Abstract
Background:
The incidence of nontraumatic fatalities in high school (HS) and National Collegiate Athletic Association (NCAA) football players has continued at a constant rate since the 1960s.
Purpose:
To describe the causes of nontraumatic fatalities in HS and NCAA football players and provide prevention strategies.
Study Design:
Descriptive epidemiology study.
Methods:
We reviewed 187 fatalities in HS and NCAA nontraumatic football players catalogued by the National Registry of Catastrophic Sports Injuries during a 20-year period between July 1998 and June 2018.
Results:
The majority (n = 162; 86.6%) of fatalities occurred during a practice or conditioning session. Most fatalities, when timing was known, (n = 126; 70.6%) occurred outside of the regular playing season, with the highest incidence in the August preseason (n = 64; 34.2%). All documented conditioning sessions were supervised by a coach (n = 92) or strength and conditioning coach (n = 40). The exercise regimen at the time of the fatality involved high-intensity aerobic training in 94.7%. Punishment was identified as the intent in 36 fatalities. The average body mass index of the athletes was 32.6 kg/m2. For athletes who died due to exertional heat stroke, the average body mass index was 36.4 kg/m2, and 97.1% were linemen.
Conclusion:
Most nontraumatic fatalities in HS and NCAA football players occurred during coach-supervised conditioning sessions. The primary cause of exertion-related fatalities was high-intensity aerobic workouts that might have been intended as punishment and/or excess repetitions. Exertion-related fatalities are potentially preventable by applying standards in workout design, holding coaches accountable, and ensuring compliance with the athlete’s health and current welfare policies.
Keywords: football, fatalities, cardiac, sickle cell trait, exertional heat stroke, asthma, prevention
Football, one of the most popular team sports in the United States, is also associated with the highest number of fatalities for any high school (HS) or college sport.6,23 From the 1960s to the 2010s, the incidence of traumatic deaths declined sharply in HS and college football, reflecting the ban on spear tackling, new helmet design, and medical care of brain injuries.7 During this time, however, there has been less focus on preventing nontraumatic deaths in football players. This may be because of traumatic fatalities occurring mostly during games and being defined as a direct result of the sport, whereas nontraumatic fatalities were erroneously defined as not being directly caused by sport participation. There is a perception that trauma may be mitigated via rules and equipment. In contrast, nontraumatic fatalities imply inherent individual frailty for which neither sport practices nor practitioners are deemed responsible.
An index point in National Collegiate Athletic Association (NCAA) football is circa 2000 when year-round training became common.2 Since 2000, nontraumatic deaths have exceeded traumatic deaths: 2-fold in HS and 4-fold in college.7 Therefore, we hypothesized that football conditioning programs have inherent design flaws, leading to fatalities. This is part 2 of a 2-part study; the purpose of part 1 was to compare the incidence of nontraumatic fatalities with that of traumatic fatalities, describe the epidemiology of nontraumatic fatalities in HS and college football players, and determine the effectiveness of NCAA policies to reduce exertional heat stroke (EHS) and exertional sickling (ES) with sickle cell trait (SCT) fatalities.7 The aim of part 2 was to explore the characteristics of the training programs to determine the causes of nontraumatic deaths in HS and NCAA football players. After the causes of these fatalities are identified, prevention strategies can be developed and implemented.1
Methods
This study was ruled exempt from institutional review board oversight. The injury definitions, methodology, and number of reports reviewed were described in part 1 of this study.7 Football fatalities were limited to HS and NCAA athletes between July 1998 and June 2018. In addition to the data collected in part 1, information was obtained on player characteristics (age, weight, height, body mass index [BMI], position played, and game or practice). The month of the fatality was categorized as out-of-season (January through August), preseason (August, a subdivision of out-of-season), and playing season (September through December). Exercise regimens at the time of the fatality were defined as high-intensity aerobic training if the athlete was performing at least 1 of the following tasks: serial sprints, agility drills, fitness tests, exercising at a work-to-rest ratio greater than 1:3, or running for greater than 30 minutes without a break. Low-intensity exercise was categorized as weight lifting, jogging, or games (average work-to-rest ratio, 1:8).31 Although the intent of punishment may be difficult to establish, we identified cases based on the NCAA description of punishment workouts as a corrective response to poor performance and being inconsistent with the conditioning level of the athlete or team. Punitive workouts are motivated by anger or frustration, are unplanned, and are not based on sound principles of exercise science and physiology; rather, they are employed to make athletes “tougher” or to create a team culture of “accountability.”39 To augment the definition, we only included cases in which a teammate or independent observer reported that the coach was being abusive (bullying or taunting players who, before their demise, were visibly struggling to finish). Supervision of the conditioning session by a coach or strength and conditioning (S&C) coach was assessed. Weather conditions on the day and at the time of each fatality were obtained from the National Climatic Data Center for EHS and ES with SCT fatalities.34
Results
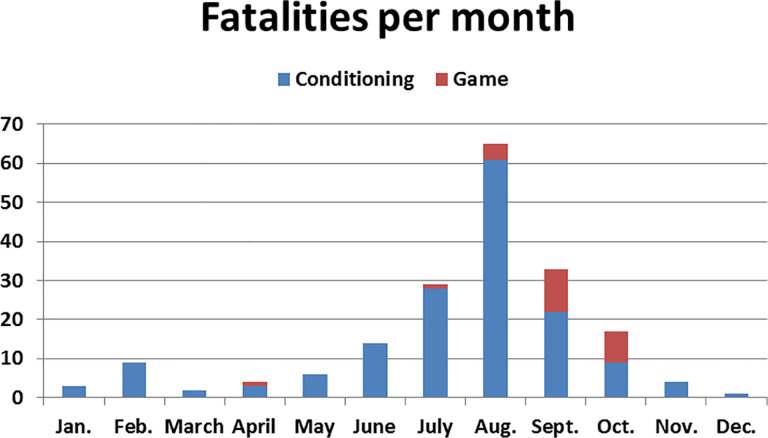
During the study period, there were 187 nontraumatic fatalitites in HS and NCAA football players (Table 1).7 Most (n = 162; 86.6%) fatalities occurred during a practice or conditioning session as compared with a game (n = 25; 13.4%) (Figure 1). All EHS, ES with SCT, and NCAA fatalities occurred during conditioning. Most fatalities, when timing was known, (n = 126; 70.6%) occurred outside of the regular playing season (Figure 1). August (n = 64; 34.2%) was the deadliest month and was when 55.8% of the EHS fatalities occurred. The majority of EHS (n = 40; 93.0%) and ES with SCT deaths (n = 18; 81.8%) occurred during off-season conditioning sessions. The exercise regimen before the death was determined in 113 of the conditioning sessions: 107 (94.7%) consisted of high-intensity aerobic training including all EHS and ES with SCT fatalities (Table 1). Punishment was identified as the intent in a minimum of 36 cases. Case examples and case reports of high-intensity aerobic training sessions and punishment drills are listed in Appendices 1 and 2. A minimum of 6 practices in which a fatality occurred had multiple players who required medical attention, with at least 3 requiring ambulance transportation to the emergency department. All documented conditioning sessions were supervised by a coach (n = 92) or S&C coach (n = 40).
