used four single-items (“global”) that measure patients’ experiences with their overall care, health plan, personal doctor, and specialist physician using a 0 to 100 rating scale. Missing values ranged from 6% for rating for health plan to 61% for experience with customer service because the items included in the questionnaire varied by survey year, did not apply to a particular patient, and/or to the Medicare plan type. Any missing values for both composite and single-item measures were excluded from the analyses.
Potential confounding
Age at the time of survey administration, individual-level education, Medicare insurance type (Medicare Advantage with part D coverage plan (MA PDP) and without part D coverage plan (MA), and fee-for-service with part D coverage plan (FFS PDP) and without part D coverage plan (FFS)), and count of self-reported comorbidities other than cancer were obtained from CAHPS data. Marital status, geographical region (West, Midwest, Northeast, South), and neighborhood poverty level based on the census tract of the address at diagnosis of breast cancer were identified from the SEER registry data.
Statistical analysis
We first examined the distribution of demographic and prognostic factors by race/ethnicity and then we examined the mean patient experiences with care using t tests and chi-squared analysis, where appropriate. To examine associations between race/ethnicity and mean ratings of patient experiences, adjusted least-square estimates and standard errors were calculated using separate linear regression analysis methods for each composite and global rating of care. There was a significant interaction between race/ethnicity and patient experiences with care and stage at diagnosis (p < 0.05); therefore, we conducted adjusted ordinal logistic regressions, stratified by race/ethnicity, for stage at diagnosis (stage 0, I, II, III, and IV) for each composite and global measure controlling for the confounding variables [28, 29]. The order of the ordinal categories was set at stage IV lowest to stage 0 highest so that odds ratios greater than 1 reflect earlier stage at diagnosis. All analyses were performed using SAS statistical software version 9.4 (SAS Institute Inc, Cary NC) with an alpha of 0.05.
Results
A total of 10,144 subjects were identified after applying inclusion and exclusion criteria. A majority of the cohort were non-Hispanic white patients (80.7%), followed by non-Hispanic black patients, Hispanic and Asian patients (7.6%, 7.1%, and 4.6%, respectively). Table 1 describes the baseline characteristics of subjects by race. The mean age of the total cohort was 74.3 (± 6.1) years. A smaller proportion of Non-Hispanic black patients were married (23.9%) compared to other racial/ethnic groups. The poverty rates varied greatly by race and were highest for non-Hispanic black patients (51.5%) and Hispanic patients (21.8%) compared to non-Hispanic white patients (12.1%) and Asian patients (13.1%). Non-Hispanic black and Hispanic patients were less likely to report completing some college or higher education (25.4%, 25.5%) than other race groups. More than half of the cohort (58.5%) lived in the West region, however, the regions varied by racial and ethnic groups. A considerably higher percentage of non-Hispanic black patients lived in the South (42.2%) and 80.2% of Asian patients lived in the West. Non-Hispanic black patients had the lowest percentage of people with FFS PDP (49.6%) compared to Hispanic patients (63.2%).
Table 1.
Distribution of sociodemographic characteristics for women diagnosed with breast cancer from 1997 to 2011
| Total | Non-Hispanic white | Non-Hispanic Black | Hispanic | Asian | |
|---|---|---|---|---|---|
| No. of subjects n (%) | 10,144 | 8,187 (80.7) | 773 (7.6) | 717 (7.1) | 467 (4.6) |
| Mean age at survey (± SD) | 74.3 (± 6.1) | 74.4 (± 6.2) | 74.0 (± 6.4) | 73.5 (± 5.7) | 73.8 (± 5.7) |
| Age at survey | |||||
