Abstract
Background
Recurrent aphthous stomatitis (RAS) is a highly prevalent oral mucosal disease. The management of RAS is quite challenging, and as yet, there is no definitive cure. The present systematic review and meta-analysis assessed the efficacy of a single application of topical doxycycline for the management of RAS.
Methods
A comprehensive online search of PubMed, Scopus, Embase, and Web of Science databases was conducted to identify all relevant studies published up to March 31, 2019. All randomized clinical trials that assessed the efficacy of a single application of topical doxycycline in the management of RAS were included. Primary outcome measures were pain scores and/or healing time, while secondary outcomes included the associated side effects. RevMan 5.3 software was used for data analysis.
Results
Five clinical trials fulfilled the eligibility criteria, three of which were included in the meta-analysis. All of the included studies found doxycycline effective in alleviating signs and symptoms of RAS. The results of the pooled 3 studies revealed a statistically significant decrease in the healing time in favor of the doxycycline group as compared to the control groups (I2 = 51%; MD: -1.77, 95% CI: − 2.11, − 1.42, P <0.00001); however, the results showed no significant differences between doxycycline and control groups with regard to pain reduction (I2 = 96%; MD: -1.28, 95% CI: − 2.83, 0.27; P = 0.11).
Conclusion
Although still inconclusive, the available evidence suggests that a single application of topical doxycycline might be effective for reducing signs and symptoms of RAS. However, owing to the limited number of the included studies, further well-designed clinical trials with adequate sample sizes are required to discern the clinical efficacy of topical doxycycline in patients with RAS.
Keywords: Recurrent aphthous stomatitis, Single application, Topical doxycycline, Efficacy
Background
Recurrent aphthous stomatitis (RAS) - also known as recurrent aphthous ulcer, canker sores, and aphthous ulcer- is the most common oral mucosal disease, affecting approximately 5 to 25% of the general population [1, 2]. RAS is characterized by recurring painful ulcers confined mostly to the non-keratinized oral mucosa. Clinically, RAS presents as one of the three forms: minor, major and herpetiform [2]. The minor form is the most common type (comprising 85% of all RAS), and presents clinically as a painful round or oval ulcer of less than 1 cm in dimension, with a gray–white pseudomembrane that is surrounded by an erythematous halo [2–4]. The lesions usually heal spontaneously within 7–10 days without scarring [2–4]. Most affected patients usually develop more than one ulcer in each episode, and experience several episodes annually [2] Despite the high prevalence, and the extensive research on RAS, its etiology is still unclear; instead, a number of predisposing factors have been proposed including, but not limited to, genetic predilection, hematologic factors, immunologic defects, vitamins deficiencies, emotional stress, and local trauma [2, 3, 5–9].
Aside from being a self-limiting disease, RAS can cause severe pain, distress, and difficulty in eating and speaking that adversely affects the patients’ quality of life, especially in patients with high frequency of recurrent attacks [3, 4]. Certainly, owing to the unclear etiology, the management of RAS is quite challenging and as yet there is no specific therapy [10]. Indeed, the primary goal of RAS therapy is to reduce pain, accelerate healing, and reduce the frequency of recurrences. Many medications have been proposed to achieve the above mentioned goals; these include topical corticosteroids, antiseptic mouthwashes, anesthetics, analgesics, and antibiotics [3, 10, 11]. In severe cases of RAS like major ulcers and/or high frequent annuals attacks, systemic immunomodulatory medications such as systemic corticosteroids, colchicine, azathioprine, dapsone and pentoxifylline are used [2, 10]. Unfortunately, however, these medications can result in numerous adverse effects limiting their use [3, 10].