Table 1.
Demographic Data and Playing Conditionsa
| All | SCA | EHS | ES With SCT | Asthma | Hyponatremia | |
|---|---|---|---|---|---|---|
| Total | 182 (100.0) | 105 (57.7) | 43 (23.6) | 22 (12.1) | 9 (4.9) | 3 (1.6) |
| Average age, y | 16.5 | 16.2 | 16.3 | 17.6 | 16.2 | 17.0 |
| Average BMI, kg/m2 | 32.6 | 30.2 | 36.4 | 31.7 | 27.9 | 28.2 |
| Practice | 162 (86.6) | 82 (78.1) | 43 (100.0) | 22 (100.0) | 8 (88.9) | 2 (66.7) |
| Game | 25 (13.4) | 23 (21.9) | 0 (0.0) | 0 (0.0) | 1 (11.1) | 1 (33.3) |
| Out of season | 126 (70.6) | 63 (60.0) | 40 (93.0) | 18 (81.8) | 5 (55.6) | 0 (0.0) |
| Preseason (August) | 64 (34.2) | 29 (27.6) | 24 (55.8) | 4 (18.2) | 4 (44.4) | 3 (100.0) |
| High-intensity aerobic trainingb | 107 (94.7) | 39 (90.7) | 43 (100.0) | 22 (100.0) | 3 (60.0) | Unknown |
| Low-intensity exerciseb | 6 (5.3) | 4 (9.3) | 0 (0.0) | 0 (0.0) | 2 (40.0) | 0 (0.0) |
| Lineman positionc | 79 (66.4) | 33 (52.4) | 34 (97.1) | 8 (66.6) | 2 (33.3) | 2 (66.6) |
aData are presented as n (%) unless otherwise specified. BMI, body mass index; EHS, exertional heat stroke; ES exertional sickling; SCA, sudden cardiac arrest; SCT, sickle cell trait.
bThe exercise regimen was known in 113 cases.
cThe player’s position was known in 119 cases. All percentages are based on total number of known data points (SCA = 63; EHS = 35; ES with SCT = 12; asthma = 6).
Figure 1.
Number of fatalities in football players per month during conditioning/practices versus games.
The average age, height, weight, and BMI were 16.5 years, 72.3 inches (183.54 cm), 242 lb (108.9 kg), and 32.6 kg/m2, respectively (Table 1). Athletes with EHS had the highest average BMI (36.4 kg/m2). The position played by the athlete was determined in 119 cases, with 79 (66.4%) linemen, 11 (9.2%) running backs, 10 (8.4%) linebackers, 7 (5.9%) defensive backs, 5 (4.2%) wide receivers, 4 (3.4%) tight ends, and 3 (2.5%) quarterbacks. Athletes with EHS had the highest percentage (97.1%) playing the lineman position.
Causes
Part 1 of this study reports the number, annual average, and incidence of fatalities for total and specific diagnoses at the HS and NCAA levels (see Table 1) as well as the percentage of each diagnosis (see Figure 3).7
Sudden Cardiac Arrest (SCA) (n = 105; 57.7%)
The specific diagnoses are provided in the cardiac results section of the companion paper.7 The majority (n = 82; 78.1%) of SCA fatalities occurred during a conditioning session. All game fatalities occurred in HS athletes. The exercise regimen was determined in 42 fatalities: sprinting in 31, intense agility drills in 6, work-to-rest ratio greater than 1:3 in 1, and low-intensity exercise in 4 cases. Punishment drills were recorded in 14 SCA cases. In 1 case, the athlete died while performing 2 hours of conditioning drills, including repetitive sprints, with full pads as a punishment for poor performance in a scrimmage the day before the incident. There were 11 athletes who had symptoms in a previous practice (n = 7) or abnormality on the preparticipation physical examination (PPE; n = 4) that was not fully investigated by the physician or for which medical instructions were provided but neglected by the parents.
EHS (n = 43; 23.6%)
All of the EHS fatalities (100.0%) occurred while athletes were performing high-intensity aerobic training during a conditioning session. A total of 34 of 35 (97.1%) fatalities from EHS occurred in either offensive or defensive linemen; 1 (2.9%) in a fullback; and 6 in players whose positions were unknown. Overall, 16 EHS cases were reported after punishment drills in response to a player missing an earlier practice, arriving late to a practice, or coach-perceived lack of effort. In 5 cases, water restriction was an identified component of the punishment sessions. In 1 fatality, a 315-lb (141.75-kg) lineman was required to perform 36 sprints with the team from sideline to sideline (Appendix 1). Despite struggling and falling to his knees, the coach encouraged him to continue.
The exact timing of the fatality was determined in 17 cases: 7 (41.1%) on the first day of practice, 8 (47.1%) on days 2 through 5, and 2 (11.8%) on days 6 through 14. The equipment worn was identified in 10 cases: 7 (70.0%) in players wearing no pads with or without a helmet and 3 (30.0%) in athletes wearing full equipment. The region of the heat-related death was identified in 42 cases and unknown in one. Of the known cases, most occurred in the South (n = 29; 69%), followed by the Midwest (n = 8; 18.6%), the Northeast (n = 3; 7.0%), and the West (n = 2; 4.7%); the location was unknown in 1. The states with the most fatalities were Georgia (n = 4) as well as Florida, Indiana, Maryland, and Kentucky, with 3 each.