| 65–70 | 2,785 (27.4) | 2,196 (26.8) | 236 (30.5) | 221 (30.8) | 132 (28.3) |
| 70–75 | 3,011 (29.7) | 2,412 (29.5) | 226 (29.2) | 225 (31.4) | 148 (31.7) |
| 75–80 | 2,395 (23.6) | 1,943 (23.7) | 167 (21.6) | 173 (24.1) | 112 (24.0) |
| 80–85 | 1,308 (12.9) | 1,101 (13.5) | 88 (11.4) | 66 (9.2) | 53 (11.4) |
| 85 or older | 645 (6.4) | 535 (6.5) | 56 (7.2) | 32 (4.5) | 22 (4.7) |
| Marital status | |||||
| Unmarried | 5,578 (55.0) | 4,414 (53.9) | 548 (70.9) | 385 (53.7) | 231 (49.5) |
| Married | 4,036 (39.8) | 3,347 (40.9) | 185 (23.9) | 295 (41.1) | 209 (44.8) |
| Unknown | 530 (5.2) | 426 (5.2) | 40 (5.2) | 37 (5.2) | 27 (5.8) |
| Census tract poverty | |||||
| 0% to < 5% (low poverty) | 2,756 (27.2) | 2,416 (29.5) | 65 (8.4) | 126 (17.6) | 149 (31.9) |
| 5% to < 10% | 2,946 (29.0) | 2,505 (30.6) | 107 (13.8) | 200 (27.9) | 134 (28.7) |
| 10% to < 20% | 2,683 (26.5) | 2,166 (26.5) | 186 (24.1) | 214 (29.9) | 119 (25.5) |
| 20% to 100% (high poverty) | 1,609 (15.9) | < 13% | < 52% | 156 (21.8) | < 14% |
| Missing | 148 (1.5) | < 2% | < 3% | 21 (2.9) | < 3% |
| Education level | |||||
| High school or less | 5,543 (54.6) | 4296 (52.5) | 512 (66.2) | 487 (67.9) | 248 (53.1) |
| College and higher | 4016 (40.0) | 344 (42.1) | 196 (25.4) | 183 (25.5) | 193 (41.3) |
| Missing | 585 (5.8) | 447 (5.5) | 65 (8.4) | 47 (6.6) | 26 (5.6) |
| Region | |||||
| West | 5,931 (58.5) | 4,693 (57.3) | 221 (28.6) | 575 (80.2) | 442 (94.7) |
| Midwest | 725 (7.2) | 646 (7.9) | 65 (8.4) | < 2% | < 3% |
| Northeast | 1,732 (17.1) | 1,458 (17.8) | 161 (20.8) | 100 (14.0) | 13 (2.8) |
| South | 1,756 (17.3) | 1,390 (17.0) | 326 (42.2) | < 5% | < 3% |
| Medicare type | |||||
| FFS onlya | 1,047 (10.3) | 746 (9.1) | 127 (16.4) | 104 (14.5) | 70 (15.0) |
| FFS PDP | 5,826 (57.4) | 4,696 (57.4) | 383 (49.6) | 453 (63.2) | 294 (63.0) |
| MA only | 817 (8.1) | 660 (8.1) | 86 (11.1) | 48 (6.7) | 23 (4.9) |
| MA PDP | 2,454 (24.2) | 2,085 (25.5) | 177 (22.9) | 112 (15.6) | 80 (17.1) |
| Survey method | |||||
| 8,512 (83.9) | 6,983 (85.3) | 571 (73.9) | 541 (75.5) | 417 (89.3) | |
| Phone | 1,632 (16.1) | 1,204 (14.7) | 292 (26.1) | 176 (24.6) | 50 (10.7) |
| Count of comorbidities | |||||
| 0 | 8,520 (84.0) | 6,938 (84.7) | 614 (79.4) | 582 (81.2) | 386 (82.7) |
| 1 | 1,235 (12.2) | 963 (11.8) | 109 (14.1) | 98 (13.7) | 65 (13.9) |
| 2 + | 389 (3.8) | 286 (3.5) | 50 (6.5) | 37 (5.2) | 16 (3.4) |
| Survey year | |||||
| 1997–2000 | 3,352 (33.0) | 2,767 (33.8) | 212 (27.4) | 217 (30.3) | 156 (33.4) |
| 2001–2005 | 4,442 (43.8) | 3,614 (44.1) | 305 (39.5) | 326 (45.5) | 197 (42.2) |
| 2007–2011 | 2,350 (23.2) | 1,806 (22.1) | 256 (33.1) | 174 (24.3) | 114 (24.4) |
Fee-for-service (FFS) and medicare advantage (MA) with and without part D coverage
The mean composite score and rating of care in patients’ experiences with the health care delivery system are shown in Table 2 for composite ratings and Table 3 for global ratings. Each outcome has a different number of subjects because the valid response rate for each item varied by survey year, visit experiences, and Medicare programs. The number of subjects included in the analyses ranged from 3,965 (customer service) to 9,534 (health plan) and the mean rating of experiences varied from 83.3 (getting care quickly) to 94.0 (health plan). There were significant racial/ethnic di?erences in mean composite scores and global rating. Asian patients reported the lowest mean score for getting care quickly (78.29 ± 1.62), Hispanic patients reported the lowest mean score for getting needed care (84.76 ± 1.13), and Non-Hispanic black patients reported the lowest mean score for getting needed prescription drugs (85.76 ± 1.21) compared to other racial/ ethnic groups (p < 0.05). In addition, non-Hispanic black patients reported the lowest mean score for overall health care (84.46 ± 0.89, p < 0.05) compared to other racial/ethnic groups.
Table 2.
