Abstract
Introduction
Hypertension, particularly untreated, leads to serious complications and contributes to high costs incurred by the whole society. The aim of the review was to carry out a social and economic comparison of various categories of hypertension costs from different countries.
Material and methods
The study was a systematic review. PubMed, Cochrane Library and Google Scholar databases were searched. Hypertension costs were analyzed in 8 cost categories. An attempt was made to determine whether selected economic and social factors (such as HDI or GDP) influenced hypertension costs.
Results
The review included data from 15 countries: Brazil, Cambodia, Canada, China, Greece, Indonesia, Italy, Jamaica, Kyrgyzstan, Mexico, Poland, Spain, USA, Vietnam and Zimbabwe. The papers included in the review were heterogeneous with respect to cost categories, which made comparisons difficult. The average total costs of hypertension for all the studied countries, calculated per person, amounted to 630.14 Int$, direct costs – 1,497.36 Int$, and indirect costs – 282.34 Int$. The ranking of countries by costs and by selected economic and social indices points at the possible relationship between these indices and hypertension costs.
Conclusions
The costs of hypertension calculated per country reached the region of several dozen billion Int$. Other sources usually showed lower costs than those presented in this review. This indicates a growth in costs from year to year and the future increasing burden on society. Globally uniform cost terminology and cost calculation standards need to be developed. That would facilitate making more informed decisions regarding fund allocation in hypertension management schemes.
Keywords: hypertension costs, total costs, direct costs, indirect costs, hospital costs, drug costs, socioeconomic indices
Introduction
Cardiovascular diseases (CVDs) are the leading cause of morbidity and death globally. Hypertension (HT), together with dyslipidemia, is a major risk factor for CVDs [1], regardless of sex or ethnicity [2]. The etiology of high blood pressure is varied. With prevalence from 20% to even 50% in adults, HT is the most common condition in developed countries [3]. It is usually defined as blood pressure exceeding 140/90 mm Hg [4]. This definition was adopted for the purposes of this article as valid within the time scope covered in the review. However, according to the most recent guideline for hypertension of the American College of Cardiology (ACC), hypertension is defined as blood pressure exceeding 130/80 mm Hg [2].
As a risk factor for CVDs, HT is indirectly the leading cause of death and the third cause of disability globally [5]. Its long-term effects include damage to such organs as blood vessels, heart, and kidneys [6]. Frequent HT complications are left ventricular hypertrophy [7], heart failure [8], and stroke [9].
The aim of this study was to collect and compare data on the costs of hypertension management, morbidity, and mortality across different countries and across different cost categories. An attempt was made to adopt a global perspective, including cost data from as many countries in the world as possible. The aim of this approach was to identify the categories where the costs are the highest. Such information would allow for better planning of future healthcare spending, for example through changes in fund allocation or reorganization of hypertension care focused on primary prevention. Consequently, this could contribute to more cost-effective hypertension management. Additionally, the authors tried to go beyond the cost analysis and adopt a socio-economic perspective with the use of indices commonly used in international rankings.
The cost data come from original research papers analyzing the phenomenon for a particular country or a region of a country (such as Quebec in Canada or particular states in Mexico). HT costs were divided into the following categories: total costs – the sum of direct and indirect costs, direct costs connected with HT therapy (drugs, medical equipment, diagnostics, hospitalization, consultations, nursing, medical transport, etc.), indirect costs, i.e. economic losses caused by decreased productivity of employees (presenteeism), their absence from work caused by sickness (absenteeism) and premature deaths, hospital costs, i.e. those related specifically to hospitalization, drug costs, i.e. the costs related to the purchase and management of medications, pharmaceutical care costs, i.e. costs related to pharmacist’s participation in the treatment, out-of-pocket expenses, i.e. the expenses paid directly by the patient, and finally costs of stroke as a separate category of direct costs. Such cost classification and definitions are commonly used in pharmacoeconomic analyses, for instance in the study by Mitchell-Fearon et al. [10]. Since stroke is a frequent complication of HT, the costs of stroke were also included in the study. As was noted by Turin et al., the lifetime risk of stroke for men at the age of 45 was 17.21% for men without HT and 32.79% for hypertensive men [11].
Material and methods
According to the categories presented above, HT costs were calculated and presented in tables, either on a per patient basis or as a total. Additional analyses were carried out as regards cost structure. Finally, countries were ranked by costs and by selected socioeconomic indices in order to check whether an increase of costs coincided with an increase of particular indices.
Literature search
The search was carried out in PubMed, Cochrane and Google Scholar. In each case, the following search terms were used: hypertension costs, hypertension economic burden, hypertension economic impact, hypertension economic effects and hypertension social effects. The terms were searched for in both titles and abstracts. The following filters were used in PubMed: free full texts available, a publication date from 1 January 2014 to 31 December 2018, and English as the language of publication.
The filters used in Cochrane Library were: a trial as the type of study, and a publication date from 2014 to 2018.
In the Google Scholar database, the only filter used was a publication date from the year 2014 onwards. The default sorting by relevance was retained.
Out of the publications found, all of the results from PubMed and Cochrane Library databases were taken into account. By contrast, only the first 100 pages of search results from Google Scholar (sorted by relevance) were taken into account, as further pages presented results irrelevant to the search terms. In addition, reference lists of included publications were also searched manually to be able to include also paid publications from journals subscribed by our institution.
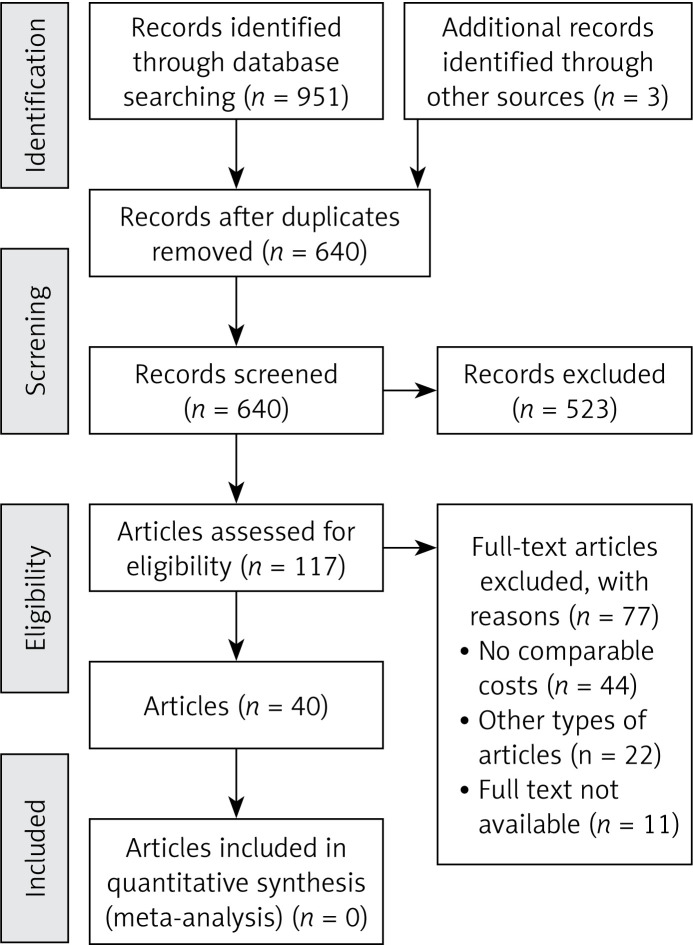
Selection was carried out by two authors independently in accordance with the PRISMA Statement [12]. First, duplicate records and articles not related to HT costs were excluded. Next, the authors excluded articles not available as the full text, those which were not original research, and those where the presented costs were not comparable. Studies based on forecasting (e.g. Markov modeling) were included on the assumption that the models used permit reliable cost estimates. Subsequently, the quality of the articles was assessed using the Downs and Black checklist [13]. As a result, 40 publications were included in the review. Since the data in the selected studies turned out not to be homogeneous enough, no meta-analysis was conducted (Figure 1).
