Abstract
Objectives
To study (i) the association of general self-efficacy (GSE) on the course of subjective (i.e. basic and instrumental activities of daily living (ADLs and IADLs) and objective physical performance outcomes (short physical performance battery (SPPB)) among older persons from discharge up to 3 months post-discharge and (ii) the extent to whether motivational factors such as depressive symptoms, apathy and fatigue mediate this association.
Methods
Prospective multi-centre cohort of acutely hospitalised patients aged ≥70 (Hospital-ADL study). Structural equation modelling was used to analyse the structural relationships.
Results
The analytic sample included 236 acutely hospitalised patients. GSE had a significant total effect on the course of subjective and objective performance outcomes (ADLs: β = −0.21, P < 0.001, IADLs: β = −0.24, P < 0.001 and SPPB: β = 0.17, P < 0.001). However, when motivational factors as mediator were included into the same model, motivational factors (IADLs: β = 0.51, P < 0.001; SPPB: β = 0.49, P < 0.001) but not GSE remained significantly associated with IADLs (β = −0.06, P = 0.16) and SPPB (β = 0.002, P = 0.97). Motivational factors partially mediated the relationship between GSE and ADLs (β = −0.09, P = 0.04). The percentage of mediation was 55, 74 and 99% for ADLs, IADLs and SPPB, respectively.
Conclusions
Motivational factors and GSE are both associated with subjective and objective performance outcomes. However, the relationship between GSE and subjective and objective performance outcomes was highly mediated by motivational factors. Taken together, this suggests that GSE is important to being physically active but not sufficient to becoming more physical active in acutely hospitalised older patients; motivation is important to improving both subjective and objective performance.
Keywords: structural equation modelling, depressive symptoms, apathy, motivation, activities of daily living, older people
Key Points
General self-efficacy (GSE) was associated with a worse course of subjective and objective physical performances.
However, when motivational factors were taken into account, GSE became no longer significantly associated with physical outcomes.
Taken together, GSE is important to be physically active but not sufficient in becoming more physical active in older patients.
Future research needs to focus on interventions that affect motivation instead of GSE to prevent poor physical outcomes.
Introduction
Self-efficacy is conceptualised as one’s belief in his or her personal capabilities to successfully execute courses of action [1]. In general, self-efficacy is interpreted as being a task- or domain-specific concept [2]. However, previous research has also described a more trait-like generalised belief of self efficacy, defined as general self-efficacy (GSE) [3]. This latter concept refers to ‘a broad and stable sense of personal competence in mastering a variety of stressful situations’ [4]. This broad GSE concept may be useful in investigating the wellbeing of patients (for example, among acutely hospitalised older patients) who have had to adapt to the consequences of their acute medical illness [5].
Among older adults, acute illness leading to hospital admission frequently precipitates limitations in activities of daily living (ADL), and the prognosis for older adults with new or additional ADL limitations after hospitalisation is poor [6]. Research has shown that GSE is linked with ADL limitations in older persons [7,8]. It is important to note that self-efficacy is also related to motivational factors, such as depressive symptoms [2, 9], apathy [10], and fatigue [11]. However, to our knowledge, this is the first study that investigated the impact of motivational factors in the relationship between GSE and performance outcomes.
Considering the potential importance of GSE on physical outcomes among older adults, as well as a lack of studies investigating GSE in relation to motivational factors among acutely hospitalised older patients, this study aims to investigate the mutual influence of GSE on performance outcomes and the extent to which motivational factors mediate this association.
Methods
Design
The current analysis was based on the data from the prospective multi-centre Hospital-ADL cohort study, previously described in detail elsewhere [12]. Local approval has been provided by all participating hospitals. The study has been approved by an institutional review board in the Netherlands. The research was performed according to the Dutch Medical Research Involving Human Subjects Act and the principles of the Declaration of Helsinki (1964).