Description of patient demographics and report of their experiences with the health care delivery system (composite ratings)
| Customer service | Physician communication | Getting care quickly | Getting needed care | Getting needed prescription drugs | |
|---|---|---|---|---|---|
| No. analyzed n (%) | 3965 (39.1) | 7962 (75.8) | 7,290 (71.9) | 8,534 (84.1) | 8,265 (81.5) |
| Mean score (± SD) | 83.6 (26.2) | 87.6 (17.5) | 83.3 (23.8) | 89.2 (20.6) | 89.4 (23.2) |
| Total n (%) | 62.4 (2475) | 65.4 (5028) | 58.9 (4296) | 70.2 (5993) | 76.5 (6319) |
| Race/ethnicity | |||||
| Non-Hispanic white | 76.50 (± 1.47) | 88.57 (± 0.65) | 83.04 (± 0.90) | 88.09 (± 0.76) | 89.59 (± 0.84) |
| Non-Hispanic black | 74.12 (± 2.05) | 88.85 (± 0.95) | 80.26 (± 1.34) | 85.83 (± 1.09) | 85.76 (± 1.21) |
| Hispanic | 73.54 (± 2.08) | 88.53 (± 1.01) | 82.06 (± 1.39) | 84.76 (± 1.13) | 87.56 (± 1.26) |
| Asian | 76.69 (± 2.67) | 89.48 (± 1.18) | 78.29 (± 1.62) | 86.74 (± 1.32) | 87.92 (± 1.49) |
| Age at survey | |||||
| 65–70 | 76.84 (± 1.68) | 88.73 (± 0.77) | 80.67 (± 1.06) | 85.73 (± 0.89) | 86.24 (± 0.99) |
| 70–75 | 75.63 (± 1.69) | 88.90 (± 0.76) | 80.65 (± 1.05) | 85.91 (± 0.88) | 86.51 (± 0.97) |
| 75–80 | 76.68 (± 1.74) | 88.21 (± 0.79) | 80.41 (± 1.10) | 87.00 (± 0.91) | 87.36 (± 1.01) |
| 80–85 | 74.20 (± 1.96) | 89.47 (± 0.88) | 81.27 (± 1.22) | 87.11 (± 1.00) | 89.15 (± 1.12) |
| 85 or older | 72.72 (± 2.40) | 88.99 (± 1.08) | 81.56 (± 1.48) | 86.03 (± 1.21) | 89.27 (± 1.36) |
| Marital status | |||||
| Unmarried | 76.38 (± 1.57) | 89.02 (± 0.69) | 81.30 (± 0.95) | 86.16 (± 0.80) | 87.56 (± 0.89) |
| Married | 77.57 (± 1.67) | 89.87 (± 0.74) | 80.90 (± 1.01) | 87.83 (± 0.85) | 88.47 (± 0.95) |
| Unknown | 71.69 (± 2.24) | 87.69 (± 1.08) | 80.53 (± 1.51) | 85.09 (± 1.22) | 87.09 (± 1.36) |
| Census tract poverty | |||||
| 0% to < 5% poverty | 75.72 (± 1.66) | 88.81 (± 0.76) | 82.14 (± 1.05) | 86.62 (± 0.86) | 86.77 (± 0.97) |
| 5% to < 10% poverty | 75.38 (± 1.64) | 88.93 (± 0.75) | 81.65 (± 1.04) | 86.73 (± 0.85) | 87.55 (± 0.95) |
| 10% to < 20% poverty | 74.73 (± 1.64) | 88.73 (± 0.75) | 81.37 (± 1.03) | 86.15 (± 0.86) | 87.43 (± 0.95) |
| 20% to 100% poverty | 75.02 (± 1.72) | 88.59 (± 0.79) | 82.15 (± 1.09) | 86.10 (± 0.91) | 87.05 (± 1.00) |
| Missing | 75.21 (± 3.92) | 89.23 (± 1.71) | 77.25 (± 2.35) | 86.18 (± 2.01) | 89.73 (± 2.21) |
| Education level | |||||
| High school or less | 76.46 (± 1.53) | 88.91 (± 0.68) | 89.89 (± 1.09) | 87.68 (± 0.79) | 87.87 (± 0.87) |
| College and higher | 73.79 (± 1.61) | 87.79 (± 0.74) | 81.10 (± 1.02) | 85.52 (± 0.84) | 87.32 (± 0.94) |
| Missing | 75.39 (± 2.37) | 89.89 (± 1.09) | 79.18 (± 1.49) | 85.87 (± 1.26) | 87.94 (± 1.41) |
| Region | |||||
| West | 77.03 (± 1.55) | 87.92 (± 0.70) | 79.08 (± 0.96) | 84.54 (± 0.81) | 89.40 (± 0.89) |
| Midwest | 76.55 (± 2.38) | 89.11 (± 1.03) | 82.19 (± 1.41) | 87.64 (± 1.16) | 87.39 (± 1.29) |
| Northeast | 71.48 (± 1.81) | 88.81 (± 0.83) | 81.38 (± 1.15) | 86.16 (± 0.95) | 86.35 (± 1.07) |
| South | 75.78 (± 1.81) | 89.60 (± 0.84) | 81.00 (± 1.16) | 87.08 (± 0.96) | 87.69 (± 1.07) |
| Medicare type | |||||
| FFS onlya | 74.04 (± 1.86) | 87.90 (± 0.82) | 83.09 (± 1.13) | 89.84 (± 0.93) | 90.53 (± 1.05) |
| FFS PDP | 68.45 (± 2.87) | 90.48 (± 0.94) | 79.64 (± 1.29) | 84.91 (± 1.13) | 86.58 (± 1.19) |
| MA only | 80.42 (± 1.59) | 87.02 (± 0.77) | 80.60 (± 1.05) | 87.21 (± 0.87) | 84.23 (± 0.98) |
| MA PDP | 77.93 (± 1.91) | 90.04 (± 0.90) | 80.31 (± 1.22) | 83.46 (± 1.07) | 89.49 (± 1.12) |
| Count of comorbidities | |||||
| 0 | 76.37 (± 1.54) | 89.32 (± 0.67) | 80.69 (± 0.92) | 86.97 (± 0.77) | 90.02 (± 0.85) |
| 1 | 75.89 (± 1.79) | 89.89 (± 0.82) | 81.04 (± 1.13) | 87.19 (± 0.95) | 85.97 (± 1.05) |
| 2 + | 73.38 (± 2.36) | 87.36 (± 1.14) | 81.01 (± 1.56) | 84.91 (± 1.31) | 87.13 (± 1.46) |
Bolded means are significant at p < 0.05
Fee-for-service (FFS) and Medicare Advantage (MA) with and without part D coverage
Table 3.