Figure 1.
PRISMA flow diagram showing the record selection process
Synthesis of literature
The following information on the included articles was collated: the name of the main author, country or region described, study population, type of research, reference year for costs, and cost currency. All the extracted cost information was allocated to a specific cost category and, in the few cases where the cost was not given in international dollars (Int$), conversion was carried out. The exchange rates for this currency were taken from the databases of the World Bank [14] for the year given as a reference year for costs in a given study. If the reference year was not specified, it was assumed that the cost data refer to the year when a given study was accepted for publication. Amounts in local currencies were given using ISO 4217 currency codes. As the exchange rate for international dollars in relation to a local currency is always calculated on the basis of the purchasing power parity of the United States dollar (USD), the Int$/USD exchange rate always equals 1. In the case of a few Polish studies where costs were given in euro (EUR) despite the official Polish currency being the Polish zloty (PLN), the Int$/EUR exchange rate in Germany in a given year was used.
Results
When assessed for data quality (very low, low, moderate, high), 22 of the 40 publications presented data of low quality, 17 presented data of moderate quality, and 1 presented data of high quality. There were no publications with very low quality of data. The quality of a majority of publications was on the borderline between low and moderate.
Table I presents all the publications included in the review [10, 15–53]. Table II shows HT costs – divided into comparable categories – extracted from the publications included in the review.
Table I.
Details of the included studies
| Record | Country (region) | Population | Type of study | Reference year for costs (currency) | Purchasing power parity |
|---|---|---|---|---|---|
| Alvarez-Sabin 2016 [15] | Spain | 176 aged over 18 years, mean age 72.1 years (54.8% males) | Epidemiological, observational, prospective, multicenter study | 2012 (EUR) | Int$ 1 = 0.695 EUR |
| Arredondo 2015 [16] | Mexico | 654 701 reported cases of adults with hypertension | Cost estimation | 2015 (USD) | – |
| Arredondo 2016 [17] | Mexico (Hidalgo, Jalisco, Morelos, Sinaloa, Yucatán) | Unspecified | Time series study | 2015 (USD) | – |
| Bernard 2014 [18] | USA | 9383 aged 18–64 years (49.9% males) | Study based on data from the Medical Expenditure Panel Survey – Household Component (MEPS – HC) | 2009 (USD) | – |
| Bigdeli 2016 [19] | Cambodia | 1 250 aged over 18 years, mean age 56 years (33.0% males) | Cross-sectional household survey | 2014 (USD) | – |
| Boan 2014 [20] | USA | 84 179 aged over 25 years (35.5% blacks, 37.0% aged over 65 years) | Study based on data from the State Inpatient Hospital Discharge Database | 2014 (USD) | – |
| Boubouchairopoulou 2014 [21] | Greece | 116 aged over 30 years | Costs estimation | 2014 (EUR) | Int$ 1 = 0.611 EUR |
| Bueno 2017 [22] | Brazil | 806 aged over 60 years (39.1% males) | Cross-sectional study | 2015 (USD) | – |
| Cazarim 2018 [23] | Brazil | 104 aged 38–83 years | Cost-effectiveness study | 2015 (USD) | – |
| Finkelstein 2014 [24] | Indonesia | 10 795 mean age 53.3 years (47.8% males) | Study based on data from Indonesian Family Life Survey (IFLS) | 2008 (Int$) | – |
| Gilmer 2014 [25] | USA | 71 617 aged 3–17 years (49.0% males) | Prospective dynamic cohort study | 2010 (USD) | – |
| Huang 2016 [26] | China | 21 925 mean age 61.05 years (48.7% males) | Study based on data from National Health Services Utilization Survey | 2016 (CNY) | Int$ 1 = 3.473 CNY |
| Kawalec 2015 [27] | Poland | 74 745 mean age 59.7 years (41.5% males) | Cost estimation | 2014 (PLN) | Int$ 1 = 1.767 PLN |
| Kirkland 2018 [28] | USA | 83 018 aged 18–85 years (45.6% males) | Study based on data from Medical Expenditure Panel Survey | 2016 (USD) | – |
| Lekoubou 2018 [29] | USA | 7421 aged 18–85 years (45.4% males) | Study based on data from Medical Expenditure Panel Survey Household Component | 2016 (USD) | – |
| Liu 2016 [30] | China | 414 mean age 64.3 years (34.1% males) | Study based on data from Cross-sectional surveys | 2015 (CNY) | Int$ 1 = 3.478 CNY |
| Marra 2017 [31] | Canada | Mean age 63.5 years (48.8% males) | Cost-effectiveness study | 2015 (CAD) | Int$ 1 = 1.247 CAD |
| Milan 2017 [32] | Canada (Quebec) | 881 aged over 65 years (36.6% males) | Study based on data from “Étude sur la santé des aînés” | 2017 (CAD) | Int$ 1 = 1.251 CAD |
| Mitchell-Fearon 2017 [10] | Jamaica | 2 934 aged over 60 years (47.9% males) | Cost estimation | 2012 (USD) | – |
| Moise 2016 [33] | USA | 35–74 years | Cost estimation | 2016 (USD) | – |
| Murphy 2016 [34] | Kyrgyzstan | 9109 (47.7% males) | Study based on data from Kyrgyzstan Integrated Household Survey (KIHS) | 2016 (USD) | – |
| Mutowo 2016 [35] | Zimbabwe | 344 mean age 58.6 years (36.3% males) | Retrospective study based on secondary data from medical records | 2016 (USD) | – |
| Nguyen 2014 [36] | Vietnam | 230 mean age 64.3 years (46.5% males) | Retrospective study | 2011 (USD) | – |
| Paczkowska 2014 [37] | Poland | 480 aged 16–18 years (69.4% males) | Retrospective study | 2013 (EUR) | Int$ 1 = 0.775 EUR |
| Park 2017 [38] | USA | 26 049 aged over 18 years (49.0% males) | Study based on data from Medical Expenditure Panel Survey | 2014 (USD) | – |
| Ricci 2017 [39] | Italy | Unspecified | Cost estimation | 2011 (EUR) | Int$ 1 = 0.759 EUR |
| Ritchey 2016 [40] | USA | Over 18 years | Study based on data from IMS Health’s National Prescription Audit | 2015 (USD) | – |
| Shireman 2016 [41] | USA | 494 mean age 53.5 years (35% males, 100% blacks) | Cost-effectiveness study | 2015 (USD) | – |
| Specogna 2017 [42] | Canada | 987 mean age 72 years (55% males) | Cohort study | 2017 (USD) | – |
| Stafylas 2015 [43] | Greece | Mean age 53.2 years (55.3% males) | Cost-utility study | 2013 (EUR) | Int$ 1 = 0.631 EUR |
| Tajeu 2017 [44] | USA | 30 239 over 45 years mean age 66.8 years (44.5% males) | Cost-utility study | 2012 (USD) | – |
| Tamblyn 2018 [45] | Canada (Quebec) | 3592 over 18 years (44.7% males) | Single-blind cluster randomized trial | 2017 (CAD) | Int$ 1 = 1.251 CAD |
| Vasudeva 2016 [46] | USA | 35–74 years | Cost-effectiveness study | 2015 (USD) | – |
| Wang G. 2017 [47] | USA | 40 746 over 18 years (59.0% males) | Study based on data from Medical Expenditure Panel Survey | 2014 (USD) | – |
| Wang G., Fang J. 2014 [48] | USA | Over 25 years, mean age 67.8 years | Study based on data from National Hospital Discharge Survey | 2008 (USD) | – |
| Wang G., Zhang Z. 2014 [49] | USA | 18–64 years | Study based on data from MarketScan inpatient database | 2008 (USD) | – |
| Wang Q. 2014 [50] | China | 1528 over 18 years | Study based on data on medical payments | 2014 (USD) | – |
| Wang Z. 2017 [51] | China | 793 aged 18–70 years, mean age 56.3 years (59.0% males) | Cost-effectiveness study, randomized, open-label, prospective clinical trial | 2016 (USD) | – |
| Weaver 2015 [52] | Canada | 608 157 mean age 62.3 years (48.6% males) | Study based on data from Alberta Kidney Disease Network | 2014 (CAD) | Int$ 1 = 1.23 CAD |
| Zhang 2017 [53] | USA | Over 18 years | Study based on data from Medical Expenditure Panel Survey | 2015 (USD) | – |
Table II.
