Abstract
Objective
To evaluate the efficacy of the figure-of-eight (FOE) suture technique in the treatment of tunnel bleeding after femoral artery puncture compared with manual compression (MC).
Methods
This prospective, randomized, controlled study enrolled patients that had received transfemoral coronary artery angiography or percutaneous coronary intervention and then developed tunnel bleeding. They were randomly assigned into two groups: FOE suture group (ES group) and manual compression group (MC group). Total treatment time, performance frequency, performance time, rate of deep vein thrombosis (DVT) and in-hospital time after the procedure were compared.
Results
A total of 152 patients were enrolled in the study (ES group, n = 63; MC group, n = 89). Compared with the MC group, the total treatment time (mean ± SD: ES 22.3 ± 5.4 h versus MC 26.8 ± 6.8 h), performance frequency (mean ± SD: ES 2.1 ± 0.7 versus MC 2.6 ± 1.1), performance time (mean ± SD: ES 8.9 ± 2.5 min versus MC 12.3 ± 4.1 min), in-hospital time after the procedure (mean ± SD: ES 3.5 ± 1.2 days versus MC 4.8 ± 2.1 days) and DVT rate (ES 0.0% versus MC 6.7%) were significantly lower in the ES group.
Conclusion
The FOE suture technique effectively treated tunnel bleeding after femoral artery puncture.
Keywords: Femoral artery puncture, tunnel bleeding, figure-of-eight suture, haemostasis method, compression
Introduction
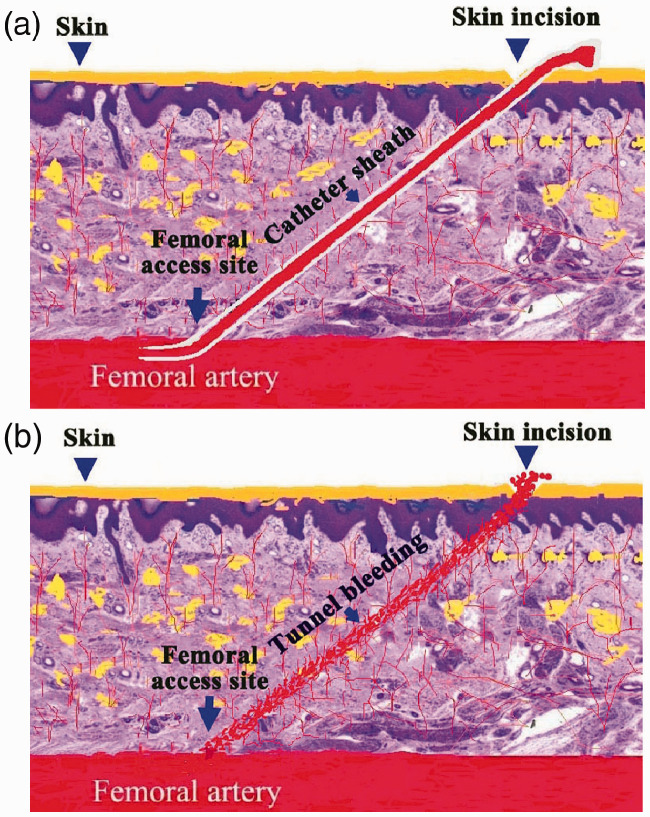
Femoral artery puncture is a basic technique that is used routinely for coronary artery disease diagnosis and treatment. Along with the widespread use of radial artery puncture as a default way of catheter insertion,1 the use of the femoral artery as the puncture site has been reduced considerably. However, the choice of the femoral artery as the catheter route remains irreplaceable in some special clinical situations. Femoral artery puncture is associated with more bleeding complications that require more post-procedure treatments compared with radial artery puncture.1 Vascular closure devices (VCDs) can reduce the occurrence of serious bleeding complications from the femoral artery,2 but they cannot decrease the incidence of incision bleeding.3 When a catheter or catheter sheath pass though subcutaneous tissue, they can produce a subcutaneous tunnel between the skin incision and the artery access site. When the catheter or catheter sheath are withdrawn, the tunnel can bleed because of the injury caused to the tissue surrounding the tunnel. This type of bleeding is called tunnel bleeding (Figure 1). Tunnel bleeding is characterized by slow incision bleeding caused by capillary haemorrhage, which can be stopped by compressing or suturing the tunnel. Bleeding from the skin incision may also originate from the femoral artery access site, which will be much faster and more severe than the tunnel bleeding.
