Abstract
PURPOSE
While there are studies under way to characterize the direct effects of the COVID-19 pandemic on the care of patients with cancer, there have been few quantitative reports of the impact that efforts to control the pandemic have had on the normal course of cancer diagnosis and treatment encounters.
METHODS
We used the TriNetX platform to analyze 20 health care institutions that have relevant, up-to-date encounter data. Using this COVID and Cancer Research Network (CCRN), we compared cancer cohorts identified by querying encounter data pre-COVID (January 2019-April 2019) and current (January 2020-April 2020). Cohorts were generated for all patients with neoplasms (malignant, benign, in situ, and of unspecified behavior), with new incidence neoplasms (first encounter), with exclusively malignant neoplasms, and with new incidence malignant neoplasms. Data from a UK institution were similarly analyzed. Additional analyses were performed on patients with selected cancers, as well as on those having had cancer screening.
RESULTS
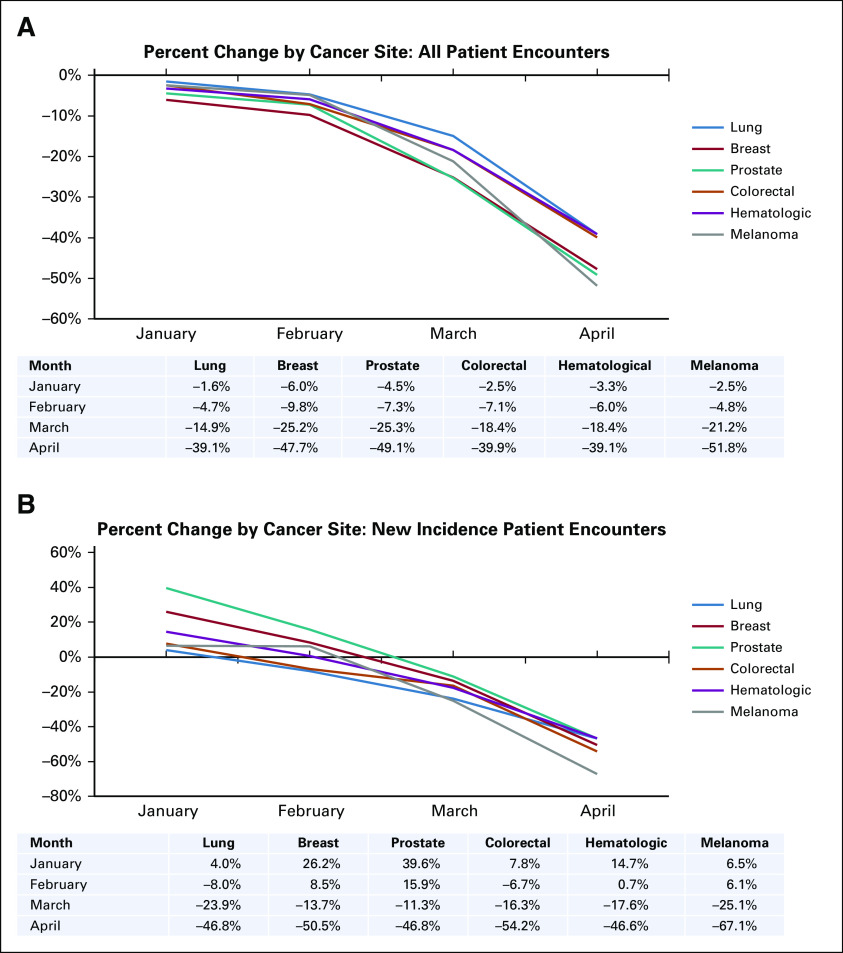
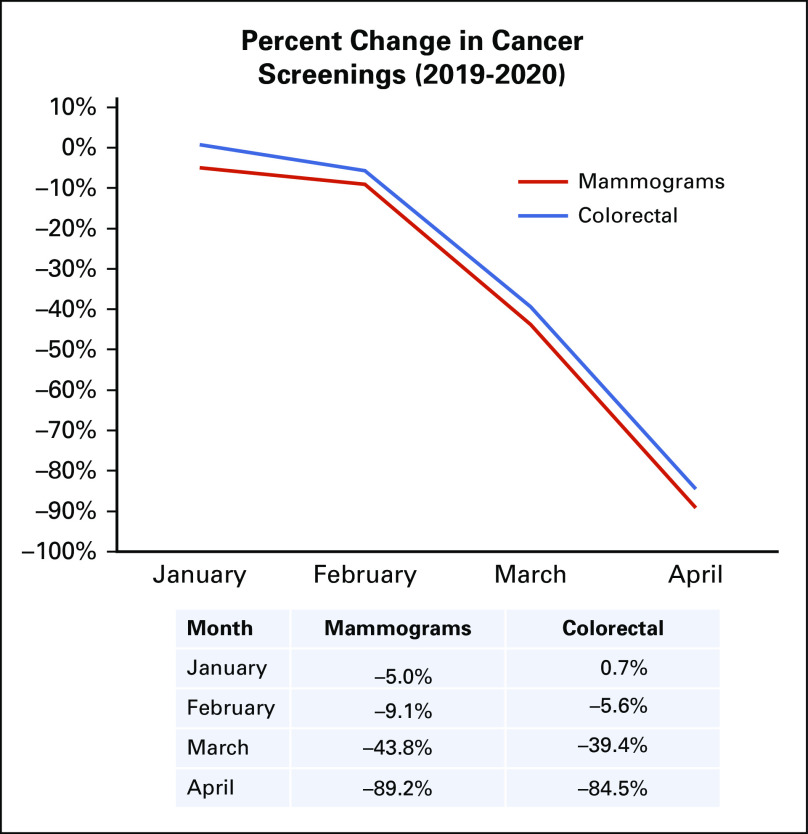
Clear trends were identified that suggest a significant decline in all current cohorts explored, with April 2020 displaying the largest decrease in the number of patients with cancer having encounters. Of the cancer types analyzed, lung, colorectal, and hematologic cancer cohorts exhibited smaller decreases in size in April 2020 versus 2019 (−39.1%, −39.9%, −39.1%, respectively) compared with cohort size decreases for breast cancer, prostate cancer, and melanoma (−47.7%, −49.1%, −51.8%, respectively). In addition, cancer screenings declined drastically, with breast cancer screenings dropping by −89.2% and colorectal cancer screenings by −84.5%.
CONCLUSION
Trends seen in the CCRN clearly suggest a significant decrease in all cancer-related patient encounters as a result of the pandemic. The steep decreases in cancer screening and patients with a new incidence of cancer suggest the possibility of a future increase in patients with later-stage cancer being seen initially as well as an increased demand for cancer screening procedures as delayed tests are rescheduled.
INTRODUCTION
Since the emergence of COVID-19, steps taken to mitigate the spread of the virus have affected almost everyone. This is certainly the case for patients diagnosed with cancer. There are a number of key efforts under way to gather data on the pandemic’s effect on patients with cancer, including the COVID-19 and Cancer Consortium1-4 and the ASCO Survey on COVID-19 in Oncology5 registries. Anecdotal reports, such as a Boston Globe article,6 have described local drops in cancer screening tests, such as mammography and colonoscopy, either because of patient reluctance to appear at clinics for these services or providers postponing the availability of such services. However, there have been few studies to quantify the immediate impact COVID-19 has had on deviation from normal cancer care activities, including cancer screening efforts.