Tetracyclines have long been used for the management of RAS [11–13]. In addition to their antibacterial properties, these agents have anti-collagenase and anti-inflammatory effects, explaining their therapeutic action in the treatment of RAS [14, 15]. Doxycycline, a newer semisynthetic tetracycline, has been reported to have more potent anti-inflammatory and anti-collagenase properties than other tertracyclines [12–14]. More specifically, it effectively suppresses prostaglandin production and leukocytes activities; inhibits the gelatinolytic effects of collagenases; and downregulates the Matrix Metalloproteinase Collagenase (MMP)-an interstitial collagenase which is thought to play an important role in tissue destruction events in RAS [13, 14]. A recent systematic review has addressed the effects of systemic and topical doxycycline in the management of oral ulcerative lesions, and has found a significant improvement in the signs and symptoms associated with these lesions [16]. In context of the efficacy of a single application of topical doxycycline for the treatment of RAS, a number of clinical trials showed conflicting results [4, 13, 17–19]. However, no attempt has been made so far to systematically review and/or meta-analyze the available evidence in this regard. Therefore, this systematic review and meta-analysis aimed to evaluate the available evidence regarding the safety and clinical efficacy of a single application of topical doxycycline in the management of RAS.
Methods
Research question
The present systematic review was conducted following the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines and according to the Participants, Interventions, Control, and Outcomes (PICO) principles [20]. The protocol of the present systematic review was registered at PROSPERO (ID: CRD42019128974). The addressed research question was: “Is a single application of topical doxycycline effective in the management of RAS?”
Eligibility criteria
The studies were selected according to the following PICOS components as follows:
Participants (P): Healthy individuals aged 15 years and above, diagnosed with RAS.
Intervention (I): Single dose of topical doxycycline.
Comparator (C): Any medical interventions or placebo controls.
Outcomes (O): The primary outcomes included reduction of pain and/or healing time. The secondary outcomes included: 1) side effects of the intervention and 2) adhesive retention time.
Study design (S): Randomized control trials (RCTs) and controlled clinical trials.
Uncontrolled clinical trials, case series, case reports, animal studies, review papers, editorials, letters to the editor, commentary and monographs were excluded.
Search strategy
A literature search of PubMed/MEDLINE, Embase, Scopus, and Web of science was conducted in April, 2019 to identify all relevant studies published up to 31 March 2019, using various combinations of the following keywords: doxycycline, aphthous stomatitis, recurrent aphthous stomatitis, recurrent aphthous ulcers, recurrent oral ulcers, and canker sores. The reference lists of the selected articles were also hand-searched for additional studies. Titles and abstract of all identified articles were screened by two independent co-authors (SA and NMQ), and irrelevant studies were excluded. Full-texts of the potentially relevant studies were obtained and thoroughly evaluated by the two authors; disagreements, if any, were resolved via consensus.
Quality assessment
Two independent co-authors (SA and NMQ) evaluated the methodological quality and the risk of bias of each included study according to the revised recommendation of the CONSORT statement tool [21]. Based on six domains (sample size estimation, randomization, blinding of participants and personnel, inclusion/exclusion criteria, comparable baseline values, completeness of follow-up, and statistical analyses), the overall estimation risk of bias was calculated for each selected study, and rated as follows: low, all criteria met; moderate, one or more criteria partly met; or high, one or more criteria were not met.
Data extraction
For each study the following data were extracted: authors, year and country of the study, study design, types of interventions, and description of the participants (sample size, mean age, and gender), follow-up period, clinical variables (pain and healing time and side effects), drugs formulation, and the main outcomes. For meta-analyses, the means and standard deviations of the parameters of interests (primary outcomes) were extracted.
Statistical analysis
Statistical analysis was performed using Review Manager (RevMan) Version 5.3. Copenhagen: The Nordic Cochrane Centre, the Cochrane Collaboration, 2014. The meta-analysis was conducted by measuring the mean difference between the groups along with 95% confidence intervals (CI). A P- value < 0.05 was considered statistically significant. Heterogeneity was evaluated using Chi-square test and the I2 statistics. Fixed-effects model was used for low/moderate heterogeneity while random effect model was applied for significant heterogeneity (P < 0.10 and I2 was higher than 50%).