Description of patient demographics and report of their mean rating of experiences with the health care delivery system (global ratings)
| Health care | Health plan | Primary physician | Specialist physician | |
|---|---|---|---|---|
| No. analyzed n (%) | 7718 (76.1) | 9534 (94.0) | 8401 (82.8) | 4946 (48.8) |
| Mean score (± SD) | 87.9 (16.2) | 85.6 (18.0) | 88.5 (16.4) | 87.8 (17.9) |
| Total % (n) | 66.7 (5151) | 61.8 (5889) | 68.1 (5722) | 69.0 (3413) |
| Race/ethnicity | ||||
| Non-Hispanic white | 86.79 (± 0.61) | 85.88 (± 0.61) | 90.10 (± 0.60) | 87.87 (± 0.85) |
| Non-Hispanic black | 84.46 (± 0.89) | 86.03 (± 0.89) | 90.08 (± 0.87) | 87.94 (± 1.32) |
| Hispanic | 85.74 (± 0.93) | 85.63 (± 0.91) | 90.24 (± 0.90) | 87.23 (± 1.30) |
| Asian | 86.05 (± 1.09) | 84.86 (± 1.07) | 89.85 (± 1.04) | 85.13 (± 1.61) |
| Age at survey | ||||
| 65–70 | 85.91 (± 0.71) | 85.05 (± 0.72) | 89.80 (± 0.69) | 87.18 (± 1.01) |
| 70–75 | 85.74 (± 0.74) | 86.21 (± 0.74) | 89.59 (± 0.72) | 86.78 (± 1.04) |
| 75–80 | 86.69 (± 0.81) | 86.99 (± 0.82) | 91.21 (± 0.79) | 88.27 (± 1.15) |
| 80–85 | 85.74 (± 0.99) | 86.43 (± 0.98) | 91.04 (± 0.96) | 86.79 (± 1.41) |
| 85 or older | 84.73 (± 0.71) | 83.34 (± 0.72) | 88.69 (± 0.70) | 86.19 (± 1.02) |
| Marital status | ||||
| Unmarried | 86.30 (± 0.64) | 86.03 (± 0.65) | 90.43 (± 0.63) | 87.58 (± 0.92) |
| Married | 86.71 (± 0.68) | 85.91 (± 0.69) | 90.51 (± 0.67) | 87.32 (± 0.98) |
| Unknown | 84.27 (± 1.00) | 84.87 (± 0.99) | 89.26 (± 0.97) | 86.23 (± 1.39) |
| Census tract poverty | ||||
| 0% to < 5% (low poverty) | 85.71 (± 0.70) | 85.28 (± 0.71) | 89.81 (± 0.69) | 88.16 (± 0.97) |
| 5% to < 10% | 85.28 (± 0.69) | 85.51 (± 0.70) | 89.28 (± 0.68) | 87.29 (± 0.96) |
| 10% to < 20% | 85.75 (± 0.69) | 85.96 (± 0.70) | 89.86 (± 0.68) | 86.59 (± 0.97) |
| 20% to 100% (high poverty) | 86.68 (± 0.73) | 85.73 (± 0.74) | 90.16 (± 0.71) | 87.30 (± 1.05) |
| Missing | 85.38 (± 1.58) | 85.54 (± 1.61) | 91.22 (± 1.56) | 85.87 (± 2.38) |
| Education level | ||||
| High school or less | 86.22 (± 0.63) | 87.52 (± 0.64) | 90.54 (± 0.62) | 88.31 (± 0.91) |
| College and higher | 85.15 (± 0.68) | 83.69 (± 0.69) | 89.30 (± 0.67) | 86.52 (± 0.96) |
| Missing | 85.91 (± 1.01) | 85.59 (± 1.02) | 90.36 (± 0.99) | 86.30 (± 1.43) |
| Region | ||||
| West | 84.62 (± 0.65) | 85.74 (± 0.65) | 89.18 (± 0.63) | 86.22 (± 0.93) |
| Midwest | 85.97 (± 0.95) | 86.39 (± 0.95) | 89.91 (± 0.91) | 86.20 (± 1.34) |
| Northeast | 85.89 (± 0.77) | 83.29 (± 0.78) | 90.45 (± 0.76) | 86.93 (± 1.08) |
| South | 86.56 (± 0.77) | 86.99 (± 0.78) | 90.72 (± 0.76) | 88.82 (± 1.10) |
| Medicare type | ||||
| FFS onlya | 87.53 (± 0.76) | 86.15 (± 0.76) | 89.87 (± 0.74) | 87.53 (± 1.06) |
| FFS PDP | 85.00 (± 0.87) | 85.61 (± 0.90) | 91.71 (± 0.87) | 88.31 (± 1.23) |
| MA only | 86.52 (± 0.71) | 85.12 (± 0.71) | 88.07 (± 0.69) | 86.38 (± 0.99) |
| MA PDP | 83.99 (± 0.82) | 85.53 (± 0.83) | 90.61 (± 0.83) | 85.96 (± 1.22) |
| Count of comorbidities | ||||
| 0 | 86.67 (± 0.62) | 85.31 (± 0.61) | 90.19 (± 0.60) | 86.53 (± 0.90) |
| 1 | 86.73 (± 0.76) | 85.91 (± 0.77) | 91.20 (± 0.74) | 87.16 (± 1.08) |
| 2 + | 83.88 (± 1.05) | 85.59 (± 1.09) | 88.80 (± 1.05) | 87.44 (± 1.42) |
Bolded models are significant at p < 0.05
Fee-for-service (FFS) and medicare advantage (MA) with and without part D coverage
Regression analyses
Composite scores
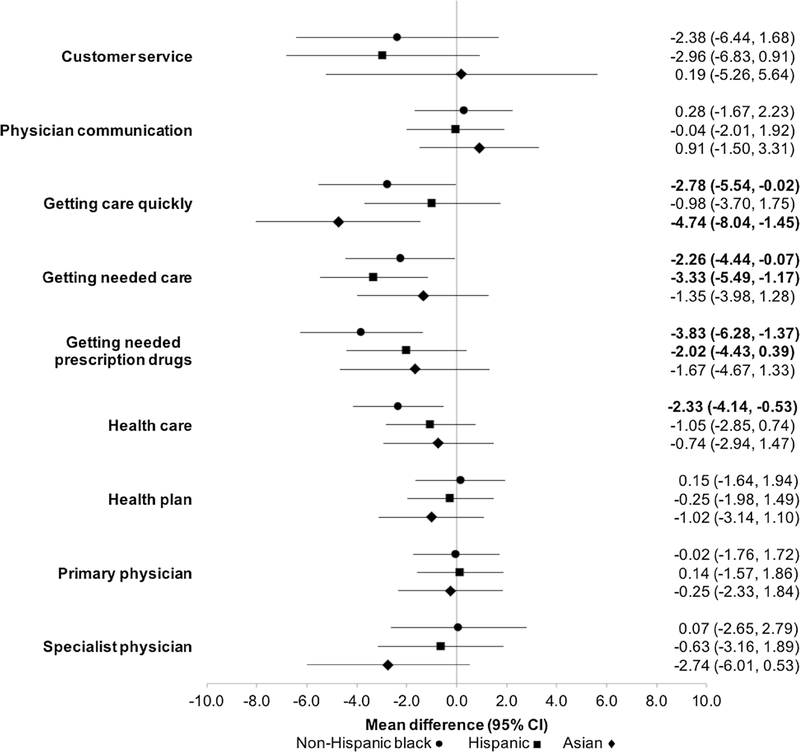
Adjusted regression analyses for composite scores and global ratings by race/ethnicity are presented in Fig. 1. Each score/ rating represents a regression model adjusted for covariates. Coefficients reflect the mean difference in composite score or global rating for each racial/ethnic group compared to non-Hispanic white patients. Non-Hispanic black patients had significantly lower adjusted mean scores for getting care quickly (β = −2.78), getting needed care (β = −2.26), and getting needed prescription drugs (β = −3.83) compared to Non-Hispanic white patients. Hispanic patients also had significantly lower adjusted mean composite scores for getting needed care (β = −3.33) and getting needed prescription drugs (β = −2.02), and Asian patients had significantly lower adjusted mean scores for getting care quickly (β = 4.74), compared to Non-Hispanic white patients.