CONTEXT
Key Objective
This study quantifies the effects that the COVID-19 pandemic has had on current and prospective patients with cancer by utilizing a network of 20 US institutions that have > 28 million patients.
Knowledge Generated
By comparing patient encounter data from January 2019 to April 2019 with the same months in 2020, we identified significant declines in both existing and new incidence neoplasms (malignant, benign, in situ, and unspecified behavior) as well as substantial decreases in breast cancer (−89.2%) and colorectal cancer (−84.5%) screenings.
Relevance
Our findings indicate a significant decline in all neoplasm-related encounters as a result of the COVID-19 pandemic, which suggests the potential for increases in later-stage disease at presentation and increased screening demand in the future. Together, this confirms the need to monitor both the short-term and the long-term effects the pandemic will have on this population.
This article contributes metrics on patients who have had cancer-related encounters in the early days of the COVID-19 pandemic in the United States. We were able to leverage an existing health research network platform (TriNetX; Cambridge, MA)7 to analyze data from 20 different provider institutions across the United States that represent > 28 million patients and that have immediate data on relevant patient encounters. We focused on patients seen at these health care organizations (HCOs) with diagnostic codes for malignant, benign, in situ, and unspecified neoplasms (International Classification of Diseases, Tenth Revision [ICD-10], codes C00-D49). We looked at the number of these patients having encounters for March 2020 and April 2020 compared with the same months in 2019. We also focused on the subset of these patients with malignant neoplasm diagnoses (ICD-10 codes C00-C96, D37-D49). We also obtained the number of these patients (all with neoplasms and malignancies only) being seen for the first time at these institutions possibly for screening, initial diagnosis, second opinion, or treatment initiation. Finally, patient metrics for site-specific malignancies were analyzed (lung, breast, prostate, colorectal, and hematologic cancers and melanoma). Furthermore, we considered the data from an HCO in the United Kingdom to initiate exploration of the global applicability of the trends we observed for our US network.
