Abstract
Over 30 years into the US HIV/AIDS epidemic, Black men who have sex with men (BMSM) continue to carry the highest burden of both HIV and AIDS cases. There is then, an urgent need to expand access to HIV prevention and treatment for all gay and bisexual men, underscoring the importance of the federal initiative ‘Ending the Epidemic: A Plan for America’. This research examines structural factors associated with BMSM HIV testing coverage over time (2011–2016) in 85 US Metropolitan Statistical Areas (MSAs). We calculated MSA-specific annual measures of BMSM HIV testing coverage (2011–2016). Variables suggested by the Theory of Community Action (i.e., need, resource availability, institutional opposition and organized support) were analyzed as possible predictors of coverage using multilevel modeling. Relationships between BMSM HIV testing and the following covariates were positive: rates of BMSM living with HIV (b = 0.28), percent of Black residents employed (b = 0.19), Black heterosexual testing rate (b = 0.46), health expenditures per capita (b = 0.16), ACT UP organization presence in 1992 (b = 0.19), and syringe service presence (b = 0.12). Hard drug arrest rates at baseline (b = − 0.21) and change since baseline (b = − 0.10) were inversely associated with the outcome. Need, resources availability, organized support and institutional opposition are important determinants of place associated with BMSM HIV testing coverage. Efforts to reduce HIV incidence and lessen AIDS-related disparities among BMSM in the US require improved and innovative HIV prevention approaches directed toward BMSM including a fuller understanding of structural factors that may influence place variation in BMSM testing patterns and risk behavior in places of high need.
Keywords: Structural determinants, HIV testing, Black MSM, Theory of community action, US Metropolitan Statistical Areas, Place research
Introduction
Over 30 years into the US HIV/AIDS epidemic, Black men who have sex with men (BMSM) continue to carry the highest burden of both HIV and AIDS cases [1–6]. Black MSM account for approximately 50% of AIDS cases and have the highest rates of AIDS mortality among MSM. HIV prevalence and incidence rates are disproportionately high among BMSM compared to other racial/ethnic groups of MSM. In 2017, MSM accounted for more than half (59%) of new HIV diagnoses among Blacks overall and a majority (80%) of new diagnoses among Black men [1–6]. Additionally, rates of unrecognized HIV infection and sexually transmitted infections still remained higher among BMSM than among other MSM [6–9]. Approximately 20% of BMSM living with HIV are estimated to be undiagnosed (by comparison, only 12.5% of White MSM living with HIV estimated to be undiagnosed) [1, 2, 6–9].
HIV testing efforts to reduce HIV incidence and lessen AIDS-related disparities among BMSM is a key objective of the National HIV/AIDS Strategy [10, 11]. HIV testing is the first step to enable persons at risk to know their HIV status, be linked to medical care and services that improve survival, and reduce the likelihood that they will transmit HIV to others [1, 2, 7–9]. Determining differences in HIV testing patterns among specific risk and racial/ethnic groups is an essential component of CDC’s HIV prevention strategies [1, 2, 10, 11]. However, research on understanding these differences has been limited.
Individual risk behavior alone does not account for the disproportionate burden of HIV among MSM, more specifically among BMSM [12–15]. It can be argued that variations in HIV and HIV disparities among BMSM is linked to the socio-structural and political conditions of particular localities [12, 15–23]. Millett et al. [12, 21] for example, argued that structural barriers, notably incarceration, unemployment and low education are crucial factors in understanding barriers to disparities in HIV infection among BMSM. Peterson and Jones [8] and Brooks et al. [23] discussed the need for socio-structural interventions to reduce HIV-related racial disparities—including stigma, racism, barriers to healthcare, and incarceration—on HIV risk among BMSM. Additionally, Levy et al. [24] conducted an extensive review of the literature on structural barriers to HIV testing and prevention services among BMSM across four domains: healthcare, stigma and discrimination, incarceration, and poverty. Employing a social systems framework, this research found that BMSM experience a number of barriers to HIV testing and prevention services, including: (1) inadequate access to culturally competent services; (2) stigma and discrimination impeding access to services; (3) a deficiency of services in correctional institutions; and (4) limited services in places where BMSM live. Lastly, Mays et al. [25] and others [12, 15, 23–25] have argued for a more rigorous HIV prevention research agenda into the role of structural factors as barriers to HIV testing and prevention services to address disparities among BMSM HIV infection.
This present research builds on previous scholarly work on the role of place in predicting the presence and coverage of health services to investigate structural determinants associated with BMSM HIV testing coverage. Research has established the role of place characteristics in predicting health and health service coverage in vulnerable populations and found they are related to the utilization of syringe service programs (SSPs); drug treatment programs; and HIV testing among people who inject drugs (PWID) [26–33]. We present theory-driven predictors of BMSM HIV testing coverage rates as a function of program need, resource availability, institutional opposition, and organized support, factors which may impact the extent of HIV test coverage among BMSM. As previously conceived [28, 29, 31–33] this framework emphasizes four types of place characteristics as important to the distribution and implementation of institutionalized programs in cities or MSAs. Below we present the “theory of community action” (TCA), a theoretical framework for predicting program presence and coverage.
Identifying structural determinants associated with the likelihood of HIV testing among BMSM is important to public health agencies, which can use these insights to direct enhanced HIV-testing outreach efforts to places that are likely to lag in testing needs. Developing a better understanding of how structural factors affect utilization of, and access to, HIV testing and prevention services may help us advance effective social interventions and public policies to increase HIV testing and prevention programming among BMSM in places of high need.
Theory Framework
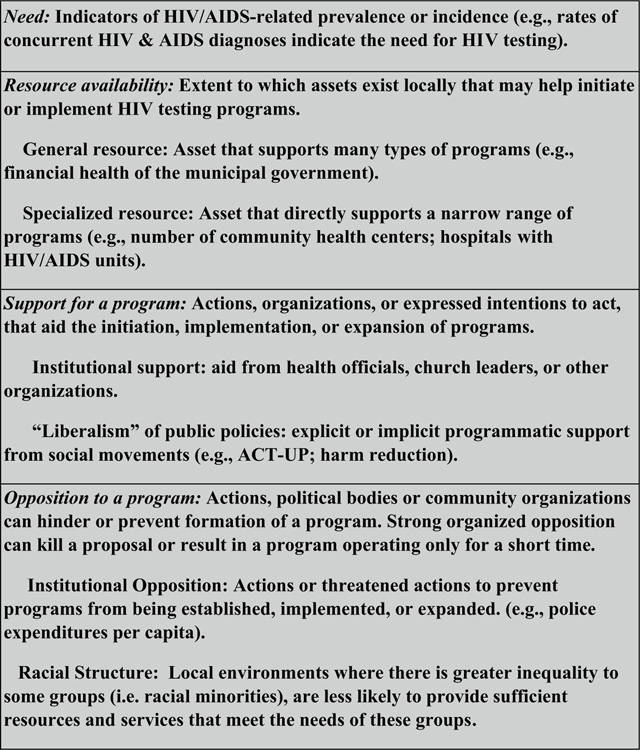
Figure 1 displays the conceptual model of TCA. This framework utilizes concepts from urban studies [34–36] social movement theory [37–39] and diffusion of innovations theory [40–43]. It has been used to identify a variety of place characteristics that are likely to affect the extent to which a community carries out and sustains an action. Rosser and Horvath, for example, found that successful rural HIV prevention was less likely in states with more religious and Evangelical Protestant adherents and more successful in states with more “gay community” infrastructure [44]. Further community actions have been carried out and concerns programs related to condom distribution [45, 46], HIV counseling and testing services [46–48], specialized programs to reduce opiate misuse [28, 29, 31–33, 49–51], or treatment for people who are mentally ill [52, 53]. Here we expand previous research on determinants of program presence and coverage to encompass HIV testing coverage for BMSM with our past analyses of the determinants of program presence and coverage for PWID [28, 29, 31–33].