Results
Study selection
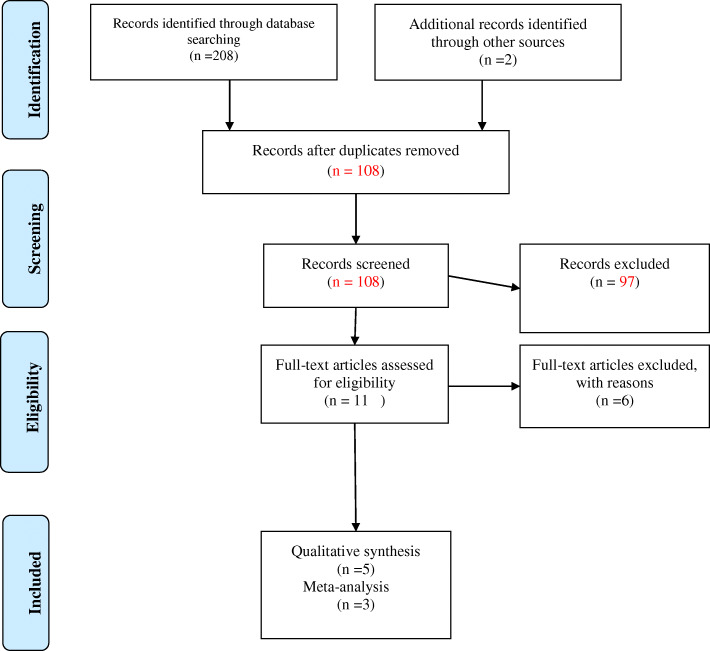
Online search yielded a total of 208 studies. Two additional studies were identified through hand-search, summing up to a total of 210 articles (Fig. 1). After duplicates removal (102 articles), 108 publications remained. After screening the titles and abstracts, 97 studies were found to be irrelevant, and were thus excluded. A full-text review was conducted on the remaining 11 studies, and 6 were excluded for various reasons: two used multiple doses of doxycycline [12, 15]; two were letters to the editor [22, 23]; one was in-vitro study [14]; and one [24] was a conference abstract. The remaining five studies [4, 13, 17–19] fulfilled the eligibility criteria and were further processed for data extraction. Of these, only three studies [4, 17, 19] were eligible for the meta-analysis (Fig. 1).
Fig. 1.
Flow-chart of methodology according to PRISMA guidelines
General characteristics of the included studies
Five randomized clinical trials (RCT) comprising 201 patients (86 in the intervention group and 115 controls) were included [4, 13, 17–19]. Four studies were conducted in India [4, 17–19] and one was in Finland [13]. Number of subjects ranged from 30 to 50 subjects, with mean ages ranging from 15 to 64 years. The follow-up period ranged from 7 to 10 days (Table 1). All studies included patients with minor RAS. Diagnosis of RAS was based on clinical features and history of recurrent minor ulcers. The duration of RAS at the time of recruitment was reported by three studies [4, 18, 19], which ranged between 10 h and 72 h. However, no information was given about RAS duration (before intervention) by the other two studies [13, 17].
Table 1.
General characteristics of the included studies
| Author (year) | Country | Intervention | Controls | Sample size test/control | Gender | Mean age (range) |
Type of RAS | Follow-up(days) |
|---|---|---|---|---|---|---|---|---|
| Sharma et al (2018) [18] | India | Topical Doxycycline |
G1: 5% Amlexanox; G2: 0.1% Triamcinolone acetonide G3: Benzocaine gel G4: placebo gel |
10/40 | 50% | 26.5 | Minor | 10 |
| Thriveni et al, (2018) [17] | India | Topical Doxycycline | Placebo 100 mg (starch, lactose, sodium starch glycolate, talc, magnesium stearate) | 20/20 | NA | NA | Minor | 10 |
| Chandak et al, (2017) [19] | India | Topical Doxycycline | 0.1% triamcinolone acetonide paste | 15/15 |
M = 14 F = 16 |
15–40 | Minor | 7 |
| Vijayabala et al. (2013) [4] | India | Topical Doxycycline | Placebo 100 mg (starch, lactose, sodium starch glycolate, talc, magnesium stearate) | 25/25 |
M = 30 F = 20 |
25.14 | Minor | 10 |
| Ylikontiola (1997) [13] | Finland | Topical Doxycycline | Placebo (calcii gluconase) | 16/15 |
M = 4 F = 27 |
23–63 | Minor | 10 |
F Female, M Male, NA Not Available
Intervention and control groups
In all included studies, a single dose of topical doxycycline was applied. The efficacy of doxycycline was compared with placebo in three studies [4, 13, 17]; 0.1% triamcinolone acetonide in one study [19]; and with four control groups in one study [18]: 5% amlexanox, 0.1% triamcinolone acetonide, 20% Benzocaine gel, and placebo gel (Table 2).