The average maximum temperature and average maximum wet-bulb globe temperature (WBGT) recorded on the day of the fatality were 90.8°F (range, 76°F-104°F) and 76.7°F (range, 65°F-94°F), respectively (Table 2). The core body temperature at the hospital, identified in 13 cases, averaged 107.8°F (range, 105°F-111°F). The time of death from the onset of EHS symptoms was within 24 hours in 27 (62.8%) athletes, greater than 24 hours but less than 2 weeks in 14 (32.6%) athletes, and greater than 2 weeks in 2 (4.7%) athletes.
Table 2.
Weather Conditions for ES With SCT and EHS on Day of Fatalitya
| Diagnosis | Average Temperature | Maximum Temperature | Departure From Historic Average Temperature | Relative Humidity | Average WBGT | Maximum WBGT | Altitude (ft) |
|---|---|---|---|---|---|---|---|
| ES with SCT | 73.5 (30 to 89) | 83.0 (37 to 101) | 1.2 (–7 to 13) | 72.8 (45 to 88) | 65.2 (25 to 78) | 68.8 (30 to 80) | 596 (6 to 3294) |
| EHS | 79.8 (48 to 91) | 90.8 (76 to 104) | 2.6 (–37 to 15) | 75.7 (55 to 91) | 72.8 (58 to 79) | 76.7 (65 to 94) | 440 (6 to 1285) |
aData are presented as average (range). Temperatures are in Fahrenheit. EHS, exertional heat stroke; ES, exertional sickling; SCT, sickle cell trait; WBGT, wet-bulb globe temperature.
ES With SCT (n = 22; 12.1%)
All ES with SCT deaths (n = 22; 100.0%) occurred while athletes were performing high-intensity aerobic training during a conditioning session supervised by the coach or S&C coach (Table 1). At least 8 incidents had a component of punishment. In one 2001 ES with SCT fatality, the athletes were performing their annual mat drills, referred to as “10 days of hell”42 (Appendix 1). Overall, 3 segments, lasting 21 minutes each, of intense conditioning drills were performed with no break between segments. Stations were set up with trash cans for vomiting. According to one report, the assistant coach traditionally addressed the players on the first day of mat drills by stating, “You will pass out before you die. If you pass out, the trainers will take care of you.”42 The athlete had passed out the previous week while performing similar drills.
A total of 6 ES with SCT deaths occurred during the first day of regular-season (n = 3), off-season (n = 2), or summer (n = 1) practice; 3 of the conditioning sessions were held indoors. For the remaining 19 cases, the average maximum temperature and average maximum WBGT recorded on the day of the fatality were 83.0°F (range, 37°F-101°F) and 68.8°F (range, 30°F-80°F), respectively (Table 2).
Asthma (n = 9; 4.9%)
A total of 8 (88.9%) of the 9 asthma deaths occurred during conditioning sessions. In the lone NCAA case, 1 athlete performing the requisite 28 serial sprints (2160 yd) with a 1:1 work-to-rest ratio developed breathing difficulties and died; 4 other athletes who collapsed during the same intense workout required attention at the emergency department (Appendix 1).
Hyponatremia (n = 3; 1.6%)
A total of 3 deaths resulted from hyponatremia, all during the month of August: 2 during a practice and 1 during a game. Symptoms before death included confusion, headaches, slurred speech, vomiting, and seizures. All 3 athletes died as a result of cerebral edema from excessive hydration. One athlete consumed 4 gallons of water and electrolyte beverages between practice sessions.
Discussion
The most glaring finding in this study is that most (86.6%) nontraumatic fatalities (100.0% of EHS, ES with SCT, and NCAA) in HS and NCAA football athletes did not occur while competing in a game but rather during conditioning sessions supervised by a coach or S&C coach. The risk of nontraumatic exertion-related fatalities in practice sessions was previously identified.3,6 The causes and preventive strategies become evident in this robust data set and demonstrate a common theme of high-intensity aerobic exercise activity during out-of-season training, with lineman being an at-risk position, especially in EHS fatalities. While these fatalities may appear as isolated events, when assessed together over 20 years, they demonstrate a recurrent problem, indicating that extreme conditioning is unjustifiable.
In football, training is often by tradition, as athletes become coaches and tend to train future generations as they were trained.13 A common scenario is a coach, angry at a perceived lack of effort, subjecting players to excessive sprints and other conditioning drills. The focus is more on creating toughness and discipline than developing football fitness and skills.3,24,42 There is no evidence supporting the practice that abuse in conditioning enhances athletic performance or winning. In fact, this report demonstrates predictive adverse consequences from this coaching strategy. Establishing that exertion-related nontraumatic fatalities are directly caused by poorly organized training sessions versus inherent medical conditions is intrinsic to strategies preventing these deaths.
Although this report focused on fatalities, documented nonfatal EHS, ES with SCT, and exertional rhabdomyolysis cases are occurring via similar overexertion methods.16–18 The incidence of team outbreaks of exertional rhabdomyolysis due to excessive conditioning drills and a requirement that all athletes exert at the same pace and intensity is equally concerning.17 The pattern is clear: coaches exposing players to extreme drills and novel exertion. The drills are often designed to intimidate or punish athletes with the intent to inflict pain and push to the limit in the false belief that there is no limit. This pattern of coach-induced overexertion in nonfatal events is similar to the exercise regimens causing nontraumatic fatalities in this study.17 Regulating this training is overdue.
The findings in this study reveal that the workout leading to death often involved serial sprinting with high work-to-rest ratios. This contrasts with a football game, where most plays last on average 4 to 8 seconds with approximately 35 to 55 seconds of rest between standard plays and 15 to 20 seconds during hurry-up, no-huddle offense.20,31,40 Football drills should mimic game situations with applicable work-to-rest ratios. Conditioning programs should have a lower work-to-rest ratio early in the season, with a gradual progression over time.9 Conditioning drills should never be employed as retribution.
In this study, the majority of fatalities, especially EHS cases (average BMI, 36.4 kg/m2), occurred in linemen. Training regimens should be designed to be position specific, with, for example, skill players versus linemen, given differing sport demands and player habitus. This is also critical in at-risk players and settings, such as diminished level of player fitness, athletes returning from extended rehabilitation, transition to off-season and/or preseason, hot and/or humid conditions, and athletes with SCT. All transition periods (preseason, start of off-season, and return from injury) should allow for a minimum 7- to 10-day acclimation in exercise intensity with apt work-to-rest ratios. The S&C coach should work cooperatively with the medical staff in developing exercise science–based workout plans focused on sport-specific conditioning with a priority to improve sport skills.9 Further research is clearly necessary to determine safe work-to-rest ratios based on sport specificity and individual fitness level. One prevention strategy is to publicly post conditioning programs to foster accountability.
