Abstract
Background
Biofilm is known to be tolerant towards antibiotics and difficult to eradicate. Numerous studies have reported minimum biofilm eradication concentration (MBEC) values of antibiotics for many known biofilm pathogens. However, the experimental parameters applied in these studies differ considerably, and often the rationale behind the experimental design are not well described. This makes it difficult to compare the findings. To demonstrate the importance of experimental parameters, we investigated the influence of biofilm growth age, antibiotic concentration and treatment duration, and growth media on biofilm eradication. Additionally, OSTEOmycin™, a clinically used antibiotic containing allograft bone product, was tested for antibiofilm efficacy.
Results
The commonly used Calgary biofilm device was used to grow 24 h and 72 h biofilms of Staphylococcus aureus and Pseudomonas aeruginosa, which were treated with time-dependent vancomycin (up to 3000 mg L− 1) and concentration-dependent tobramycin (up to 80 mg L− 1), respectively. Two common bacteriological growth media, tryptic soy broth (TSB) and cation-adjusted Mueller Hinton broth (CaMHB), were tested. We found for both species that biofilms were more difficult to kill in TSB than in CaMHB. Furthermore, young biofilms (24 h) were easier to eradicate than old biofilms (72 h). In agreement with vancomycin being time-dependent, extension of the vancomycin exposure increased killing of S. aureus biofilms. Tobramycin treatment of 24 h P. aeruginosa biofilms was found concentration-dependent and time-independent, however, increasing killing was indicated for 72 h P. aeruginosa biofilms. Treatment with tobramycin containing OSTEOmycin T™ removed 72 h and 168 h P. aeruginosa biofilms after 1 day treatment, while few 72 h S. aureus biofilms survived after 2 days treatment with vancomycin containing OSTEOmycin V™.
Conclusions
This study demonstrated biofilm removal efficacy was influenced by media, biofilm age and antibiotic concentration and treatment duration. It is therefore necessary to taking these parameters into consideration when designing experiments. The results of OSTEOmycin™ products indicated that simple in vitro biofilm test could be used for initial screening of antibiofilm products. For clinical application, a more clinically relevant biofilm model for the specific biofilm infection in question should be developed to guide the amount of antibiotics used for local antibiofilm treatment.
Background
To improve diagnosis, treatment and prevention of infections, it is necessary to differentiate between acute infections with primarily planktonic microorganisms and biofilm infections with overweight of clusters of microbial cells [1–4]. Most microorganisms in a biofilm grow slowly with down-regulated virulence and are heterogeneously distributed. They are less susceptible to antibiotics compared with their planktonic counterpart and can often not be cleared by the immune system [5–7]. Biofilm related infections can be device-related biofilm infections, such as prosthetic joint infections, or native tissue infections e.g. chronic osteomyelitis and cystic fibrosis. The current most effective treatment of biofilm related infections is to remove the infected medical device and to debride the infected tissue in combination with antibiotic therapy [8]. However, treatment failure is often, and many novel antibiofilm candidates are under research such as quorum sensing inhibitors, biofilm matrix degrading enzymes, and antimicrobial peptides.
An early and correct diagnosis is necessary for proper antibiotic administration. The minimum inhibitory concentration (MIC) is defined as the lowest concentration of the antibiotics preventing visible bacterial growth, while minimum bactericidal concentration (MBC) is the lowest concentration required to kill the bacteria. MICs are used by diagnostic laboratories mainly to confirm resistance. Determination of MIC and MBC is based on planktonic cells, whereas the minimum biofilm eradication concentration (MBEC) is defined as the lowest concentration of antibiotic required to eradicate the biofilm. MBEC has not been implemented in the clinical setting yet, and the published MBEC data are often incomparable because of different experimental conditions. Tables 1–2 illustrate examples of two important biofilm pathogens Staphylococcus aureus and Pseudomonas aeruginosa, and their MIC and MBEC values determined in several studies. As shown in Tables 1– 2, tryptic soy broth (TSB) and cation-adjusted Mueller Hinton broth (CaMHB) media are often used in these studies. TSB is a complex nutrient-rich general-purpose medium, while CaMHB is recommended for MIC testing of non-fastidious organisms according to ISO standard 20776–1: 2006 and is the standard medium in clinical laboratories in the US and European committee on antimicrobial susceptibility testing. High throughput methods for MBEC determination are most frequently used including 96-well microtiter plate combined with crystal violet staining, the Calgary biofilm device (CBD), or its commercial version the MBEC™ Assay (Innovotech, Canada) [23]. As shown in Table 1-2, MIC values were similar for most of the studies. However, MBEC of vancomycin towards S. aureus varies from 1 to more than 8000 mg L− 1. Similarly, the MBEC of tobramycin towards P. aeruginosa varies from 2 to 2560 mg L− 1. This large discrepancy in MBEC values is surprising, especially in light of some studies using the same strain. We hypothesize that the different test parameters and lack of standardization contributed to the large disparity.
Table 1.
MBEC values of vancomycin for S. aureus found in a few studies. Please note ATCC 29213 were tested in several studies with different MBEC values
| S. aureus strains | MIC (mg L− 1) | Challenge medium | Biofilm age (h) | Treatment duration (hours) | Biofilm model | MBEC (mg L− 1) |
|---|---|---|---|---|---|---|
| ATCC 49230 | 2 | TSB | 24 | 24, 72, 120 | 96-well microtiter plate | > 8000, > 8000, 2000 [9] |
| ATCC BAA1556 | 2 | TSB | 24 | 24, 72, 120 | 96-well microtiter plate | > 8000, 8000, 2000 [9] |
| ATCC 6538P, MRSA 16 | 0.5, 1 | Not mentioned | 24 | 24 | Beads | > 2000 [10] |
| ATCC 29213, UOC18 | 1–2 | CaMHB | 24 | 1–72 | CBD | > 1024 [11] |
| ATCC 29213 | 1 | CaMHB | 24 | overnight | CBD | > 1024 [12] |
| ATCC 29213 | 1 | MHB | 48 | 24 | CBD | > 512 [13] |
| ATCC 35556 | 1 | CaMHB | 24 | 24 | CBD | > 256 [14] |
| ATCC 29213, ATCC 33591, VRS5 | 1–2 | CaMHB | 24 | 24 | CBD | > 128 [15] |
| B341002, B346846 | 0.5–1 | CaMHB | 24 | overnight | CBD | 128, 64 [16] |
| Clinical isolates | 0.5–1 | CaMHB | 18 | 24 | 96-well microtiter plate | 8–16 [17] |
| Clinical isolates | 0.5–1 | CaMHB | 18 | 24 | 96-well microtiter plate | 4–32 [18] |
|
40 MRSA isolates |
1 | TSB | 24 | overnight | CBD | 1–64 [19] |
Table 2.