Fig. 1.
Theory of community action framework: definitions and examples of key constructs
In this analysis, need refers to rates of epidemiologic factors related to risk behaviors (i.e., BMSM living with HIV per 10,000 BMSM population) or sexually transmitted infections among adult males. The notions that need leads to response suggest that Metropolitan Statistical Areas (MSAs) with greater epidemiologic need will respond to such need by providing more health services in high needs areas.
Resource availability refers to the extent to which assets that exist locally are useful in initiating and implementing a program. Higher levels of local resource availability are hypothesized to be associated with higher rates of service provision. Local resources can be categorized as either general or specialized. General resources might support a wide range of activities and may be positively associated with a number of social and health programs that may have an impact (either directly or indirectly) on HIV prevention programs [28, 29, 31–33, 54]. Specialized resources support the development of only a narrow range of programs, such as breast cancer programming, mental health programs, or health insurance for children [55–57]. Specialized resources might include skilled labor force coming from medical and public health schools; hospitals with special HIV/AIDS units and staff; including HIV/AIDS counseling; or health expenditures per capita in an MSA [58–60]. Levels of specialized resources are expected to affect key outcomes and the presence of HIV testing and counseling programs.
Organized and Potential Institutional Support for Programs.
Organized support for programs is hypothesized by the present research to predict increases in, or higher levels of, HIV testing coverage. Indicators of organized or potential support can come from the presence of outreach efforts, ACT UP chapters, or local area strength of the American Public Health Association. Organized or potential support for a program can determine its presence, its size, and its longevity [28, 30, 32, 33]. Support can come from institutionalized sources like public health departments or social movements. Institutional support from health officials, medical and public health researchers, church leaders, education, and/or school administrators might provide support and outreach for a needed HIV program [28, 29, 31–33, 49–51]. Institutional support can also come in the form of funding for public policies and programs, such as public funding for syringe services programs. We can think of this as a general willingness of government to spend money on social services for the public good. Here, we hypothesize that HIV testing is generally a “liberal” response [28, 29, 33, 50, 51] to at risk populations in need of HIV services and that financial or other support from policy and institutional sources for HIV testing and counseling programs therefore reflects a higher degree of “liberalism” than does a lack of such support.
Social movements, ranging from the feminist health movement to AIDS activism, have helped to shape programs, and policies in the U.S. (such as treatment services, health care reform, and AIDS policy), and have also helped to shape public opinion about health-related issues (such as the de-stigmatization of groups, including MSM) [15, 18, 25, 28, 37, 58, 61]. For example, gay political influence and concern among the gay community regarding HIV/AIDS prevention (including the direct involvement of gay and lesbian activists in ACT UP) helped form and sustain many HIV/AIDS and harm reduction programs in the US [28, 33, 37, 56–59].
Organized and Potential Institutional Opposition to Programs.
Theoretically converse to the notion of support to programs, opposition (even presumed opposition) can hinder or prevent formation of a program. Strong organized opposition can kill a proposal or result in a program operating only for a short time. Harm reduction type services for example, in US communities remain controversial and face ongoing obstacles from law enforcement and local communities, including ‘not-in-my-backyard’ community opposition [28, 33, 49–51, 62–66].
The strength of institutional opposition has often contributed to greater delays in implementation or total lack of implementation of HIV prevention programs for marginalized at risk groups in US cities and metropolitan areas [28, 33, 49–51, 62–66]. In addition, institutional opposition has often contributed to a lack of service utilization of HIV prevention programs. Spurred by racialized policing and the war on drugs institutional opposition can impact access and service usage due to fear of being arrested [10, 12, 14, 15, 18, 22, 26–28, 58–61]. Weakening or prevention of harm reduction programs due to opposition has been found by Tempalski et al., [28, 30, 33, 62–66]; Downing et al. [49] and Des Jarlais et al. [47, 67]. Likewise, opposition has been identified as a hindrance to services and programs for the homeless, to housing programs for the mentally ill, to half- way houses for people living with AIDS, and to health-related facilities for persons with AIDS [58, 59, 67–73].
Additionally, previous research has shown that racial economic and political structures may adversely affect the health of a variety of racial/ethnic groups as well as reducing the resources and services available to them [12, 14, 15, 18, 22, 26–28, 58–61]. Racial structures such as greater inequality between racial groups, for example, might contribute to, or be reflective of, local environments that are more institutionally oppressive to some groups (i.e. racial minorities), and therefore less likely to provide sufficient resources and services that meet the needs of these groups. Here, we hypothesize that structural conditions of racial/ethnic inequality may be associated with stronger opposition to HIV testing services, and thus may be associated with less HIV testing coverage among BMSM.
Methods and Measures
Data sources for the rate of BMSM HIV testing events and independent variables in 85 large US MSAs are outlined in Supplemental Table SI.
Outcome
We calculate HIV testing coverage among BMSM—using Formula 1.
| (1) |
The numerator was the total number of testing events at CDC funded testing sites among BMSM [74]. CDC-funded HIV testing often occurs in locations such as community based organizations and community health centers. Testing events reported by the CDC are specific to CDC-funded sites and not testing events at private clinics.
The denominator is BMSM population estimate created for the parent study and based on the Gallup Daily Tracking survey, a national probability sample collected from June–December 2012 and July 2013–June 2014 [75]. Gallup surveyed 184,854 men of whom 2.0% to 7.5% identified as gay or bisexual across MSAs according to the question, “Do you, personally, identify as lesbian, gay, bisexual, or transgender?” Population estimates from the 2010 census were used to derive the number of men aged 15 and older in each MSA [76]. The percentage of men who identify as gay or bisexual within each MSA (pGBT menMSA) was then applied to the population figures to derive MSA-level estimates for the number of gay and bisexual men aged 15 and older (Formula 2). Estimates from Formula 2 were extrapolated across time using the adult male population in MSAs for each year.
| (2) |
Independent Variables Within TCA Domains
Need: (1) the rate of BMSM living with HIV per 10,000; (2) deaths within 12 months of HIV diagnosis separately among Black persons with injection drug use (PWID) and BMSM per 10,000 Black adults; (3) Black PWID HIV testing per 10,000 Black adults; (4) male syphilis, gonorrhea, and chlamydia rates; (5) the hepatitis C mortality rate for Black adults; and (6) the percent of Black residents in poverty.