Table 2.
Drug formulation and the main outcomes of the included studies
| Study | Formulation and dose | Outcome measures | Adverse effects |
Main outcomes |
|---|---|---|---|---|
| Sharma et al (2018) [18] | Topical, Doxycycline Hyclate 100 mg was crushed and mixed with denture adhesive and saline |
Pain Size of the ulcer Erythema |
None | On day 4, Doxycycline and Triamcinolone acetonide groups showed better efficacy in reducing pain and ulcer size compared to other groups, but without any significant differences between the two groups. |
| Thriveni et al, (2018) [17] | Topical, Doxycycline Hyclate 100 mg was crushed and mixed with denture adhesive and saline |
Pain Healing time |
NA | Doxycycline hyclate showed a significant reduction in pain at follow-up visits as compared to placebo group (P < 0.001). |
| Chandak et al, (2017) [19] | Topical, Doxycycline Hyclate 100 mg was crushed and mixed with denture adhesive and saline |
Pain Healing time |
None |
Healing of the ulcer was significantly faster in doxycycline group compared to triamcinolone ointment (P < 0.01). However, there was no a significant difference in pain reduction between the two groups (P > 0.05). |
| Vijayabala et al. (2013) [4] | Topical, Doxycycline Hyclate 100 mg was crushed and mixed with denture adhesive and saline |
pain Healing time |
8 patients reported transient bitter taste | A single application of doxycycline hyclate was significantly more effective in alleviating pain and reducing healing time as compared to placebo group (P < 0.001) |
| Ylikontiola (1997) [13] | Doxycycline 150 mg was crushed and mixed with saline. One drop of isobutyl cyanoacrylate as adhesive | Pain | NA | A significant reduction in pain in doxycycline group from day 2 to day 7 as compared to control group (P < 0.05). |
NA Not Available
Formulations and dose
Four studies [4, 17–19] used 100 mg Doxycycline Hyclate and one study [13] used 150 mg Doxycycline. In all included studies, doxycycline was crushed and mixed with saline. For retention of the remedy, four studies [4, 17–19] used denture adhesive while one study [13] used isobutyl cyanoacrylate (Table 2).
Outcome measurements
All included studies [4, 13, 17–19] evaluated the efficacy of Doxycycline in reducing pain using the Visual Analog Scale (VAS). Three studies evaluated the healing time [4, 17, 19], and only one study evaluated the ulcer size [18].
Results
Qualitative results
All included studies found single application of doxycycline to be effective in reducing signs and symptoms of RAS [4, 13, 17–19].
Reduction of pain
All the included studies reported on this outcome; three studies [4, 13, 17] reported a significant reduction of pain with doxycycline intervention compared to placebo. Two studies [18, 19] found doxycycline as effective as 0.1% triamcinolone acetonide in reducing pain (Table 2).
Healing time
Three studies reported on this outcome [4, 17, 19], and revealed a significant decrease in the healing time with doxycycline intervention compared to the control comparators (placebo in two studies and 0.1% triamcinolone acetonide in one study).
Adverse effects and adhesive retention time
Four studies [4, 17–19] reported on the adverse effects. Three studies [17–19] did not find any side effects; one study [4] reported that 8 patients in doxycycline group suffered a transient bitter taste, but no side effects were reported among the placebo group. One study did not provide any information about the side effects [13]. With regards to the mean adhesive retention time, only two studies reported on this outcome, and ranged from 2.1 to 3.5 h [4, 13].