METHODS
COVID and Cancer Research Network Creation
Data for this study were obtained from a subset of HCOs that are members of the TriNetX Research Network. TriNetX7 is a global federated health research network that provides access to aggregate data from electronic medical records (EMRs), including demographics, diagnoses, procedures, medications, laboratory testing, vital signs, and genomic information. The network consists of academic medical centers, community hospitals, and physician practices. The COVID and Cancer Research Network (CCRN) subnet was formed of HCOs that have immediate, relevant data (ie, reliable, comprehensive data) on the diagnoses of patients with encounters at the organization for the period January 1, 2019, through April 30, 2020. This primarily means that the HCO had established data acquisition for the TriNetX platform as of January 1, 2019, and had refreshed these data so that encounters through April 30, 2020, would be included. This resulted in a study network of 20 different institutions across the United States, representing > 28 million patients. Separately, data from University Hospitals Plymouth NHS Trust, a UK HCO member of the TriNetX network, were also accessed to provide an indication of the trends being studied at a non-US HCO. As with all real-world health data, revisions are always possible in ensuing months, although major changes that would affect clear trends would not be expected.
Cohort Definitions
Two main categories of patients were studied: those with HCO encounters who had diagnostic ICD-10 codes for neoplasms (C00-D49) and those who had diagnostic ICD-10 codes for the subset of malignant neoplasms (C00-C96, D37-D49). The first category includes benign, in situ, and unspecified neoplasms along with malignant neoplasms. The second category is only patients with encounters related to malignant neoplasms. For each of the 2 main categories, a subgroup of patients with no previous encounter with the HCO related to the indicated diagnosis (defined as new incidence encounters) was added. These patients with new incidence disease may have been seen at the HCO for screening, initial diagnosis, second opinion, or treatment initiation. While it is of interest to interrogate newly diagnosed patients, such designation is required by the HCO’s tumor registry, which can distinguish between patients initially diagnosed at the institution versus those previously diagnosed elsewhere.
Additional subgroups of these main groups were formed around specific malignant cancer diagnoses (ICD-10), including breast (C50), lung (C34), prostate (C61), colorectal (C18-21), hematologic (C81-96), and melanoma (C43). Additional patient cohorts were defined for patients having undergone cancer screening procedures, including mammograms (ICD-10 codes R92.0-R92.2, Z12.31; Current Procedural Terminology [CPT] codes 77067, 1029705) and colorectal cancer screening (ICD-10 code Z12.11; CPT codes 1022231, 1007534, 1020217).
Cohort Comparison and Analysis
For all groups, patient cohort sizes were obtained by constructing TriNetX platform queries with the appropriate diagnosis (ICD-10), procedure (ICD-10, CPT), and date constraints (eg, April 1, 2020, through April 30, 2020, for the month of April 2020). The platform then returns patient cohort data for these queries. Patients found to satisfy a query in multiple instances (eg, multiple encounters in the time period) were counted only once. Percent change between each month was calculated by subtracting the patient count in 2019 from the same month in 2020 and dividing by the total patient count from 2019.