Resource availability measures include: (A) General resources: (1) the Black median household income; (2) percent of all residents without health insurance (our data source did not identify the number of persons with health insurance); and (3) percent of Black residents employed. (B) Specialized resources: (1) the rate of Black heterosexual HIV testing per 10,000 Black adults as a measure of testing resources in a community; (2) health expenditures per capita; and (3) the male ARV prescription rate per male PLWH which we categorized as at/above or below the median rate (1 = at/above the median, 0 = below the median rate).
Support for a program measures include: (A) Institutional support: (1) AIDS organizations per capita; and (2) percent of males with college education. B) “Liberalism” of public policies we included three binary (1 = present, 0 = absent) measures: (1) the presence of AIDS Coalition to Unleash Power (ACT UP) organizations in 1990; (2) presence of syringe service programs (SSPs); and (3) a variable capturing state historic passage of laws pertaining to the rights of sexual minorities.1
Opposition to a program measures include: (A) Institutional opposition: (1) the hard drug arrest rate; (2) percent of incarcerated males; and (3) number of police per 1000 residents by impeding access to testing. (B) racial structure: (1) percent Black residential isolation; (2) the odds ratio of being denied a home loan application for Black residents compared to Whites; and (3) Black-White poverty inequality as the ratio of the percent of Black compared to White residents in poverty.
Analysis
We make use of descriptive statistics to summarize each variable’s distribution. We employed a 4-stage multilevel model-building process, first modeling temporal changes in the outcome (Stage 1), next conducting bivariate modeling (Stage 2), domain analyses modeling (Stage 3), and multivariable modeling (Stage 4). We selected a 3-level multilevel linear modelling (MLM) [77, 78] approach since it allowed us to model trajectories of change over time and account for correlation of clustered observations (e.g., time nested within MSAs and MSAs nested within states). Our study sought to analyze a census of all MSAs with a population of 500,000 or larger; therefore, assumptions regarding interpretation of p values and confidence intervals do not hold [79, 80]. We therefore determined substantive significance using the magnitude of association. Associations were deemed substantively significant if a standardized coefficient for a variable was ≥|0.10| in the final model [81]. We report findings using magnitudes of association and standardized coefficients, obtained by creating z scores for variables, in all stages of analysis and report confidence intervals as a heuristic guide [77, 78]. We conducted our analyses in SAS 9.4 [82].
Stage 1: Modeling Change in the Outcome Over Time
We modeled change over time for the outcome. We natural log transformed the outcome to linearize its relationship with covariates because of its skewed distribution. All models (Stages 1–4) used 3-level MLM to account for the clustering of annual observations within MSAs and MSAs within states. To quantify the variability of the outcome within and between MSAs, we assessed covariance parameters and calculated intraclass correlation coefficients (ICCs) [79]. We tested linear, quadratic, and cubic time functions and selected the time function with the smallest Akaike information criterion (AIC).
Stage 2: Bivariate Models
We visually inspected plots of each covariate over time and centered each time-varying continuous covariate at baseline to aid interpretation. Centering produced variable “dyads” for each time-varying covariate, with one variable capturing the baseline value and another capturing yearly change in the variable since baseline (current year minus baseline year’s observation for each time-varying variable). For SSP presence, survey response rates over time were unstable and these data were not reliable after baseline; we therefore modeled this variable for the baseline year only. We did not expect changes in independent variables to have an instantaneous effect on the outcome, and so we tested 1-, 2-, and 3-year lags between independent variables and the outcome and selected the lag with the largest association (see Table 1).
TABLE 1 –
Descriptive Statistics for Rates of Black MSM HIV Testing Events (per 10,000) Among Black MSM (Aged 15–64) and Structural Independent Variables in 85 large US Metropolitan Statistical Areas, 2011–2016a
| Variable and Domain | Mean | Standard Deviation |
Median | 25th Percentile | 75th Percentile |
|---|---|---|---|---|---|
| Dependent Variable | |||||
| Black MSM HIV testing rate per 10,000 Black MSM | |||||
| Baseline 2011 | 991.6 | 607.4 | 876.3 | 621.5 | 1,201.1 |
| Change between 2011 and 2016 | −1.77 | 685.82 | −17.89 | −313.40 | 280.56 |
| Need Domain | |||||
| Black MSM living with HIV per 10,000 Black MSM | |||||
| Lagged baseline (2010) | 1,726.07 | 654.64 | 1,681.02 | 1,267.73 | 2,099.32 |
| Change between 2010 and 2015 | 484.81 | 400.91 | 445.50 | 174.99 | 695.18 |
| Black PWID late HIV diagnoses rate (death within 12 months of diagnosis) per 10,000 Black adults | |||||
| Lagged baseline (2010) | 0.03 | 0.07 | 0.00 | 0.00 | 0.02 |
| Change between 2010 and 2015 | −0.01 | 0.08 | 0.00 | 0.00 | 0.00 |
| Black MSM late HIV diagnoses rate (death within 12 months of diagnosis) per 10,000 Black adults | |||||
| Lagged baseline (2010) | 0.05 | 0.08 | 0.00 | 0.00 | 0.09 |
| Change between 2010 and 2015 | −0.01 | 0.08 | 0.00 | −0.01 | 0.00 |
| Black PWID testing rate per 10,000 Black adults | |||||
| Lagged baseline (2010) | 4.24 | 5.31 | 2.34 | 1.14 | 5.29 |
| Change between 2010 and 2015 | −0.90 | 4.94 | −0.08 | −2.58 | 1.05 |
| Male syphilis rate per 100,000 | |||||
| Lagged baseline (2008) | 7.7 | 7.2 | 5.8 | 2.8 | 9.7 |
| Change between 2008 and 2013 | 3.3 | 5.8 | 2.6 | 0.4 | 5.8 |
| Male chlamydia rate per 100,000 | |||||
| Lagged baseline (2010) | 248.0 | 87.1 | 231.9 | 195.2 | 299.7 |
| Change between 2010 and 2015 | 68.3 | 52.7 | 72.3 | 45.1 | 94.3 |
| Male gonorrhea rate per 100,000 | |||||
| Lagged baseline (2009) | 98.5 | 55.5 | 92.7 | 53.7 | 135.0 |
| Change between 2009 and 2014 | 31.2 | 40.3 | 33.1 | 9.5 | 55.0 |
| Black hepatitis C mortality rate per 10,000 Black adults | |||||
| Lagged baseline (2010) | 20.3 | 25.3 | 12.0 | 4.0 | 25.0 |
| Change between 2010 and 2015 | −0.6 | 9.4 | 0.5 | −4.0 | 4.0 |