MBEC values of tobramycin for P. aeruginosa in a few studies
| Strains | MIC (mg L−1) | Challenge media | Biofilm inoculation (hours) | Treatment duration (hours) | Biofilm model | MBEC (mg L−1 |
|---|---|---|---|---|---|---|
| ATCC 27853 | 0.25–16 | CaMHB | 24 | 1, 2, 4 | 96-well microtiter plate | 160–2560 [20] |
| ATCC 27853 | 0.25 | TSB | 24 | 24, 72, 120 | 96-well microtiter plate | 2000, ≤250, ≤250 [9] |
| Strain K (PAK) | Not tested | LB | 72 | 18 | 96-well microtiter plate | 200–1600 [21] |
| PAO1 | < 2 | CaMHB | 6 | 16–20 | CBD | 64 [22] |
| ATCC 27853 | 0.5 | CaMHB | 24 | overnight | CBD | 2 [12] |
Biofilm infections such as prosthetic joint infections and chronic osteomyelitis are difficult to treat by oral or parenteral antibiotic therapy alone and debridement is needed for physical removal of biofilms [24, 25]. Management of orthopedic infections often involves use of local antibiotic impregnated cement after debridement to eradicate the potentially remaining planktonic bacteria and residues of biofilms. However, the applied antibiotic dose is often based on personal experiences of the surgeon as no recommendations are available regarding the amount of antibiotics to be used for spacer impregnation [26]. Despite of application of high doses, re-infections occur at 19% of cases [27]. Ideally, MBEC should be determined to guide the amount of antibiotics to be impregnated in the cement.
The purpose of this study was to demonstrate the influences of biofilm age, growth media, and antibiotics exposure time on S. aureus and P. aeruginosa biofilm removal using vancomycin (up to 3000 mg L− 1) and tobramycin (up to 80 mg L− 1), respectively. These two antibiotics were chosen because they are recommended for serious and life-threatening infections caused by Gram-positive bacteria and Gram-negative bacteria. TSB and CaMHB were chosen enabling comparison with studies in Tables 1 and 2. Four biofilm-forming strains were selected for this study. S. aureus strains DSM 110939 [28] was isolated from prosthetic knee infection while S. aureus ATCC 49230 was originally from chronic osteomyelitis. Both infections are known to be associated with biofilms. P. aeruginosa strain PA14 is a well-known biofilm former [29] and P. aeruginosa ATCC 15442 is also known to form biofilms [30, 31]. In addition, we investigated the possibility of using simple in vitro biofilm test such as Calgary biofilm method as initial screening of antibiofilm product by testing OSTEOmycin™, an allograft bone product loaded with either vancomycin or tobramycin [32, 33]. The available release profile of the OSTEOmycin™ products [34] made it possible to estimate concentration.
Results
All four tested strains in this study were found susceptible to the tested antibiotics. The vancomycin MIC for both S. aureus strains was determined to be 1.25 mg L− 1, which is lower than breakpoint (2 mg L− 1) for S. aureus. Likewise, the tobramycin MIC for both P. aeruginosa strains was 0.63 mg L− 1, which is lower than breakpoint (4 mg L− 1) for P. aeruginosa according to Clinical breakpoints – bacteria (v 9.0) in European Committee on Antimicrobial Susceptibility Testing (http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_9.0_Breakpoint_Tables.pdf).
Influence of biofilm age
Biofilm growth is dynamic and mature biofilms are thought to be more antibiotic tolerant. In this study biofilms grew for 24 h or 72 h first and then were subjected to antibiotics challenge for different duration. It was found that the number of colony forming units (CFUs) were higher for 72 h biofilms than for 24 h biofilms by up to 1-log difference (P < 0.01, Figures S1 and S2). Additionally, 72 h biofilms were more difficult to eradicate than 24 h (P < 0.001) as shown in Figs. 1 and 2. It is important to stress that each data point in Figs. 1, 2 and 3 represents results for a minimum of 20 replicates from two independent experiments. Instead of MBEC value which defines complete killing of biofilms, biofilm survival ratio was chosen to present the percentage of replicates survived after treatment. The reason is that biofilm eradication was different among the replicates and a single MBEC value could not provide the information.
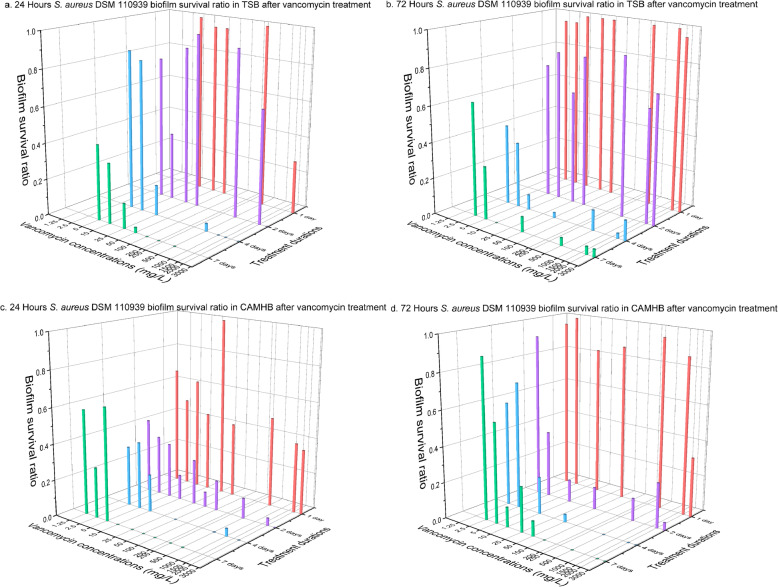
Fig. 1.
S. aureus DSM 110939 biofilm survival ratio after vancomycin treatment. Biofilms of S. aureus DSM 110939 were grown for 24 h or 72 h in TSB or CaMHB medium followed by vancomycin treatment for 1, 2, 4 or 7 days. Each data point contained at least 20 replicates conducted at two occasions
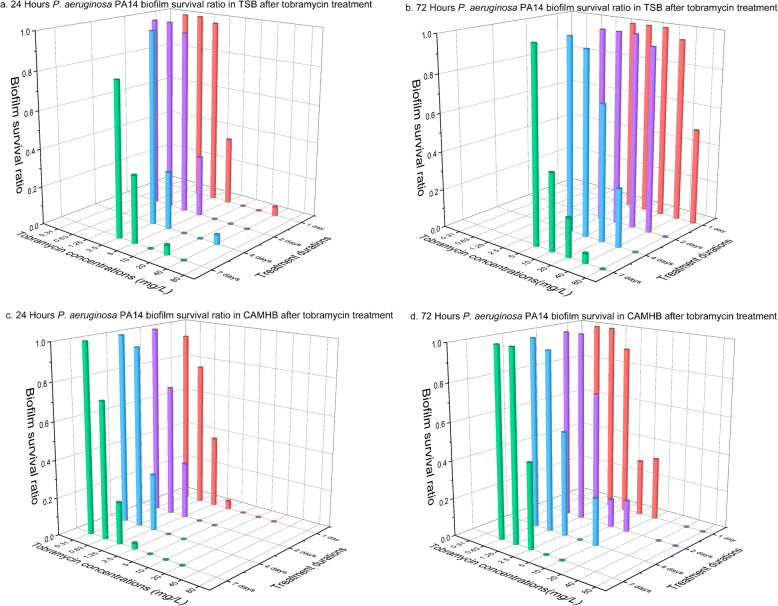
Fig. 2.