Meta-analysis results
Only 3 studies were eligible for the meta-analysis [4, 17, 19]. The remaining two studies [13, 18] were excluded from the statistical analysis because of data unavailability. We confirm that we contacted the authors many times requesting the missing data, but unfortunately they failed to supply the necessary data.
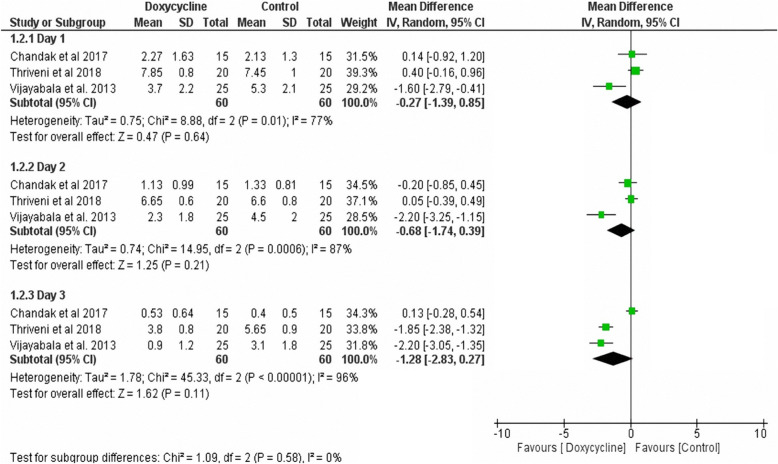
Reduction of pain
The pooled data of the three trials [4, 17, 19] showed no significant differences in pain reduction between doxycycline intervention and the comparator interventions at day 1. At day 2 and 3, doxycycline showed better results, but again the differences were not statistically significant (Fig. 2).
Fig. 2.
Meta-analysis of pain scores
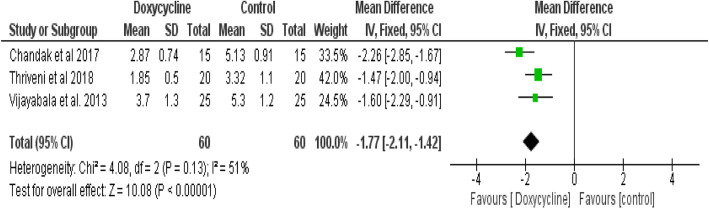
Healing time
The pooled data of three trials [4, 17, 19] showed statistically significant less healing time in favour of Doxycycline intervention compared to the control interventions (I2 = 51%; mean difference (MD): -1.77, 95% CI: − 2.11, − 1.42, P <0.00001) (Fig. 3).
Fig. 3.
Meta-analysis of healing time
Quality of the included studies
A summary of the risk of bias for the included studies is presented in Table 3. Three studies [13, 17, 19] showed a high risk of bias, and only two studies [4, 18] showed a moderate risk of bias. The most common methodological insufficiencies were: lack of sample size calculation, improper randomization, and absence of/inadequate blinding (Table 3).
Table 3.
CONSORT-based quality analysis of the included studies
| Study | Sample size (0–2) |
Randomization (0–2) | Inclusion/ exclusion criteria (0–1) |
Follow up (0–1) |
Baseline (0–2) |
Masking (0–2) |
Statistical analysis (0–2) | score | Total Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|
| Sharma et al. (2018) [18] | 1 | 2 | 1 | 1 | 2 | 2 | 2 | 11 | moderate |
| Thriveni et al, (2018) [17] | 0 | 1 | 1 | 0 | 2 | 1 | 2 | 8 | High |
| Chandak et al, (2017) [19] | 0 | 1 | 1 | 0 | 2 | 0 | 1 | 6 | High |
| Vijayabala et al. (2013) [4] | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 9 | moderate |
| Ylikontiola et al. (1997) [13] | 0 | 1 | 1 | 1 | 2 | 1 | 2 | 10 | high |
Discussion
A number of clinical trials have investigated the efficacy of a single application of topical doxycycline in comparison to other treatment modalities in reducing signs and symptoms of RAS [4, 17, 19]. Therefore, the present systematic review was conducted to summarize the available evidence regarding the clinical efficacy of a single application of topical doxycycline for the management of RAS.