Figure 1.
Schematic diagram of the development of tunnel bleeding as a consequence of inserting a catheter into the femoral artery: (a) before drawing the catheter sheath out; (b) tunnel bleeding after drawing the catheter sheath out. The colour version of this figure is available at: http://imr.sagepub.com.
Although tunnel bleeding is slow and minor, it can induce discomfort and anxiety in patients. If treated inappropriately, it can give rise to severe secondary complications such as deep vein thrombosis (DVT).4 Traditional haemostasis methods involving prolonged manual compression can be very tiring for physicians and healthcare professionals; and they can limit the patient’s regular movement of the inferior extremity for a long period of time, which can lead to venous thrombosis.4,5 The figure-of-eight (FOE) suture technique is simple and easy to perform. In a study of femoral vein haemostasis after cryoballoon ablation for atrial fibrillation, the FOE suture technique provided advantages over manual compression.6 In terms of treating incision bleeding from the femoral artery route after percutaneous coronary intervention (PCI) or angiography, there is no evidence of whether the FOE suture technique is more effective than manual compression. This current study evaluated the efficacy of the FOE suture technique in the treatment of tunnel bleeding after femoral artery puncture compared with manual compression.
Patients and methods
Study design and patient population
This prospective, randomized, controlled study with blind endpoint evaluation enrolled patients that underwent the diagnosis and treatment of chest discomfort in the Department of Cardiology, The First Medical Centre, Chinese PLA General Hospital, Beijing, China between December 2013 and December 2016. The inclusive criteria were as follows: (i) age range 40–80 years; (ii) no obviously abnormal hepatic or renal function; (iii) coagulation parameters and platelet counts were within the normal range; (iv) tunnel bleeding after femoral artery puncture. The exclusive criteria were as follows: (i) taking anticoagulation drugs; (ii) history of DVT; (iii) existing focal complication including haematoma (diameter >5 cm), pseudoaneurysm and artery venous fistula; (iv) with femoral venous puncture. These patients were randomly assigned into one of two groups: the FOE suture group (ES group) and the manual compression group (MC group). Randomization was performed using a computer-generated randomization schedule at entry of the eligible patients to the study.
This study was conducted in accordance with the Declaration of Helsinki and the protocol was approved by The Institutional Review Boards of the Chinese PLA General Hospital, Beijing, China in November 2013. Written informed consent to participate was obtained from all of the study participants.
Definition of tunnel bleeding
Regardless of whether or not a VCD was used, the incision was routinely compressed and covered with a dressing followed by an elastic bandage after removal of the catheter or catheter sheath from the incision. If blood permeated the dressing, the dressing was replaced with a new one and then observed without any compression being applied for 1 min. During the observation period, if the new dressing became permeated with blood, tunnel bleeding was diagnosed. If the new dressing was rapidly permeated with blood, and/or the tissue around the incision rapidly swelled, bleeding from the femoral artery access site was diagnosed. Patients that experienced bleeding from the femoral artery access site were withdrawn from the study.