P. aeruginosa PA14 biofilm survival ratio after tobramycin treatment. Biofilms of P. aeruginosa PA14 were grown for 24 h or 72 h in TSB or CaMHB medium followed by tobramycin treatment for 1, 2, 4 or 7 days. Each data point contained at least 20 replicates conducted at two occasions
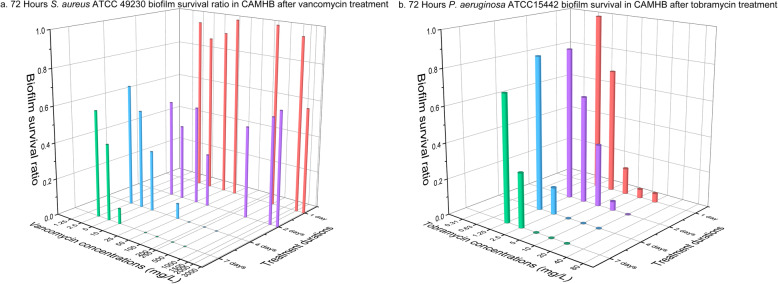
Fig. 3.
Survival ratio of 72 h S. aureus ATCC 49230 biofilms after vancomycin treatment (a) and 72 h P. aeruginosa ATCC 15442 biofilm after tobramycin treatment (b). Each data point contained at least 20 replicates conducted at two occasions
For complete killing of 24 h DSM 110939 biofilms in TSB medium, i.e. MBEC, exposure of the biofilms with a minimum of 1000 mg L− 1 of vancomycin for 4 days or 100 mg L− 1 for 7 days was required (Fig. 1a), whereas some 72 h biofilms still survived even with 3000 mg L− 1 of vancomycin after 7 days (Fig. 1b). In CaMHB medium it required 10 mg L− 1 of vancomycin for 7 days to remove 24 h DSM 110939 biofilms (Fig. 1c) and 10-fold more for 72 h biofilms (Fig. 1d).
In the case of strain PA14, a minimum of 10 mg L− 1 of tobramycin killed almost all 24 h biofilms in TSB media regardless of exposure duration (Fig. 2a) while for 72 h biofilms 80 mg L− 1 of tobramycin for at least 2 days was needed (Fig. 2b). In CaMHB medium, complete killing of 24 h biofilms was achieved with 5 mg L− 1 of tobramycin regardless of exposure duration (Fig. 2c), while it required more than 10 mg L− 1 for 72 h biofilms when the treatment was shorter than 7 days (Fig. 2d).
Media
Biofilm formation depends on many factors including nutrient availability. The main nutrients in both TSB and CaMHB media are amino acids. In addition, TSB contains glucose (2.5 g L− 1) while CaMHB has starch (1.5 g L− 1). The number of CFUs in the biofilms growing in these two media were different (P < 0.05, Figure S1 and S2). On average, slightly more CFUs were found in biofilms growing in CaMHB than TSB, except 72 h PA14 biofilms.
When challenged with antibiotics, biofilms were more difficult to kill in TSB than in CaMHB. For 24 h DSM 110939 biofilms (Fig. 1a and c), seven-day treatment with 100 mg L− 1 and 10 mg L− 1 of vancomycin were required to kill all biofilms in TSB and CaMHB media, respectively. For 72 h DSM 110939 biofilms, none of the vancomycin treated achieved complete killing in TSB medium, while 100 mg L− 1 of vancomycin removed all biofilms after 7 days exposure in CaMHB (Fig. 1b and d). For all four treatment duration, 24 h PA14 biofilms, four-fold more tobramycin was needed in TSB than in CaMHB (10 and 2.5 mg L− 1, respectively) for near complete killing (Fig. 2a and c), while for 72 h biofilms, two-fold more tobramycin was required (80 mg L− 1 in TSB and 40 mg L− 1 in CaMHB) (Fig. 2b and d).
Antibiotics exposure time
Extending vancomycin exposure time from 1 to 4 days reduced survival ratio of DSM 110939 biofilm in TSB (Fig. 1a and b, Table 3) and CaMHB media (Fig. 1c and d, Table 3). Prolonging treatment from 4 to 7 days showed no further killing except 24 h biofilms in TSB (Table 3). Increased killing by prolonging vancomycin exposure was also found for S. aureus ATCC 49230 biofilms (Fig. 3a).
Table 3.
P-values for difference between S. aureus DSM 110939 biofilm survival ratio after vancomycin treatment of different durations. ** indicates P < 0.001
| TSB | CaMHB | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Biofilm age (hours) | Treatment durations (days) | 1 | 2 | 4 | 7 | 1 | 2 | 4 | 7 |
| 24 | 1 | – | ** | ** | ** | – | ** | ** | ** |
| 2 | – | ** | ** | – | 0.110 | 0.251 | |||
| 4 | – | ** | – | 0.790 | |||||
| 7 | – | – | |||||||
| 72 | 1 | – | ** | ** | ** | – | ** | ** | ** |
| 2 | – | ** | ** | – | 0.220 | 0.027 | |||
| 4 | – | 0.578 | – | 0.391 | |||||
| 7 | – | – | |||||||
In contrast to vancomycin, tobramycin is known to exhibit concentration-dependent bactericidal activity [35]. Removal efficacy of 24 h P. aeruginosa PA14 biofilm was not enhanced when duration was extended (Fig. 2a and c, Table 4). However, increasing killing was indicated for 72 h PA14 biofilms (Fig. 2b and d, Table 4) as well as for 72 h P. aeruginosa ATCC 15442 biofilms (Fig. 3b).
Table 4.
P-values for difference between P. aeruginosa PA14 biofilm survival ratio after tobramycin treatment of different durations. * indicates P < 0.01 and ** indicates P < 0.001
| TSB | CaMHB | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Biofilm age (hours) | Treatment durations (days) | 1 | 2 | 4 | 7 | 1 | 2 | 4 | 7 |
| 24 | 1 | – | 0.553 | 0.188 | 0.578 | – | 0.042 | 0.535 | 0.309 |
| 2 | – | 0.220 | 0.518 | – | * | 0.218 | |||
| 4 | – | 0.101 | – | 0.113 | |||||
| 7 | – | – | |||||||
| 72 | 1 | – | * | ** | ** | – | 0.016 | ** | ** |
| 2 | – | ** | ** | – | 0.128 | * | |||
| 4 | – | ** | – | 0.233 | |||||
| 7 | – | – | |||||||
Strains
The two S. aureus strains have the same vancomycin MIC value. Although the necessary concentration of vancomycin for biofilm eradication differed slightly, the same tendency is indicated for both strains that prolonged vancomycin treatment eradicated more biofilms. Similarly, the two P. aeruginosa strains have the same tobramycin MIC value and extended tobramycin treatment lowered MBEC values for 72 h biofilms for both strains.