Fig. 1.
Adjusted mean difference of patient experiences with aspects of their health care by race/ethnicity compared to non-Hispanic white patients (composite scores and ratings). Adjusted for age at survey, marital status at diagnosis, census tract poverty indicator, education level, time from survey to diagnosis, SEER region, Medicare type, and comorbidity
Global ratings of care
There were significant racial/ethnic differences in adjusted mean global ratings of healthcare, where non-Hispanic black patients had significantly lower ratings of their health care (β = −2.33) and Asian patients had lower ratings with specialist physician (β = −2.74) compared to non-Hispanic white patients prior to the date of diagnosis.
Ordinal logistic regression
The results from the adjusted ordinal logistic regression models are presented in Table 4, which show the association composite and global ratings of care and cancer stage among each racial/ethnic group. Among non-Hispanic black patients those who had a one unit increase in rating for customer service had 4 percent increased odds of having earlier stage at diagnosis (OR 1.04; 95% CI 1.01–1.06; p < 0.05). Similarly, among non-Hispanic black patients, those who had a one unit increase in rating in their ability to get care quickly had three percent increased odds of having earlier stage diagnosis (OR 1.03; 95% CI 1.01–1.05; p < 0.05). Asian patients who had one unit increase in rating in getting needed prescription drugs had two percent decreased odds of having earlier stage at diagnosis (OR 0.98; 95% CI 0.95–1.00; p < 0.05). We did not observe a significant association between any of the patient experiences with care and stage at diagnosis among non-Hispanic white or Hispanic breast cancer patients prior to their diagnosis.
Table 4.
Multivariable ordinal logistic regression model of patient experiences with rating of health care and earlier stage at diagnosis, by race/ethnicity
| No. analyzed | Non-Hispanic white | Non-Hispanic black | Hispanic | Asian | |
|---|---|---|---|---|---|
| Experience with | |||||
| Customer service | 3,693 | 1.00 (0.99–1.01) | 1.04 (1.01–1.06) | 1.01 (0.99–1.04) | 0.97 (0.93–1.01) |
| Physician communication | 7,209 | 1.00 (0.99–1.01) | 1.03 (1.00–1.05) | 1.01 (0.98–1.04) | 0.98 (0.94–1.014) |
| Getting care quickly | 6,831 | 1.00 (0.99–1.01) | 1.03 (1.01–1.05) | 1.01 (0.99–1.03) | 0.99 (0.97–1.02) |
| Getting needed care | 8,002 | 1.00 (0.99–1.01) | 1.01 (0.99–1.03) | 1.00 (0.98–1.02) | 0.99 (0.96–1.01) |
| Getting needed Rx drugs | 7,758 | 0.99 (0.99–1.00) | 1.21 (0.98–1.50) | 0.99 (0.98–1.01) | 0.98 (0.95–1.00) |
| Rating for | |||||
| Health care | 7,236 | 1.00 (0.99–1.01) | 1.00 (0.98–1.03) | 1.00 (0.97–1.02) | 0.99 (0.95–1.02) |
| Health plan | 8,939 | 1.00 (0.99–1.01) | 1.01 (0.98–1.03) | 1.00 (0.98–1.02) | 0.98 (0.95–1.01) |
| Primary physician | 7,892 | 1.01 (0.99–1.01) | 1.02 (0.99–1.05) | 1.03 (0.99–1.04) | 0.99 (0.96–1.03) |
| Specialist physician | 4,653 | 0.99 (0.98–1.00) | 0.98 (0.94–1.02) | 1.01 (0.98–1.04) | 0.99 (0.95–1.03) |
Adjusted for age at survey, marital status at diagnosis, census tract poverty indicator, education level, time from survey to diagnosis, SEER region, Medicare type, and comorbidities
Bolded models are significant at p < 0.05
Discussion
In this large retrospective cohort study, we used data from the SEER-CAHPS linked dataset to investigate whether there are racial/ethnic disparities in patient experiences with aspects of their medical care among breast cancer patients prior to their cancer diagnosis and their possible association with stage of diagnosis. After controlling for demographic and health characteristics, we found disparities in mean adjusted scores between non-Hispanic white patients and other racial/ethnic groups. Non-Hispanic black, Hispanic, and Asian breast cancer patients reported lower mean scores of getting care quickly, getting needed care, getting needed prescription drugs, and ratings of overall health care prior to their date of diagnosis. More importantly, we also found that patient experiences matter more for certain racial/ethnic groups when we examined stage at diagnosis. Non-Hispanic black patients with higher ratings of customer service and getting care quickly had increased odds of having earlier cancer stage at diagnosis.