Haemostasis treatment methods for the two study groups
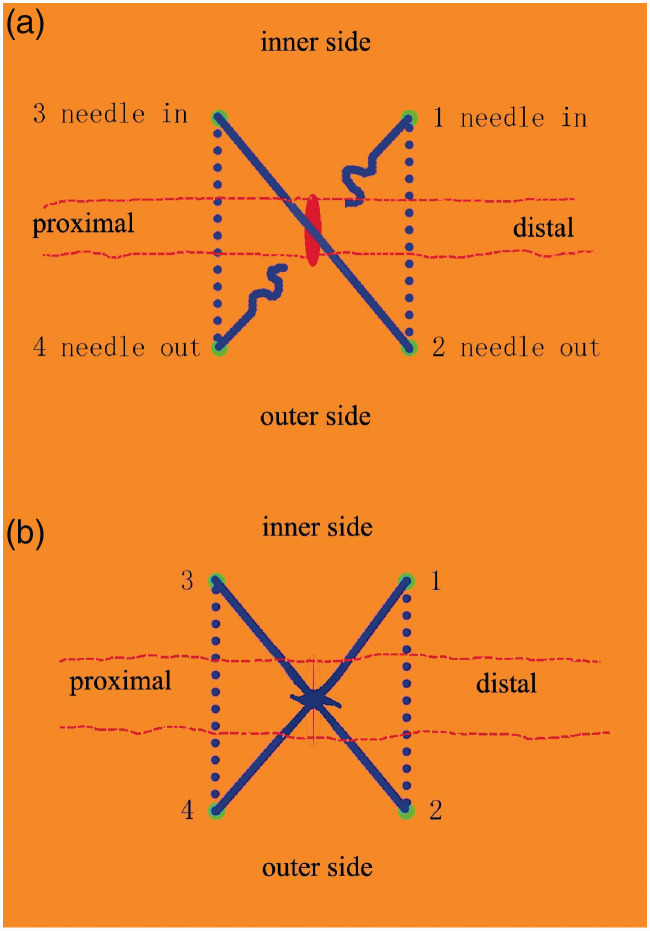
All haemostasis techniques were performed by trained physicians (Y.H., J.G.N. & Q.X.). For the FOE group (ES group), the FOE suture technique was undertaken as follows. A 26 mm needle (Plastic/Skin W2511-Ethicon with 45 cm silk braided non-absorbable suture; Johnson & Johnson Medical (China) Ltd., Shanghai, China) was used to puncture the skin at the first point (distal point: 2 mm from the inner side of the incision) with about 2 mm depth, then the needle was moved parallel to the incision line and pushed out of the skin at the second point (distal point: 2 mm from the outer side of the incision) (Figure 2). The needle was then moved across the incision and inserted into the skin at the third point (proximal point: 2 mm from the inner side of the incision) with about 2 mm depth, then it was moved parallel to the incision line and pushed out of the skin at the fourth point (proximal point: 2 mm from the outer side of the incision). The width between the in and out of the needle point was a little bit bigger than that of the incision line. The suture was completed by a ligation at the surface of the incision centre and it formed the shape of a figure-of-eight (i.e. 8). The bleeding tunnel was then closed. The ligation and suture were removed the following day. Following the FOE suture technique, routine elastic bandages were applied. If the bleeding was not stopped after insertion of the first suture, then suturing could be repeatedly performed until the bleeding was stopped.
Figure 2.
Schematic diagram of the figure-of-eight (FOE) suture technique used in the current prospective, randomized study: (a) the route of the needle moving; (b) the incision closed by the FOE suture. Note: inner side (inner side of the incision), outer side (outer side of the incision), proximal (proximal side of the incision), distal (distal side of the incision), red oval (incision), red line (sutured incision), four green points (in and out points of the needle), blue full line (suture on the surface of the skin), blue dotted line (subcutaneous suture), 1, 2, 3 and 4 (in and out sequence of the needle). The colour version of this figure is available at: http://imr.sagepub.com.
For the manual compression group (MC group), firm compression and/or prolonged compression time were used to treat the tunnel bleeding, followed by the application of routine elastic bandages. If the bleeding was not stopped after one application of firm compression, the compression was repeated until the bleeding stopped.
The routine method of treating bleeding from a femoral artery access site in the Department of Cardiology, The First Medical Centre, Chinese PLA General Hospital was as follows. Coronary angiography was undertaken at the right anterior oblique projection using the transfemoral path. The haemostasis methods used for femoral artery access site bleeds were as follows: (i) a VCD Angio-seal (Terumo Medical Corp., Somerset, NJ, USA) with a catheter diameter of 6F or 7F was used to seal the puncture site if the focal anatomy was suitable for it. Elastic bandage compression and limb immobilization was maintained for 6 h after the closure of the punctured artery. Off-bed activity was allowed after 24 h after the closure of the punctured artery; (ii) manual compression was chosen as an alternate method if the focal anatomy was not suitable for the VCD procedure. The elastic bandage compression and limb immobilization was prolonged to 8–12 h. The time interval between the manual compression and the off-bed activity was the same as for the VCD users. In order to avoid incision injury induced by sudden movements, all patients were educated to protect the incision site by manual compression during body position changes.