While overexertion is a primary component of a nontraumatic fatality, these fatalities, as evidenced by the case examples and reports (Appendices 1 and 2), may be accompanied by an inadequate medical response, even in the presence of an athletic trainer (AT). Instead of immediate withdrawal of a struggling athlete for assessment and treatment, the ATs often ignored distressed athletes, exhorted athletes to continue through the symptoms and complete the drill, or did not enact immediate proper treatment. This may partially be caused by subjection of ATs to a coach who prioritizes “performance” over medical care, with pressure to conform to a coach’s desire of teaching toughness in which medical care is considered as contributing to weakness of the mind and body. One solution to this problem, which has received consensus support9,11 and has been adopted by the NCAA as a bylaw,37 is “to establish an administrative structure that provides independent medical care and affirms the unchallengeable autonomous authority of primary health care providers to determine medical management and return-to-play decisions related to student-athletes.”38
Sudden Cardiac Arrest
The results of this study also indicate that intense physical activity can trigger covert cardiac conditions. However, compared with EHS, ES with SCT, and asthma fatalities, it is more difficult to directly link overexertion and cardiac deaths, as 23 of the cardiac fatalities, all in HS athletes, occurred during a game. In a report of sudden death due to a cardiovascular cause, there was a noted association with intense physical activity.28 Although overexertion is surely not the sole cause, it is a predominant component of sport-related cardiac fatalities for football players in training, with 99% of college SCA fatalities occurring during a practice or conditioning session.
Prevention strategies for cardiac fatalities include detecting cardiac abnormalities during the PPE, establishing and rehearsing an emergency action plan (EAP), and immediate on-field treatment of SCA using an automated external defibrillator (AED).8 Despite the focus on detecting covert cardiovascular conditions during the PPE, effective methods with high detection rates are lacking.27–29 Until cost-effective screening tests better identify at-risk athletes, priority should be placed on identifying athletes with previous exertion-related symptoms, noting abnormalities on the PPE, and completing any requested cardiology work-up based on PPE findings. While screening for cardiac conditions in the athlete has had limited effectiveness, athletes who experience SCA during exercise on HS campuses have a high survival rate, with immediate recognition and AED application within 3 minutes.8,12
Exertional Heat Stroke
We believe that the reason for failure of the 2003 out-of-season NCAA guidelines7 and the persistent rate of HS EHS fatalities is that current guidelines focus on the environment and uniform as causes of EHS while ignoring body habitus and exertion.8,10 We recommend a paradigm shift to prevent overexertion, the primary component of EHS fatalities.41 In this study, athletes were commonly performing bursts of intense exercise, typically sprinting. This supports EHS as predominantly exertional, not environmental.18,41 A second critical risk factor for heat stroke is body habitus, with 97.1% of the fatalities in this study occurring in linemen who had an average BMI of 36.4 kg/m2. During intense exertion, they have a diminished capacity to shed metabolic heat. Linemen should not be trained the same as skill players. Modifying exercise regimens for linemen and eliminating sustained, intense aerobic training are critical prevention recommendations. The weather conditions in this report did not reveal exceedingly hot environmental conditions, further implicating exertion. The average maximum temperature and average maximum WBGT on the day of the fatalities were only 90.8°F and 76.7°F, respectively, indicating that temperatures were most likely in the high 80s or low 90s during sport participation. However, there was an average 2.6°F elevation of temperature from normal in the EHS fatalities, which argues for the necessity of regional activity modification guidelines based on the change in weather conditions from baseline as opposed to universal WBGT thresholds that do not account for large changes in weather conditions.19 The football uniform may be overstated as an EHS risk factor. Overall, 70.0% of athletes with EHS fatalities in this report where the equipment worn was known were wearing shorts and a T-shirt, indicating that conditioning football players without pads, with or without a helmet, does not confer “safe” training. Last, hydration does not provide immunity from EHS. Most coaches, apart from the punishment reports, repeatedly avowed that they were providing frequent water breaks. Hydration is important, but dehydration is not the primary contributing factor for EHS.
Unlike SCA in which the athlete collapses and dies within minutes, in EHS deaths, the demise often occurs over several hours. In a minimum of 12 EHS cases, the athlete was found in distress after the practice. These findings support the continuation of monitoring, especially for high-risk athletes, even after completion of the practice sessions.
A renewed focus on acclimation with attention to baseline fitness, position-specific conditioning for linemen, regional acclimatization accounting for changes in baseline weather conditions, recognition of EHS signs and symptoms, a well-rehearsed EAP, and mandatory availability of an ice bath is recommended.
ES With SCT
The primary precipitating factor for all ES with SCT fatalities in this study, and corroborated by others,14,15 was sustained vigorous bouts of conditioning drills or sprints without adequate rest periods, which triggered sickling and explosive rhabdomyolysis.16 A minimum of 36% of the episodes were associated with punishment drills. SCT status knowledge is an invaluable clinical determinant.7 Natal screening tests should be easily accessible by a medical professional. SCT status must be confirmed on the PPE for all sports at all levels. The PPE provides a key opportunity for counseling an athlete with SCT with specific education for the risk of ES before the commencement of strenuous athletic participation.43 In the lone NCAA Division II ES with SCT fatality, the athlete signed a waiver declining the screening (Appendix 1). The NCAA must eliminate the opt-out waiver and require SCT status knowledge for all athletes.
The NCAA provides a proven model for the prevention of ES with SCT.7,36 When the status is known, targeted education follows, tailored precautions are implemented, and significant morbidity and mortality due to ES with SCT are prevented.7 There were 10 Division I football ES with SCT deaths in the 10 years before the NCAA screening and precautions began in 2010 and only 1 Division I death in the 9 years after the bylaw was adopted.1,7,16 According to the NCAA Sports Medicine Handbook, athletes with SCT should be allowed to train at their own pace; receive adequate hydration; be excused from performance tests, such as serial sprints or timed miles; never be urged to exercise at 100% beyond 2 or 3 minutes without a break; and discontinue activity upon struggling or experiencing symptoms.35 There were no recorded HS or NCAA ES deaths when the SCT status was known, education ensued, and precautions were heeded.