The results from this study suggest that significant racial/ ethnic differences exist for getting care quickly, getting needed care, getting needed prescription drugs, and overall health care experience. The poorer ratings with health care are consistent with earlier work among a general sample of Medicare managed care patients that found Non-Hispanic black patients reported worse experiences with care than Non-Hispanic white patients [30]. Other studies have also shown that racial/ethnic minority patients with other chronic conditions were more likely to report worse patient experiences with care than non-Hispanic white patients [31–34].
Our results also show that Hispanic patients had significantly lower scores for getting needed care and getting needed prescription drugs, while Asian patients reported significantly lower scores for getting care quickly, compared to Non-Hispanic whites. These findings suggest that the significant racial/ethnic disparities that exist are in patient’s access to health care services. This is supported by other studies that have found similar disparities in patient experience with care among Asian and Hispanic patients [34, 35]. For example, a study by Paddison and colleagues found that minority patients with end-stage renal disease are more likely than non-Hispanic white patients to report poor experience with care, specifically on getting care quickly, getting needed prescription drugs, and getting needed care with a specialist physician [32].
Interestingly, our results show no significant racial/ethnic differences for patient scores and ratings on physician communication, primary physician, and specialist physician communication. This suggests that patients perceived their interactions with medical providers similarly, which supports the general pattern that patients who are diagnosed with life-threatening non-acute illnesses (i.e., cancer) typically report higher satisfaction and greater patient experiences than patients without these conditions [36]. This may be attributed to the frequent contact that patients typically have with their providers over an extended period of time. While our study suggests no significant differences in patients experience with physician communication prior to diagnosis, other studies that have surveyed breast cancer survivors have found contrasting results. A study by Palmer et al., found that compared to white survivors, Hispanic and Asian survivors reported poorer overall communication, and Asian survivors were less likely to report high quality of care [31]. This is particularly important when considering the impact of poor provider-patient communication can prematurely have on patient’s stage of diagnosis, perceptions of care, and adherence to medical appointments. A study by Peterson and colleagues found provider-patient communication is particularly important because provider recommendations are a necessary component for optimal adherence to cancer screening, which is critical for reducing patient’s risk of late-stage diagnosis [37]. Although our study found no racial/ethnic differences in physician communication, these findings suggest that there are no racial/ ethnic disparities in provider-patient communication prior to diagnosis, but that the significant disparities may arise after diagnosis among oncologists and other providers related to diagnosis and treatment.
Our study puts forward that racial disparities persist for patient experiences with care and that among certain racial/ethnic groups these patient experiences with care are an important predictor of stage at breast cancer diagnosis. In particular, the lower scores and ratings for getting care quickly, getting needed care, getting needed prescription drugs, health care and physician specialty may reflect worse access to care and lower quality of care for minority patients prior to diagnosis. Additionally, as our study suggests, poor patient experiences with care may contribute to later stage at diagnosis for non-Hispanic black patients. To the best of our knowledge, no studies have examined the association between patient experience with care and later stage at diagnosis. A study by Tatalovich and colleagues found higher rates of late-stage breast cancer in areas with low socioeconomic status and screening availability and with high levels of racial segregation [38]. Other factors associ ated with late stage at diagnosis include low income and racial/ethnic minority groups [39–41], lower levels of education [42], health insurance status [42], health care access [43], and neighborhood context such as areas of residence socioeconomic status (SES) and urban versus rural settings [44–46], which we were able to control for in our study. Our findings contribute to this literature by demonstrating that patient experiences with care, at least for non-Hispanic black patients, is also associated with later stage at diagnosis. Patient experiences such as an inability to get care quickly and get needed care, both self-reported measures of health care access, may lead to non-adherence to screening guidelines and delays in diagnosis after abnormal screening; this may result in later stage at breast cancer diagnosis. However, more research is needed to tease apart the directionality of the association. In other words, whether patients with poor medical experiences tend to have poor screening behaviors and have poor access to care, or whether a lack of screening and access to care leads to poor patient experiences with care will need to be examined further.
Our study had a few limitations. First, patient experiences with care were assessed at one snapshot in time prior to their breast cancer diagnosis and may presumably change over time due to the use of medical services and health care needs. However, in a sensitivity analysis where we stratified the analysis based on the time from survey completion to the date of diagnosis, we found that patient experiences with care were similarly associated with stage at diagnosis even among those patients that completed the survey greater than 3 years prior to their date of diagnosis. Second, questions in patient experience with care were related to overall experience with medical care rather than care related specifically to breast cancer screening and diagnosis because patients had not yet received a breast cancer diagnosis at the time the survey was administered. Third, the study population was limited to patients age 65 and older enrolled in Medicare fee-for-service and Medicare advantage who were diagnosed with cancer within the SEER-registry regions; thus, results may not be generalizable to younger cancer survivors. Fourth, to be included in the study, individuals had to be able to complete a CAHPS survey and although proxies were able to complete a survey on behalf of the individual, we may have fewer individuals in poorer health prior to a breast cancer diagnosis. Finally, we did not have information pertaining to the type of setting (academic center, community clinic, private, etc.) in which the patient received their care. The type of setting where patients received their care could act as confounder to the differences in patient experiences observed in this study [47].