Costs of arterial hypertension
| Record | Total costs (TC)/Total costs per person (TCpp) Direct costs (DC)/Direct costs per person (DCpp) Indirect costs (IC)/Indirect costs per person (ICpp) | Hospital costs (HC)/ Hospital costs per person (HCpp) Hospital costs per admission (HCpa) Drug costs (DrC)/Drug costs per person (DrCpp) | Pharmaceutical care costs (PCC)/Pharmaceutical care costs per person (PCCpp) Out-of-pocket expenses (OOPE) Costs of stroke (COS)/Costs of stroke per person (COSpp) |
|---|---|---|---|
| Alvarez-Sabin 2016 [15] | 41,575.54 Int$ (COSpp) | ||
| Arredondo 2015 [16] | 6,880,020,349.00 Int$ (TC) 3,261,937,129.00 Int$ (DC) 3,618,083,220.00 Int$ (IC) |
358,812,888.00 Int$ (HC) 456,671,390.00 Int$ (DrC) |
411,003,513.00 Int$ (COS) |
| Arredondo 2016 [17] | 8,297,635.00 Int$ (DC – Hidalgo)/796.17 Int$ (DCpp – Hidalgo) 18,413,820.00 Int$ (DC – Jalisco)/590.77 Int$ (DCpp – Jalisco) 10,007,786.00 Int$ (DC – Morelos)/625.10 Int$ (DCpp – Morelos) 14,769,269.00 Int$ (DC – Sinaloa)/470.27 Int$ (DCpp – Sinaloa) 5,485,622.00 Int$ (DC – Yucatán)/579.57 Int$ (DCpp – Yucatán) |
||
| Bernard 2014 [18] | 174.00 Int$ (OOPE) | ||
| Bigdeli 2016 [19] | 399.00 Int$ (DCpp) | 350.00 Int$ (DrCpp) | |
| Boan 2014 [20] | 2,770,000,000.00 Int$ (COS) | ||
| Boubouchairopoulou 2014 [21] | 2,411.62 Int$ (DCpp) | 405.24 Int$ (DrCpp) | |
| Bueno 2017 [22] | 30.23 Int$ (DrCpp) | ||
| Cazarim 2018 [23] | 23,350.38 Int$ (PCC)/224.52 Int$ (PCCpp) | ||
| Finkelstein 2014 [24] | 1,320,000,000.00 Int$ (TC)/70.00 Int$ (TCpp) 540,000,000.00 Int$ (DC)/30.00 Int$ (DCpp) 780,000,000.00 Int$ (IC)/50.00 Int$ (ICpp) |
290,000,000.00 Int$ (COS)/380.00 Int$ (COSpp) |
|
| Gilmer 2014 [25] | 1,972.00 Int$ (DCpp) | ||
| Huang 2016 [26] | 193.32 Int$ (DCpp) | 2,967.90 Int$ (HCpa) | 45.68 Int$ (OOPE) |
| Kawalec 2015 [27] | 9,439.26 Int$ (OOPE) | ||
| Kirkland 2018 [28] | 9,089.00 Int$ (DCpp) | 2,731.00 Int$ (HCpp) 2,371.00 Int$ (DrCpp) |
|
| Lekoubou 2018 [29] | 316,000,000,000.00 Int$ (TC) 193,000,000,000.00 Int$ (DC) 123,000,000,000.00 Int$ (IC) |
98,300,000,000.00 Int$ (COS)/17,165.00 Int$ (COSpp) |
|
| Liu 2016 [30] | 1,936.23 Int$ (HCpa) | ||
| Marra 2017 [31] | 209,658.38 Int$ (PCC) 64,093.83 Int$ (COSpp) |
||
| Milan 2017 [32] | 28.78 Int$ (OOPE) | ||
| Mitchell-Fearon 2017 [10] | 204,676,723.54 Int$ (TC)/1,190.28 Int$ (TCpp) 116,173,000.90 Int$ (DC)/675.59 Int$ (DCpp) 88,503,722.64 Int$ (IC)/514.68 Int$ (ICpp) |
10,851,082.11 Int$ (HC)/3.10 Int$ (HCpp) 37,038,595.58 Int$ (DrC)/215.39 Int$ (DrCpp) |
3,000.00 Int$ (OOPE) |
| Moise 2016 [33] | 11,994.00 Int$ (HCpp) | 26,000.00 Int$ (COSpp) | |
| Murphy 2016 [34] | 12.70 Int$ (OOPE) | ||
| Mutowo 2016 [35] | 914.00 Int$ (HCpa) | ||
| Nguyen 2014 [36] | 64.95 Int$ (HCpa) | ||
| Paczkowska 2014 [37] | 116.08 Int$ (DCpp) | 159.82 Int$ (HCpp) 68.84 Int$ (DrCpp) |
|
| Park 2017 [38] | 9,841.00 Int$ (DCpp) | 9,555.00 Int$ (COSpp) | |
| Ricci 2017 [39] | 3,666,930,171.28 Int$ (DC) | ||
| Ritchey 2016 [40] | 28,810,000,000.00 Int$ (DrC) | 359.00 Int$ (OOPE) | |
| Shireman 2016 [41] | 104.80 Int$ (PCCpp) | ||
| Specogna 2017 [42] | 12,856.72 Int$ (COSpp) | ||
| Stafylas 2015 [43] | 4,154.65 Int$ (HCpp) 10,877.88 Int$ (DrCpp) |
||
| Tajeu 2017 [44] | 189.48 Int$ (DrCpp) | 69,642.00 Int$ (COSpp) | |
| Tamblyn 2018 [45] | 436.77 Int$ (DrCpp) | 209.03 Int$ (OOPE) | |
| Vasudeva 2016 [46] | 12,000.00 Int$ (HCpp) | 26,000.00 Int$ (COSpp) | |
| Wang G. 2017 [47] | 8,854.00 Int$ (DCpp) | ||
| Wang G., Fang J. 2014 [48] | 113,390,000,000.00 Int$ (HC) 8,480.00 Int$ (HCpa) |
||
| Wang G., Zhang Z. 2014 [49] | 23,256.00 Int$ (COSpp) | ||
| Wang Q. 2014 [50] | 93.50 Int$ (OOPE) | ||
| Wang Z. 2017 [51] | 63.40 Int$ (DrCpp) | ||
| Weaver 2015 [52] | 11,300,813,008.13 Int$ (DC)/1,903.25 Int$ (DCpp) |
||
| Zhang 2017 [53] | 1494.00 USD Int$ (DCpp) |
The lowest cost values were observed 9 times in Indonesia, 6 times in Jamaica, 3 times in Brazil, twice in Mexico, once in Kyrgyzstan, once in the USA, and once in Vietnam. The highest cost values were observed 15 times in the USA, twice in Jamaica, twice in Canada, once in Brazil, once in Greece, once in Spain, and once in Poland (Table III).