OSTEOmycin™
Both 72 h and 168 h biofilms were challenged with OSTEOmycin™ for one, two, four, and seven days (in total eight conditions). All PA14 biofilms were cleared after 1 day exposure to OSTEOmycin T™ and remained sterile after 7 days exposure. All S. aureus ATCC 49230 biofilms were eradicated except that three replicates of 72 h biofilms survived 2 days treatment.
Discussion
Biofilm age
Several biofilm models have been developed, each with many experimental parameters that can be adjusted. This flexibility inevitably makes it difficult to compare results obtained with varying conditions chosen in different studies. In the current study we confirmed previous findings that mature biofilm have reduced antibiotics susceptibility compared with young biofilms [36–39]. However, no definition of young and mature biofilm has been universally adopted. In the case of P. aeruginosa, some considered 4 h biofilm as young and 24 h as mature [40], while others considered 24 h as young and 12 days biofilm as mature [38]. Similarly, 6 h S. aureus biofilm was considered as young and 24 h as mature [41], whereas some considered 7 days old biofilm as mature [42]. The inconsistency in the different biofilm studies underlines the need for a form of consensus definition and a simple way to measure maturity. The textbook version of biofilm formation involves bacterial initial attachment to a solid surface, the formation of microcolonies on the surface, and finally differentiation of microcolonies into exopolysaccharide-encased, mature biofilms. However, studies often assume the maturity of the biofilm without looking into the structure of the biofilms or even CFUs of biofilm. In the case of MIC testing, a crucial parameter is inoculum size which is set to be 5 × 105 CFU mL− 1. It is because MIC values can increase concurrently with increasing number of CFUs [43].
The current study treated 24 h biofilms as young and 72 h as mature. The CFU per biofilm shown in Figure S1 and S2 indicated continuous growth in cell number after 24 h for up to 1-log. In batch culture, bacterial growth curve defines the different stages of planktonic culture growth. Similarly, the biofilm formation curves can be established for each strain and growth condition. It was shown previously [12] that using CBD the number of E. coli ATCC 25922 and P. aeruginosa ATCC 27853 continuously increased over 24 h while the growth of S. aureus stagnated after 7 h under the same condition. As the growth phase of the biofilm influences antimicrobial susceptibility, it is therefore important to construct the biofilm growth curve for each strain under the chosen conditions.
Growth media
Biofilm eradication was found different with the two media (Fig. 1 and Fig. 2). Different composition of media is reported to change the activity of antibiotics [44–46]. The Ca2+ and Mg2+ ions in CaMHB media are required for a correct antimicrobial susceptibility testing because those ions reflect the divalent cation concentration in human blood [43, 47–49]. Neither of the two tested media, TSB and CaMHB, resembles in vivo conditions. However, use of CaMHB makes it possible to compare with MIC results, while TSB has been frequently used in other publications (Tables 1 and 2). Other media such as brain-heart infusion broth [50], TSB supplemented with glucose [51], LB [21], and chemically defined media such as basal medium 2 and M9 minimal media [52] have also been used in studies. The choice of media is known to affect biofilm formation [53, 54], but a standardized medium to assess the activity of antibiofilm agents has not been established. It is difficult to standardize because the in vivo environment of biofilm infections varies depending on the location of the infection, hence the optimal medium should be developed for each infection, for example, medium supplemented with mucin for studying cystic fibrosis lung infection [55], or saliva containing medium for studying oral biofilms [56], or human urine for urinary tract infections [57, 58]. Besides nutrient source, in vivo conditions are far more complex with presence of immune systems and varying oxygen level etc., the antibiotics concentration needed for biofilm eradication will most likely be different from in vitro results. For comparison across different studies, a simple and widely available culture medium is suitable, but for estimation of in vivo biofilm killing host factors in form of, for example, serum, plasma, or blood should be included in testing medium.
Antibiotics exposure time
Vancomycin displayed a time-dependent eradication of S. aureus biofilms (Table 2) which has been demonstrated in other studies [42, 59, 60]. Post et al. have shown continuous reduction of viable S. aureus biofilm cells over 28 days [42]. This indicates that further killing could be possible by prolonging the antibiotic exposure time in the current study and complete eradication could be achieved at lower vancomycin concentration.
In contrast to vancomycin, tobramycin exhibits concentration-dependent activity [61–64]. The current study indicated that tobramycin displayed concentration-dependent activity for 24 h PA14 biofilms. However, increased killing of 72 h biofilms were observed with prolonged exposure. Castaneda et al. found increased biofilm antimicrobial susceptibility with increasing antimicrobial exposure time including tobramycin against P. aeruginosa biofilms [9], whereas Walters et al. only found little reduction in P. aeruginosa biofilm cell count with longer tobramycin treatment [65]. Futures studies are needed to investigate the time-dependency of tobramycin antibiofilm effect.
Regardless of the antimicrobials being time-dependent or concentration-dependent on planktonic bacteria, it may be different on biofilm cells because of the presence of biofilm matrix. Exposure time may play an important role in determination of killing effect, because the biofilm matrix may slow down antimicrobial penetration [66]. Therefore, a killing curve is much more informative than a definitive MBEC value determined at a fixed time point.
OSTEOmycin™
Since the antibiotic concentration needed for biofilm eradication is far above the parenterally administrated levels, local delivery of antibiotics may achieve concentrations high enough for biofilm killing. In this study, OSTEOmycin™ showed a strong biofilm eradication efficacy and completely removed biofilm in all tested conditions except three 72 h S. aureus biofilms. OSTEOmycin™ is a product developed based on Winkler et al. 2000 [34]. According to the study, 1 g human cancellous bone impregnated with vancomycin released around 20,000 mg L− 1 vancomycin in 3 mL of 5% human albumin solution after 1 day and decreased to around 100 mg L− 1 after 7 days. Accordingly, it implies that approximately 16,800 mg L− 1 of vancomycin after 1 day and 84 mg L− 1 after 7 days were released with the applied amount in this study. When impregnated with tobramycin, it released more than 10,000 mg L− 1 tobramycin after 1 day and decreased to around 30 mg L− 1 after 7 days [34], suggesting 6600 mg L− 1 of vancomycin after 1 day and 19.8 mg L− 1 were released after 7 days with the applied amount in this study. These concentrations are much higher than the MBEC values found in Figs. 1 and 2, which likely explains the high efficacy. This indicates that prolonged antibiotics treatment may not be necessary when sufficiently high concentration of antibiotics is administered in the beginning of treatment. OSTEOmycin was also shown to be efficient for local treatment of osteomyelitis in the clinic although recurrence may still occur in complex cases within an unknown period of time [33]. The limitation of this study is that OSTEOmycin™ was not tested in a medium resembling the nutrient composition in the bone under in vivo like conditions, and more clinically used or candidate antibiofilm products for osteomyelitis could have been evaluated, such as antibiotics impregnated cement or hydrochlorous acid. Ideally, the in vitro effect of these antibiofilm products could be compared to clinical outcome to validate the assay. Assays developed in such as way could be used to guide the dose of antibiotics for clinical application.