Unlike athletes with heat stroke, athletes with ES with SCT can collapse after a brief period of intense exercise. In contrast to SCA, athletes with ES with SCT can usually talk after they hit the ground. ES with SCT is a medical emergency. High-flow oxygen of 15 L/min with a non-rebreather mask should be initiated. Vital signs should be monitored, and if obtunded, the EAP should be activated. Emergency department physicians should be notified of the athlete’s SCT status and be warned of the possibility of explosive rhabdomyolysis, engaging a nephrologist and cardiologist to address potentially grave complications.
Asthma
Both our results (88.9%) and those of a comprehensive study (78%)5 on asthma deaths in athletes demonstrate that the majority of asthma-related deaths in organized sport occurred during a practice session. In the lone fatality in a college athlete, the workout required serial sprints at a 1:1 work-to-rest ratio, evidencing overexertion’s role in these fatalities.26 Prevention strategies for asthma-related deaths require parents and guardians of athletes with asthma to notify all medical personnel and the coaching staff of their medical condition and treatment plan, listing medications and the person responsible for ensuring that medications are present during practices and competitions.21
Hyponatremia
Hyponatremia in young athletes participating in team sports is rare and was identified in only 3 athletes in this study. One athlete in this study consumed 4 gallons of water and electrolyte beverages between practice sessions. The treatment of early hyponatremia requires medical referral for observation, restriction of fluids, and ingestion of hypertonic fluids or salty foods. For advanced cases, rapid sodium replacement with a hypertonic saline infusion intravenously is recommended. Prevention is paramount and best accomplished by educating athletes regarding fluid replacement and the potential risks of hyperhydration.30
Limitations
Our study is limited in that we were not able to document the exercise program in all of the cases. Nonetheless, the high percentage of documented cases in athletes performing high-intensity aerobic conditioning, all non-SCA cases, plus the numerous reports of punishment indicate that this trend likely would have persisted in the remaining cases. Nonetheless, this is the most comprehensive study on nontraumatic fatalities in football players, containing abundant information to substantiate our hypothesis that the primary cause of nontraumatic fatalities is overexertion.
Conclusion
The majority of nontraumatic fatalities in HS and NCAA football athletes did not occur in games but rather during out-of-season, coach-supervised conditioning sessions. The primary cause of exertion-related fatalities was intense aerobic workouts, often associated with punishment drills, with linemen being an at-risk group for EHS fatalities. Exertion-related fatalities are potentially preventable via an organizational structure: applying exercise science in the workout design based on position played and body habitus, holding coaches accountable, and ensuring compliance with the athlete’s health and current welfare policies. Further research is necessary to develop safe conditioning programs.
APPENDIX 1
Conditioning Errorsa
| Diagnosis | Description |
|---|---|
| Asthma | Post-thunderstorm: The head coach designed the “test,” consisting of 2160 yard of 28 serial sprints with a 1:1 work-to-rest ratio in approximately 12 minutes (ten 100-yard dashes in ≤15 seconds, then 15 seconds of rest, eight 80 seconds in ≤13 seconds, then 13 seconds of rest, and continue sequence). The athlete had four 40 seconds left when he collapsed, unable to breathe, and died an hour later. He had a history of asthma. The workout lacked exercise science, sport specificity, and compliance. |
| ECAST | Fast-tempo multiple conditioning stations: The athlete was not informed of his SCT condition, even though he tested positive. He pushed to continue during practice despite physically struggling. There was no targeted education or tailored precautions. |
| ECAST | 2 minutes of continuous sprints with short breaks for 20 minutes on the first full day of practice. |
| ECAST | Annual mat drills (“10 days of hell”): 3 segments, 21 minutes each, on padded mats with no break between each segment (jumping and scrambling, running through ropes, ducking under plastic pipes, stringent conditioning, and agility work). “Excruciating” stations were set up with trash cans for vomiting. One of the coaches said, “The body is a wonderful machine. You will pass out before you die. If you pass out, the trainers will take care of you.” The athlete had passed out the prior week while performing drills. During the fatal incident, the athlete collapsed on the ground and could not stand back up. “Come on!” his teammates cried. “You got to go 4 quarters!” They clapped to try to rally him, grabbed his arms, held him upright, and did the drills with him, just as they did in previous mat drills when he had struggled, never dreaming that they were dragging and exhorting him to his death. His foursome was ordered back to redo a set of drills, and when he fell behind again, he was sent back once more, the last man, finishing alone. The coach later said that he “worked himself to death.” The coach believed in pushing athletes to the breaking point.42 The SCT status was known, education occurred, and no precautions were implemented. |
| ECAST | Repetitive 300-yard “do-or-die” shuttle runs. The athlete collapsed after 2 repetitions (600 yard). He was SCT positive at another school but signed a waiver at the new school, so it was unaware of his positive status (records were not transferred). He had a similar medical episode in 2014 but recovered. |
| ECAST | Each session with 3 to 4 hours of intense football conditioning. The athlete collapsed at the end of the second session on day 1. A similar medical episode occurred 1 year earlier during football. The SCT status was unknown before the fatality. |
| ECAST | Punishment drills: 16 consecutive 100-yard sprints. The SCT status was unknown before the fatality. |
| ECAST | Punishment drills with obstacle course and extra sprints ordered because of players hanging their heads after a drill. Witnesses said that the player fell and was struggling but that the coach cursed and reprimanded him and ordered him to stand up and complete the drills. The SCT status was known, and no precautions were implemented. |
| ECAST | Sprints at the end of football practice. The coaches yelled for the athlete to continue, despite his struggling and having difficulty breathing. The SCT status was reported on the PPE form. |
| ECAST | The athlete collapsed on day 1 during the first 10 minutes of practice while running serial sprints. He ran half-speed sprints for 10 minutes and complained of calf cramps. He knew he had SCT but did not list it on his PPE form. |
| ECAST | The athlete completed 4 of 6 conditioning stations and appeared fatigued, leaning on a teammate’s shoulder and then crawling on his knees. He said, “I’m trying…I’m not weak. I just can’t go on.” A strength and conditioning coach recalled that he was pushed too hard. Coaches made him repeat because they did not feel that he gave a full effort. The SCT status was unknown before the fatality. |
| EHS | 36 sprints from sideline to sideline. |