Table III.
Lowest cost/highest cost/range/average for all countries/standard deviation
| Type of costs | Lowest cost | Highest cost | Difference between the lowest and the highest cost | Average for all countries | Standard deviation |
|---|---|---|---|---|---|
| Total costs | 204 676 723.54 Int$ (Jamaica) | 316 000 000 000.00 Int$ (USA) | 315 795 323 276.46 Int$ | 81 101 174 268.14 Int$ | 156 626 431 466.60 Int$ |
| Total costs per person | 70.00 Int$ (Indonesia) | 1 190.28 Int$ (Jamaica) | 1 120.28 Int$ | 630.14 Int$ | 792.16 Int$ |
| Direct costs | 116 173 000.90 Int$ (Jamaica) | 193 000 000 000.00 Int$ (USA) | 192 883 826 999.10 Int$ | 35 314 308 884.89 Int$ | 77 354 376 229.69 Int$ |
| Direct costs per person | 30.00 Int$ (Indonesia) | 6 250.00 Int$ (USA) | 6 220.00 Int$ | 1 497.36 Int$ | 950.18 Int$ |
| Indirect costs | 88 503 722.64 Int$ (Jamaica) | 123 000 000 000.00 Int$ (USA) | 122 911 496 277.36 Int$ | 31 871 646 735.66 Int$ | 60 771 427 761.53 Int$ |
| Indirect costs per person | 50.00 Int$ (Indonesia) | 514.68 Int$ (Jamaica) | 464.68 Int$ | 282.34 Int$ | 328.58 Int$ |
| Hospital costs | 10 851 082.11 Int$ (Jamaica) | 113 390 000 000.00 Int$ (USA) | 113 379 148 917.89 Int$ | 37 919 887 990.04 Int$ | 65 359 265 788.81 Int$ |
| Hospital costs per person | 3.10 Int$ (Jamaica) | 8 908.33 Int$ (USA) | 8 905.23 Int$ | 3 306.48 Int$ | 4 199.76 Int$ |
| Hospital costs per admission | 64.95 Int$ (Vietnam) | 8 480.00 Int$ (USA) | 8 415.05 Int$ | 2 977.76 Int$ | 3 798.88 Int$ |
| Drug costs | 37 038 595.58 Int$ (Jamaica) | 28 810 000 000.00 Int$ (USA) | 28 772 961 404.42 Int$ | 9 767 903 328.53 Int$ | 16 492 274 165.65 Int$ |
| Drug costs per person | 30.23 Int$ (Brazil) | 5 641.56 Int$ (Greece) | 5 611.33 Int$ | 1 092.81 Int$ | 2 052.85 Int$ |
| Pharmaceutical care costs | 23 350.38 Int$ (Brazil) | 209 658.38 Int$ (Canada) | 186 308 Int$ | 116 504.38 Int$ | 131 739.65 Int$ |
| Pharmaceutical care costs per person | 104.80 Int$ (USA) | 224.52 Int$ (Brazil) | 119.72 Int$ | 164.66 Int$ | 84.65 Int$ |
| Out-of-pocket expenses | 12.70 Int$ (Kyrgyzstan) | 9 439.26 Int$ (Poland) | 9 426.56 Int$ | 2 557.61 Int$ | 4 045.64 Int$ |
| Costs of stroke | 290 000 000.00 Int$ (Indonesia) | 50 535 000 000.00 Int$ (USA) | 50 245 000 000.00 Int$ | 17 078 667 837.67 Int$ | 28 974 096 737.95 Int$ |
| Costs of stroke per person | 380.00 Int$ (Indonesia) | 41 575.54 Int$ (Spain) | 41 195.54 Int$ | 27 258.46 Int$ | 18 753.27 Int$ |
On average, direct costs turned out to constitute a slightly bigger share (51.5%) of the total costs than indirect costs (48.5%). Generally, it can be assumed that the proportion of one type of costs to the other does not exceed 60% vs. 40%. Such analysis of cost structure was carried out for only four countries, since only in these cases were all the necessary data (i.e. total costs, direct costs and indirect costs) available (Table IV).
Table IV.
Proportions of direct and indirect costs in total costs
| Country | Direct costs (%) | Indirect costs (%) |
|---|---|---|
| Indonesia | 41 | 59 |
| Jamaica | 57 | 43 |
| Mexico | 47 | 53 |
| USA | 61 | 39 |
| Average | 51.5 | 48.5 |
On average, the biggest share in the cost structure is that of other costs (53.33%) and hospital costs (26.33%), while the smallest share is that of drug costs (20.33%). A possible reason for the considerable differences in the cost structure between the analyzed countries is, apart from the specific character of each country, the different methodology of gathering component data. This analysis was carried out for only three countries for which all the necessary data (i.e. direct costs, hospital costs and drug costs) were available (Table V).
Table V.
Cost structure within direct costs
| Country | Hospital costs (%) | Drug costs (%) | Other costs (%) |
|---|---|---|---|
| Jamaica | 9 | 32 | 59 |
| Mexico | 11 | 14 | 75 |
| USA | 59 | 15 | 26 |
| Average | 26.33 | 20.33 | 53.33 |
Additional socio-economic data are presented in Tables VI and VII.
Table VI.