Study outcomes
A schematic diagram that shows the treatment course for the two groups is presented in Figure 3. During the course of treatment of the tunnel bleeding, the following parameters were recorded: (i) total treatment time, which was the time from the commencement of haemostasis to when the bleeding stopped and the dressing and elastic bandage were removed; (ii) performance frequency, which was the total number of times that the dressing was changed because of tunnel bleeding; (iii) performance time, which was the total time taken to perform the FOE sutures or manual compression; (iv) rate of DVT, as detected and diagnosed by ultrasound, after coronary angiography or PCI; (v) in-hospital time after procedure, which was the total time spent in hospital after the final procedure of coronary angiography or PCI. All of the parameters were recorded by technicians and nurses who were specially trained and blinded to the haemostasis method.
Figure 3.
Schematic diagram of the treatment procedure used in the figure-of-eight suture technique group (ES) and the manual compression group (MC). DB, dressing beginning; TB, tunnel bleeding; FDR, final dressing removal; long blue bar, total treatment time; short green bar, performance time; number of short green bars, performance frequency. The colour version of this figure is available at: http://imr.sagepub.com.
Statistical analyses
All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 22.0 (IBM Corp., Armonk, NY, USA). The statistician (Q.Z.F.) was blinded to the haemostasis methods. Data are presented as mean ± SD unless otherwise stated. Student’s t-test was used to compare mean values. Comparisons of proportions between the two groups were performed using a two-sided χ2-test. A two-tailed P-value of ≤0.05 was considered statistically significant.
Results
This study screened a total of 23 126 consecutive patients between December 2013 and December 2016. Of these, 152 patients met the inclusive criteria and were included in the study. The baseline clinical and demographic data for the two groups are shown in Table 1. There were no significant differences between the two groups at baseline.
Table 1.
Baseline clinical and demographic data for the patients enrolled in this study of the efficacy of the figure-of-eight (FOE) suture technique (ES group) compared with manual compression (MC group) in the treatment of tunnel bleeding after percutaneous coronary intervention or angiography.
| Characteristic | ES groupn = 63 | MC groupn = 89 |
|---|---|---|
| Sex, female | 35 (55.6) | 40 (44.9) |
| Age, years | 57.3 ± 14.2 | 52.8 ± 17.5 |
| Body mass index, kg/m2 | 26.5 ± 7.4 | 27.6 ± 9.1 |
| GPT, U/l | 25.6 ± 5.9 | 28.1 ± 9.3 |
| eGFR, % | 78.5 ± 23.3 | 88.2 ± 35.6 |
| PCI | 42 (66.7) | 70 (78.7) |
| Hypertension | 47 (74.6) | 75 (84.3) |
| Diabetes mellitus | 38 (60.3) | 49 (55.1) |
| Vascular closure device use | 46 (73.0) | 75 (84.3) |
| Catheter model | ||
| 7F | 11 (17.5) | 18 (20.2) |
| 6F | 52 (82.5) | 71 (79.8) |
Data presented as mean ± SD or n of patients (%).
No significant between-group differences (P > 0.05); Student’s t-test was used to compare mean values; comparisons of proportions between the two groups were performed using a two-sided χ2-test.
GPT, glutamic pyruvic transaminase; eGFR, estimated glomerular filtration rate; PCI, percutaneous coronary intervention.
Comparison of the study outcomes between the two groups is shown in Table 2. Compared with the MC group, the total treatment time, performance frequency, performance time, in-hospital time after the procedure and DVT rate were significantly lower in the ES group (P < 0.05 for all comparisons). There was no femoral pseudoaneurysms in either group.
Table 2.
Comparison of the study outcomes for the patients enrolled in this study of the efficacy of the figure-of-eight (FOE) suture technique (ES group) compared with manual compression (MC group) in the treatment of tunnel bleeding after percutaneous coronary intervention or angiography.
| Study outcome | ES groupn = 63 | MC groupn = 89 | Statistical analysisa |
|---|---|---|---|
| Total treatment time, h | 22.3 ± 5.4 | 26.8 ± 6.8 | P < 0.0001 |
| Performance frequency, number of times | 2.1 ± 0.7 | 2.6 ± 1.1 | P = 0.0018 |
| Performance time, min | 8.9 ± 2.5 | 12.3 ± 4.1 | P < 0.0001 |
| In-hospital time after procedure, days | 3.5 ± 1.2 | 4.8 ± 2.1 | P < 0.0001 |
| Deep vein thrombosis | 0 (0.0) | 6 (6.7) | P = 0.0419 |
Data presented as mean ± SD or n of patients (%).