Study population
A total of 401 participants, aged 70 years and above, were recruited from patients who were acutely admitted at the Department of Internal Medicine, Cardiology and Geriatrics. Inclusion criteria consisted of the following: (i) being admitted for ≥48 h, (ii) Dutch language proficiency sufficient to complete questionnaires and (iii) Mini-Mental State Examination (MMSE) score of 15 or higher [13]. Notably, we were not able to include delirious patients, due to the short time frame of inclusion, i.e. within 48 h after admission. A delirium was often still present at this point, which meant that an MMSE could not be performed or patients scored below 15 points. The confusion assessment methodwas used to identify the presence of delirium [14]. Patients were excluded if they exhibited any of the following: (i) had a life expectancy of 3 months or less according to the attending medical doctor or (ii) were disabled in all six basic ADLs as determined by the Katz-6 ADL index [15].
Procedures
Two researchers (R.V.S. and L.R.) contacted eligible patients within 48 h after hospital admission. Patients were informed about the objectives of the Hospital-ADL study and the study procedures. All participants provided written informed consent before inclusion. After informed consent was obtained, patients were enrolled in the study. A trained geriatric team completed personal interviews within 48 h after admission, at discharge, and at 1 and 3 months post-discharge. All interviews were performed face-to-face in the hospital or at the participants’ places of residence.
Measurements
Independent variable
The ALCOS-12 (In Dutch: Algemene Competentie Schaal) was used to measure GSE (Cronbach’s α = 0.78 [16]). It is based on the self-efficacy scale [17] and consists of 12 items on a five-point Likert scale: 1, strongly disagree; 2, disagree; 3, no disagreement/agreement; 4, agree and 5, strongly agree. The total score was the sum of the 12 items (range: 12–60), whereby higher scores indicated more self-efficaciousness. Due to the fact that GSE refers to a broad and stable sense of personal competence [17, 18], it was measured once at discharge.
Mediator
The course of motivational factors was the latent variable, which consisted of depressive symptoms, apathy and fatigue, measured from discharge up to 3 months post-discharge. Apathy was measured with the apathy subscale of the Geriatric Depression Scale-15 (GDS-15) and consisted of the following questions: ‘Have you dropped many of your activities and interests?’, ‘Do you prefer to stay at home, rather than going out and doing new things?’ and ‘Do you feel full of energy?’ [19]. The GDS-3A has been reported to have a sensitivity of 69% and a specificity of 85% in detecting apathy based on the customary cut off (>13) of the 14-item apathy scale of Starkstein et al. [20] in older adults [19]. Depressive symptoms were measured with the 12 remaining items of the GDS-15 (GDS-12D) [21]. Higher scores indicated more symptoms of depression and apathy (range GDS-12D: 0–12; range GDS-3A: 0–3). Fatigue was measured with the numeric rating scale (NRS), which is a continuous scale with a score range from 0 to 10 (0 represents no fatigue and 10 the worst possible fatigue).
Dependent variables
The outcomes were longitudinal, subjective (i.e. basic ADLs and IADLs) and objective physical performance (as determined by a short physical performance battery (SPPB)). The course of subjective physical performances was measured with the 15 items modified Katz ADL index [22] from discharge up to 3 months post-discharge. The first six items on the modified Katz ADL index were used to measure the ADLs and consisted of statements of the patients’ independence in performing basic ADLs [15]. The remaining nine items consisted of statements of their independence in performing IADLs. Higher scores indicated more dependencies in ADLs and IADLs (range ADLs: 0–6; range IADLs: 0–9). The course of objective physical performance was also measured from discharge up to 3 months post-discharge. The SPPB was applied to measure the balance, strength and gait speed of the participants. They were asked to stand with their feet in various balance positions, walk 3 or 4 metres and to rise from a chair and return to the seated position five times as quickly as possible. Higher scores indicated a better performance (range: 0–12) [23].