| Percent Black residents in poverty | |||||
| Lagged baseline (2008) | 20.8 | 6.9 | 20.4 | 16.5 | 26.1 |
| Change between 2008 and 2013 | 1.7 | 2.6 | 1.8 | 0.4 | 3.2 |
| General Resources Domain | |||||
| Black median household income ($) | |||||
| Lagged baseline (2008) | 42,188.1 | 11,454.0 | 41,728.0 | 33,372.0 | 47,030.0 |
| Change between 2008 and 2013 | 844.4 | 7,358.7 | 423.5 | −1,948.5 | 3,201.0 |
| Percent without health insurance | |||||
| Lagged baseline (2010) | 19.9 | 6.0 | 19.2 | 15.8 | 23.6 |
| Change between 2010 and 2015 | −8.0 | 2.8 | −7.5 | −9.2 | −5.8 |
| Percent Black residents employed | |||||
| Lagged baseline (2008) | 61.0 | 6.3 | 61.7 | 58.1 | 65.1 |
| Change between 2008 and 2013 | −0.9 | 2.1 | −0.8 | −2.3 | 0.8 |
| Specialized Resources Domain | |||||
| Black heterosexual HIV testing rate per 10,000 Black adults | |||||
| Lagged baseline (2010) | 172.99 | 152.19 | 122.78 | 40.02 | 271.07 |
| Change between 2010 and 2015 | −32.96 | 140.51 | −20.01 | −125.58 | 30.27 |
| Health expenditures per capita ($) | |||||
| Lagged baseline (2008) | 135.4 | 107.4 | 117.0 | 48.8 | 198.1 |
| Change between 2008 and 2013 | 12.0 | 48.1 | 2.7 | −4.7 | 25.2 |
| Male ARV prescription rate per male PLWH (above the median) | |||||
| Lagged baseline (2008) n (%) | 34.0 (40.0) | ||||
| 2013 n (%) | 42.0 (49.4) | ||||
| Liberalism of Public Policies Domain | |||||
| ACT UP organization presence | |||||
| Lagged baseline (1990) n (%) | 16.0 (18.8) | ||||
| Syringe service program presence | |||||
| Lagged baseline (2008) n (%) | 34.0 (40.0) | ||||
| History of state laws supportive of same sex minorities (2 class) | |||||
| Class 1 - supportive from 1990–2014 n (%) |
39 (45.9) | ||||
| Institutional Support Domain | |||||
| AIDS organizations per capita | |||||
| Lagged baseline (2008) | 2.0 | 1.2 | 1.8 | 1.4 | 2.5 |
| Change between 2008 and 2013 | −0.3 | 0.3 | −0.3 | −0.5 | −0.1 |
| Percent of males with college education | |||||
| Lagged baseline (2008) | 19.3 | 3.8 | 19.2 | 16.8 | 21.7 |
| Change between 2008 and 2013 | 0.6 | 0.5 | 0.6 | 0.3 | 0.9 |
| Institutional Opposition Domain | |||||
| Hard drug arrest rate per 10,000 | |||||
| Lagged baseline (2009) | 20.2 | 13.0 | 15.1 | 11.9 | 21.8 |
| Change between 2009 and 2014 | 0.2 | 9.5 | 1.2 | −3.1 | 4.1 |
| Percent incarcerated males | |||||
| Lagged baseline (2009) | 1.5 | 1.3 | 1.3 | 0.9 | 1.7 |
| Change between 2009 and 2014 | 0.0 | 0.2 | 0.0 | −0.1 | 0.0 |
| Police per 1,000 residents | |||||
| Lagged baseline (2010) | 2.5 | 1.2 | 2.2 | 1.9 | 2.8 |
| Change between 2010 and 2015 | −0.1 | 0.2 | −0.1 | −0.2 | 0.0 |
| Racial Structure Domain | |||||
| Percent isolated Black residents | |||||
| Lagged baseline (2008) | 33.7 | 19.0 | 34.3 | 16.2 | 45.7 |
| Change between 2008 and 2013 | −1.8 | 1.3 | −1.8 | −2.6 | −0.8 |
| Odds ratio of home loan denial for Blacks compared to whites | |||||
| Lagged baseline (2008) | 2.4 | 0.2 | 2.4 | 2.3 | 2.6 |
| Change between 2008 and 2013 | −0.6 | 0.2 | −0.6 | −0.7 | −0.4 |
| Black-White poverty inequality ratio | |||||
| Lagged baseline (2008) | 2.6 | 0.7 | 2.5 | 2.3 | 2.9 |
| Change between 2008 and 2013 | −0.1 | 0.3 | −0.1 | −0.3 | 0.0 |
2011 to 2016 refers to the timeframe for the HIV diagnoses outcome. Independent variables were lagged 1–3 years using the lag with the strongest association with the outcome. Note: Independent variables were lagged because we did not expect a change in the independent variables to have an instantaneous effect on the outcome.
We regressed BMSM testing rates on time (operationalized as years since baseline) and the lagged independent variable dyad (baseline and change since baseline). To assess the magnitude of association, we summed the absolute value of each dyad’s standardized coefficients. Based on effect size literature and previous research, we a priori selected a cut point of 0.20 as a minimum effect size of practical significance [80] and when a dyad’s magnitude of association in the bivariate model was >|0.20|, we included that dyad in the final model [81]. For variables that were non-time varying we used a threshold ≥|0.10| for standardized coefficients.
Stage 3: Domain Analysis
In the domain analysis stage we selected independent variables that met the threshold in bivariate analyses. We included these variables in multivariable models for each domain (1. need; 2. resource availability; 3. support for a program; and 4. opposition to a program). We applied the same criteria used in Stage 2 (absolute sum of variable dyad standardized coefficients > 0.20) to the results of domain analyses to determine which variables to include in the final multivariable model.
Stage 4: Final Multivariable Model
We used multivariable MLM models to test the relationship between independent variables and BMSM testing rates including variables selected at the bivariate model and domain analysis stages. Variables were decomposed into dyads and we were interested in baseline or change since baseline measures as potentially meaningful covariates in the multivariable model; therefore utilizing a threshold >|0.10| for individual standardized coefficients to determine substantive significance, instead of using >|0.20| for the variable dyad. We tested the multivariable model for multicollinearity using condition index and variance decomposition proportions [83]. Standardized coefficients are interpreted as the number of standard deviations of change in the logged outcome given a one standard deviation increase in the independent variable. Since we log transformed the outcome, we used back transformation of the standardized coefficients to calculate percent change in the BMSM testing rate, in standard deviation units, per one standard deviation increase in independent variables [84].
Results
The outcome measure displayed considerable variation across MSAs at baseline. In 2011 the median rate of BMSM testing event across the 85 MSAs was 876 per 10,000 BMSM (25th and 75th percentiles: 622/10,000, 1,201/10,000; Table 1); this rate decreased approximately 2% from 2008 to 2016, to 858/10,000 (25th and 75th percentiles for change over time: − 313/10,000, 281/10,000). Analysis of the ICC showed that a substantial proportion of the outcome variance was due to differences between MSAs (62%) and states (11%), thus warranting multilevel analysis. The unconditional growth model yielded the smallest AIC when time since baseline was modeled using linear time.