Student’s t-test was used to compare mean values; comparisons of proportions between the two groups were performed using a two-sided χ2-test.
Discussion
Femoral artery puncture has been widely used and developed since 1967 when it was designed to be used for coronary angiography.7As a consequence of the complications and discomfort associated with the femoral artery puncture procedure, researchers have been seeking other ways to replace this technique. The use of transradial access coronary artery angiography was first reported in 1989.8 Subsequently, the use of transradial coronary artery angiography and PCI was reported in 1993.9 Since then, transradial coronary artery angiography and PCI have become more popular because this technique is associated with improved comfort, less bleeding complications, immediate off-bed mobilization and early discharge after the procedure than femoral artery puncture.1 Although it would seem that femoral artery puncture could be discarded permanently, there are special conditions when cardiologists will have to use transfemoral access, such as during severe spasm or tortuosity of the radial artery and/or truncus brachiocephalicus, distortion of the ascending aorta and aortic sinus, ectopia of the coronary artery ostium, when a larger catheter (>7F) is needed and when bilateral coronary artery angiography in required because of chronic complete occlusion.10,11 Therefore, despite the usefulness and popularity of transradial access, transfemoral access remains an important access technique.
For many years, manual compression was used as the default method for treating bleeding at the puncture site after the transfemoral access procedure. This method is associated with patient discomfort and a vasovagal reaction that may induce adverse effects, especially for patients that have undergone PCI.4 Manual compression is a very laborious technique for physicians and healthcare professionals to perform for long periods of time. Therefore, VCDs were developed in the 1990s to close the access site of the femoral artery. However, a special complication of using VCDs gradually emerged as their use became more widespread.12 As a consequence of inserting the VCD catheter, which is often larger in diameter than routine catheters, in and out repeatedly, the tiny vessels in the subcutaneous tunnel become injured.13 This damage often results in subcutaneous tunnel bleeding, especially when strong anti-thrombosis medication is also being administered.13
This current prospective, randomized, controlled study focused on one of the complications of femoral access, the bleeding from the subcutaneous tunnel, which to the best of our knowledge has not been described in the literature to date. This current study investigated the use of an alternate haemostasis technique to manual compression that involved the use of a FOE suture technique. The results of this current study demonstrated that the FOE suture technique provided benefits to the patients with tunnel bleeding in terms of a significantly lower total treatment time, performance frequency, performance time, in-hospital time after the procedure and DVT rate compared with manual compression. The application of firm pressure on the subcutaneous tissues around the tunnel, which was provided by both haemostasis methods investigated in this current study, was the mechanism responsible for stopping the bleeding. The better efficacy of the FOE suture technique might have been due to the continuous application of firm pressure on the tissue around the tunnel compared with shorter durations of firm pressure that were provided by manual compression.
Figure-of-eight sutures for haemostasis have been used to treat bleeding after the intervention via the femoral vein.6,14,15 The FOE suture can reduce the risk of rebleeding, shorten the duration of bed rest and relieve patient discomfort.6,15 When used for haemostasis following intervention via the femoral vein, the suture silks are placed in the site before removal of the catheter or catheter sheaths.6 Considering the high risk of bleeding from the femoral artery, the FOE suture was inserted after removing the catheter or catheter sheaths and closing the femoral artery access site in this current study. The efficacy of the FOE suture technique was demonstrated to be better than manual compression in the current study and no femoral pseudoaneurysms occurred.
In addition to the improved efficacy, the use of the FOE suture technique did not increase the cost of treatment because of no expensive medication or devices were used. The FOE suture technique is a basic procedure used during surgery, although physicians might not be used to performing it in their routine work. The results of the current study suggest that the FOE suture technique would be a good choice for treating subcutaneous tunnel bleeding as it easily and quickly resolves the bleeding.
This current randomized study had several limitations. First, the study was conducted in a single centre and only included 152 patients. The study did not perform a sample size estimate and the small sample size might have some effects on the generalizability of the findings. Secondly, the firmness of the applied manual compression might have varied between patients as it is a manual procedure. As the firmness was adjusted to stop the bleeding without causing ischaemia of the inferior extremity, the variability was unlikely to affect the results. Thirdly, the use of a VCD was not randomly assigned. VCD use might have had some effects on tunnel injury and bleeding, but there was no significant difference in the rate of VCD use between the two groups, which suggests that the effect of this bias on the results was very small. Finally, this study was designed to investigate the treatment of tunnel bleeding and not the DVT outcomes.