Overall, the qualitative analysis of all included studies showed that a single application of topical Doxycycline is effective in reducing pain and accelerating the healing time. Additionally, the meta- analysis results revealed a significant decrease in the healing time in favor of the Doxycycline group. Nevertheless, the results showed an insignificant difference between doxycycline and control groups with regard to pain reduction. Generally, the results of this review should be read with caution, given the limitations highlighted at the end of this section.
The main outcomes assessed in this review were reduction of pain and healing time of the ulcers. RAS can cause severe pain and distress that can severely impact patients’ quality of life [3]. All of the included studies assessed the efficacy of doxycycline in pain reduction using VAS, a well-known and very reliable tool for subjective assessment of pain. The results showed that doxycycline was superior to placebo but comparable to corticosteroids in reducing pain. The significant reduction in pain immediately after the treatment (starting day one after treatment) suggests a quick and potent analgesic action of topical doxycycline in patients with RAS. In line with that, the pooled data results have showed superiority of doxycycline in reducing the time required for ulcer healing. The mechanism behind the efficacy of doxycycline in reducing pain and shortening the ulcers healing time can be explained largely by its nonmicrobial properties- potent anti-inflammatory and anti-collagenase properties- in addition to its antimicrobial properties [14, 15]. Doxycycline has been shown to inhibit prostaglandin production, suppress leukocytes and inhibit MMP, thus promoting healing of the ulcer with subsequent reduction in pain [11, 13–15]. The results of the present review corroborates previous studies that found that subantimicrobial doses of systemic or topical doxycycline is highly effective in reducing pain, duration and frequency of RAS [12, 15].
One important aspect of RAS management is related to the side effects of the therapeutic agents, especially corticosteroid, the most commonly used agents. Long term use of corticosteroids, topically or systemically, is associated with serious complications like mucosal thinning, secondary candida infections, and adrenal insufficiencies, among others [3, 10, 25]. The present review revealed that the topical use of doxycycline was safe and well-tolerated by the patients without any serious adverse effects. Another important drawback of the current RAS therapeutic modalities is related to the patients’ compliance, particularly in patients with long-standing and highly frequent episodes, where the patient needs to apply the medication multiple times daily for several days. It is worth mentioning here that the single application of topical doxycycline is highly advantageous in this regard compared to other medications, resulting in a better compliance and satisfaction. In addition to the side effects and patients’ compliance, the cost of treatment is another limitation of the current therapies, especially in patients with a low socioeconomic background. Hence, a safe, efficacious, and cost- effective remedy like topical doxycycline can be considered as a good therapeutic candidate for RAS.
The present systematic review, the first of its kind, has shown promising effects of a single application of topical doxycycline in the management of RAS. However, this review has certain limitations that should be taken into account. The first limitation is related to the limited number of the included studies, and the considerable heterogeneity among the included studies with respect to the comparator group, outcome measures, duration of the ulcers, and the age of the patients. Another important limitation is related to the poor quality of the included studies reflected by the high risk of bias due to the inadequate blinding, improper randomisation and/or small sample sizes. Additionally, the short follow-up period is an obvious shortcoming of the included studies, and thus no attempt was made to assess the efficacy of doxycycline on the recurrence rate of the episodes. Therefore, further high-quality clinical trials with large sample sizes and adequate follow-up periods are required to discern the efficacy of a single application of topical doxycycline for treating RAS.
Conclusions
Within the limitations of the available evidence drawn from the current systematic review and meta-analysis, we can conclude that a single application of topical doxycycline has a promising effect in reducing pain and accelerating healing time in patients with RAS. However, given the limited number of the included studies and low quality of these studies, further well-designed multicenter RCTs are highly warranted.
Acknowledgements
Not applicable.