Statistical methodology
Baseline characteristics were summarised with descriptive statistics, using SPSS version 24 (SPSS Inc., Chicago, IL, USA). To investigate the influence of GSE on motivational factors and physical performance, we performed a path analysis by using structural equation modelling (SEM) with Stata, version 15.0. The SEM analysis was performed in two steps: (i) the total effect of GSE on subjective performance and objective performance was examined, and then (ii) the direct and indirect effects of GSE on subjective and objective performance were examined, considering motivational factors as potential mediators. To remove the biased effect of measurement error [24], depressive symptoms (GDS-12D), apathy (GDS-3A) and fatigue (NRS) were used as a latent variable, called ‘motivational factors’ (Figure 1). The following effects were measured: (i) total effect of GSE on performance outcomes (path c in Figure 1), (ii) the effect of GSE on motivational factors (path a in Figure 1), (iii) the effect of motivational factors on the performance outcomes (path b in Figure 1) and (iv) the effect of GSE on performance outcomes, taking into account motivational factors (path c′ in Figure 1). Path c′ is called the direct effect, and the amount of mediation is estimated by a × b or c–c′. The percentage of mediation was estimated by indirect effect/total effect (*100%). For all analyses, standardised regression coefficients were reported, and because the present analyses were performed in the context of a larger study, no a priori sample size calculations were performed [12].
Figure 1 .
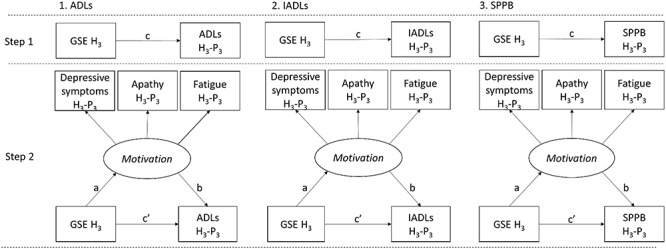
Conceptual model of SEM. H3 = at discharge; H3–P3 = longitudinal (i.e. from discharge up to 3 months post-discharge); c = total effect; a = effect a; b = effect b; c′ = direct effect; a*b = indirect effect.
Results
Description of the sample
There were 1,024 acutely hospitalised patients admitted to the participating hospital wards for ≥48 h between October 2015 and February 2017. Of the 1,024 unplanned admissions, 519 met the inclusion criteria and were contacted by the researchers. Of these, 401 agreed to participate. There were 165 patients without any GSE data; they were excluded from the sample. The analytic sample for the current study included 236 acutely hospitalised patients (mean age = 79.4 years; SD = 6.6). The total number of observations was 708. Table 1 shows the baseline characteristics of the participants and Appendix 1 (Supplementary data are available in Age and Ageing online) shows means, standard deviations, Cronbach’s α and Pearson r correlations of the main variables.
Table 1.
Baseline characteristics of analytic sample
| Characteristics | All patients |
|---|---|
| (N = 236) | |
| Demographics | |
| Age, y, mean (SD) | 79.4 (6.6) |
| Male sex, n (%) | 117 (49.6) |
| Education, n (%) | |
| Primary school | 61 (25.8) |
| ETS/DSS | 54 (22.9) |
| SVE | 74 (31.4) |
| HLHS/TLE | 47 (19.9) |
| Hospital department, n (%) | |
| Cardiology | 63 (26.7) |
| Internal medicine | 133 (56.4) |
| Geriatrics | 40 (16.9) |
| Hospital admission diagnoses, n (%) | |
| Cardiac | 67 (28.4) |
| Gastrointestinal | 25 (10.6) |
| Infection | 33 (14.0) |
| Respiratory | 46 (19.5) |
| Cancer (including haematology) | 9 (3.8) |
| Electrolyte disturbance | 7 (3.0) |
| Renal | 7 (3.0) |
| Other | 42 (17.8) |
| Cognitive impairment, n (%)a | 40 (17.5) |
| Severity of comorbid diseases | |
| CCI score, mean (SD)b | 5.7 (2.0) |
SD = standard deviation; n = number of participants; y = years; PS=primary school; ETS/DSS = elementary technical school/domestic science school; SVE = secondary vocational education; HLHS/TLE = higher level high school/third-level education.
aCognitively impaired if a score of less than 24 on the MMSE at admission (range, 0–30).
bAge-combined Charlson Comorbidity Index score: a higher score indicating more or more severe comorbidity.