In this study, the used conditions (nutrient rich media, pH, atmospheric oxygen level, shear, biofilm growth in static system, mono species biofilm etc.) were not specific for a distinct biofilm infection and more suitable for initial testing of antibiofilm product. It was by no means meant as a standardization or guideline for clinical application. The purpose was to raise the awareness that biofilm eradication depends on many factors, including the ones mentioned here, but also pH, oxygen level, temperature, shear, and complicated by polymicrobial community interactions and the presence of human factors such as the human immune systems. For specific biofilm infections, we think it is necessary to develop assays with in vivo like environment and validate obtained results by comparing with clinical outcome.
Conclusion
This study showed biofilm removal efficacy was influenced by media, biofilm age and antibiotics treatment duration. It is therefore necessary to take these parameters into consideration when designing experiments. We recommend choosing the conditions most similar to the in vivo situation and explaining the rationale when reporting. This study also showed that in vitro biofilms were possible to be eradicated when treated with long-term high concentrations of antibiotics. This finding needs to be confirmed by in vivo studies.
Methods
Bacterial strains, growth media and antibiotics
S. aureus strains DSM 110939 [28] and ATCC 49230 were tested with vancomycin (Sigma-Aldrich). P. aeruginosa strains PA14 and ATCC 15442 were tested with tobramycin (Sigma-Aldrich). Both tryptic soy broth (TSB) (Sigma-Aldrich) and cation-adjusted Mueller Hinton broth (CaMHB) (Sigma-Aldrich) media were employed in susceptibility testing.
Minimum inhibitory concentration (MIC) determined by the broth microdilution method
The broth microdilution method was used to determine the MIC of each strain according to the procedures described in Wiegand et al. [43]. Briefly, each strain was inoculated on TSB agar plate for 24 h. Then five well-isolated colonies were selected and inoculated in a 50 mL tube with 20 mL CaMHB until the OD600 value of the culture reached around 0.6. The culture was diluted to approximately 1 × 106 colony-forming unit (CFU) mL− 1. Then, 100 μl of the diluted culture was added into each well of a 96-well-plate containing 100 μl of antibiotics at concentrations from 0.31 to 80 mg L− 1 of tobramycin or from 1.25 to 3000 mg L− 1 of vancomycin). The plate was covered and inoculated at 37 °C with shaking at 150 rpm for 24 h. After that, OD595 of each well was measured by Infinite F200 Pro (Tecan Group Ltd., Switzerland) to determine MIC.
Biofilm antibiotics susceptibility testing by Calgary biofilm device (CBD)
CBD [67] was used to grow biofilms. An illustration of the experimental procedure is given in Figure S3. Briefly, biofilms were formed by immersing the pegs of a microtiter lid (Nunc™ 445497) into the biofilm growth microtiter plate, 150 μl of the diluted culture containing 104 CFU was added into the wells of 96 well microtiter plate (Thermo Fisher Scientific) and then covered with peg lid The biofilms were allowed to grow in TSB or CaMHB media at 37 °C with shaking at 150 rpm for 24 h or 72 h. After incubation, the lid with biofilms was transferred to a rinse plate containing 200 μl saline in each well and incubated for 1 min. The rinsed lid was then transferred to a challenge plate containing 200 μl antibiotics solution in each well. The antibiotics were prepared in the media used for growing biofilms. The plates were challenged for 24, 48, 96 or 168 h at 37 °C with shaking at 150 rpm. After challenged in the antibiotics solution, the lid containing biofilms was rinsed twice with fresh saline each time and then transferred to a recovery plate containing 200 μl sterile media followed by sonication at 40KHz for 5 min.
After removal of the lid, the recovery plate was inoculated for another 24 h at 37 °C with shaking at 150 rpm and OD595 measured by Infinite F200 Pro to determine the biofilm removal efficacy. All tests were repeated at least on two occasions with minimum 10 replicates each time. Percentage of the surviving replicates was calculated and presented as biofilm survival ratio.
Biofilm eradication by OSTEOmycin™
OSTEOmycin™ samples were obtained from European Cell and Tissue Bank. Two clinical strains S. aureus ATCC 49230 and P. aeruginosa PA14 were chosen for this test. Seventy-two hours (3-days) or 168 h (7-days) biofilms were challenged with OSTEOmycin™ for 1, 2, 4 or 7 days following the method described above. S. aureus ATCC 49230 biofilms were challenged with 280 g L− 1 OSTEOmycin V™ in CaMHB, while P. aeruginosa PA14 biofilms were subjected to 220 g L− 1 OSTEOmycin T™.
Statistics analysis
ANOVA was used to calculate the difference between biofilm formation on CBD pegs. Binary logistic regression model was used to compare biofilm removal efficacy under different conditions.
Supplementary information
Additional file 1: Figure S1. S. aureus biofilm formation on CBD. After 24 or 72 h of growth, biofilms were removed from the pegs, transferred into the recovery plate and harvested by sonication. Six random wells of each row were selected for CFU count, in total 48 wells per plate. The number of CFUs per peg were different under different conditions. Generally 3 days incubation resulted in more CFUs per peg. Figure S2. P. aeruginosa PA14 biofilm formation on CBD. After 24 or 72 h of growth, biofilms were removed from the pegs, transferred into the recovery plate and harvested by sonication. Six random wells of each row were selected for CFU count, in total 48 wells per plate. The number of CFUs per peg were different under different conditions. Generally 3 days incubation resulted in more CFUs per peg. Figure S3. Flow diagram of the MBEC assay.
Acknowledgements
We thank technician Susanne Bielidt for her assistance in the laboratory.
Abbreviations
- CaMHB
Cation-adjusted Mueller Hinton broth
- CBD
Calgary biofilm device
- CFU
Colony forming units
- MBEC
Minimum biofilm eradication concentration
- MBC
Minimum bactericidal concentration
- MIC
Minimum inhibitory concentration
- TSB
Tryptic soy broth
Authors’ contributions
TRT, HW and YX designed the study, XC performed the experimental work. XC, TRT, and YX performed data analysis, XC, TRT and YX drafted the manuscript. All authors were involved in revising the manuscript. The author(s) read and approved the final manuscript.
Funding
This study was supported by Det Obelske Familiefond (grant no 27751). The foundation was not involved in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12866-020-01947-9.