Abbreviations
- RAS
Recurrent Aphthous Stomatitis
- RCTs
Randomized Clinical Trials
- VAS
Visual Analog Scale
- MD
Mean Difference
- MMP
Matrix MetalloProteinase
Authors’ contributions
SAA and ES participated in designing the study, interpretation of the data and drafting the manuscript. SA, NMQ and AYA participated in extraction of the data and statistical analysis. KY and MNA participated in data collection and drafting the manuscript. All authors read and approved the final manuscript.
Funding
No funding.
Availability of data and materials
The datasets supporting the findings of this article are available from the corresponding author.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ship JA, Chavez EM, Doerr PA, Henson BS, Sarmadi M. Recurrent aphthous stomatitis. Quintessence Int. 2000;31(2):95–112. [PubMed] [Google Scholar]
- 2.Tarakji B, Gazal G, Al-Maweri SA, Azzeghaiby SN, Alaizari N. Guideline for the diagnosis and treatment of recurrent aphthous stomatitis for dental practitioners. J Int Oral Health. 2015;7(5):74–80. [PMC free article] [PubMed] [Google Scholar]
- 3.Saikaly SK, Saikaly TS, Saikaly LE. Recurrent aphthous ulceration: a review of potential causes and novel treatments. J Dermatolog Treat. 2018;29(6):542–552. doi: 10.1080/09546634.2017.1422079. [DOI] [PubMed] [Google Scholar]
- 4.Vijayabala GS, Kalappanavar AN, Annigeri RG, Sudarshan R, Shettar SS. Single application of topical doxycycline hyclate in the management of recurrent aphthous stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(4):440–446. doi: 10.1016/j.oooo.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Bao ZX, Shi J, Yang XW, Liu LX. Hematinic de fi ciencies in patients with recurrent aphthous stomatitis: variations by gender and age. Med Oral Patol Oral Cir Bucal. 2018;23(2):e161–e167. doi: 10.4317/medoral.21885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slezakova S, Borilova Linhartova P, Masopustova L, Bartova J, Petanova J, Kuklinek P, Fassmann A, Dusek L, Izakovicova Holla L. Association of the NOD-like receptor 3 (NLRP3) gene variability with recurrent aphthous stomatitis in the Czech population. J Oral Pathol Med. 2018;47(4):434–9. [DOI] [PubMed]
- 7.Izakovicova Holla L, Valova S, Borilova Linhartova P, Bartova J, Petanova J, Kuklinek P, Fassmann A. Association study of interleukin-1 family, interleukin-6, and its receptor gene polymorphisms in patients with recurrent aphthous stomatitis. J Oral Pathol Med. 2017;46(10):1030–1035. doi: 10.1111/jop.12594. [DOI] [PubMed] [Google Scholar]
- 8.Oztekin A, Oztekin C. Vitamin D levels in patients with recurrent aphthous stomatitis. BMC Oral Health. 2018;18(1):186. doi: 10.1186/s12903-018-0653-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Maweri SA, Halboub E, Al-Sufyani G, Alqutaibi AY, Shamala A, Alsalhani A. Is vitamin D deficiency a risk factor for recurrent aphthous stomatitis? A systematic review and meta-analysis. Oral Dis. 2019. 10.1111/odi.13189. [published online ahead of print, 2019 Sep 6]. [DOI] [PubMed]
- 10.Brocklehurst P, Tickle M, Glenny AM, Lewis MA, Pemberton MN, Taylor J, Walsh T, Riley P, Yates JM. Systemic interventions for recurrent aphthous stomatitis (mouth ulcers) Cochrane Database Syst Rev. 2012;9:Cd005411. doi: 10.1002/14651858.CD005411.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yarom N, Zelig K, Epstein JB, Gorsky M. The efficacy of minocycline mouth rinses on the symptoms associated with recurrent aphthous stomatitis: a randomized, double-blind, crossover study assessing different doses of oral rinse. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123(6):675–679. doi: 10.1016/j.oooo.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Preshaw PM, Grainger P, Bradshaw MH, Mohammad AR, Powala CV, Nolan A. Subantimicrobial dose doxycycline in the treatment of recurrent oral aphthous ulceration: a pilot study. J Oral Pathol Med. 2007;36(4):236–240. doi: 10.1111/j.1600-0714.2007.00507.x. [DOI] [PubMed] [Google Scholar]