Bivariate Analyses
In bivariate models adjusted for time and state fixed effects, 14 of 26 independent variables met the threshold (absolute sum of variable dyad standardized coefficients > 0.20) to proceed to the next phase of analysis shown in Table 2.
TABLE 2 –
Standardized Multilevela Bivariate, Domain, and Multivariable Results of Regressing Natural Loggedb Rates of Black MSM Testing Events (per 10,000) Among Black MSM (Aged 15–64 Years) on Structural Independent Variables in 85 Large US Metropolitan Statistical Areas, 2011–2016c
| Variable and Domain | Standardized Bivariate Models - Coefficient (CI) | Standardized Domain Analysis Models - Coefficient (CI) | Standardized Multivariable Model - Coefficient (CI) |
|---|---|---|---|
| Need Domain | |||
| Black MSM living with HIV per 10,000 Black MSM | |||
| Lagged baseline (2010) | 0.35 (0.17, 0.52)* | 0.28 (0.08, 0.48)* | 0.28 (0.12, 0.43)* |
| Change since baseline | −0.02 (−0.11, 0.07)* | −0.01 (−0.11, 0.08)* | −0.02 (−0.11, 0.07) |
| Black PWID late HIV diagnoses rate (death within 12 months of diagnosis) per 10,000 Black adults | |||
| Lagged baseline (2010) | −0.01 (−0.20, 0.18) | ||
| Change since baseline | 0.01 (−0.07, 0.09) | ||
| Black MSM late HIV diagnoses rate (death within 12 months of diagnosis) per 10,000 Black adults | |||
| Lagged baseline (2010) | −0.08 (−0.26, 0.09) | ||
| Change since baseline | −0.04 (−0.11, 0.03) | ||
| Black PWID HIV testing rate per 10,000 Black adults | |||
| Lagged baseline (2010) | 0.03 (−0.13, 0.2) | ||
| Change since baseline | 0.02 (−0.06, 0.09) | ||
| Male syphilis rate per 100,000 | |||
| Lagged baseline (2008) | 0.20 (0.05, 0.35)* | 0.07 (−0.10, 0.25) | |
| Change since baseline | 0.01 (−0.07, 0.09)* | 0.0 (−0.08, 0.08) | |
| Male chlamydia rate per 100,000 | |||
| Lagged baseline (2010) | 0.10 (−0.04, 0.25)* | 0.02 (−0.13, 0.17) | |
| Change since baseline | 0.10 (0.02, 0.18)* | 0.09 (0.0, 0.17) | |
| Male gonorrhea rate per 100,000 | |||
| Lagged baseline (2009) | 0.18 (0.03, 0.33) | ||
| Change since baseline | 0.01 (−0.07, 0.09) | ||
| Black hepatitis C mortality rate per 10,000 Black adults | |||
| Lagged baseline (2010) | 0.12 (−0.03, 0.26) | ||
| Change since baseline | −0.01 (−0.08, 0.06) | ||
| Percent Black residents in poverty | |||
| Lagged baseline (2008) | −0.02 (−0.18, 0.15) | ||
| Change since baseline | −0.07 (−0.18, 0.03) | ||
| General Resources Domain | |||
| Black median household income ($) | |||
| Lagged baseline (2008) | −0.03 (−0.19, 0.12) | ||
| Change since baseline | 0.04 (−0.03, 0.12) | ||
| Percent without health insurance | |||
| Lagged baseline (2010) | −0.18 (−0.37, 0.02)* | −0.14 (−0.33, 0.06) | |
| Change since baseline | −0.05 (−0.15, 0.06)* | −0.02 (−0.14, 0.10) | |
| Percent Black residents employed | |||
| Lagged baseline (2008) | 0.25 (0.10, 0.40)* | 0.18 (0.04, 0.33)* | 0.19 (0.07, 0.32)* |
| Change since baseline | 0.08 (0.0, 0.16)* | 0.05 (−0.04, 0.14)* | 0.06 (−0.02, 0.14) |
| Specialized Resources Domain | |||
| Black heterosexual HIV testing rate per 10,000 Black adults | |||
| Lagged baseline (2010) | 0.35 (0.11, 0.58)* | 0.36 (0.12, 0.59)* | 0.46 (0.24, 0.68)* |
| Change since baseline | 0.09 (0.0, 0.18)* | 0.09 (0.0, 0.18)* | 0.09 (0.0, 0.17) |
| Health expenditures per capita ($) | |||
| Lagged baseline (2008) | 0.17 (−0.1, 0.44)* | 0.18 (−0.08, 0.44)* | 0.16 (−0.07, 0.4)* |
| Change since baseline | −0.04 (−0.38, 0.3)* | −0.01 (−0.34, 0.30)* | 0.02 (−0.28, 0.31) |
| Male ARV prescription rate per male PLWH (above the median) | |||
| Lagged baseline (2008) | −0.06 (−0.38, 0.27) | ||
| Yearly rate | 0.01 (−0.15, 0.16) | ||
| Liberalism of Public Policies Domain | |||
| ACT UP organization presence | |||
| Lagged baseline (1990) | 0.52 (0.15, 0.89)* | 0.47 (0.09, 0.86)* | 0.19 (−0.12, 0.50)* |
| Syringe service program presence | |||
| Lagged baseline (2008) | 0.29 (−0.07, 0.64)* | 0.14 (−0.18, 0.45)* | 0.12 (−0.14, 0.38)* |
| History of state laws supportive of same sex minorities (2 class) | |||
| Class 1 - supportive from 1990–2014 | −0.07 (−0.44, 0.30) | ||
| Institutional Support Domain | |||
| AIDS organizations per capita | |||
| Lagged baseline (2008) | 0.20 (0.06, 0.35)* | 0.13 (−0.04, 0.30) | |
| Change since baseline | −0.05 (−0.14, 0.05)* | −0.05 (−0.15, 0.05) | |
| Percent of males with college education | |||
| Lagged baseline (2008) | 0.21 (0.07, 0.36)* | 0.14 (−0.02, 0.30) | |
| Change since baseline | −0.0 (−0.10, 0.09)* | −0.01 (−0.10, 0.09) | |
| Institutional Opposition Domain | |||
| Hard drug arrest rate per 10,000 | |||
| Lagged baseline (2009) | −0.21 (−0.39, −0.04)* | −0.16 (−0.34, 0.02)* | −0.21 (−0.36, −0.06)* |
| Change since baseline | −0.11 (−0.18, −0.03)* | −0.10 (−0.18, −0.02)* | −0.10 (−0.17, −0.02)* |
| Percent incarcerated males | |||
| Lagged baseline (2009) | −0.19 (−0.33, −0.06)* | −0.15 (−0.28, −0.01) | |
| Change since baseline | 0.01 (−0.08, 0.10)* | 0.01 (−0.08, 0.10) | |
| Police per 1,000 residents | |||
| Lagged baseline (2010) | 0.08 (−0.07, 0.22) | ||
| Change since baseline | 0.05 (−0.01, 0.12) | ||
| Racial Structure Domain | |||
| Percent isolated Black residents | |||
| Lagged baseline (2008) | 0.20 (0.03, 0.37)* | 0.20 (0.03, 0.37)* | 0.02 (−0.15, 0.18) |
| Change since baseline | 0.04 (−0.07, 0.16)* | 0.04 (−0.07, 0.16)* | 0.07 (−0.03, 0.18) |
| Odds ratio of home loan denial for Blacks compared to Whites | |||
| Lagged baseline (2008) | 0.05 (−0.12, 0.21) | ||
| Change since baseline | 0.07 (−0.03, 0.17) | ||
| Black-White poverty inequality ratio | |||
| Lagged baseline (2008) | 0.12 (−0.04, 0.28) | ||
| Change since baseline | 0.01 (−0.08, 0.09) | ||
Three level multilevel model with yearly observations (2011, 2012, 2013, 2014, 2105, 2016) nested within MSA and MSA nested within state. All models include a linear time function.