| EHS | Punishment conditioning session to discipline several athletes for violating team rules. Players were required to run for over 1 hour without a break. |
| EHS | Punishment drills. The coach restricted water and was known for being verbally and physically abusive. |
| EHS | The athlete collapsed after a second 3-hour practice on the second day of preseason practice, which was called one of the “hardest workouts of the year.” He blacked out several times during practice but tried to push through while wearing shorts and a T-shirt. |
| EHS | Punishment drills. The athlete collapsed after morning practice. He had similar symptoms in high school and was trying to tough it out and be macho. |
| EHS | The athlete was found unconscious in a bathroom before the third practice of day 1. A coach took him to practice in which he participated without treatment, despite exhibiting symptoms of heat illness. His symptoms continued through the night. He attended practice on day 2, lost consciousness after practice, and subsequently died. There were punishment drills, with coaches threatening and shouting profanities. They ignored signs and symptoms while the athlete was experiencing a medical emergency. |
| EHS | Practice (102°F heat index) ended with 1100 yards of intense serial sprinting. After the drill, the athlete wandered off and was found approximately 15 minutes later by a dentist driving by 100 to 200 yards past the training room. |
| EHS | Circuit conditioning: 4 minutes at each station, 2-minute rest period, and then rotating to the next station while wearing shorts and a T-shirt. After the first 2 conditioning stations, the athlete told a member of the coaching staff that he did not feel well. He was instructed to drink water and return to practice, despite exhibiting clear signs and symptoms of heat illness. |
| EHS | The team’s first practice (105°F heat index) lasted 3.5 hours and ended with 16 sprints. An ambulance was called for another player immediately after practice, and a third player later went to the hospital. The second player was discharged, and the third player was kept overnight for observation. |
| EHS | Practice lasted 3.5 hours and ended with 16 sprints. Signs and symptoms were missed, and the athlete collapsed after practice. |
| EHS | 200-yard sprints after weight-training session. Coaches forced players who did not complete the sprints in less than 45 seconds to run additional sprints. Practice was called “voluntary,” but failure to participate yielded additional more extreme exercises or being cut from the team. |
| EHS | Running wind sprints. The athlete asked another player to help him up so that he could “finish his last sprint.” |
| EHS | Punishment drills for poor practice: 12 consecutive 220-yd sprints in 94°F heat with helmets and pads. The coach repetitively said, “We’re going to run till somebody quits.” The athlete was “struggling and went down to one knee.” The coach told a player to “help him up so he could finish his last sprint.” Another player collapsed 15 minutes before the deceased athlete but recovered after 2 days in the hospital.24 |
| EHS | Punishment run, wearing full pads, at 5:45 AM for players who missed other preseason practices. |
| EHS | Second practice of first day. The coach withheld water breaks as punishment. The player was vomiting during practice. He was found incoherent in the shower after practice, surrounded by ice packs, having been placed there by coaches. |
| EHS | 3-day conditioning camp. The player was vomiting during the first practice. He collapsed during the second practice after a 1.5-mile run. |
| EHS | Punishment drills: wind sprints after showing up late for practice. |
| EHS | Thirty-six 50-yard sprints. The athlete was denied water. Up to 6 teammates said that he struggled in the sprints, 2 said he took a knee, and all agreed that the head coach loudly berated him. |
| SCA | Punishment practice for poor performance in a scrimmage the day before: strenuous physical exertion of repetitive gassers. |
| SCA | Second practice of the day. The athlete had symptoms since the first practice and worsened during the second practice, with loss of balance. He could not respond to questions and was sent to the sidelines, unsupervised for 45 minutes. He was coerced to continue drills, and the coach pushed him and called him names. He complained of dizziness and chest pain, collapsed, and began having a seizure. |
| SCA | A walk-on athlete collapsed during indoor noncontact drills. He reported to the coach that he was not feeling well and asked to be excused. The coach challenged him to participate and replied, “Either practice or get your (expletive) out of here and don’t return.” |
| SCA | Punishment drill for throwing helmet. The athlete collapsed near the end of a 2-mile run while sprinting on the straightaway. |
| SCA | Sprint drills. |
| SCA | The player collapsed while running laps. A malignant environment was reported. After the player collapsed, one coach yelled at him and grabbed him by the shirt; another coach grabbed him by the waistline of his pants, picked him up, and then dropped him. |
| SCA | The athlete collapsed after sprints at the end of practice. Coaches yelled at him to continue when he was struggling. |
| SCA | Practice with full pads as punishment for poor performance in a scrimmage the day before. The athlete collapsed during a strenuous conditioning drill including sprints. |
aECAST, exertional collapse associated with SCT; EHS, exertional heat stroke; NCAA, National Collegiate Athletic Association; PPE, preparticipation physical examination; SCA, sudden cardiac arrest; SCT, sickle cell trait.
APPENDIX 2
Case Examplesa
Case Report 1
EHS. The athlete was a 19-year-old, 6-ft 4-inch, 290-lb (BMI, 35.3 kg/m2), African American, NCAA Division I, sophomore offensive lineman. The day-1 summer out-of-season session, planned and supervised by the S&C coach, commenced with the head coach present. The temperature at the onset of the conditioning session, consisting of ten 110-yd sprints, was 80°F. Hydration was a priority. Every player had a gallon of water in his locker, of which the athlete drank none. As the prescribed sprinting drills concluded, the athlete was visibly struggling to meet performance expectations. Videotape revealed that teammates assisted him to finish the exercise. After expletives were hurled at the player by the staff, the athlete, who was hyperventilating and cramping, was walked in the opposite direction of the athletic training facility by 2 ATs to perform position drills.25 At 34 minutes after the onset of symptoms, he was removed from the field by ATs. In the athletic training facility, cool towels were applied. The core temperature was not obtained, and ice bath immersion was not employed.25 Once mental status changes manifested, an AT called the team physician instead of 911. At 45 minutes after the onset of symptoms, 911 was called.25 At some disputed point between the onset of symptoms and the arrival of the emergency medical technicians, the athlete had a seizure. Emergency medical services identified the player as unconscious and transported him to a local hospital. He was subsequently transferred to a regional trauma center. At 2 hours after the onset of symptoms, his core body temperature was recorded to be 106°F. Rapid cooling reduced his temperature to 102°F in 15 minutes. The player subsequently received a liver transplant. Never regaining consciousness, he died 2 weeks later secondary to complications from EHS.