In conclusion, the FOE suture technique effectively treated tunnel bleeding after femoral artery puncture and was superior to a traditional manual compression method.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Quan-Zhou Feng https://orcid.org/0000-0001-5157-087X
References
- 1.Ratib K, Mamas MA, Anderson SG, et al. Access site practice and procedural outcomes in relation to clinical presentation in 439,947 patients undergoing percutaneous coronary intervention in the United Kingdom. JACC Cardiovasc Interv 2015; 8: 20–29. [DOI] [PubMed] [Google Scholar]
- 2.Holm NR, Sindberg B, Schou M, et al. Randomised comparison of manual compression and FemoSeal™ vascular closure device for closure after femoral artery access coronary angiography: the CLOSure dEvices Used in everyday Practice (CLOSE-UP) study. EuroIntervention 2014; 10: 183–190. [DOI] [PubMed] [Google Scholar]
- 3.Alshehri AM, Elsharawy M. Comparison of Angioseal and Manual Compression in Patients Undergoing Transfemoral Coronary and Peripheral Vascular Interventional Procedures. Int J Angiol 2015; 24: 133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chisci E, Setacci F, Giubbolini M, et al. Stroke and pulmonary embolism following manual and bandage compression after bleeding from a common femoral artery access site. J Cardiovasc Surg (Torino) 2011; 52: 849–851. [PubMed] [Google Scholar]
- 5.Sisante JF, Abraham MG, Phadnis MA, et al. Ambulatory Status Protects against Venous Thromboembolism in Acute Mild Ischemic Stroke Patients. J Stroke Cerebrovasc Dis 2016; 25: 2496–2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar V, Wish M, Venkataraman G, et al. A randomized comparison of manual pressure versus figure-of-eight suture for hemostasis after cryoballoon ablation for atrial fibrillation. J Cardiovasc Electrophysiol 2019; 30: 2806–2810. [DOI] [PubMed] [Google Scholar]
- 7.Judkins M, Judkins E. Coronary arteriography and left ventriculography: Judkins technique In: SI King, JJ Douglas. (eds). Coronary Arteriography and Angioplasty. New York: McGraw-Hill, 1985, pp. 182–217. [Google Scholar]
- 8.Campeau L. Percutaneous radial artery approach for coronary angiography. Cathet Cardiovasc Diagn 1989; 16: 3–7. [DOI] [PubMed] [Google Scholar]
- 9.Kiemeneij F, Laarman GJ. Percutaneous transradial artery approach for coronary stent implantation. Cathet Cardiovasc Diagn 1993; 30: 173–178. [DOI] [PubMed] [Google Scholar]
- 10.Yang CH, Guo GB, Chen SM, et al. Feasibility and safety of a transradial approach in intervention for chronic total occlusion of coronary arteries: a single-center experience. Chang Gung Med J 2010; 33: 639–645. [PubMed] [Google Scholar]
- 11.Kiemeneij F, Laarman GJ, Odekerken D, et al. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol 1997; 29: 1269–1275. [DOI] [PubMed] [Google Scholar]
- 12.Krishnasamy VP, Hagar MJ, Scher DJ, et al. Vascular Closure Devices: Technical Tips, Complications, and Management. Tech Vasc Interv Radiol 2015; 18: 100–112. [DOI] [PubMed] [Google Scholar]
- 13.Dangas G, Mehran R, Kokolis S, et al. Vascular complications after percutaneous coronary interventions following hemostasis with manual compression versus arteriotomy closure devices. J Am Coll Cardiol 2001; 38: 638–641. [DOI] [PubMed] [Google Scholar]
- 14.Cilingiroglu M, Salinger M, Zhao D, et al. Technique of temporary subcutaneous “Figure-of-Eight” sutures to achieve hemostasis after removal of large-caliber femoral venous sheaths. Catheter Cardiovasc Interv 2011; 78: 155–160. [DOI] [PubMed] [Google Scholar]
- 15.Okada M, Inoue K, Tanaka K, et al. Efficacy and Safety of Figure-of-Eight Suture for Hemostasis After Radiofrequency Catheter Ablation for Atrial Fibrillation. Circ J 2018; 82: 956–964. [DOI] [PubMed] [Google Scholar]