RESULTS
Network Characteristics
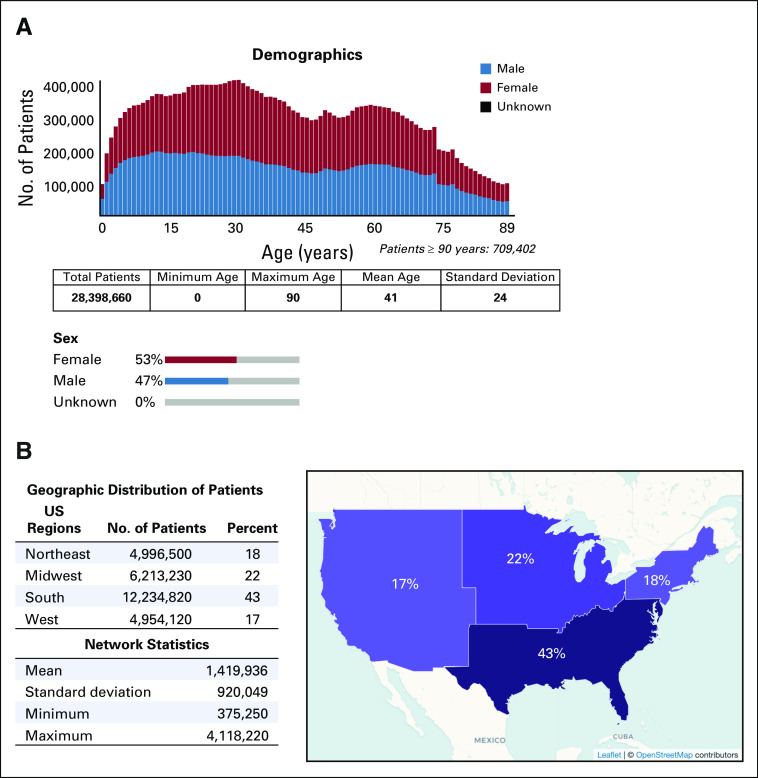
The CCRN comprises data from 20 distinct institutions across the United States, representing data from > 28 million patients. The institutions included were selected after verifying data quality and continuity across 2019 and 2020 to reduce potential artifacts that arise from differences in data coverage. The mean age of patients included in the CCRN was 41 years, with a slightly higher proportion of patients in the network being female (53% v 47%; Fig 1A). Geographically, the CCRN is represented by sites from across the United States, with 43% of patients seen at institutions in the South, 22% in the Midwest, 18% in the Northeast, and 17% in the West (Fig 1B).
FIG 1.
COVID and Cancer Research Network descriptive statistics and demographics. (A) Distribution of patient age and sex within the network. (B) Geographic distribution split into Northeast, Midwest, South, and West. Network statistics represent the distribution in sizes of individual institutions included in the network.
Incidence of Patients With Neoplasms
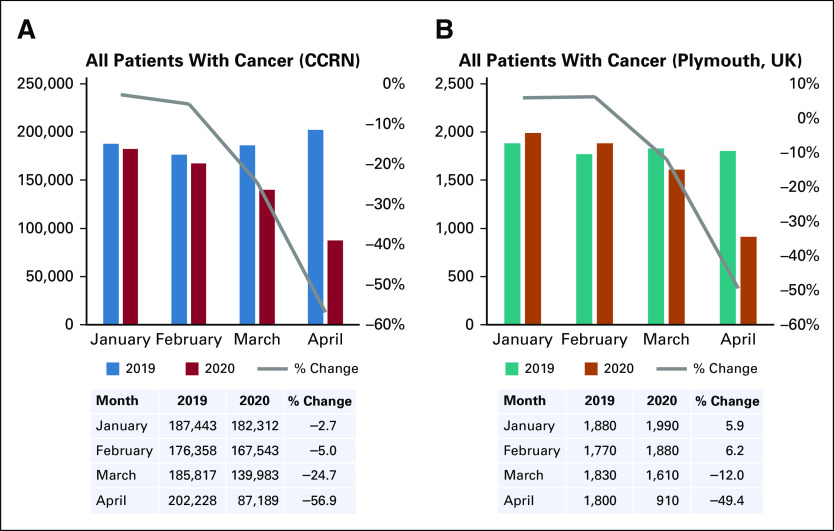
To quantify the effects of COVID-19 mitigation policies on the cancer population, the CCRN was queried for all patients with a neoplasm-related ICD-10 diagnostic code (C00-D49). Cohorts were generated by month, using January 2019 through April 2019 and the same months in 2020 to account for natural seasonal differences in patient presentation, with January representing a pre-COVID baseline. As shown in Figure 2A, the number of patients identified in January 2020 declined slightly compared with January 2019, decreasing by −2.7% (187,443 to 182,312). Similarly, February 2020 declined by −5.0% (176,358 to 167,543) compared with February 2019. Patients with cancer identified in March 2020 versus March 2019 decreased by −24.7% (185,817 to 139,983), and by April, the reduction in patients was −56.9% (202,228 to 87,189). To compare these trends with a health care institution outside the United States, site-specific data from University Hospitals Plymouth NHS Trust in the United Kingdom were used. Unlike the CCRN, patients with cancer seen increased in January 2020 and February 2020 compared with 2019 (by 5.9% and 6.2%, respectively; Fig 2B). However, March 2020 and April 2020 exhibited marked decreases in cancer-related patient encounters, with declines of −12.0% (1,830 to 1,610) and −49.4% (1,800 to 910), respectively. Taken together, these data show a striking reduction in the number of cancer-related patient encounters as the measures to contain the COVID-19 pandemic progressed and suggest that these trends are not specific to institutions in the United States.