According to the independent investigation, with interviews of 165 people and a review of thousands of documents, the coach was “effectively accountable to no one, and the training staff went relatively unsupervised for extended periods of time.”4 There was an abusive coaching environment based on fear, intimidation, humiliation, and embarrassment led by the S&C coach and supported by the head football coach.22 The report revealed that the S&C coach attempted to humiliate players in front of teammates by throwing weights, food, and on 1 occasion a trash can full of vomit.4 Other bullying incidents by the S&C coach included choking a player with a weight bar, belittling a player who was having problems breathing during a practice session, and moving an injured player’s locker to the showers. Extreme verbal abuse of players was commonplace. The degrading of players and hurling of obscenity-laced epithets and homophobic slurs were thought to “toughen up the players.” Players were also threatened with loss of their scholarships if they could not complete a conditioning session. One player was verbally belittled despite passing out during a drill. The coaches endorsed unhealthy eating habits and used food punitively; a player claimed that he was forced to overeat to the point of vomiting.
Case Report 2
ES With SCT. The athlete was a 21-year-old, African American, NCAA Division I linebacker/defensive lineman, known to be SCT positive, who died during an out-of-season early morning football conditioning drill in February 2014. The player, head AT, and head S&C coach all had knowledge of the athlete’s SCT status and were provided targeted education for the condition. The S&C coach attested that players with SCT are conditioned identically to all other players with no modifications unless signs and symptoms are observed and then there would be an intervention. The team physician’s precaution allowed for a player with SCT to set his own pace in the drill.
The day’s workout, designed and overseen by the S&C coach, was highlighted by a 10-repetition rope drill.32 The players sprinted, in groups, up a steep hill while holding a rope, with the entirety of the group in forced exertion at the same pace. It was a competition, pitting group against group, with the goal to finish the hill and arrive at the stadium as fast as possible. “Rest” was accounted as occurring during the jog downhill, before the next uphill sprint. According to a deposition from a teammate,32 the drill’s purpose was to instill “toughness.” Players rated it as the hardest, or among the hardest, workout that they had ever endured.
The head AT was present but unable to view the players on the hill because of the distance and darkness. According to teammates, at least 2 other linemen, in addition to the athlete, collapsed. One fell, rolled several times, and lay with a blank face “like a boxer knocked out.” No AT presented to assess. After eventual completion of the drill, with teammates assisting him, the player stumbled to the stadium with no memory of what had just happened.
The athlete led his group for 5.5 laps, at which point he started to struggle (look “ghostly”) and dropped out of the lead. Over the next few laps, he started to decompensate and was reported by teammates to be dazed and confused. By the 9th lap, he collapsed for 20 seconds. His group helped him upright so that they could finish the competition. Meanwhile, the coaching staff urged the players to continue, while the AT watched the drill and failed to intervene. At the beginning of the 10th repetition, he collapsed again and went limp. The players in his group tied the rope around the athlete, and 2 teammates supported him to finish the drill. Struggling to breathe, his legs and arms so dead that they had difficulty holding him up, they dragged him forward as he kept slipping through their arms.
By the end of the 10th and final repetition, the athlete collapsed for a third time. It was at this point that care was initiated. Signs and symptoms mirrored ES in an athlete known to have SCT. Initial efforts were focused on hydration; there was no oxygen or AED on site. As he became obtunded, he was transported emergently to the hospital, where he died at 7:52 AM the morning of his collapse. Based on teammate depositions,33 the S&C coach was renowned for a culture of hypermachismo and massive punishment drills at 5 AM for poor player performance and violation of team rules, among others. In a punitive session 3 months before this case report, because of 1 player being absent from a workout, the S&C coach doubled the attending players’ drills to the point where several were vomiting.
aAED, automated external defibrillator; AT, athletic trainer; BMI, body mass index; EHS, exertional heat stroke; ES exertional sickling; NCAA, National Collegiate Athletic Association; SCT, sickle cell trait; S&C, strength and conditioning.
Footnotes
Final revision submitted April 2, 2020; accepted April 23, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: K.M.F. has received consulting fees from Flexion Therapeutics. AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the University of Oklahoma.
References
- 1. Adams WM, Casa DJ, Drezner JA. Sport safety policy changes: saving lives and protecting athletes. J Athl Train. 2016;51(4):358–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson S. NCAA football off-season training: unanswered prayers…a prayer answered. J Athl Train. 2017;52(2):145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anderson SA. The Junction Boys syndrome. J Strength Cond Res. 2012;26(5):1179–1180. [DOI] [PubMed] [Google Scholar]
- 4. Azar FM, Bernstein BL, Ehrlich RL, Jr, et al. Report to the university system of Maryland of an independent investigation of the University of Maryland football program. 2018. https://a.espncdn.com/pdf/2018/1025/MarylandReport.pdf. Accessed October 20, 2018.