Motivational factors as mediator between GSE and physical outcomes
Figure 2 shows the final mediation models with standardised regression coefficients. Initially, Model 1 showed a significant total effect of GSE at discharge on ADLs from discharge up to 3 months post-discharge (β = −0.21, P < 0.001). However, when motivational factors such as depressive symptoms, apathy and fatigue were taken into account, the coefficient decreased to −0.09 (P = 0.04), leading to a percentage of mediation of 55%. This was due to a significant relation between GSE and motivational factors (β = −0.35, P < 0.001) and between motivational factors and ADLs (β = 0.33, P < 0.001). Model 2 also showed a significant total effect of GSE on the course of IADLs (β = −0.24, P < 0.001), and here again, when motivational factors were taken into account, the standardised coefficient decreased to −0.06 (P = 0.16), leading to a percentage of mediation of 74%. This was due to a highly significant relation between GSE and motivational factors (β = −0.34, P < 0.001) and between motivational factors and IADLs (β = 0.51, P < 0.001). Finally, Model 3 also showed a significant total effect of GSE on the course of objective physical performance (β = 0.17, P < 0.001). However, once again, when motivational factors were taken into account, the standardised coefficient decreased to 0.002 (P = 0.97), leading to a percentage of mediation of 99%. This was due to a highly significant relation between GSE and motivational factors (β = 0.34, P < 0.001) and between motivational factors and SPPB (β = 0.49, P < 0.001).
Figure 2 .
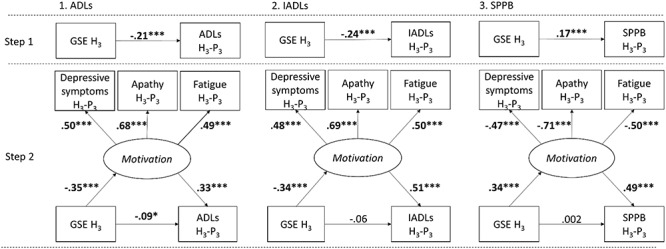
Final mediation model with standardised regression coefficients by using SEM. H3 = at discharge; H3–P3 = longitudinal (i.e. from discharge up to 3 months post-discharge). ***P < 0.001, *P < 0.05.
Discussion
This study found that GSE was associated with a worse course of physical performance outcomes among acutely hospitalised older patients up to 3 months post-discharge. However, when motivational factors such as depressive symptoms, apathy and fatigue were considered, motivational factors, but no longer GSE became significantly associated with both IADLs and SPPB. Motivational factors partially mediated the relationship between GSE and ADLs. An explanation for this finding could be that motivation may play a smaller role with many of the basic ADLs that recur at routine intervals compared with more complex activities [25]. With the repetition of behaviour in stable contexts, actions become more automatic in the sense that deliberation about actions is superfluous [25]. The findings of the current study show the importance of improving motivational factors to encourage older persons to become more physically active during and after acute hospitalisation.
Goal setting is essential to enhance motivation and to minimise the loss of functioning [26]. However, the implementation of a comprehensive goal-setting process in the context of an acute care setting is an ongoing problem [27], possibly due to a discrepancy between older patients and professionals regarding recovery goals [28]. Older patients wished to regain independence in ADLs [28], whereas professionals in the acute setting focussed on discharge-related goals, with the aim of getting patients ready for discharge as soon as possible [28, 29]. Moreover, given the high levels of physical inactivity during acute hospitalisation [30], it is conceivable that it may be difficult for older patients to achieve goals post-discharge. Therefore, it seems crucial that professionals set goals that are easy to accomplish [28] and they should make a distinction between goals that are important during acute hospitalisation and goals that are important to achieve post-discharge. Furthermore, among patients with depressive symptoms, it appears crucial to encourage them to think of goals as a process rather than as outcomes, [31] especially because these persons are more inclined to believe that wellbeing depends on achieving goals [32]. In other words, when addressing older patients’ long-term post-discharge goals, professionals should focus on a home rehabilitation approach that is adjusted to the individual activities and specific daily needs of the patient [33]. Previous home rehabilitation studies have been proven cost-effective [34, 35] and, perhaps more importantly, show beneficial effects on functional outcomes [36, 37]. To help older patients accomplish their goals, home rehabilitation interventions should be focussed on behavioural activation and exercises to improve mobility [38]. Therefore, thought should also be given to the use of sensor monitoring in combination with the coaching of cognitive behavioural therapy principles (of which goal setting is a component) by occupational therapists to improve ADL and physical activities back at home [39].