The outcome was natural log transformed to linearize its association to the independent variables.
2011 to 2016 refers to the timeframe for the outcome. Independent variables were lagged 1–3 years using the lag with the strongest association with the outcome. Note: Independent variables were lagged because we did not expect a change in the independent variables to have an instantaneous effect on the outcome.
Removed from the multivariate model due to multicollinearity assessed using condition indices > 15 and VDP > 0.50.
Significant at the a priori cut point. In bivariate and domain analysis models, independent variables proceeded to the next phase of analysis if the absolute sum of the variable dyad coefficients was |≥.20| or for baseline only variables |≥.10|. Variables in the multivariable model are substantively significant if the standardized coefficient is |≥.10|
Domain Analyses
We included all variables that met the criteria at the bivariate stage in domain analyses. Eight independent variables met the criterion for inclusion in final multivariable model as displayed in Table 2.
Multivariable Analysis
Several baseline variables and one variable dyad (baseline and change since baseline) met the threshold (standardized coefficient ≥ 0.10) for substantive significance in the multivariable model that controlled for time (Table 2). The relationships between the outcome, logged BMSM testing, and baseline BMSM living with HIV (b = 0.28), percent of Black residents employed (b = 0.19), Black heterosexual testing rate (b = 0.46), health expenditures per capita (b = 0.16), ACT UP organization presence (b = 0.19), and SSP presence (b = 0.12) were positive and baseline standardized coefficients for these variables were substantively significant in the multivariable model. Standardized coefficients for hard drug arrest rates, at baseline (b = − 0.21) and change since baseline (b = − 0.10), were substantively significant and hard drug arrests were inversely associated with logged BMSM testing.
Table 3 shows back transformation of the multivariable model and suggests that MSAs with one standard deviation increase in hard drug arrest rates had BMSM testing rates that were 19% lower at baseline and 10% lower over time (in standard deviation units). Substantively significant relationships and the direction of these relationships persisted across bivariate, domain, and multivariable models.
TABLE 3–
Standardized Multilevela Multivariable Results of Regressing Rates of Black MSM Testing Events (per 10,000) Among Black MSM (Aged 15–64 Years) on Structural Independent Variablesb in 85 Large US Metropolitan Statistical Areas, 2011–2016c
| Variable and Domain | Percent Change in Black MSM Testing Rate (in standard deviation units) Per Standard Deviation Increase in the Independent Variabled (CI) |
|---|---|
| Need Domain | |
| Black MSM living with HIV per 10,000 Black MSM | |
| Lagged baseline (2010) | 31.68 (12.30, 54.40)* |
| Change since baseline | −2.29 (−10.8, 7.04) |
| General Resources Domain | |
| Percent Black residents employed | |
| Lagged baseline (2008) | 21.46 (7.56, 37.14)* |
| Change since baseline | 6.37 (−1.79, 15.20) |
| Specialized Resources Domain | |
| Black heterosexual HIV testing rate per 10,000 Black adults | |
| Lagged baseline (2010) | 58.71 (27.35, 97.78)* |
| Change since baseline | 8.98 (0.11, 18.63) |
| Health expenditures per capita ($) | |
| Lagged baseline (2008) | 17.73 (−7.08, 49.15)* |
| Change since baseline | 1.60 (−24.44, 36.59) |
| Liberalism of Public Policies Domain | |
| ACT UP organization presence | |
| Lagged baseline (1990) | 21.01 (−11.48, 65.4)* |
| Syringe service program presence | |
| Lagged baseline (2008) | 12.76 (−12.79, 45.79)* |
| Institutional Opposition Domain | |
| Hard drug arrest rate per 10,000 | |
| Lagged baseline (2009) | −19.27 (−30.54, −6.17)* |
| Change since baseline | −9.50 (−15.49, −2.11)* |
| Racial Structure Domain | |
| Percent isolated Black residents | |
| Lagged baseline (2008) | 1.55 (−13.84, 19.7) |
| Change since baseline | 7.70 (−3.01, 19.59) |
Three level multilevel model with yearly observations (2011, 2012, 2013, 2014, 2105, 2016) nested within MSA and MSAs nested within state. All models include a linear time function.
Variables significant in the final multivariable model shown.
2011 to 2016 refers to the timeframe for the HIV diagnoses outcome. Independent variables were lagged 1–3 years using the lag with the strongest association with the outcome. Note: Independent variables were lagged because we did not expect a change in the independent variables to have an instantaneous effect on the outcome.
Results of back transformation of standardized models with the natural logged outcome to obtain percent change in the MSM testing rate (in standard deviation units) per 1 standard deviation increase in the independent variable.
Binary independent variable.
Significant at the a priori cut point. Variables in the multivariable model are substantively significant if the coefficient is |>.10|
Sensitivity Analysis
We conducted a sensitivity analysis comparing the final model with and without the variable capturing state’s historic passage of laws pertaining to the rights of sexual minorities from the public policy liberalism domain. The state law variable did not proceed beyond the bivariate analysis stage; however, we were interested in how citizenship rights for LGBT persons may be associated with HIV testing rates among BMSM. There were no differences between models with and without the state law variable and the standardized coefficient (b = − 0.05) for this variable did not meet our threshold for substantive significance.
Discussion
This multilevel analysis found that several characteristics of the 85 MSAs in this study are associated with BMSM HIV testing coverage. Relationships between BMSM HIV testing and the following covariates were positive: (1) rates of BMSM living with HIV (b = 0.28); (2) percent of Black residents employed (b = 0.19); (3) Black heterosexual testing rate (b = 0.46); (4) health expenditures per capita (b = 0.16); (5) ACT UP organization presence in 1992 (b = 0.19); and (6) syringe service presence (b = 0.12). Hard drug arrest rates at baseline (b = − 0.21) and change since baseline (b = − 0.10) were inversely associated with the outcome.