References
- 1.Burmølle M, Thomsen TR, Fazli M, Dige I, Christensen L, Homøe P, Tvede M, Nyvad B, Tolker-Nielsen T, Givskov M, Moser C, Kirketerp-Møller K, Johansen HK, Høiby N, Jensen PØ, Sørensen SJ, Bjarnsholt T. Biofilms in chronic infections – a matter of opportunity – monospecies biofilms in multispecies infections. FEMS Immunol Med Microbiol. 2010;59:324–336. doi: 10.1111/j.1574-695X.2010.00714.x. [DOI] [PubMed] [Google Scholar]
- 2.Flemming H-C, Wingender J. The biofilm matrix. Nat Rev Microbiol. 2010;8:623–633. doi: 10.1038/nrmicro2415. [DOI] [PubMed] [Google Scholar]
- 3.Watnick P, Kolter R. Biofilm, City of microbes. J Bacteriol. 2000;182:2675–2679. doi: 10.1128/jb.182.10.2675-2679.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Costerton JW. Introduction to biofilm. Int J Antimicrob Agents. 1999;11:217–221. doi: 10.1016/s0924-8579(99)00018-7. [DOI] [PubMed] [Google Scholar]
- 5.Fux CA, Stoodley P, Hall-Stoodley L, Costerton JW. Bacterial biofilms: a diagnostic and therapeutic challenge. Expert Rev Anti-Infect Ther. 2003;1:667–683. doi: 10.1586/14787210.1.4.667. [DOI] [PubMed] [Google Scholar]
- 6.Alhede M, Bjarnsholt T, Jensen PØ, Phipps RK, Moser C, Christophersen L, Christensen LD, van Gennip M, Parsek M, Høiby N, Rasmussen TB, Givskov M. Pseudomonas aeruginosa recognizes and responds aggressively to the presence of polymorphonuclear leukocytes. Microbiology. 2009;155:3500–3508. doi: 10.1099/mic.0.031443-0. [DOI] [PubMed] [Google Scholar]
- 7.Bjarnsholt T, Jensen PØ, Burmølle M, Hentzer M, Haagensen JAJ, Hougen HP, Calum H, Madsen KG, Moser C, Molin S, Høiby N, Givskov M. Pseudomonas aeruginosa tolerance to tobramycin, hydrogen peroxide and polymorphonuclear leukocytes is quorum-sensing dependent. Microbiology. 2005;151:373–383. doi: 10.1099/mic.0.27463-0. [DOI] [PubMed] [Google Scholar]
- 8.Wilkins M, Hall-Stoodley L, Allan RN, Faust SN. New approaches to the treatment of biofilm-related infections. J Infect. 2014;69:S47–S52. doi: 10.1016/j.jinf.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 9.Castaneda P, McLaren A, Tavaziva G, Overstreet D. Biofilm antimicrobial susceptibility increases with antimicrobial exposure time. Clin Orthop Relat Res. 2016;474(7):1659–64. [DOI] [PMC free article] [PubMed]
- 10.Meije Y, Almirante B, Del Pozo JL, Martín MT, Fernández-Hidalgo N, Shan A, Basas J, Pahissa A, Gavaldà J. Daptomycin is effective as antibiotic-lock therapy in a model of Staphylococcus aureus catheter-related infection. J Inf Secur. 2014;68:548–552. doi: 10.1016/j.jinf.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 11.Kostenko V, Ceri H, Martinuzzi RJ. Increased tolerance of Staphylococcus aureus to vancomycin in viscous media. FEMS Immunol Med Microbiol. 2007;51:277–288. doi: 10.1111/j.1574-695X.2007.00300.x. [DOI] [PubMed] [Google Scholar]
- 12.Ceri H, Olson ME, Stremick C, Read RR, Morck D, Buret A. The Calgary biofilm device: new technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J Clin Microbiol. 1999;37:1771–1776. doi: 10.1128/jcm.37.6.1771-1776.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coraça-Hubér DC, Fille M, Hausdorfer J, Pfaller K, Nogler M. Evaluation of MBEC™-HTP biofilm model for studies of implant associated infections. J Orthop Res. 2012;30:1176–1180. doi: 10.1002/jor.22065. [DOI] [PubMed] [Google Scholar]
- 14.LaPlante KL, Mermel LA. In vitro activities of Telavancin and Vancomycin against biofilm-producing Staphylococcus aureus, S. epidermidis, and enterococcus faecalis strains. Antimicrob Agents Chemother. 2009;53:3166–3169. doi: 10.1128/AAC.01642-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Belley A, Neesham-Grenon E, McKay G, Arhin FF, Harris R, Beveridge T, Parr TR, Moeck G. Oritavancin kills stationary-phase and biofilm Staphylococcus aureus cells in vitro. Antimicrob Agents Chemother. 2009;53:918–925. doi: 10.1128/AAC.00766-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.LaPlante KL, Woodmansee S. Activities of Daptomycin and Vancomycin alone and in combination with rifampin and gentamicin against biofilm-forming methicillin-resistant Staphylococcus aureus isolates in an experimental model of endocarditis. Antimicrob Agents Chemother. 2009;53:3880–3886. doi: 10.1128/AAC.00134-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Antunes ALS, Trentin DS, Bonfanti JW, Pinto CCF, Perez LRR, Macedo AJ, Barth AL. Application of a feasible method for determination of biofilm antimicrobial susceptibility in staphylococci. APMIS. 2010;118:873–877. doi: 10.1111/j.1600-0463.2010.02681.x. [DOI] [PubMed] [Google Scholar]
- 18.Antunes ALS, Bonfanti JW, Perez LRR, Pinto CCF, de Freitas ALP, Macedo AJ, Barth AL. High vancomycin resistance among biofilms produced by Staphylococcus species isolated from central venous catheters. Mem Inst Oswaldo Cruz. 2011;106:51–55. doi: 10.1590/s0074-02762011000100008. [DOI] [PubMed] [Google Scholar]
- 19.Rose WE, Poppens PT. Impact of biofilm on the in vitro activity of vancomycin alone and in combination with tigecycline and rifampicin against Staphylococcus aureus. J Antimicrob Chemother. 2009;63:485–488. doi: 10.1093/jac/dkn513. [DOI] [PubMed] [Google Scholar]
- 20.Dosler S, Karaaslan E. Inhibition and destruction of Pseudomonas aeruginosa biofilms by antibiotics and antimicrobial peptides. Peptides. 2014;62:32–37. doi: 10.1016/j.peptides.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 21.Reighard KP, Schoenfisch MH. Antibacterial action of nitric oxide-releasing chitosan oligosaccharides against Pseudomonas aeruginosa under aerobic and anaerobic conditions. Antimicrob Agents Chemother. 2015;59:6506–6513. doi: 10.1128/AAC.01208-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Kievit TR, Parkins MD, Gillis RJ, Srikumar R, Ceri H, Poole K, Iglewski BH, Storey DG. Multidrug efflux pumps: expression patterns and contribution to antibiotic resistance in Pseudomonas aeruginosa biofilms. Antimicrob Agents Chemother. 2001;45:1761–1770. doi: 10.1128/AAC.45.6.1761-1770.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Macia MD, Rojo-Molinero E, Oliver A. Antimicrobial susceptibility testing in biofilm-growing bacteria. Clin Microbiol Infect. 2014;20:981–990. doi: 10.1111/1469-0691.12651. [DOI] [PubMed] [Google Scholar]