- 5. Becker JM, Rogers J, Rossini G, Mirchandani H, D’Alonzo GE., Jr Asthma deaths during sports: report of a 7-year experience. J Allergy Clin Immunol. 2004;113(2):264–267. [DOI] [PubMed] [Google Scholar]
- 6. Boden BP, Breit I, Beachler JA, Williams A, Mueller FO. Fatalities in high school and college football players. Am J Sports Med. 2013;41(5):1108–1116. [DOI] [PubMed] [Google Scholar]
- 7. Boden BP, Fine KM, Breit I, Lentz W, Anderson SA. Nontraumatic exertional fatalities in football players, part 1: epidemiology and effectiveness of NCAA rule changes. Orthop J Sports Med. 2020;8(8):2325967120942490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Casa DJ, Almquist J, Anderson SA, et al. The inter-association task force for preventing sudden death in secondary school athletics programs: best-practices recommendations. J Athl Train. 2013;48(4):546–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Casa DJ, Anderson SA, Baker L, et al. The inter-association task force for preventing sudden death in collegiate conditioning sessions: best practices recommendations. J Athl Train. 2012;47(4):477–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Casa DJ, Csillan D, Armstrong LE, et al. Preseason heat-acclimatization guidelines for secondary school athletics. J Athl Train. 2009;44(3):332–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Courson R, Goldenberg M, Adams KG, et al. Inter-association consensus statement on best practices for sports medicine management for secondary schools and colleges. J Athl Train. 2014;49(1):128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Drezner JA, Toresdahl BG, Rao AL, Huszti E, Harmon KG. Outcomes from sudden cardiac arrest in US high schools: a 2-year prospective study from the National Registry for AED Use in Sports. Br J Sports Med. 2013;47(18):1179–1183. [DOI] [PubMed] [Google Scholar]
- 13. Durell DL, Pujol TJ, Barnes JT. A survey of the scientific data and training methods utilized by collegiate strength and conditioning coaches. J Strength Cond Res. 2003;17(2):368–373. [DOI] [PubMed] [Google Scholar]
- 14. Eichner ER. Sickle cell trait in sports. Curr Sports Med Rep. 2010;9(6):347–351. [DOI] [PubMed] [Google Scholar]
- 15. Eichner ER. Preventing exertional sickling deaths: the right way, the wrong way, and the Army way. Curr Sports Med Rep. 2013;12(6):352–353. [DOI] [PubMed] [Google Scholar]
- 16. Eichner ER. “A stitch in time” and “if 6 was 9”: preventing exertional sickling deaths and probing team rhabdomyolysis outbreaks. Curr Sports Med Rep. 2016;15(3):122–123. [DOI] [PubMed] [Google Scholar]
- 17. Eichner ER. Football team rhabdomyolysis: the pain beats the gain and the coach is to blame. Curr Sports Med Rep. 2018;17(5):142–143. [DOI] [PubMed] [Google Scholar]
- 18. Epstein Y, Moran DS, Shapiro Y, Sohar E, Shemer J. Exertional heat stroke: a case series. Med Sci Sports Exerc. 1999;31(2):224–228. [DOI] [PubMed] [Google Scholar]
- 19. Grundstein AJ, Hosokawa Y, Casa DJ. Fatal exertional heat stroke and American football players: the need for regional heat-safety guidelines. J Athl Train. 2018;53(1):43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hoffman JR. The applied physiology of American football. Int J Sports Physiol Perform. 2008;3(3):387–392. [DOI] [PubMed] [Google Scholar]
- 21. Huggins RA, Scarneo SE, Casa DJ, et al. The inter-association task force document on emergency health and safety: best-practice recommendations for youth sports leagues. J Athl Train. 2017;52(4):384–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jenkins S. Culture didn’t kill Jordan McNair. Negligence did. DJ Durkin is responsible for both. Washington Post. October 1, 2018. [Google Scholar]
- 23. Kucera K, Klossner D, Colgate B, Cantu R. Annual survey of football injury research, 1931-2017. https://nccsir.unc.edu/files/2019/02/Annual-Football-2018-Fatalities-FINAL.pdf. Accessed November 10, 2018.
- 24. Lake T. The boy who died of football. Sports Illustrated. 2010;113(21):130–142. [Google Scholar]
- 25. Maese R, Dougherty J, Giambalvo E. Maryland says football staff made mistakes treating player before his death, apologizes to family. Washington Post. August 14, 2018. [Google Scholar]
- 26. Mariotti J. The tragic cost of pride. The Sporting News. August 13, 2001. Accessed February 4, 2019.
- 27. Maron BJ. Sudden death in young athletes. N Engl J Med. 2003;349(11):1064–1075. [DOI] [PubMed] [Google Scholar]
- 28. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8):1085–1092. [DOI] [PubMed] [Google Scholar]
- 29. Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes: clinical, demographic, and pathological profiles. JAMA. 1996;276(3):199–204. [PubMed] [Google Scholar]
- 30. McDermott BP, Anderson SA, Armstrong LE, et al. National Athletic Trainers’ Association position statement: fluid replacement for the physically active. J Athl Train. 2017;52(9):877–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McGrew CA. NCAA football and conditioning drills. Curr Sports Med Rep. 2010;9(4):185–186. [DOI] [PubMed] [Google Scholar]
- 32. Muchnick I. Ted Agu Papers. Close friend describes multiple collapses during fatal drill “like an army movie”; Coach Harrington’s taunt “Berkeley was making us soft”; transfer in disgust after Cal lied to players. http://concussioninc.net/?s=Ted+Agu+Papers%3A+Close+Friend+Describes&x=0&y=0. Accessed October 13, 2018.
- 33. Muchnick I. Ted Agu Papers. Player describes Cal Football Strength Coach Damon Harrington’s “punishment drills” and “swagger games,” obsession with “down south mental toughness”. http://concussioninc.net/?s=Ted+Agu+Papers%3A+Player+Describes&x=0&y=0. Accessed October 13, 2018.
- 34. National Climatic Data Center. NOAA satellite and information service. https://www.ncdc.noaa.gov/cdo-web/datatools/lcd. Accessed October 28, 2018.
- 35. National Collegiate Athletic Association. 2014-15 NCAA Sports Medicine Handbook. 25th ed NCAA; 2014:97–102. [Google Scholar]
- 36. National Collegiate Athletic Association. NCAA Division I Manual. Bylaw 13.11.3.7.3: Mandatory Medical Examination. NCAA; 2018. [Google Scholar]
- 37. National Collegiate Athletic Association. NCAA Division I Manual. NCAA Bylaw: DI 3.2.4.17 Independent Medical Care (Effective 2016), DII 3.3.4.17, and DIII 3.2.4.19 (Adopted 1/21/17; Effective 8/1/17). NCAA; 2018. [Google Scholar]
- 38. NCAA Sport Science Institute. Interassociation consensus: independent medical care for college student-athletes best practices. https://www.ncaa.org/sites/default/files/2017SSI_IndependentMedicalCare_20170626.pdf. Accessed February 22, 2019.
- 39. Parsons JT, Anderson SA, Casa DJ, Hainline B. Preventing catastrophic injury and death in collegiate athletes: interassociation recommendations endorsed by 13 medical and sports medicine organisations. Br J Sports Med. 2020;54(4):208–215. [DOI] [PubMed] [Google Scholar]
- 40. Pincivero DM, Bompa TO. A physiological review of American football. Sports Med. 1997;23(4):247–260. [DOI] [PubMed] [Google Scholar]
- 41. Rav-Acha M, Hadad E, Epstein Y, Heled Y, Moran DS. Fatal exertional heat stroke: a case series. Am J Med Sci. 2004;328(2):84–87. [DOI] [PubMed] [Google Scholar]
- 42. Smith G. Soul survivor. Sports Illustrated. 2002;97(22):64–80. [Google Scholar]
- 43. Taylor C, Kavanagh P, Zuckerman B. Sickle cell trait: neglected opportunities in the era of genomic medicine. JAMA. 2014;311(15):1495–1496. [DOI] [PubMed] [Google Scholar]