In conclusion, our findings show higher ratings of a patient’s ability to get care quickly and customer services are associated with earlier stage at breast cancer diagnosis among non-Hispanic black Medicare beneficiaries; however, more research is needed to identify the mechanism that leads to these disparities. A mixed methods approach is needed to better understand what factors are influencing racial differences in patient experiences with care and the mechanism by which patient experiences with care may lead to earlier stage at cancer diagnosis, such as improvements in breast cancer screening adherence and shorter time periods between abnormal detection to diagnosis and treatment. These findings are particularly important for identifying and reducing disparities in cancer stage at diagnosis and underscore the importance of patient-centered medical care.
Acknowledgments
The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Centers for Medicare & Medicaid Services; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-CAHPS database.
Funding A.J.F was a postdoctoral fellow supported by a University of Texas Health Science Center at Houston School of Public Health Cancer Education and Career Development Program grant from the National Cancer Institute (Grant No. R25-CA57712). This study used the linked SEER-CAHPS database.
Footnotes
Compliance with ethical standards
Conflict of interest The authors declare that they have no conflict of interests.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affliations.
References
- 1.Ooi SL, Martinez ME, Li CI (2011) Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Res Treat 127(3):729–738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banegas MP, Li CI (2012) Breast cancer characteristics and outcomes among Hispanic Black and Hispanic White women. Breast Cancer Res Treat 134(3):1297–1304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silber JH, Rosenbaum PR, Clark AS et al. (2013) Characteristics associated with differences in survival among black and white women with breast cancer. JAMA 310(4):389–397 [DOI] [PubMed] [Google Scholar]
- 4.Farias AJ, Du XL (2017) Racial differences in adjuvant endocrine therapy use and discontinuation in association with mortality among Medicare breast cancer patients by receptor status. Cancer Epidemiol Biomark Prev 26:1266–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tabar L, Yen MF, Vitak B, Chen HH, Smith RA, Duffy SW (2003) Mammography service screening and mortality in breast cancer patients: 20-year follow-up before and after introduction of screening. Lancet 361(9367):1405–1410 [DOI] [PubMed] [Google Scholar]
- 6.Du XL, Fang S, Meyer TE (2008) Impact of treatment and socioeconomic status on racial disparities in survival among older women with breast cancer. Am J Clin Oncol 31(2):125–132 [DOI] [PubMed] [Google Scholar]
- 7.Hewitt M, Greenfield S, Stovall E (2005) From cancer patient to cancer survivor: lost in transition. The National Academies Press, Washington, DC [Google Scholar]
- 8.Taplin SH, Anhang Price R, Edwards HM et al. (2012) (2012) Introduction: understanding and influencing multilevel factors across the cancer care continuum. J Natl Cancer Inst Monogr 44:2–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niederhuber J (2011) Institute of Medicine (IOM) workshop. Oncologist 16(12):1665–1666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institute of Medicine (2013) Delivering high-quality cancer care: charting a new course for a system in crisis. The National Academies Press, Washington, DC: [PubMed] [Google Scholar]
- 11.Rowland JH, Hewitt M, Ganz PA (2006) Cancer survivorship: a new challenge in delivering quality cancer care. J Clin Oncol 24(32):5101–5104 [DOI] [PubMed] [Google Scholar]
- 12.Starfield B, Shi L (2004) The medical home, access to care, and insurance: a review of evidence. Pediatrics 113:1493–1498 [PubMed] [Google Scholar]
- 13.Epstein RM, Street RL Jr. (2011) The values and value of patient-centered care. Ann Fam Med 9(2):100–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis K, Schoenbaum SC, Audet AM (2005) A 2020 vision of patient-centered primary care. J Gen Intern Med 20(10):953–957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hudon C, Fortin M, Haggerty JL, Lambert M, Poitras ME (2011) Measuring patients’ perceptions of patient-centered care: a systematic review of tools for family medicine. Ann Fam Med 9(2):155–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beal A, Hernandez S, Doty M (2009) Latino access to the patient-centered medical home. J Gen Intern Med 24:514–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferrer RL (2007) Pursuing equity: contact with primary care and specialist clinicians by demographics, insurance, and health status. Ann Fam Med 5(6):492–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alexander JA, Bae D (2012) Does the patient-centred medical home work? A critical synthesis of research on patient-centred medical homes and patient-related outcomes. Health Serv Manag Res 25(2):51–59 [DOI] [PubMed] [Google Scholar]
- 19.Reid RJ, Coleman K, Johnson EA et al. (2010) The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff 29(5):835–843 [DOI] [PubMed] [Google Scholar]
- 20.Reid RJ, Fishman PA, Yu O et al. (2009) Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care 15(9):e71–87 [PubMed] [Google Scholar]
- 21.Baicker K, Chandra A (2004) Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Aff 23:W4–W184 [DOI] [PubMed] [Google Scholar]
- 22.Greenfield S, Nelson EC, Zubkoff M, et al. (1992) Variations in resource utilization among medical specialties and systems of care. Results from the medical outcomes study. JAMA 267(12):1624–1630 [PubMed] [Google Scholar]
- 23.Smith LM, Anderson WL, Kenyon A et al. (2015) Racial and Ethnic disparities in patients’ experience with skilled home health care services. Med Care Res Rev 72(6):756–774 [DOI] [PubMed] [Google Scholar]
- 24.Zhu J, Weingart SN, Ritter GA, Tompkins CP, Garnick DW (2015) Racial/Ethnic disparities in patient experience with communication in hospitals: real differences or measurement errors? Med Care 53(5):446–454 [DOI] [PubMed] [Google Scholar]
- 25.Mollica MA, Enewold LR, Lines LM et al. (2017) Examining colorectal cancer survivors’ surveillance patterns and experiences of care: a SEER-CAHPS study. Cancer Causes Control 28(10):1133–1141 [DOI] [PubMed] [Google Scholar]
- 26.Chawla N, Urato M, Ambs A et al. (2015) Unveiling SEER-CAHPS(R): a new data resource for quality of care research. J Gen Intern Med 30(5):641–650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Cancer Institute. Medicare CAHPS Data Documentation. https://healthcardelivery.cancer.gov/seer-cahps/aboutdata/documentation.html Accessed October, 2019.
