Abstract
Penetrative cardiac injury can often result in life-threatening sequelae such as myocardial contusion or rupture, coronary vessel and valvular damage, pericardial effusion with tamponade, and arrhythmias of which gunshot injury is a chief culprit. We report a case of a suspected acute coronary syndrome after a cardiac gunshot injury that was conservatively managed.
Keywords: gunshot injury, cardiac, heart
Introduction
Cardiac gunshot injuries (CGSIs) are relatively rare and occur during interpersonal conflict or as a result of an inadvertently discharged firearm with exceedingly high mortality, hovering just over 80%.1,2
Most of the current literature on CGSIs has been acquired during world wars, and regional conflicts.3 Multimodal imaging with echocardiography and computed tomography are integral in determining the extent of cardiac injury in surviving patients, foreign body location, and potential ballistics information.4 Surgical intervention is typically the cornerstone of management in the hemodynamically unstable patient.5
We report a case of a suspected acute coronary syndrome (ACS) after a CGSI that was conservatively managed.
Case Report
A 60-year-old Caribbean Black male with no significant medical history was involved in an altercation after being confronted for an adulterous lover’s tryst. He was subsequently assaulted and fired upon with a reported “sawed-off shotgun” at approximately 20 feet in a full-frontal position, after which he collapsed. Emergency ambulance services were immediately contacted.
On presentation to the trauma bay, the patient was somnolent but reporting vague chest discomfort. His vital signs indicated systolic blood pressures of 105 mm Hg, heart rate of 90 beats per minute, and respiratory rate of 22 breaths per minute with an oxygen saturation of 95% on room air. His physical examination revealed several shrapnel-associated lacerations on his anterior chest wall as well as a likely left-sided hemothorax. The trauma and cardiothoracic surgery teams were immediately consulted for which they initiated routine resuscitative measures and inserted a chest tube.
A 12-lead electrocardiogram (ECG) indicated sinus rhythm with subtle 1-mm ST-segment elevation in the lead III and no evidence of advanced heart block (see Figure 1). Portable chest radiography affirmed the left hemothorax with numerous scattered shrapnel fragments (see Figure 2). Other pertinent diagnostic laboratory investigations included an admission troponin I 3.43 ng/mL (normal 0.0-0.15 ng/dL). Routine investigations revealed a hemoglobin of 8.4 g/dL (normal 12-15 g/dL) with a normal white blood cells count and serum creatinine of 1.3 mg/dL (normal 0.6-1.2 mg/dL). Bedside 2-dimensional transthoracic echocardiography demonstrated a preserved left ventricular fraction without regional wall motion abnormalities, pericardial effusion, or overt valvular injury. However, it appeared that there was significant artifact shadowing on several imaging acoustic windows (see Supplement Figure 1).
Figure 1.
Twelve-lead electrocardiogram displaying the subtle 1-mm ST-segment elevation in lead III (red box).
Figure 2.

Portable chest radiograph indicating the extent of radiopaque shrapnel throughout the thorax with left-sided hemothorax and a chest drain.
After the patient was hemodynamically stabilized and admitted to the surgical unit, the cardiovascular team was consulted due to the markedly elevated serum troponin levels (troponin I 11.21 ng/mL; normal 0.0-0.15 ng/dL) and the abnormal electrocardiographic changes that persisted the following day. A chest computed tomography scan was performed and alluded to the presence of intramyocardial shrapnel (see Figure 3). The tentative diagnosis at this juncture was myocardial contusion with a type 2 myocardial infarction or suspected ACS. After measured consideration, the patient was not initiated on any antithrombotic or neurohormonal therapies that would be standard-of-care practice for an ACS. In the setting of the abnormally elevated cardiac biomarkers, diagnostic coronary angiography was performed, which indicated mild luminal irregularities with several myocardial-wedged shrapnel fragments oscillating with each cardiac cycle. There were also 2 foreign bodies in very close proximity to the right coronary artery ostium (see Supplement Figure 2).
Figure 3.
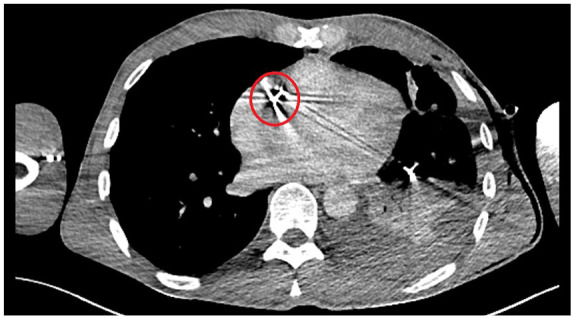
Cross-sectional computed tomography scan indicating a relatively large shrapnel fragment in the right ventricle.
The patient was stable for the remainder of his hospital course with down-trending troponin levels, and subsequent normalization of his ECG. He declined foreign body removal via surgical repair after a detailed benefit-risk analysis discussion. He was eventually discharged with a defaulted follow-up appointment.