- 24.Escudero-Sanchez R, Senneville E, Digumber M, Soriano A, Del Toro MD, Bahamonde A, Del Pozo JL, Guio L, Murillo O, Rico A, García-País MJ, Rodríguez-Pardo D, Iribarren JA, Fernández M, Benito N, Fresco G, Muriel A, Ariza J, Cobo J. Suppressive antibiotic therapy in prosthetic joint infections: a multicentre cohort study. Clin Microbiol Infect. 2020;26:499–505. doi: 10.1016/j.cmi.2019.09.007. [DOI] [PubMed] [Google Scholar]
- 25.Rao N, Ziran BH, Lipsky BA. Treating osteomyelitis: antibiotics and surgery. Plast Reconstr Surg. 2011;127:177S. doi: 10.1097/PRS.0b013e3182001f0f. [DOI] [PubMed] [Google Scholar]
- 26.Anagnostakos K. Therapeutic use of antibiotic-loaded bone cement in the treatment of hip and knee joint infections. J Bone Jt Infect. 2017;2:29–37. doi: 10.7150/jbji.16067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cochran AR, Ong KL, Lau E, Mont MA, Malkani AL. Risk of reinfection after treatment of infected Total knee Arthroplasty. J Arthroplast. 2016;31:156–161. doi: 10.1016/j.arth.2016.03.028. [DOI] [PubMed] [Google Scholar]
- 28.Xu Y, Maltesen RG, Larsen LH, Schønheyder HC, Le VQ, Nielsen JL, Nielsen PH, Thomsen TR, Nielsen KL. In vivo gene expression in a Staphylococcus aureus prosthetic joint infection characterized by RNA sequencing and metabolomics: a pilot study. BMC Microbiol. 2016;16:80. doi: 10.1186/s12866-016-0695-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedman L, Kolter R. Genes involved in matrix formation in Pseudomonas aeruginosa PA14 biofilms. Mol Microbiol. 2004;51:675–690. doi: 10.1046/j.1365-2958.2003.03877.x. [DOI] [PubMed] [Google Scholar]
- 30.Diaz De Rienzo MA, Stevenson PS, Marchant R, Banat IM. Effect of biosurfactants on Pseudomonas aeruginosa and Staphylococcus aureus biofilms in a BioFlux channel. Appl Microbiol Biotechnol. 2016;100:5773–5779. doi: 10.1007/s00253-016-7310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rienzo MADD, Stevenson PS, Marchant R, Banat IM. Pseudomonas aeruginosa biofilm disruption using microbial surfactants. J Appl Microbiol. 2016;120:868–876. doi: 10.1111/jam.13049. [DOI] [PubMed] [Google Scholar]
- 32.Winkler H. Treatment of chronic orthopaedic infection. EFORT Open Rev. 2017;2:110–116. doi: 10.1302/2058-5241.2.160063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Winkler H, Haiden P. Treatment of chronic bone infection. Oper Tech Orthop. 2016;26:2–11. [Google Scholar]
- 34.Winkler H, Janata O, Berger C, Wein W, Georgopoulos A. In vitro release of vancomycin and tobramycin from impregnated human and bovine bone grafts. J Antimicrob Chemother. 2000;46:423–428. doi: 10.1093/jac/46.3.423. [DOI] [PubMed] [Google Scholar]
- 35.Beringer PM, Vinks AA, Jelliffe RW, Shapiro BJ. Pharmacokinetics of tobramycin in adults with cystic fibrosis: implications for once-daily administration. Antimicrob Agents Chemother. 2000;44:809–813. doi: 10.1128/aac.44.4.809-813.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tré-Hardy M, Macé C, Manssouri NE, Vanderbist F, Traore H, Devleeschouwer MJ. Effect of antibiotic co-administration on young and mature biofilms of cystic fibrosis clinical isolates: the importance of the biofilm model. Int J Antimicrob Agents. 2009;33:40–45. doi: 10.1016/j.ijantimicag.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 37.Hengzhuang W, Wu H, Ciofu O, Song Z, Høiby N. Pharmacokinetics/pharmacodynamics of Colistin and Imipenem on Mucoid and Nonmucoid Pseudomonas aeruginosa biofilms. Antimicrob Agents Chemother. 2011;55:4469–4474. doi: 10.1128/AAC.00126-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nagant C, Tré-Hardy M, El-Ouaaliti M, Savage P, Devleeschouwer MJ, Dehaye J-P. Interaction between tobramycin and CSA-13 on clinical isolates of Pseudomonas aeruginosa in a model of young and mature biofilms. Appl Microbiol Biotechnol. 2010;88:251–263. doi: 10.1007/s00253-010-2748-3. [DOI] [PubMed] [Google Scholar]
- 39.Ito A, Taniuchi A, May T, Kawata K, Okabe S. Increased antibiotic resistance of Escherichia coli in mature biofilms. Appl Environ Microbiol. 2009;75:4093–4100. doi: 10.1128/AEM.02949-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bowler LL, Zhanel GG, Ball TB, Saward LL. Mature Pseudomonas aeruginosa biofilms prevail compared to young biofilms in the presence of Ceftazidime. Antimicrob Agents Chemother. 2012;56:4976–4979. doi: 10.1128/AAC.00650-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu S, Yang T, Luo Y, Li X, Zhang X, Tang J, Ma X, Wang Z. Efficacy of the novel oxazolidinone compound FYL-67 for preventing biofilm formation by Staphylococcus aureus. J Antimicrob Chemother. 2014;69:3011–3019. doi: 10.1093/jac/dku240. [DOI] [PubMed] [Google Scholar]
- 42.Post V, Wahl P, Richards RG, Moriarty TF. Vancomycin displays time-dependent eradication of mature Staphylococcus aureus biofilms. J Orthop Res. 2017;35:381–388. doi: 10.1002/jor.23291. [DOI] [PubMed] [Google Scholar]
- 43.Wiegand I, Hilpert K, Hancock REW. Agar and broth dilution methods to determine the minimal inhibitory concentration (MIC) of antimicrobial substances. Nat Protoc. 2008;3:163–175. doi: 10.1038/nprot.2007.521. [DOI] [PubMed] [Google Scholar]
- 44.Digranes A, Dibb WL, Benonisen E, Ostervold B. The in vitro activity of gentamicin, tobramycin and netilmicin against 500 clinical isolates of bacteria. A comparative study using three different test media. Acta Pathol Microbiol Immunol Scand B. 1983;91:135–139. doi: 10.1111/j.1699-0463.1983.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 45.Cruz RC, Werneck SMC, Oliveira CS, Santos PC, Soares BM, Santos DA, Cisalpino PS. Influence of different media, incubation times, and temperatures for determining the MICs of seven antifungal agents against Paracoccidioides brasiliensis by microdilution. J Clin Microbiol. 2013;51:436–443. doi: 10.1128/JCM.02231-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barry AL, Miller GH, Thornsberry C, Hare RS, Jones RN, Lorber RR, Ferraresi R, Cramer C. Influence of cation supplements on activity of netilmicin against Pseudomonas aeruginosa in vitro and in vivo. Antimicrob Agents Chemother. 1987;31:1514–1518. doi: 10.1128/aac.31.10.1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nanavaty J, Mortensen JE, Shryock TR. The effects of environmental conditions on the in vitro activity of selected antimicrobial agents against <emphasis type=“italic”>Escherichia coli</emphasis>. Curr Microbiol. 1998;36:212–215. doi: 10.1007/s002849900296. [DOI] [PubMed] [Google Scholar]