Total hypertension costs versus selected social and economic indices: Human Development Index in 2017, coverage of essential health services, physicians (per 1,000 people), total number of NCD deaths, prevalence of obesity with BMI > 30 (% of population 18+), harmful use of alcohol, defined according to the national context as alcohol per capita consumption (in population 15+) within a calendar year in liters of pure alcohol, prevalence of insufficient physical activity (% of population 18+, age-standardized estimate)
| Country (rank in the world, group of countries*) | Total costs (rank in the current comparison) | Human Development Index (rank in the current comparison) | Coverage of essential health services (rank in the current comparison) | Physicians (per 1,000 people) (rank in the current comparison) | Total number of NCD deaths (rank in the current comparison) | Prevalence of obesity, BMI > 30 (% of population 18+) (rank in the current comparison) | Harmful use of alcohol (rank in the current comparison) | Prevalence of insufficient physical activity (% of population 18+, age-standardized estimate) (rank in the current comparison) |
|---|---|---|---|---|---|---|---|---|
| USA (13, VH) | 316,000,000,000.00 Int$ (1) | 0.924 (1) | 80 (1) | 2.568 (1) | 2,343,000 (1) | 36.2 (1) | 9.8 (1) | 40.0 (1) |
| Mexico (74, H) | 6,880,020,349.00 Int$ (2) | 0.774 (2) | 76 (2) | 2.231 (2) | 492,000 (3) | 28.9 (2) | 6.5 (2) | 28.9 (3) |
| Indonesia (116, M) | 1,320,000,000.00 Int$ (3) | 0.694 (4) | 49 (4) | 0.201 (4) | 1,340,000 (2) | 6.9 (4) | 0.8 (4) | 22.6 (4) |
| Jamaica (97, H) | 204,676,723.54 Int$ (4) | 0.732 (3) | 60 (3) | 0.472 (3) | 15,000 (4) | 24.7 (3) | 4.2 (3) | 32.6 (2) |
VH – very high human development, H – high human development, M – medium human development, L – low human development, according to 2018 HDI ranking of 189 countries.
Table VII.
Total hypertension costs per person vs. other cost-related indices: GDP per capita, PPP (current international $), current health expenditure (% of GDP), current health expenditure per capita, PPP (current international $), domestic general government health expenditure per capita, PPP (current international $), out-of-pocket expenditure per capita, PPP (current international $)
| Country | Total costs per person (rank in the current comparison) | GDP per capita, PPP (current international $) (rank in the current comparison) | Current health expenditure (% of GDP) (rank in the current comparison) | Current health expenditure per capita, PPP (current international $) (rank in the current comparison) | Domestic general government health expenditure per capita, PPP (current international $) (rank in the current comparison) | Out-of-pocket expenditure per capita, PPP (current international $) (rank in the current comparison) |
|---|---|---|---|---|---|---|
| USA | 977.10 Int$ (1) | 53.129 (1) | 8.478 (1) | 9,535.95 (1) | 4,801.94 (1) | 1,057.00 (1) |
| Jamaica | 72.04 Int$ (2) | 4.798 (3) | 3.472 (2) | 511.38 (3) | 299.61 (3) | 121.22 (4) |
| Mexico | 54.65 Int$ (3) | 9.946 (2) | 3.059 (3) | 1,008.68 (2) | 526.21 (2) | 417.29 (2) |
| Indonesia | 5.76 Int$ (4) | 4.131 (4) | 1.279 (4) | 369.29 (4) | 141.05 (4) | 178.37 (3) |
Discussion
No reviews were found with a scope so wide as the scope of this review. The only study covering more than one country was that by Mullins 2004 [54], which compared hospital costs and outpatient treatment costs for HT complications, including stroke. Therefore, the data from this review were compared mainly to studies covering individual countries.
In one study carried out in the USA (Benjamin 2019) [55], total HT costs were estimated at 55,900,000,000 USD, direct costs at 51,300,000,000 USD, and indirect costs at 4,600,000,000 USD (with the last amount seeming grossly underestimated). The current review estimates HT costs in the USA as follows: total costs – 316,000,000,000 Int$, direct costs – 193,000,000,000 Int$, indirect costs – 123,000,000,000 Int$. The USD-Int$ exchange rate is always 1 : 1. The data presented in this review seem to be more reliable. According to a recent study from Australia, indirect HT costs amount to 137,200,000,000 AUD (Hird 2019) [56].
Goetzel estimated direct costs per capita in the USA at 392 USD (Goetzel 2004) [57], while Burnier suggested a much wider range between 4,871 and 11,238 USD, depending on patient compliance as regards medication (Burnier 2019) [58]. Owing to the generally high prices in the USA, direct costs per person in the region of several thousand USD appear to be more realistic than amounts in the region of a few hundred USD. The high costs in the USA are also confirmed by the current review, where direct costs per person are estimated at 6,250.00 Int$ in the USA, and 1,903.25 Int$ in Canada.
The British National Health Service spends 250,000,000 GBP (pound sterling) annually only on angiotensin II receptor blockers used as antihypertensive medications (Grosso 2011) [59]. In 2010 in Malaysia, the annual cost of HT drugs was estimated to be 6,273.70 MYR per patient [60]. There are also studies reporting pharmacotherapy costs in dollars per quality-adjusted life-year (QALYs) gained. They were not included in this review due to difficulty comparing financial costs with costs per QALY. For example, in the Republic of South Africa drug costs in dollars per QALYs gained ranged from 700 to 11,000 USD, depending on the number of cardiovascular risk factors present (Gaziano 2005) [61]. In the USA, drug costs per QALY are as follows: angiotensin-converting-enzyme inhibitors – 34,244 USD, calcium channel blockers – 13,016 USD, β-blockers – from 1,498 to 18,137 USD (Park 2017) [62]. In the USA, drug costs per hospitalized person treated with sacubitril/valsartan amount to 248 USD, while costs per hospitalized person treated with angiotensin-converting-enzyme inhibitors or angiotensin II receptor blockers amount to 1,122 USD (Albert 2019) [63]. Thus, the sacubitril/valsartan treatment seems the most cost-effective pharmacological treatment. This review estimates the mean drug costs for all the analyzed countries at 9,767,903,328.53 Int$ in total and at 1,092.81 Int$ per person.
Among the studies exploring costs of stroke, the most comprehensive is that by Mullins (2004), estimating post-stroke hospitalization costs per person to be 23,109 USD in Canada, 16,415 USD in the USA, 7,703 USD in Spain, 5,003 USD in France, 4,980 USD in Italy, 4,567 USD in Germany, 2,639 USD in Australia and 2,607 USD in the UK. According to the same study, post-stroke inpatient care costs per person amount to 31,694 USD in the USA, 14,188 USD in France, 12,744 USD in Australia, 7,188 USD in Germany, 3,094 USD in Spain, and 606 USD in the UK (Mullins 2004) [64]. According to a different estimate, stroke costs per person in Canada equal 110,471 CAD (Canadian dollar) (Anis 2006) [65]. In Finland, they were estimated to reach 1,600,000,000 USD annually, while costs per person for a year after a stroke ranged from 29,580 to 42,570 USD depending on the kind of stroke, with higher costs generated by hemorrhagic strokes related to HT (Meretoja 2007) [66]. In Sweden, stroke costs per person for a year after a stroke ranged from 15,970 to 39,254 USD depending on stroke severity (Claesson 2000) [62]. According to European research, hospital costs per admission caused by strokes ranged from 466 USD in Latvia to 8,512 USD in Denmark (Grieve 2001) [67]. In the UK, post-stroke rehabilitation costs ranged from 326 to 19,901 GBP per person (Luengo-Fernandez 2006) [68]. In Canada, post-hospital care for stroke patients after early supported discharge was estimated to cost 7,748 USD per person, while traditional hospital care was estimated to cost 11,065 USD per person (Teng 2003) [69]. To compare, this review estimates mean stroke costs for all the analyzed countries at 17,078,667,837.67 Int$ in total, and 27,258.46 Int$ per person.