The current study has potential clinical implications for an acute hospital care setting. First, clinical training could be offered to physicians and healthcare professionals not accustomed to assessing psychiatric disorders in order to better detect the presence of proximal motivational risk factors to prevent poor performance outcomes. For example, symptoms of apathy are frequently reported among acutely hospitalised older adults [40], and depressive symptoms are often undiagnosed in older individuals [41], are highly persistent post-acute hospitalisation, and are associated with worse functional outcomes [42]. Second, professionals need to be aware of the high physical inactivity among acutely hospitalised older patients during hospitalisation [30, 43] and that they may be at high risk of having a passive attitude post-discharge. Education by professionals for patients and caregivers that discusses the importance of behavioural activation during and post-acute hospitalisation as well as the relation with activity engagement in older individuals may be helpful [44].
The main strength of this study was the use of a longitudinal research design, which made it possible to establish the influence of GSE (which was rather stable over time) on the temporal sequence of motivational factors and performance outcomes. Some limitations should also be noted. First, it is unclear whether depressive symptoms, apathy and/or fatigue were all full mediators because they are parts of a latent variable. However, these factors were chosen intentionally due to the fact that depressive symptoms, apathy, and fatigue are overlapping constructs (and often comorbid). Therefore, they have a good deal of shared variance. Second, the interpretation of being fatigued as a motivational concept might be questioned. Future research is needed to investigate the distinction between fatigue as a psychological or a physical aspect and its predictiveness of functional recovery. Finally, we were not able to include data on neither the history of depression nor previous or current treatment of depression because such data were often not included in hospital records. As a result, there was no control for the potential effect of related medication on depressive symptoms. Future research is warranted on the impact of antidepressant medication as a predictor, mediator or confounder in acutely hospitalised older patients.
Supplementary Material
Declaration of Conflicts of Interest:
None.
Funding:
This work was supported by The Netherlands Organization for Health Research and Development (NWO-ZonMw) (grant number 16156071 to B.B.). (a full list of 44 references can be found in the supplementary data, appendix 2).
References
- 1. Bandura A. Social Foundations of Thought and action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall, 1986. [Google Scholar]
- 2. Bandura A. Self-efficacy: The Exercise of Control. New York: W.H. Freeman and Company, 1997. [Google Scholar]
- 3. Chen G, Gully SM, Whiteman JA, Kilcullen RN. Examination of relationships among trait-like individual differences, state-like individual differences, and learning performance. J Appl Psychol 2000; 85: 835–47. [DOI] [PubMed] [Google Scholar]
- 4. Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol 2005; 139: 439–57. [DOI] [PubMed] [Google Scholar]
- 5. Bonetti D, Johnston M, Rodriguez-marin Jet al. Dimensions of perceived control: a factor analysis of three measures and an examination of their relation to activity level and mood in a student and cross-cultural patient sample. Psychol Health 2001; 16: 655–74. [Google Scholar]
- 6. Boyd CM, Landefeld CS, Counsell SRet al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc 2008; 56: 2171–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hoogendijk EO, Hout HP, Horst HEet al. Do psychosocial resources modify the effects of frailty on functional decline and mortality? J Psychosom Res 2014; 77: 547–51. [DOI] [PubMed] [Google Scholar]
- 8. Kempen GI, Sonderen E. Psychological attributes and changes in disability among low-functioning older persons: does attrition affect the outcomes? J Clin Epidemiol 2002; 55: 224–9. [DOI] [PubMed] [Google Scholar]
- 10. Esposito F, Gendolla GHE, Van der Linden M. Are self-efficacy beliefs and subjective task demand related to apathy in aging? Aging Ment Health 2014; 18: 521–30. [DOI] [PubMed] [Google Scholar]