FIG 2.
The effects of COVID-19 on patients with any neoplasm-related encounter. (A) Plot representing patient counts identified by month from January to April in either 2019 (blue) or 2020 (red) using International Classification of Diseases, Tenth Revision, diagnosis codes for all neoplasms, including benign and in situ (C00-D49), with percent change from 2019 to 2020 indicated by gray line. Also shown are patient counts and percent change for each indicated month and year. (B) Patient counts for 2019 (green) and 2020 (orange) from University Hospitals Plymouth NHS Trust in the United Kingdom (UK). Plot and table were generated identically to that shown in panel A. CCRN, COVID and Cancer Research Network.
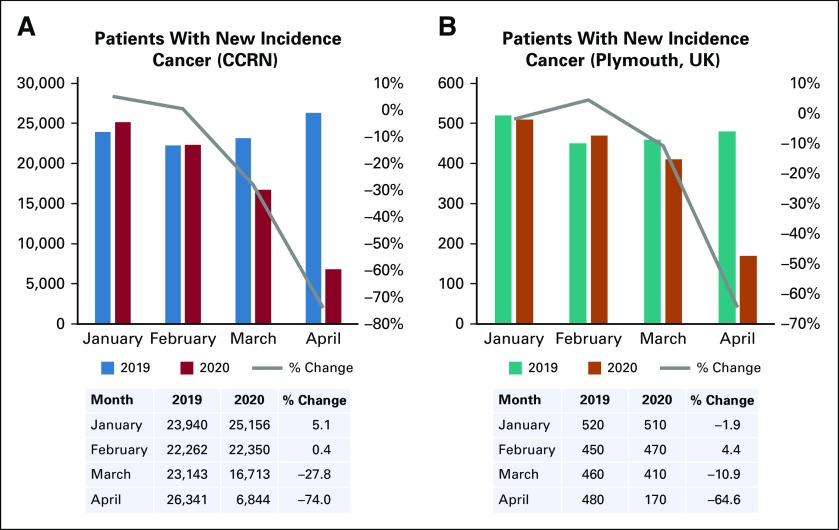
To determine potential changes in cancer screening, initial diagnosis, second opinion, or treatment initiation encounters, queries were executed to create patient cohorts that have a cancer-related diagnostic code for the first time at a given CCRN institution (patients with new incidence cancer). The number of patients with new incidence cancer exhibited minor increases in January 2020 and February 2020 versus 2019 (5.1% and 0.4%, respectively; Fig 3A). Patients with new incidence cancer were then seen to exhibit sharp decreases in March 2020 (−27.8%) and April 2020 (−74.0%), a 17.1% larger drop compared with patients with cancer as a whole. With respect to trends in the United Kingdom, patients with new incidence cancer decreased slightly in January 2020 (−1.9%) and increased in February 2020 (4.4%; Fig 3B). Patients in March 2020 displayed a −10.9% decline compared with 2019, and by April 2020, the change was −64.6%, 15.1% more than the change seen with all patients with cancer. Of note, these data suggest that patients with new incidence cancer are likely to be more affected by the pandemic than existing patients, with implications for delayed diagnosis and poorer prognosis in the future.
FIG 3.
The effects of COVID-19 on patients with new incidence encounters associated with any neoplasm. (A) Plot representing counts for patients with a new incidence encounter (ie, no previous encounter related to the indicated neoplasm diagnosis) from CCRN data. (B) Patients with new incidence encounters at University Hospitals Plymouth NHS Trust in the United Kingdom (UK). CCRN, COVID and Cancer Research Network.