Other interesting conclusions can be reached when comparing selected indices of the social and economic situation of the studied countries with HT costs reported for these countries (Tables VI and VII). Full consistency was observed between the ranking of the countries according to HT costs and their ranking according to health expenditure as a percentage of gross domestic product (GDP). Similar (but not always full) consistency can be seen for countries ranked by HT costs and by other indices such as Human Development Index (HDI), GDP per capita (Int$), health expenditure per capita (Int$), domestic general government health expenditure per capita (Int$), out-of-pocket expenses (Int$), coverage of essential health services, the number of physicians per 1,000 population, the number of deaths caused by NCDs (non-communicable diseases), the percentage of the population aged 18 years or older with BMI (body mass index) > 30, the number of liters of pure alcohol consumed per person aged 15 years or older, and the age-standardized prevalence of insufficient physical activity in the population aged 18 years or older. The analyses of the convergence between country rankings based on these indices and country rankings based on HT costs showed one difference in each case, i.e. one country holding a different rank in one of the paired rankings. The country was usually Jamaica, whose position in cost rankings was lower than the position suggested by rankings of the particular socioeconomic indices (Tables VI and VII).
The results suggest that the indices mentioned above may influence HT costs. The two questions for future research are, whether there is a causal relationship between the indices and the costs, and how strong the influence is. Such analyses should involve a bigger, representative number of countries, with a bigger number of sources providing reliable data.
The authors admit that the present review has a number of limitations. The studies analyzed in the review cover only 15 countries, thus excluding almost 65% of the global population and such populous countries as India. The review data came from only 3 sources (PubMed, Cochrane, and Google Scholar), and numerous relevant studies were presumably not listed there. As the search algorithm of Google Scholar is not known, it could only be treated as an additional source. The current review included few studies describing HT costs in European countries. Some cost categories, e.g. prevention costs, were missing; other categories were presented in such a way that making comparisons of similar data from different sources turned out to be impossible. Moreover, the information was often fragmentary – no country had a complete set of data presenting all cost categories and methods of calculating them. Consequently, costs in some categories may be skewed, i.e. over- or under-estimated, when the data for these categories included countries with particularly high or low healthcare expenditures. It should also be noted that the HT definition used for the purposes of this review is blood pressure exceeding 140/90 mm Hg, while the 2017 ACC Guideline for Hypertension sets the limit at 130/80 mm Hg [2]. The more lenient limit was adopted here because the cost data included in the review come partly from before the year 2017.
In conclusion, the current review collated data from countries whose populations altogether constitute over 35% of the global population. They include some of the most populous countries in the world: China, the USA, Indonesia, Brazil. Although the databases selected for the review provided numerous records whose titles suggested relevance to HT costs, the records actually did not pertain to HT costs or sometimes even to HT itself. The 40 articles finally included in the review turned out to be very heterogeneous with respect to the cost categories and cost sources discussed, which made comparing the data difficult. The quality of data was mostly low or moderate and fitted in the 2 middle quality categories out of 4 (very low, low, moderate, high). Additional analyses showed interesting relations between direct and indirect costs, as well as within the structure of direct costs between hospital costs, drug costs and other costs. A comparison of country rankings according to costs and according to selected economic and social indices presented an increase of costs parallel to an increase of the indices.
When compared with other studies, this review usually listed higher HT costs. This may be due to the fact that the review included articles from the last 5 years, while the literature for discussion was selected from a slightly longer period. This can testify to the fact that healthcare costs, including HT costs, are growing year by year. The trend is corroborated by the World Bank data [70]. One can expect that HT costs will be an increasingly heavy burden on society, so continuous research pertaining to this problem is necessary. To achieve this, it is necessary to develop official and uniform cost terminology and definitions and to introduce uniform standards for calculating healthcare costs to make cost comparisons easier. The improvement of data collection and publication methods would also greatly facilitate the process. All of the above measures would enable better monitoring and analysis of cost types and cost centers, which would facilitate making more informed decisions regarding fund allocation in health policies.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Dai S, Huang B, Zou Y, Liu Y. Associations of dipping and non-dipping hypertension with cardiovascular diseases in patients with dyslipidemia. Arch Med Sci. 2019;15:337–42. doi: 10.5114/aoms.2018.72609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:1269–324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 3.Bielecka-Dabrowa A, Aronow WS, Rysz J, Banach M. The rise and fall of hypertension: lessons learned from Eastern Europe. Curr Cardiovasc Risk Rep. 2011;5:174–9. doi: 10.1007/s12170-010-0152-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Du Z, Bian W, Wu S, et al. Effects of blood pressure goals on cardiovascular outcomes in hypertensive patients. Arch Med Sci. 2018;15:1381–7. doi: 10.5114/aoms.2018.80013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chruściel P, Stemplewska P, Stemplewski A, et al. Associations between the lipid profile and the development of hypertension in young individuals – the preliminary study. Arch Med Sci. journal doi: 10.5114/aoms.2019.86197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miazgowski T, Kopec J, Widecka K, Miazgowski B, Kaczmarkiewicz A. Epidemiology of hypertensive heart disease in Poland: findings from the Global Burden of Disease Study 2016. Arch Med Sci. journal doi: 10.5114/aoms.2019.85222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Irzmanski R, Barylski M, Banach M, et al. The concentration of atrial and brain natriuretic peptide in patients with idiopathic hypertension. Med Sci Monit. 2007;13:449–56. [PubMed] [Google Scholar]
- 8.Bielecka-Dabrowa A, Gluba-Brzózka A, Michalska-Kasiczak M, Misztal M, Rysz J, Banach M. The multi-biomarker approach for heart failure in patients with hypertension. Int J Mol Sci. 2015;16:10715–33. doi: 10.3390/ijms160510715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pistoia F, Sacco S, Degan D, Tiseo C, Ornello R, Carolei A. Hypertension and stroke: epidemiological aspects and clinical evaluation. High Blood Press Cardiovasc Prev. 2016;23:9–18. doi: 10.1007/s40292-015-0115-2. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell-Fearon K, McKoy-Davis J, Willie-Tyndale D, Abdulkadri AO, Eldemire-Shearer D. The economic burden of hypertension among older persons: lessons from a developing nation. J Public Health Dev Ctries. 2017;3:347–57. [Google Scholar]