This analysis investigated the extent to which characteristics of MSA are associated with rates of BMSM HIV testing. Several studies with the general population and with PWID have found that characteristics of MSAs (e.g., rates of poverty and incarceration) are associated with prevention services for PWID [26–33]. To our knowledge, this is the first analysis to assess which MSA-level characteristics in the US are associated with HIV testing coverage among BMSM. Several MSA-level place predictors were associated with HIV testing rates among BMSM. Need for HIV testing among BMSM as measured by BMSM living with HIV per 10,000 BMSM is positively associated with the outcome. From the general resources domain, we find percentage of Black residents employed is also associated with HIV testing rates among BMSM. As hypothesized, specialized resources as defined by (1) Black heterosexual testing rate; and (2) health expenditures per capita had a positive relationship with the outcome. Support for a program (i.e., liberalism of public policies domain), as measured by (1) ACT UP organization presence; and (2) SSPs were associated with increased HIV testing rates among BMSM testing coverage. Institutional opposition as measured by hard drug arrest rate per 10,000 had a significant and inverse relationship with BMSM testing at both baseline and change. Additionally, no place-level variables from the racial structure domain (as framed by opposition to a program) are associated with HIV testing rates among BMSM. Lastly, state’s historic passage of laws pertaining to the rights of sexual minorities from the public policy liberalism domain did not proceed beyond the bivariate analysis stage.
As hypothesis based on the TCA, epidemiologic need, as measured by BMSM living with HIV per 10,000 BMSM was positively associated with increasing testing coverage for BMSM at baseline. That is, higher rates of BMSM living with HIV at baseline were associated with increases in BMSM testing coverage (b = 0.28) and met our threshold for substantive significance. This finding may indicate that a rise in BMSM living with HIV might motivate MSMs to seek HIV testing and counseling services or for public health policy-makers to make more of these types of services conveniently available. In our past research on program coverage among PWID, we found that the presence of SSPs, (which target PWID) predicts lower AIDS incidence and mortality among heterosexuals [27].
These results may also reflect actions brought about by HIV/AIDS advocacy groups. During and after the introduction of AIDS in 1980s, grass-roots activists and community organizers in hard-hit communities advocated for coordinated prevention and treatment efforts and policies at the national, state, and local level on behalf of communities most affected by increased AIDS transmission [37, 38, 85, 86]. For example, ACT UP had successfully used “direct action” (i.e., political activism strategies such as demonstrations and workplace occupations) to contest the stigmatization of people with AIDS by highlighting the underlying stigmatization rooted in homophobia [37, 85, 86]. Many of the same activists adopted a similar philosophy and tactics in creating and demanding AIDS prevention services for PWID by distributing clean syringes to users regardless of legality. Still, other AIDS advocacy groups founded by Black activists fought for increased AIDS education and treatment in their vulnerable communities, supported by capacity-building organizations like the National Black Leadership Commission on AIDS (NBLCA) [87]. NBLCA’s main mission, for example, is to educate, mobilize, and empower Black leaders to meet the challenge of fighting HIV/AIDS and other health disparities in their local communities [87].
As hypothesized, results imply that resource availability does seem to shape service provision of HIV testing among BMSM. Our model indicates that general resources as measured by percentage of Black residents employed at baseline are important indicators that affect HIV testing among BMSM coverage. For every one standard deviation increase in baseline percentage of Black residents employed there was modest increase (0.19 standard deviation) in BMSM testing events per 10,000.
Additionally, we hypothesized that specialized resources might suggest a concentration of local assets that directly supports a narrow range of programs and/or support a movement for a program or expansion of a program. Previous research measured specialized resources useful for the community action being studied. Such actions have included SPP presence and HIV testing and treatment among PWID [22, 24, 26, 27, 29, 34], as well as a broad range of programs such as providing condom distribution interventions or programs [30–32], or specialized programs for treatment of people who are mentally ill [33, 34]. In the present study we found that, consistent with our hypotheses, health expenditures per capita had a positive relationship with the outcome. That is, having well-funded community health initiatives and programs makes a significance difference in access to HIV services and coverage levels. We also found that specialized resources as measured by Black heterosexual HIV testing per 100,000 is positively associated with baseline HIV testing rates among BMSM. This may reflect a perceived need that places with worse HIV epidemics motivate both MSM and policy-makers to increase HIV testing coverage in low resource areas.
As predicted localize support for a program (i.e., liberalism of public policies) is positively associated with increased HIV testing rates among BMSM. Our results indicate, on average, for every one standard deviation increase in baseline ACT UP presence there was a 0.19 standard deviation increase in BMSM testing events per 10,000, and for every one standard deviation increase in baseline SSP presence there was a 0.12 increase in MSM HIV testing coverage. Our results are consistent with current theory positing that contested HIV services (such as SSPs and drug treatment centers) are often established as a result of political pressure or direct action by grassroots activists and organizations such as ACT UP [27, 49–51, 63]. These results support previous research findings [27, 30, 32, 33, 63]. That is, both active solidarity (ACT UP presence) and potential solidarity (higher percentages of MSM in the population, suggesting more concern for HIV/AIDS issues and education) are positive factors in forming, sustaining and increasing program presence of contested HIV services in the US.
Within the institutional opposition domain standardized coefficients for hard drug arrest rates, both baseline and change since baseline, were substantively significant and hard drug arrests were inversely associated with BMSM testing. For every one standard deviation increase at both baseline (b = − 0.21) and change since baseline (b = − 0.10) in hard core drug arrest there was a significant decrease in BMSM HIV testing coverage. These results parallel similar research on drug arrests associated with PWID [30, 62, 64–66], and are possibly MSAs where the war on drugs—which is deemed as being profoundly racialized—impacts vulnerable people who are marginalized by drug use. As a result, the combined effect of both the war on drug and stigma associated with BMSM may have a negative impact on service utilization and disrupt access to services undermining whether vulnerable BMSM feel comfortable accessing HIV testing and prevention services [12–17, 23, 25]
Lastly, our sensitivity analysis capturing state’s historic passage of laws pertaining to the rights of sexual minorities from the public policy liberalism domain did not proceed beyond the bivariate analysis stage, and was not significant when forced into the multivariable model. Policies protecting or discriminating against subgroups codify treatment and social standing of targeted subgroups; these are a form of structural stigma, which impacts the health of the targeted subgroup through disruption of multiple life domains [15–17, 20, 88]. In the case of citizenship rights for MSM, we would expect MSM in states with laws more protective of sexual minorities to have more favorable trends in HIV testing than those with fewer protections. However, stigma is intersectional, and BMSM are vulnerable to not only stigma towards sexual minority status but also stigma related to racial minority status, manifested through social interactions as well as material differences in health, social, and economic resources due to deeply entrenched patterns of systematic race-based disadvantage in the US [12, 13, 15–17, 20, 88]. Our current findings suggest that among BMSM, these more proximal barriers related to race/ethnicity are more salient to obtaining HIV testing than the more distal exposures of state policies related to MSM minority status.