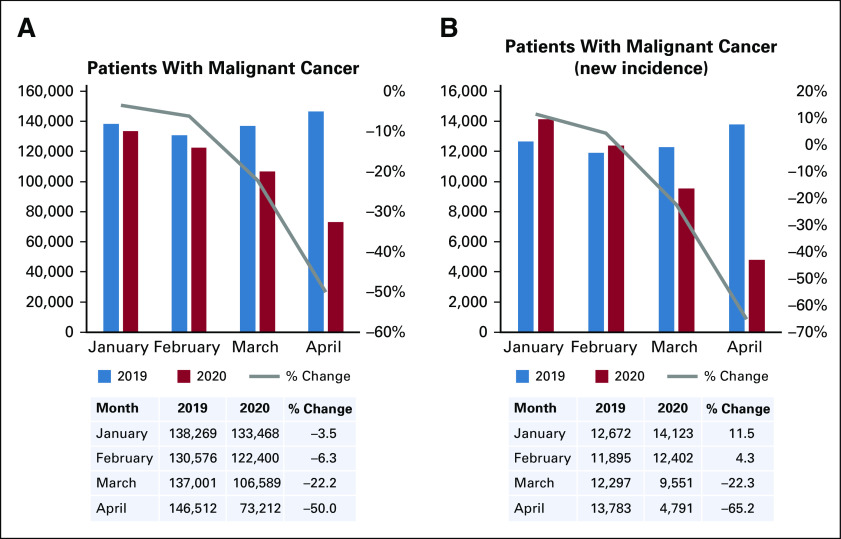
Malignant Cancer Incidence
The pandemic control efforts corresponded to a significant decline in the number of all patients with cancer encountered as well as patients with new incidence cancer. While these trends were detected using all neoplasm diseases (malignant, benign, in situ, unspecified) as filter criteria, changes to the numbers of patients with malignant cancer (having ICD-10 diagnostic codes C00-C96, D37-D49) were explored using a similar methodology. The number of patients with malignant cancer decreased by −3.5% (138,269 to 133,468) in January 2020 versus 2019, while February 2020 showed declines by −6.3% (130,576 to 122,400; Fig 4A). March 2020 showed a drop in patients of −22.2% (137,001 to 106,589), and April 2020 showed the most drastic decline, with the number patients with malignant cancer falling by −50% compared with those seen in 2019. Similar to the queries performed for all patients with cancer, those with new incidence malignant cancer were next interrogated. While January and February both showed an increased number of patients in 2020 compared with 2019 (11.5% and 4.3%, respectively), this trend reversed by March 2020, with a change of −22.3% (12,297 to 9,551; Fig 4B).
FIG 4.
The effects of COVID-19 on patients with a malignant neoplasm–associated encounter. (A) Patients identified by month as previously described, using International Classification of Diseases, Tenth Revision, diagnosis codes for any malignant neoplasm (C00-C96, D37-D49). (B) Counts of patients with new incidence malignant neoplasm diagnosis.
Consistent with other queries, April 2020 displayed the most drastic drop in identified patients with malignant cancer, with a −65.2% decline in 2020 (13,783 to 4,791). On balance, data exclusively from patients with malignant cancer diagnoses followed similar trends as all patients with cancer, which suggests possible future deleterious effects on diagnosis and treatment of these patients.
Tumor Type–Specific Impact
It is clear that the efforts to control the spread of COVID-19 have drastically reduced the number of encounters with patients with new and current neoplasms, both malignant and benign. To determine whether all cancer types showed similar trends, the malignant cancer cohort was divided into tumor type–specific cohorts: lung cancer, breast cancer, prostate cancer, colorectal cancer, hematologic cancers, and melanoma. While all cancer types displayed similar trends in the reduction of patients from January 2020 to April 2020 compared with 2019, some cancer types were more affected than others. Melanoma, prostate cancer, and breast cancer displayed the largest decrease in patients identified, with a −51.8%, −49.1%, and −47.7% drop in April 2020 versus 2019, respectively (Fig 5A). Of note, lung cancer and hematologic cancers showed the smallest reductions, both with a −39.1% fall in patients from April 2020 versus 2019, while colorectal cancer fell by −39.9%. Next, patients with new incidence cancer were interrogated in these cancer types. Patients with new incidence melanoma dropped by −67.1% in April 2020 compared with 2019, while lung cancer was the least altered (−46.8%; Fig 5B). Of note, while patients with new incidence colorectal cancer (−54.2%) and hematologic cancers (−54.2%) showed decreases compared with the trends seen with all patients, those with new incidence prostate cancer and breast cancer fell at similar rates as patients with these cancers as a whole (−46.8% and −50.5%, respectively).
FIG 5.
The effects of COVID-19 among cancer types. (A) Patient counts were generated for the indicated month for each cancer type in 2019 and 2020 using International Classification of Diseases, Tenth Revision, diagnosis codes: breast cancer (C50), lung cancer (C34), prostate cancer (C61), colorectal cancer (C18-21), hematologic cancers (C81-96), and melanoma (C43). Percent change from 2019 to 2020 is shown. (B) Patient counts were generated using the diagnosis codes indicated in panel A, filtering on patients with new incidence encounters.