Discussion
As aforementioned, most of the information on CGSIs has been accrued from major military and civilian warfare, with eventual fatality being the most likely outcome.6,7 In fact, it is estimated that approximately 90% of afflicted victims do not survive to initial medical care due to almost immediate exsanguination.8 The most frequently injured structure is the right ventricle due to its anterior anatomical location within the mediastinum.9,10 Projectile injuries to the heart can be classified as (1) myocardial contusion, (2) chamber laceration or perforation, (3) valve, leaflets, or subvalvular structure injury, (4) septal injury, and (5) coronary vessel injury.11 There is also the possibility of a foreign body or shrapnel embolization, for example, bullet fragments being translocated to the right ventricle.12,13 The main pathophysiological mechanisms associated with cardiac trauma are (1) hemorrhage, (2) tamponade, and (3) heart failure. A hemorrhaging patient is the most frequent presentation, and they usually exsanguinate to death by a penetrating or perforating wound. Impaired cardiac function is rare and usually associated with heart valve dysfunction, arrhythmias, or a compromised coronary artery. Cardiac tamponade is also relatively common in surviving patients. In some cases, tamponade can be a double-edged sword as it prolongs survival by preventing further exsanguination and allowing definitive therapy but is also associated with high mortality. Clinical presentation of CGSI is contingent on a multitude of factors such as type of object, wound size, compromised structures, presence of tamponade as well as other coexistent injuries.14 Several complications can ensue such as laceration of the coronary artery that we postulated as an etiology in our case; hemopericardium, coronary arteriovenous fistula, cardiac perforation, and embolization.15-17
Our patient likely incurred a myocardial contusion from embedded shrapnel; however, this was difficult to ascertain in the setting of chest pain, ECG ST-T changes, and disproportionately elevated serum troponins. There is no gold standard to clinch this diagnosis; however, the diagnostic time frame is limited and occurs earlier than ACS. Jackson et al suggested serum troponin levels should be measured at admission and at 4 to 6 hours, which was done for our patient in addition to further surveillance intervals, which steadily trended upward.18 ECG is also critical in evaluating CGSI. In the case of myocardial contusion, up to 80% of patients will display abnormalities such as ST-T changes, ventricular fibrillation, atrial fibrillation, and bundle branch blocks.19 Our patient had borderline, ST-segment elevation in lead III, which persisted with ongoing chest pain amid steadily increasing serum troponin levels, hence the rationale for subsequent cardiac catheterization. Both transthoracic and transesophageal echocardiography are complementary as the former can image the adjacent thoracic aorta, while the latter can image the right ventricular outflow tract. They are also useful for detecting aneurysm or fistula formation. Both imaging modalities are usually indicated in CGSI patients with abnormal biomarkers and ECGs, hemodynamic instability with shock or arrhythmias.20 Computed tomography imaging can provide in-depth visualization of other structural injuries such as great vessel lacerations and possible fistulous connections. It can also provide crucial anatomical information for potential operative intervention. Cardiac catheterization is usually required when there is a regional wall motion abnormality, reduced ejection fraction, or valvular injury requiring immediate surgery. As aforementioned, in our patient, it was prompted by a considered risk-benefit analysis for suspected ACS. There was a concern about potential coronary vessel injury based on the investigations. There are a few case reports that describe occluded coronary arteries by bullet fragments or shrapnel, which was our shared concern. Although our patient did not have an occluded vessel, fragments were in very close proximity to the vessel course, especially as its ostium.
The management of CSGI is predicated on the etiology of the insult. Some pericardial injuries with resultant effusion and tamponade may be treated with pericardiocentesis; however, if the patient is hemodynamically unstable, immediate thoracotomy and surgical repair may be required in the setting of valvular injury, coronary artery, and myocardial perforation or rupture. Standard surgical techniques with mattress sutures, skin staplers, and sealants can be used to achieve hemostatic control.21 In the future, endovascular techniques may be considered to repair lacerated vessels. Foreign bodies can be extricated either surgically via open repair percutaneously based on its dimensions and composition. If retained, the patient may develop infective endocarditis, pericarditis, arrhythmias, thrombi, and mood disorders, which may obligate urgent removal.22 Some authors suggest that the foreign bodies may be left if asymptomatic for a time frame.
Conclusion
We report a case of a suspected ACS after a CGSI that was conservatively managed. The physician should be aware of the clinical implications of a CGSI, its diagnosis using complementary imaging techniques, and its invasive and noninvasive management strategies.
Supplementary Material
Footnotes
Authors’ Note: All available data can be obtained by contacting the corresponding author.
Author Contributions: TK, RS, VS, SP, CJ, and NS contributed equally in writing the manuscript. All authors read and approved the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent: The patient provided express written, informed consent to have the details of his case published.