- 11.Turin TC, Okamura T, Afzal AR, et al. Hypertension and lifetime risk of stroke. J Hypertens. 2016;34:116–22. doi: 10.1097/HJH.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 12.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 13.Downs H, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The World Bank PPP conversion factor. https://data.worldbank.org/indicator/PA.NUS.PPP?end=2017&start=2017&view=map (access: 1 July 2019)
- 15.Alvarez-Sabın J, Quintana M, Masjuan J, et al. Economic impact of patients admitted to stroke units in Spain. Eur J Health Econ. 2017;18:449–58. doi: 10.1007/s10198-016-0799-9. [DOI] [PubMed] [Google Scholar]
- 16.Arredondo A, Cuadra SM, Duarte MB. Challenges of the epidemiological and economic burdens associated with hypertension in middle income countries: evidence from Mexico. BMC Public Health. 2015;15:1106. doi: 10.1186/s12889-015-2430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arredondo A, Orozco E, Alcalde-Rabanal J, Navarro J, Azar A. Challenges on the epidemiological and economic burden of diabetes and hypertension in Mexico. Rev Saude Publica. 2018;52:23. doi: 10.11606/S1518-8787.2018052000293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bernard DM, Johansson P, Fang Z. Out-of-pocket healthcare expenditure burdens among nonelderly adults with hypertension. Am J Manag Care. 2014;20:406–13. [PubMed] [Google Scholar]
- 19.Bigdeli M, Jacobs B, Men CR, Nilsen K, Van Damme W, Dujardin B. Access to treatment for diabetes and hypertension in rural cambodia: performance of existing social health protection schemes. PLoS One. 2016;11:e0146147. doi: 10.1371/journal.pone.0146147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boan AD, Feng WW, Ovbiagele B. Persistent racial disparity in stroke hospitalization and economic impact in young adults in the buckle of stroke belt. Stroke. 2014;45:1932–8. doi: 10.1161/STROKEAHA.114.004853. [DOI] [PubMed] [Google Scholar]
- 21.Boubouchairopoulou N, Karpettas N, Athanasakis K. Cost estimation of hypertension management based on home blood pressure monitoring alone or combined office and ambulatory blood pressure measurements. J Am Soc Hypertens. 2014;8:732–8. doi: 10.1016/j.jash.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 22.Bueno DR, de Fátima Nunes Marucci M, Gobbo LA, de Almeida-Roediger M, de Oliveira Duarte YA, Lebrão ML. Expenditures of medicine use in hypertensive/diabetic elderly and physical activity and engagement in walking: cross secctional analysis of SABE Survey. BMC Geriatrics. 2017;17:70. doi: 10.1186/s12877-017-0437-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cazarim MS, Pereira LRL. Cost-effectiveness analysis of pharmaceutical care for hypertensive patients from the perspective of the public health system in Brazil. PLoS One. 2018;13:e0193567. doi: 10.1371/journal.pone.0193567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finkelstein EA, Chay J, Bajpai S. The economic burden of self-reported and undiagnosed cardiovascular diseases and diabetes on indonesian households. PLoS One. 2014;9:e99572. doi: 10.1371/journal.pone.0099572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gilmer TP, O’Connor PJ, Sinaiko AR. Impact of hypertension on health care costs among children. Am J Manag Care. 2014;20:622–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Huang Y, Liu Y, Yang X, Li J, Fang P. Global budget payment system helps to reduce outpatient medical expenditure of hypertension in China. SpringerPlus. 2016;5:1877. doi: 10.1186/s40064-016-3565-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kawalec P, Holko P, Stawowczyk E, Borowiec Ł, Filipiak KJ. Economic evaluation of single-pill combination of indapamide and amlodipine in the treatment of arterial hypertension in the Polish setting. Kardiol Pol. 2015;73:768–80. doi: 10.5603/KP.a2015.0089. [DOI] [PubMed] [Google Scholar]
- 28.Kirkland EB, Heincelman M, Bishu KG, et al. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003–2014. J Am Heart Assoc. 2018;7:e008731. doi: 10.1161/JAHA.118.008731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lekoubou A, Bishu KG, Ovbiagele B. Nationwide healthcare expenditures among hypertensive individuals with stroke: 2003-2014. J Stroke Cerebrovasc Dis. 2018;27:1760–9. doi: 10.1016/j.jstrokecerebrovasdis.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 30.Liu X, Sun X, Zhao Y, Meng Q. Financial protection of rural health insurance for patients with hypertension and diabetes: repeated cross-sectional surveys in rural China. BMC Health Serv Res. 2016;16:481. doi: 10.1186/s12913-016-1735-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marra C, Johnston K, Santschi V, Tsuyuki RT. Cost-effectiveness of pharmacist care for managing hypertension in Canada. Can Pharm J. 2017;150:184–97. doi: 10.1177/1715163517701109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Milan R, Vasiliadis HM, Gontijo Guerra S, Berbiche D. Out-of-pocket costs and adherence to antihypertensive agents among older adults covered by the public drug insurance plan in Quebec. Patient Prefer Adherence. 2017;11:1513–22. doi: 10.2147/PPA.S138364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moise N, Huang C, Rodgers A, et al. Comparative cost-effectiveness of conservative or intensive blood pressure treatment guidelines in adults aged 35-74 years: the CVD Policy Model. Hypertension. 2016;68:88–96. doi: 10.1161/HYPERTENSIONAHA.115.06814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Murphy A, Jakab M, McKee M, Richardson E. Persistent low adherence to hypertension treatment in Kyrgyzstan: how can we understand the role of drug affordability? Health Policy Plan. 2016;31:1384–90. doi: 10.1093/heapol/czw080. [DOI] [PubMed] [Google Scholar]
- 35.Mutowo MP, Lorgelly PK, Laxy M, Renzaho AMN, Mangwiro JC, Owen AJ. The hospitalization costs of diabetes and hypertension complications in Zimbabwe: estimations and correlations. J Diabetes Res. 2016;2016:9754230. doi: 10.1155/2016/9754230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nguyen TP, Nguyen TB, Nguyen TT, et al. Direct costs of hypertensive patients admitted to hospital in Vietnam – a bottom-up micro-costing analysis. BMC Health Serv Res. 2014;14:514. doi: 10.1186/s12913-014-0514-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Paczkowska A, Koligat D, Nowakowska E, Hoffmann K, Bryl W. Analysis of direct costs of hypertension treatment among adolescents in Poland. Acta Polon Pharmaceut Drug Res. 2014;71:197–203. [PubMed] [Google Scholar]
- 38.Park C, Fang J, Hawkins NA, Wang G. Comorbidity status and annual total medical expenditures in U.S. hypertensive adults. Am J Prev Med. 2017;53(6 Suppl 2):172–81. doi: 10.1016/j.amepre.2017.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ricci G, Pirillo I, Tomassoni D, Sirignano A, Grappasonni I. Metabolic syndrome, hypertension, and nervous system injury: epidemiological correlates. Clin Exp Hypertens. 2017;39:8–16. doi: 10.1080/10641963.2016.1210629. [DOI] [PubMed] [Google Scholar]