Cancer Screening
Finally, to explore the effects of the pandemic on cancer screening rates, screening for both breast cancer and colorectal cancer was considered. As shown in Figure 6, screening for both malignancies showed extreme reductions in the percent change between 2020 and 2019. Breast cancer screening declined by −5.0% and −9.1% in January and February 2020, respectively. Similarly, colorectal cancer screening remained largely unchanged in January (0.7%) and decreased by −5.6% in February 2020. Patients with breast cancer and colorectal cancer who underwent screening in March 2020 were shown to fall by −43.8% and −38.4%, respectively. Consistent with data using patient diagnoses, April displayed the greatest drop in screenings. Patients with breast cancer who underwent screening declined by −89.2%, while screening of patients with colorectal cancer fell by −84.5% when comparing 2020 with 2019. Together, these data validate the underlying trends observed using diagnosis data and suggest a potential increase in the presentation of later-stage disease for newly diagnosed patients in future months.
FIG 6.
The effects of COVID-19 on cancer screening. Patient counts were generated for breast cancer screening encounters using International Classification of Diseases, Tenth Revision (ICD-10), codes R92.0-R92.2 and Z12.31 and Current Procedural Terminology (CPT) codes 77067 and 1029705 and colorectal cancer screening encounters using ICD-10 code Z12.11 and CPT codes 1022231, 1007534, and 1020217. Percent change from 2019 to 2020 is shown in the indicated months.
DISCUSSION
To our knowledge, this study is the largest to date to quantify the changes caused by the COVID-19 pandemic with regard to normal cancer care activities. Descriptions of measures taken to manage patients with cancer2,3,8 as well as anecdotal reports6 on declines in cancer screening have been published. The current study utilizes the CCRN, a TriNetX network of 20 US institutions with > 28 million patients, to quantify the deviations from normal cancer encounters and screening procedures. Similar to what has been suggested through physician surveys,9 rates of cancer diagnoses, both recurring and new incidence, were seen to dramatically decrease as the pandemic progressed. This could have a significant impact on the prognosis of patients with cancer across cancer types in the near future because later-stage initial encounters may increase. In addition, increased use of cancer screening and treatment resources may occur as pandemic mitigation restrictions are eased and previously postponed procedures resume.
The CCRN comprises institutions from different geographical locations in the United States; however, the majority of patients in this network were seen at sites in the southern United States (Fig 1B). Because the effects of the virus were first felt in the Northeast, it is possible that the current network is skewed to under-report the magnitude of the changes to cancer-related patient encounters simply because of differences in the contributing institutions’ geographical locations. It will be important to continue to use the CCRN to track changes moving forward and to test the potential for delayed responses in other locations.
Overall, a substantial decline was observed in the number of patients with a neoplasm-related diagnosis (ICD-10 codes C00-D49) encountered, with patient counts declining by −56.9% in April 2020 versus April 2019 (Fig 2A). Unexpectedly, a small decline in patient counts was seen starting in January and February 2020 in the CCRN, which warrants further investigation. With respect to institutions outside of the United States, University Hospitals Plymouth NHS Trust ultimately showed similar, albeit delayed, trends in patient decline (Fig 2B). This delay is likely to be due to differences in the timing of the spread of COVID-19 in each country. However, it is important to note that the comparison is with a single hospital in the United Kingdom, and more data are necessary for validation.
While the decline in patients with cancer as a whole was clearly evident, decreases specific to those with new incidence cancer were shown to be even more drastic. In the CCRN, the number of patients with new incidence cancer seen in April 2020 decreased by −74.0% compared with April 2019, while in the University Hospitals Plymouth NHS Trust data set, this drop was shown to be −64.6%. These declines may suggest that while a patient with a known cancer-related diagnoses would be more inclined to continue treatment or keep a scheduled visit, potential patients with a new incidence (cancer screening, initial diagnosis, second opinion, or treatment initiation encounters) may be more likely to delay these encounters. Similar trends were seen when filtering specifically on patients with a diagnosis for a malignant neoplasm, with a −50% drop in all patients but a −65.2% fall in new incidence for this cohort. While these trends for malignant neoplasms are slightly less severe than with all neoplasms, the decline in patients remains substantial for both groups and further confirms the need to consider the future impact of delayed initial cancer screening and care.
Declining patient counts varied by cancer type, with breast cancer, prostate cancer, and melanoma being most affected, while lung, colorectal, and hematologic cancers were the least affected. While the decrease in patients with lung cancer seen was expected to be less significant because of respiratory symptoms common to COVID-19 motivating patients to seek care, the current data do not support this hypothesis, as colorectal and hematologic cancers had similar drops in patients with encounters. In comparison, a report of patients referred to Beth Israel Deaconess Medical Center described drops in patients with breast cancer by 65% and with hematologic cancer by 61%.6 While not showing the same difference in magnitude as in our study for these 2 diseases, in both studies, the decreases were substantial.