- 48.D’amato RF, Thornsberry C, Baker CN, Kirven LA. Effect of calcium and magnesium ions on the susceptibility of Pseudomonas species to tetracycline, gentamicin polymyxin B, and carbenicillin. Antimicrob Agents Chemother. 1975;7:596–600. doi: 10.1128/aac.7.5.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rhomberg PR, Sader HS, Jones RN. Reproducibility of daptomycin MIC results using dry-form commercial trays with appropriate supplemental calcium content. Int J Antimicrob Agents. 2005;25:274–276. doi: 10.1016/j.ijantimicag.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 50.Singh AK, Prakash P, Achra A, Singh GP, Das A, Singh RK. Standardization and classification of in vitro biofilm formation by clinical isolates of Staphylococcus aureus. J Glob Infect Dis. 2017;9:93–101. doi: 10.4103/jgid.jgid_91_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lade H, Park JH, Chung SH, Kim IH, Kim J-M, Joo H-S, Kim J-S. Biofilm formation by Staphylococcus aureus clinical isolates is differentially affected by glucose and sodium chloride supplemented culture media. J Clin Med. 2019;8:1853. doi: 10.3390/jcm8111853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haney EF, Trimble MJ, Cheng JT, Vallé Q, Hancock REW. Critical assessment of methods to quantify biofilm growth and evaluate Antibiofilm activity of host Defence peptides. Biomolecules. 2018;8:29. doi: 10.3390/biom8020029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hancock V, Witsø IL, Klemm P. Biofilm formation as a function of adhesin, growth medium, substratum and strain type. Int J Med Microbiol. 2011;301:570–576. doi: 10.1016/j.ijmm.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 54.Wijesinghe G, Dilhari A, Gayani B, Kottegoda N, Samaranayake L, Weerasekera M. Influence of laboratory culture media on in vitro growth, adhesion, and biofilm formation of Pseudomonas aeruginosa and Staphylococcus aureus. Med Princ Pract. 2019;28:28–35. doi: 10.1159/000494757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Haley CL, Colmer-Hamood JA, Hamood AN. Characterization of biofilm-like structures formed by Pseudomonas aeruginosa in a synthetic mucus medium. BMC Microbiol. 2012;12:181. doi: 10.1186/1471-2180-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahn S-J, Ahn S-J, Wen ZT, Brady LJ, Burne RA. Characteristics of biofilm formation by Streptococcus mutans in the presence of saliva. Infect Immun. 2008;76:4259–4268. doi: 10.1128/IAI.00422-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sm J, Me S. Proteus mirabilis biofilms and catheter-associated urinary tract infections. Virulence. 2011;2:460–465. doi: 10.4161/viru.2.5.17783. [DOI] [PubMed] [Google Scholar]
- 58.Hancock V, Ferrières L, Klemm P. Biofilm formation by asymptomatic and virulent urinary tract infectious Escherichia coli strains. FEMS Microbiol Lett. 2007;267:30–37. doi: 10.1111/j.1574-6968.2006.00507.x. [DOI] [PubMed] [Google Scholar]
- 59.Rybak MJ. The pharmacokinetic and pharmacodynamic properties of vancomycin. Clin Infect Dis. 2006;42(Suppl 1):S35–S39. doi: 10.1086/491712. [DOI] [PubMed] [Google Scholar]
- 60.Vandecasteele SJ, De Vriese AS, Tacconelli E. The pharmacokinetics and pharmacodynamics of vancomycin in clinical practice: evidence and uncertainties. J Antimicrob Chemother. 2013;68:743–748. doi: 10.1093/jac/dks495. [DOI] [PubMed] [Google Scholar]
- 61.Kapusnik JE, Hackbarth CJ, Chambers HF, Carpenter T, Sande MA. Single, large, daily dosing versus intermittent dosing of tobramycin for treating experimental pseudomonas pneumonia. J Infect Dis. 1988;158:7–12. doi: 10.1093/infdis/158.1.7. [DOI] [PubMed] [Google Scholar]
- 62.Craig WA, Ebert SC. Killing and regrowth of bacteria in vitro: a review. Scand J Infect Dis Suppl. 1990;74:63–70. [PubMed] [Google Scholar]
- 63.Vogelman B, Gudmundsson S, Leggett J, Turnidge J, Ebert S, Craig WA. Correlation of antimicrobial pharmacokinetic parameters with therapeutic efficacy in an animal model. J Infect Dis. 1988;158:831–847. doi: 10.1093/infdis/158.4.831. [DOI] [PubMed] [Google Scholar]
- 64.Leggett JE, Fantin B, Ebert S, Totsuka K, Vogelman B, Calame W, Mattie H, Craig WA. Comparative antibiotic dose-effect relations at several dosing intervals in murine pneumonitis and thigh-infection models. J Infect Dis. 1989;159:281–292. doi: 10.1093/infdis/159.2.281. [DOI] [PubMed] [Google Scholar]
- 65.Walters MC, Roe F, Bugnicourt A, Franklin MJ, Stewart PS. Contributions of antibiotic penetration, oxygen limitation, and low metabolic activity to tolerance of Pseudomonas aeruginosa biofilms to ciprofloxacin and tobramycin. Antimicrob Agents Chemother. 2003;47:317–323. doi: 10.1128/AAC.47.1.317-323.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stewart PS. Antimicrobial tolerance in biofilms. Microbiol. Spectr. 2015;3:269–85. [DOI] [PMC free article] [PubMed]
- 67.Harrison JJ, Stremick CA, Turner RJ, Allan ND, Olson ME, Ceri H. Microtiter susceptibility testing of microbes growing on peg lids: a miniaturized biofilm model for high-throughput screening. Nat Protocols. 2010;5:1236–1254. doi: 10.1038/nprot.2010.71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. S. aureus biofilm formation on CBD. After 24 or 72 h of growth, biofilms were removed from the pegs, transferred into the recovery plate and harvested by sonication. Six random wells of each row were selected for CFU count, in total 48 wells per plate. The number of CFUs per peg were different under different conditions. Generally 3 days incubation resulted in more CFUs per peg. Figure S2. P. aeruginosa PA14 biofilm formation on CBD. After 24 or 72 h of growth, biofilms were removed from the pegs, transferred into the recovery plate and harvested by sonication. Six random wells of each row were selected for CFU count, in total 48 wells per plate. The number of CFUs per peg were different under different conditions. Generally 3 days incubation resulted in more CFUs per peg. Figure S3. Flow diagram of the MBEC assay.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.