- 13.Ylikontiola L, Sorsa T, Hayrinen-Immonen R, Salo T. Doxymycine-cyanoacrylate treatment of recurrent aphthous ulcers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83(3):329–333. doi: 10.1016/S1079-2104(97)90238-9. [DOI] [PubMed] [Google Scholar]
- 14.Hayrinen-Immonen R, Sorsa T, Pettila J, Konttinen YT, Teronen O, Malmstrom M. Effect of tetracyclines on collagenase activity in patients with recurrent aphthous ulcers. J Oral Pathol Med. 1994;23(6):269–272. doi: 10.1111/j.1600-0714.1994.tb00057.x. [DOI] [PubMed] [Google Scholar]
- 15.Skulason S, Holbrook WP, Kristmundsdottir T. Clinical assessment of the effect of a matrix metalloproteinase inhibitor on aphthous ulcers. Acta Odontol Scand. 2009;67(1):25–29. doi: 10.1080/00016350802526559. [DOI] [PubMed] [Google Scholar]
- 16.Piacentini M, Borghetti RL, Zancanaro de Figueiredo MA, Cherubini K, Gonçalves Salum F. Doxycycline: An option in the treatment of ulcerated oral lesions?. J Clin Pharm Ther. 2019;44(6):838–43. [DOI] [PubMed]
- 17.Thriveni R, Anjum G, Ramesh D, Byatnal A, Wale M, Pragati K. A novel treatment modality for recurrent aphthous stomatitis–single application of doxycycline hyclate. J Indian Acad Oral Med Radiol. 2018;30(1):96. doi: 10.4103/jiaomr.jiaomr_135_17. [DOI] [Google Scholar]
- 18.Sharma R, Pallagatti S, Aggarwal A, Sheikh S, Singh R, Gupta D. A randomized, double-blind, placebo-controlled trial on clinical efficacy of topical agents in reducing pain and frequency of recurrent Aphthous ulcers. Open Dent J. 2018;12:700–713. doi: 10.2174/1745017901814010700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chandak R, Sonule S, Chandak M, Rawlani S, Gaikwad R. Efficacy of single application of topical doxycycline hyclate and triamcinolone acetonide in denture adhesive in the management of recurrent aphthous stomatitis: a comparative study. J Oral Res Rev. 2017;9(2):72. doi: 10.4103/jorr.jorr_43_16. [DOI] [Google Scholar]
- 20.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. Ann Intern Med. 2001;134(8):657–662. doi: 10.7326/0003-4819-134-8-200104170-00011. [DOI] [PubMed] [Google Scholar]
- 22.Shoor H, Pai KM. Single application of topical doxycycline hyclate in the management of recurrent aphthous stomatitis: remarks. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(4):533. doi: 10.1016/j.oooo.2013.11.501. [DOI] [PubMed] [Google Scholar]
- 23.Vijayabala GS. Single application of topical doxycycline hyclate in the management of recurrent aphthous stomatitis: reply to remarks. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(4):533–534. doi: 10.1016/j.oooo.2013.12.411. [DOI] [PubMed] [Google Scholar]
- 24.Reichert C. Doxycycline in the management of aphthous stomatitis. J Orofac Orthop. 2014;75(6):415–416. doi: 10.1007/s00056-014-0268-y. [DOI] [PubMed] [Google Scholar]
- 25.Al-Maweri SA, Kalakonda B, Al-Soneidar WA, Al-Shamiri HM, Alakhali MS, Alaizari N. Efficacy of low-level laser therapy in management of symptomatic oral lichen planus: a systematic review. Lasers Med Sci. 2017;32(6):1429–1437. doi: 10.1007/s10103-017-2233-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the findings of this article are available from the corresponding author.