- 11. Akin S, Kas GC. Investigation of the relationship among fatigue, self-efficacy and quality of life during chemotherapy in patients with breast, lung or gastrointestinal cancer. Eur J Cancer Care 2019; 28: e12898. [DOI] [PubMed] [Google Scholar]
- 13. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–98. [DOI] [PubMed] [Google Scholar]
- 14. Inouye SK, Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113: 941–8. [DOI] [PubMed] [Google Scholar]
- 15. Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA 1963; 185: 914–9. [DOI] [PubMed] [Google Scholar]
- 16. Bosscher RJ, Smit JH, Kempen GI. Algemene competentieverwachtingen bij ouderen: Een onderzoek naar de psychometrische kenmerken van de Algemene Competentieschaal (ALCOS)/Global expectations of self-efficacy in the elderly: an investigation of psychometric characteristics of the general self-efficacy scale. Nederlands Tijdschrift voor de Psychologie en haar grensgebieden 1997; 239–48. [Google Scholar]
- 19. van der Mast RC, Vinkers DJ, Stek MLet al. Vascular disease and apathy in old age. The Leiden 85-Plus Study. Int J Geriatr Psychiatry 2008; 23: 266–71. [DOI] [PubMed] [Google Scholar]
- 21. Eurelings LS, van Dalen JW, Ter Riet Get al. Apathy and depressive symptoms in older people and incident myocardial infarction, stroke, and mortality: a systematic review and meta-analysis of individual participant data. Clin Epidemiol 2018; 10: 363–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Laan W, Zuithoff NP, Drubbel Iet al. Validity and reliability of the Katz-15 scale to measure unfavorable health outcomes in community-dwelling older people. J Nutr Health Aging 2014; 18: 848–54. [DOI] [PubMed] [Google Scholar]
- 23. Guralnik JM, Simonsick EM, Ferrucci Let al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49: M85–94. [DOI] [PubMed] [Google Scholar]
- 24. Fiske ST, Gilbert DT, Lindze G. Handbook of Social Psychology. New Jersey: John Wiley & Sons Inc, 2010. [Google Scholar]
- 26. Schunk DH. Self-efficacy, motivation, and performance. J Appl Sport Psychol 1995; 7: 112–37. [Google Scholar]
- 28. Seben R, Smorenburg SM, Buurman BM. A qualitative study of patient-centered goal-setting in geriatric rehabilitation: patient and professional perspectives. Clin Rehabil 2019; 33: 128–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Street H. Exploring relationships between goal setting, goal pursuit and depression: a review. Aust Psychol 2002; 37: 95–103. [Google Scholar]
- 33. Wade D. Rehabilitation – a new approach. Overview and part one: the problems. Clin Rehabil 2015; 29: 1041–50. [DOI] [PubMed] [Google Scholar]
- 35. Sritipsukho P, Riewpaiboon A, Chaiyawat P, Kulkantrakorn K. Cost-effectiveness analysis of home rehabilitation programs for Thai stroke patients. J Med Assoc Thai 2010; 93: S262–70. [PubMed] [Google Scholar]
- 37. Stevens-Lapsley JE, Loyd BJ, Falvey JRet al. Progressive multi-component home-based physical therapy for deconditioned older adults following acute hospitalization: a pilot randomized controlled trial. Clin Rehabil 2016; 30: 776–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Verweij L, Korput E, Daams JGet al. Effects of postacute multidisciplinary rehabilitation including exercise in out-of-hospital settings in the aged: systematic review and meta-analysis. Arch Phys Med Rehabil 2019; 100: 530–50. [DOI] [PubMed] [Google Scholar]
- 39. Pol MC, Riet G, Hartingsveldt M, Kröse B, Rooij SE, Buurman BM. Effectiveness of sensor monitoring in an occupational therapy rehabilitation program for older individuals after hip fracture, the SO-HIP trial: study protocol of a three-arm stepped wedge cluster randomized trial. BMC Health Serv Res 2017; 17: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Reichardt LA, Nederveen FE, Seben Ret al. Hopelessness and other depressive symptoms in adults 70 years and older as predictors of all-cause mortality within 3 months after acute hospitalization: the Hospital-ADL study. Psychosom Med 2019; 81: 477–85. [DOI] [PubMed] [Google Scholar]
- 42. Reichardt LA, Seben R, Aarden JJet al. Trajectories of cognitive-affective depressive symptoms in acutely hospitalized older adults: the hospital-ADL study. J Psychosom Res 2019; 120: 66–73. [DOI] [PubMed] [Google Scholar]
- 44. Polenick CA, Flora SR. Behavioral activation for depression in older adults: theoretical and practical considerations. Behav Anal 2013 Spring; 36: 35–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