- 28.Dosch AR, Koru-Sengul T, Miao F, Tannenbaum SL, Byrne MM, Wright JL (2014) Racial and ethnic disparities in the diagnosis of breast cancer: changes in presenting stage in minority populations in Florida during 1981–2009. Breast Cancer Res Treat 148(2):379–387 [DOI] [PubMed] [Google Scholar]
- 29.Balazy KE, Benitez CM, Gutkin PM, Jacobson CE, von Eyben R, Horst KC (2019) Association between primary language, a lack of mammographic screening, and later stage breast cancer presentation. Wiley, New York: [DOI] [PubMed] [Google Scholar]
- 30.Price RA, Haviland AM, Hambarsoomian K et al. (2015) Do experiences with medicare managed care vary according to the proportion of same-Race/Ethnicity/language individuals enrolled in one’s contract? Health Serv Res 50(5):1649–1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palmer NRA, Kent EE, Forsythe LP et al. (2014) Racial and ethnic disparities in patient-provider communication, quality-of-care ratings, and patient activation among long-term cancer survivors. J Clin Oncol 32(36):4087–4094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paddison CAM, Elliott MN, Haviland AM et al. (2012) Experiences of care among medicare beneficiaries with ESRD: medicare consumer assessment of healthcare providers and systems (CAHPS) survey results. Am J Kidney Dis 61(3):440–449 [DOI] [PubMed] [Google Scholar]
- 33.Smith LM, Anderson WL, Kenyon A et al. (2015) Racial and Ethnic disparities in patients’ experience with skilled home health care services. Med Care Res Rev 72(6):756–774 [DOI] [PubMed] [Google Scholar]
- 34.Goldstein E, Elliott MN, Lehrman WG, Hambarsoomian K, Giordano LA (2010) Racial/Ethnic di?erences in patients’ perceptions of inpatient care using the HCAHPS survey. Med Care Res Rev 67(1):74–92 [DOI] [PubMed] [Google Scholar]
- 35.Morales LS, Elliott MN, Weeck-Maldonado R, Spritzer KL, Hays RD (2001) Differences in CAHPS [R] adult survey reports and ratings by Race and Ethnicity: an analysis of the National CAHPS [R] Benchmarking Data 1.0.(National Consumer Assessment of Health Plans) (Statistical Data Included). Health Serv Res 36(3):595. [PMC free article] [PubMed] [Google Scholar]
- 36.National Cancer Patient Experience Programme 2014 Survey (2014) Athena Information Solutions Pvt. Ltd.
- 37.Peterson EB, Ostroff JS, Duhamel KN et al. (2016) Impact of provider-patient communication on cancer screening adherence: a systematic review. Prev Med 93:96–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith B, Madak-Erdogan Z (2018) Urban neighborhood and residential factors associated with breast cancer in African American women: a systematic review. Hormones Cancer 9(2):71–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Campbell RT, Li X, Dolecek TA, Barrett RE, Weaver KE, Warnecke RB (2009) Economic, racial and ethnic disparities in breast cancer in the US: towards a more comprehensive model. Health Place 15(3):870–879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.MacKinnon JA, Duncan RC, Huang Y, Lee DJ, Fleming LE, Voti L, Rudolph M, Wilkinson JD (2007) Detecting an association between socioeconomic status and late stage breast cancer using spatial analysis and area-based measures. Cancer Epidemiol Prev Biomark 16(4):756–762 [DOI] [PubMed] [Google Scholar]
- 41.Gerend MA, Pai M (2008) Social determinants of Black-White disparities in breast cancer mortality: a review. Cancer Epidemiol Prev Biomark 17(11):2913–2923 [DOI] [PubMed] [Google Scholar]
- 42.Izadirad H, Zareban I (2015) The relationship of health literacy with health status, preventive behaviors and health services utilization in Baluchistan. Iran. Hamadan-Univ-Med-Sci 2(3):43–50 [Google Scholar]
- 43.Wang F, McLafferty S, Escamilla V, Luo L (2008) Late-stage breast cancer diagnosis and health care access in Illinois. Prof Geogr 60(1):54–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barry J, Breen N, Barrett M (2012) Significance of increasing poverty levels for determining late-stage breast cancer diagnosis in 1990 and 2000. J Urban Health 89(4):614–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fowler BA (2014) Neighborhood-level influences on delays in diagnostic follow-up from mammography screening in African-American Women: a systematic review. J Women’s Health Care 3(151):1 [Google Scholar]
- 46.Warnecke RB, Campbell RT, Vijayasiri G, Barrett RE, Rauscher GH (2019) Multilevel examination of health disparity: the role of policy implementation in neighborhood context, in patient resources, and in healthcare facilities on later stage of breast cancer diagnosis. Cancer Epidemiol Biomark Prev 28(1):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jha AK, Orav EJ, Zheng J, Epstein AM (2008) Patients’ perception of hospital care in the United States. N Engl J Med 359(18):1921–1931 [DOI] [PubMed] [Google Scholar]