The most significant finding in the current study relates to cancer screening. Patients in the CCRN displayed a decrease of −89.2% for breast cancer screening (mammogram) and for colorectal screening (colonoscopy, computed tomography scan), almost −84.5%. These results are similar to a study from the EPIC Health Research Network, using institutions on the EPIC EMR system, where breast and colorectal cancer screenings were shown to decline by > 90% in March and April 2020.10 Tracking the eventual rebound in these trends in the coming months will be important for predicting how many patients continue to delay screening because of concerns related to the pandemic.
The COVID-19 pandemic has had a tremendous immediate impact on the world, and it is clear that there will be effects for years to come. Of note, the data presented here reveal quantifiable trends that indicate substantial declines in cancer-related patient encounters. Ultimately, these observed trends have serious implications for future cancer care and validate the need to study and monitor the effect of COVID-19 mitigation on cancer diagnosis and treatment moving forward.
PRIOR PRESENTATION
Presented at the 2020 Virtual Harvard Symposium for i2b2/tranSMART, Boston, MA, June 11-12, 2020.
SUPPORT
Supported by the Sidney Kimmel Cancer Center (grant 5P30CA056036-20; C.M.).
AUTHOR CONTRIBUTIONS
Conception and design: Jack W. London, Matvey B. Palchuk, Christopher McNair
Financial support: Christopher McNair
Collection and assembly of data: Jack W. London, Elnara Fazio-Eynullayeva, Matvey B. Palchuk, Christopher McNair
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/cci/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Jack W. London
Consulting or Advisory Role: TriNetX
Stock and Other Ownership Interests: TriNetX
Elnara Fazio-Eynullayeva
Employment: TriNetX
Stock and Other Ownership Interests: TriNetX
Matvey B. Palchuk
Employment: TriNetX
Stock and Other Ownership Interests: TriNetX
Peter Sankey
Speakers’ Bureau: Astellas Pharma
Travel, Accommodations, Expenses: Bayer AG, TriNetX
No other potential conflicts of interest were reported.
REFERENCES
- 1. The COVID-19 and Cancer Consortium. https://cancerletter.com/articles/20200320_3.
- 2.Kuderer NM, Choueiri TK, Shah DP, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet. 2020;395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubinstein SM, Steinharter JA, Warner J, et al. The COVID-19 and Cancer Consortium: A collaborative effort to understand the effects of COVID-19 on patients with cancer. Cancer Cell. 2020;37:738–741. doi: 10.1016/j.ccell.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. doi: 10.1038/s43018-020-0065-z. Desai A, Warner J, Kuderer N, et al: Crowdsourcing a crisis response for COVID-19 in oncology. Nat Cancer . [epub ahead of print on April 21, 2020] [DOI] [PubMed] [Google Scholar]
- 5. American Society of Clinical Oncology: ASCO Survey on COVID-19 in Oncology (ASCO) Registry. https://www.asco.org/asco-coronavirus-information/coronavirus-registry.
- 6. Kowalczyk L. Major Boston hospital finds dramatic drop in stroke, heart attack, and cancer patients during coronavirus pandemic. https://www.bostonglobe.com/2020/05/18/nation/major-boston-hospital-finds-dramatic-drop-stroke-heart-attack-cancer-patients-during-coronavirus-pandemic.
- 7. doi: 10.1200/CCI.17.00067. Topaloglu U, Palchuk MB: Using a federated network of real-world data to optimize clinical trials operations. JCO Clin Cancer Inform 10.200/CCI.17.00067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. doi: 10.6004/jnccn.2020.7560. Ueda M, Martins R, Hendrie PC, et al: Managing cancer care during the COVID-19 Pandemic: Agility and collaboration toward a common goal. J Natl Compr Canc Netw . [epub ahead of print on March 20, 2020] [DOI] [PubMed] [Google Scholar]
- 9. American Cancer Society: COVID-19 pandemic impact on cancer patients and survivors: Survey findings summary, 2020. https://www.fightcancer.org/sites/default/files/National%20Documents/Survivor%20Views.COVID19%20Polling%20Memo.Final_.pdf.
- 10. EPIC Health Research Network: Preventive cancer screenings during COVID-19 pandemic, 2020. https://ehrn.org/wp-content/uploads/Preventive-Cancer-Screenings-during-COVID-19-Pandemic.pdf.