ORCID iD: Naveen Anand Seecheran  https://orcid.org/0000-0002-7779-0181
https://orcid.org/0000-0002-7779-0181
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Kaya A, Caliskan E, Tatlisu MA, et al. A retained bullet in pericardial sac: penetrating gunshot injury of the heart. Case Rep Cardiol. 2016;2016:2427681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Campbell NC, Thomson SR, Muckart DJ, Meumann CM, Van Middelkoop I, Botha JB. Review of 1198 cases of penetrating cardiac trauma. Br J Surg. 1997;84:1737-1740. [PubMed] [Google Scholar]
- 3. Alexi-Meskishvili V, Böttcher W. Suturing of penetrating wounds to the heart in the nineteenth century: the beginnings of heart surgery. Ann Thorac Surg. 2011;92:1926-1931. [DOI] [PubMed] [Google Scholar]
- 4. Bruss J, Jacobs LE, Kotler MN, Loli AW. Utility of transesophageal echocardiography in the conservative management of prosthetic valve endocarditis. Chest. 1992;102:1886-1888. [DOI] [PubMed] [Google Scholar]
- 5. Symbas PN, Vlasis-Hale SE, Picone AL, Hatcher CR., Jr. Missiles in the heart. Ann Thorac Surg. 1989;48:192-194. [DOI] [PubMed] [Google Scholar]
- 6. Dixon RG, McEwan P. Notes on a case of penetrating wound of the heart. Br Med J. 1916;1:755-756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Biocina B, Sutlić Z, Husedzinović I, et al. Penetrating cardiothoracic war wounds. Eur J Cardiothorac Surg. 1997;11:399-405. [DOI] [PubMed] [Google Scholar]
- 8. Asensio JA, Murray J, Demetriades D, et al. Penetrating cardiac injuries: a prospective study of variables predicting outcomes. J Am Coll Surg. 1998;186:24-34. [DOI] [PubMed] [Google Scholar]
- 9. Trinkle JK, Marcos J, Grover FL, Cuello LM. Management of the wounded heart. Ann Thorac Surg. 1974;17:230-236. [DOI] [PubMed] [Google Scholar]
- 10. Szentpetery S, Lower RR. Changing concepts in the treatment of penetrating cardiac injuries. J Trauma. 1977;17:457-461. [DOI] [PubMed] [Google Scholar]
- 11. Wani ML, Ahangar AG, Wani SN, Irshad I, Ul-Hassan N. Penetrating cardiac injury: a review. Trauma Mon. 2012;17:230-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Morton JR, Reul GJ, Arbegast NR, Okies JE, Beall AC., Jr. Bullet embolus to the right ventricle. Report of three cases. Am J Surg. 1971;122:584-590. [DOI] [PubMed] [Google Scholar]
- 13. Hussein N, Rigby J, Abid Q. Bullet embolus to the right ventricle following shotgun wound to the leg. BMJ Case Rep. 2012;2012:bcr2012007471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bali HK, Vijayvergiya R, Banarjee S, Kumar N. Gunshot injury of the heart: an unusual cause of acute myocardial infarction. Tex Heart Inst J. 2003;30:158-160. [PMC free article] [PubMed] [Google Scholar]
- 15. Doetsch N, Wolfhard U, Mathers MJ, Zerkowski HR. Survival after heart and coronary-artery penetration by an air-rifle projectile. Thorac Cardiovasc Surg. 1989;37:332-334. [DOI] [PubMed] [Google Scholar]
- 16. Mukherjee DK, Banka VS, Keosathit N, Helfant RH. Penetrating injury of the chest and coronary arteriovenous fistula. Chest. 1976;69:793-795. [DOI] [PubMed] [Google Scholar]
- 17. Hopkins HR, Pecirep DP. Bullet embolization to a coronary artery. Ann Thorac Surg. 1993;56:370-372. [DOI] [PubMed] [Google Scholar]
- 18. Jackson L, Stewart A. Best evidence topic report. Use of troponin for the diagnosis of myocardial contusion after blunt chest trauma. Emerg Med J. 2005;22:193-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bansal MK, Maraj S, Chewaproug D, Amanullah A. Myocardial contusion injury: redefining the diagnostic algorithm. Emerg Med J. 2005;22:465-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Clancy K, Velopulos C, Bilaniuk JW, et al. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg. 2012;73(5 suppl 4):S301-S306. [DOI] [PubMed] [Google Scholar]
- 21. Feliciano DV, Rozycki GS. Advances in the diagnosis and treatment of thoracic trauma. Surg Clin North Am. 1999;79:1417-1429. [DOI] [PubMed] [Google Scholar]
- 22. Balbi M, Bertero G, Bellotti S, Rolandelli ML, Caponnetto S. Right-sided valvular endocarditis supported by an unexpected intracardiac foreign body. Chest. 1990;97:1486-1488. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