- 40.Ritchey M, Tsipas S, Loustalot F, Wozniak G. Use of pharmacy sales data to assess changes in prescription- and payment-related factors that promote adherence to medications commonly used to treat hypertension, 2009 and 2014. PLoS One. 2016;11:e0159366. doi: 10.1371/journal.pone.0159366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shireman TI, Svarstad BL. Cost-effectiveness of Wisconsin TEAM model for improving adherence and hypertension control in black patients. J Am Pharm Assoc. 2016;56:389–96. doi: 10.1016/j.japh.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Specogna AV, Turin TC, Patten SB, Hill MD. Hospital treatment costs and length of stay associated with hypertension and multimorbidity after hemorrhagic stroke. BMC Neurol. 2017;17:158. doi: 10.1186/s12883-017-0930-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stafylas P, Kourlaba G, Hatzikou M, Georgiopoulos D, Sarafidis P, Maniadakis N. Economic evaluation of a single-pill triple antihypertensive therapy with valsartan, amlodipine, and hydrochlorothiazide against its dual components. Cost Eff Resour Alloc. 2015;13:10. doi: 10.1186/s12962-015-0036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tajeu GS, Mennemeyer S, Menachemi N, Weech-Maldonado R, Kilgore M. Cost-effectiveness of antihypertensive medication: exploring race and sex differences using data from the easons for geographic and racial differences in stroke study. Med Care. 2017;55:552–60. doi: 10.1097/MLR.0000000000000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tamblyn R, Winslade N, Qian CJ, Moraga T, Huang A. What is in your wallet? A cluster randomized trial of the effects of showing comparative patient out-of-pocket costs on primary care prescribing for uncomplicated hypertension. Implement Sci. 2018;13:7. doi: 10.1186/s13012-017-0701-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vasudeva E, Moise N, Huang C, et al. Comparative cost-effectiveness of hypertension treatment in non-Hispanic blacks and whites according to 2014 guidelines: a modeling study. Am J Hypertens. 2016;29:1195–205. doi: 10.1093/ajh/hpw047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang G, Zhou X, Zhuo X, Zhang P. Annual total medical expenditures associated with hypertension by diabetes status in U.S. adults. Am J Prev Med. 2017;53(6 Suppl 2):182–9. doi: 10.1016/j.amepre.2017.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang G, Fang J, Ayala C. Hypertension-associated hospitalizations and costs in the United States, 1979-2006. Blood Press. 2014;23:126–33. doi: 10.3109/08037051.2013.814751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang G, Zhang Z, Ayala C, Dunet DO, Fang J, George MG. Costs of hospitalization for stroke patients aged 18-64 years in the United States. J Stroke Cerebrovasc Dis. 2014;23:861–8. doi: 10.1016/j.jstrokecerebrovasdis.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang Q, Liu H, Lu ZX, Luo Q, Liu JA. Role of the new rural cooperative medical system in alleviating catastrophic medical payments for hypertension, stroke and coronary heart disease in poor rural areas of China. BMC Public Health. 2014;14:907. doi: 10.1186/1471-2458-14-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Z, Chen Z, Wang X. Cost-effectiveness of nitrendipine and hydrochlorothiazide or metoprolol to treat hypertension in rural community health centers in China. J Hypertens. 2017;35:886–92. doi: 10.1097/HJH.0000000000001209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weaver CG, Clement FM, Campbell NRC, et al. Healthcare costs attributable to hypertension Canadian population-based cohort study. Hypertension. 2015;66:502–8. doi: 10.1161/HYPERTENSIONAHA.115.05702. [DOI] [PubMed] [Google Scholar]
- 53.Zhang D, Wang G, Zhang P, Fang J, Ayala C. Medical expenditures associated with hypertension in the U.S., 2000–2013. Am J Prev Med. 2017;53(6 Suppl 2):164–71. doi: 10.1016/j.amepre.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mullins CD, Sikirica M, Seneviratne V, Ahn J, Akhras KS. Comparisons of hypertension-related costs from multinational clinical studies. Pharmacoeconomics. 2004;22:1001–14. doi: 10.2165/00019053-200422150-00004. [DOI] [PubMed] [Google Scholar]
- 55.Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics – 2019 update. A Report from the American Heart Association. Circulation. 2019;139:52–6. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 56.Hird TR, Zomer E, Owen AJ, Magliano DJ, Liew D. Productivity burden of hypertension in Australia. Hypertension. 2019;73:777–84. doi: 10.1161/HYPERTENSIONAHA.118.12606. [DOI] [PubMed] [Google Scholar]
- 57.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting U.S. employers. J Occup Environ Med. 2004;46:398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 58.Burnier M, Egan BM. Adherence in hypertension. A review of prevalence, risk factors, impact, and management. Circ Res. 2019;124:1124–40. doi: 10.1161/CIRCRESAHA.118.313220. [DOI] [PubMed] [Google Scholar]
- 59.Grosso AM, Bodalia PN, MacAllister RJ, Hingorani AD, Moon JC, Scott MA. Comparative clinical- and cost-effectiveness of candesartan and losartan in the management of hypertension and heart failure: a systematic review, meta- and cost-utility analysis. Int J Clin Pract. 2011;65:253–63. doi: 10.1111/j.1742-1241.2011.02633.x. [DOI] [PubMed] [Google Scholar]
- 60.Mohd-Tahir NA, Li SC. Budget impact analysis of increasing prescription of renin-angiotensin system inhibitors drugs to standard anti-hypertensive treatments in patients with diabetes and hypertension in a hypothetical cohort of Malaysian population. PLoS One. 2019;14:e0212832. doi: 10.1371/journal.pone.0212832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gaziano TA, Steyn K, Cohen DJ, Weinstein MC, Opie LH. Cost-effectiveness analysis of hypertension guidelines in South Africa. Absolute risk versus blood pressure level. Circulation. 2005;112:3569–76. doi: 10.1161/CIRCULATIONAHA.105.535922. [DOI] [PubMed] [Google Scholar]
- 62.Park C, Wang G, Durthaler JM, Fang J. Cost-effectiveness analyses of antihypertensive medicines: a systematic review. Am J Prev Med. 2017;53(6 Suppl 2):131–42. doi: 10.1016/j.amepre.2017.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Albert NM, Swindle JP, Buysman EK, Chang C. Lower hospitalization and healthcare costs with sacubitril/valsartan versus angiotensin-converting enzyme inhibitor or angiotensin-receptor blocker in a retrospective analysis of patients with heart failure. J Am Heart Assoc. 2019;8:e011089. doi: 10.1161/JAHA.118.011089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Anis AH, Sun H, Singh S, Woolcott J, Nosyk B, Brisson M. A cost-utility analysis of losartan versus atenolol in the treatment of hypertension with left ventricular hypertrophy. Pharmacoeconomics. 2006;24:387–400. doi: 10.2165/00019053-200624040-00008. [DOI] [PubMed] [Google Scholar]
- 65.Meretoja A, Kaste M, Roine RO. Direct costs of patients with stroke can be continuously monitored on a national level performance, effectiveness, and costs of treatment episodes in stroke (PERFECT Stroke) database in Finland. Stroke. 2011;42:2007–12. doi: 10.1161/STROKEAHA.110.612119. [DOI] [PubMed] [Google Scholar]
- 66.Claesson L, Gosman-Hedstrom G, Johannesson M, Fagerberg B, Blomstrand C. Resource utilization and costs of stroke unit care integrated in a care continuum: a 1-year controlled, prospective, randomized study in elderly patients. The Goteborg 70+ Stroke Study. Stroke. 2000;31:2569–77. doi: 10.1161/01.str.31.11.2569. [DOI] [PubMed] [Google Scholar]
- 67.Grieve R, Hutton J, Bhalla A. A comparison of the costs and survival of hospital-admitted stroke patients across Europe. Stroke. 2001;32:1684–91. doi: 10.1161/01.str.32.7.1684. [DOI] [PubMed] [Google Scholar]
- 68.Luengo-Fernandez R, Gray AM, Rothwell PM. Population-based study of determinants of initial secondary care costs of acute stroke in the United Kingdom. Stroke. 2006;37:2579–87. doi: 10.1161/01.STR.0000240508.28625.2c. [DOI] [PubMed] [Google Scholar]
- 69.Teng J, Mayo NE, Latimer E. Costs and caregiver consequences of early supported discharge for stroke patients. Stroke. 2003;34:528–36. doi: 10.1161/01.str.0000049767.14156.2c. [DOI] [PubMed] [Google Scholar]
- 70.The World Bank Current health expenditure per capita. https://databank.worldbank.org/source/world-development-indicators – Current health expenditure per capita, PPP (current international $) (access: 1 July 2019)