Limitations
This analysis has several limitations. First, testing data only exist where there are CDC publicly funded HIV counseling and testing sites, restricting the estimate of the percentage of BMSM tested to CDC covered/funded sites only. Thus, our testing rates may be biased to the extent that the demographic distributions of BMSM using these sites differ from those at privately funded sites. Therefore, HIV testing of BMSM occurring at a health maintenance organization, via home testing, or at privately funded clinics is not included in these data and may lead to an underestimation and variations in the number of BMSM tested for HIV. Second, reluctance to identify and report illicit and otherwise stigmatized behaviors (e.g., injection and non-heterosexual sex) may lead to misclassification and underreporting of numbers tested in the counseling and testing data, and this reluctance may vary across MSAs.
This is a study of the universe of large US MSAs with available data rather than of a sample. Our findings are descriptive of the relationships of the measured variables in this universe. They do not, however, imply that these findings can necessarily be extended to smaller MSAs, nonmetropolitan localities, other time periods, or other countries.
Conclusions
The HIV epidemic among BMSM is an urgent public health problem as BMSM are affected by HIV at disproportionate rates. Given the high estimated number of BMSM unaware of their HIV status, it is important to test high risk and vulnerable population for HIV so they become aware of and seek treatment for HIV as early as possible. If current HIV rates persist among BMSM, it is estimated that 1 in 2 BMSM will be diagnosed with HIV during their lifetime [89, 90]. Efforts to reduce HIV incidence and lessen AIDS-related disparities among BMSM in the US—key objectives of the National HIV/AIDS Strategy [10, 11]—require new and improved HIV prevention approaches directed toward BMSM including a fuller understanding of place factors that may influence variation in BMSM testing patterns and risk behavior. There is then, an urgent need to expand access to HIV prevention and treatment for all gay and bisexual men, underscoring the importance of the federal initiative ‘Ending the Epidemic: A Plan for America’ [10, 11].
Achieving HIV elimination will require an infusion of resources to employ strategic practices in places of high HIV burden to implement targeted testing and prevention strategies to BMSM. As such, developing innovative and culturally grounded approaches to improve HIV testing rates among BMSM are crucial in achieving this goal. Innovative and culturally sensitive approaches can work to reduce HIV-related stigma and discrimination while stressing the importance of confidentiality. Likewise, increased state and local funding for community-based programs providing a broad range of health services for both BMSM clients (and family) can help increase BMSM HIV testing rates and decrease risk behaviors especially in low-resource settings.
Our results indicate that structural place-based factors, such as need (i.e., BMSM living with HIV); resources availability (i.e., percentage of Black employed; Black heterosexual HIV testing per 100,000; health expenditure per capita); organized support (i.e., ACT UP and SSP presence) and institutional opposition (as measured by hard code drug arrest) are important MSA-level place factors that shape variation in BMSM HIV testing coverage. More research is needed to understand the influence and geographic variation of structural factors on BMSM HIV testing and service utilization in both high and low resource areas to reduce the burden of HIV among BMSM.
Supplementary Material
Acknowledgements
This research was supported by the National Institutes of Health: “Metropolitan Trajectories of HIV Epidemics and Responses in US Key Populations” (DA037568; HFL Cooper, SR Friedman, R Stall, M Hatzenbuehler MPIs). We thank the Centers and Disease Control and Prevention, Division of HIV/AIDS Prevention Program Evaluation Branch for processing our data request on HIV testing events from the Expanded Testing Program Initiative database (Janet Heitgerd; Guoshen Wang; Lisa Belcher).
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10461-020-02814-4) contains supplementary material, which is available to authorized users.
To create this variable, we examined state policies pertinent to gay/lesbian citizens and created a dichotomous measure of policies over time (from 1999 to 2014) using a growth mixture model. The growth mixture model was based on the number of protective laws in each year and as well as presence or absence two discriminatory laws (LGBT marriage bans and HIV criminalization laws). Policy coding was performed and made available to the authors by LGBT Movement Advancement Project (MAP, lgbtmap.org). The eight laws protective of sexual minorities were those that protected lesbian/gay citizens in the domains of: (1) employment, (2) public accommodations, and (3) housing non-discrimination laws as well as (4) adoption, (5) medical decision making, (6) school anti-bullying, (7) marriage, and (8) anti-hate crime laws. For each year we summed the number of protective laws and subtracted the number of discriminatory laws. We then used a growth mixture model to create the state law variable and assign states to one of two classes. One class reflected states that increasingly passed laws protective of sexual minorities from 1999 to 2014 and the other class included states that did not pass these laws. The state variable was mapped onto MSAs and for multistate MSAs we assigned the state where the majority of the MSA population lived in 2010.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 23 U.S. Cities, 2017. HIV Surveillance Special Report 22. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published February 2019. Accessed July 2019.
- 2.Centers for Disease Control and Prevention. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons receiving HIV care—United States, 2014; MMWR Morb Mortal Wkly Rep. vol. 67, no. 4; February 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV Surveillance Report, Diagnoses of HIV Infection in the United States and Dependent Areas, 2017, Vol. 29; November 2018. HIV diagnosis data are estimates from 50 states, the District of Columbia, and 6 U.S. dependent areas.
- 4.Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010–2016: New HIV Infections among Gay and Bisexual Men. HIV Surveillance Supplemental Report June 2019; 24. [Google Scholar]
- 5.Centers for Disease Control and Prevention. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 20 U.S. cities, 2014. HIV Surveillance Special Report. 2016;15. [Google Scholar]
- 6.Paz-Bailey G, Smith A, Masciotra S, Zhang W, Bingham T, Flynn C, German D, Al-Tayyib A, Magnus M, Lalota M, Owen M. Early HIV infections among men who have sex with men in five cities in the United States. AIDS Behav. 2015;19:2304–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Habarta N, Boudewyns V, Badal H, et al. CDC’S testing makes us stronger (TMUS) campaign: was campaign exposure associated with HIV testing behavior among black gay and bisexual men? AIDS Educ Prev. 2017;29:228–40. [DOI] [PubMed] [Google Scholar]
- 8.Peterson JL, Jones KT. HIV prevention for Black men who have sex with men in the United States. Am J Public Health. 2009;99:976–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2016. HIV Surveillance Supplemental Report. 2018;23. [Google Scholar]
- 10.Ending the HIV epidemic: a plan for America. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Accessed August 2019.
- 11.White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: updated to 2020. July 2015.
- 12.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among Black and White men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21:2083–91. [DOI] [PubMed] [Google Scholar]
- 13.Balaji AB, Bowles KE, Hess KL, Smith JC, Paz-Bailey G, NHBS study group. Association between enacted stigma and HIV-related risk behavior among MSM, National HIV Behavioral Surveillance System, 2011. AIDS Behav. 2017;21(1):227–37. 10.1007/s10461-016-1599-z. [DOI] [PubMed] [Google Scholar]
- 14.Chandler C, Bukowski LA, Egan JE, Hawk M, Matthews D, Markovic N, Stall R. Examining the impact of a psychosocial syndemic on past six-month HIV screening behavior of black men who have sex with men in the United States: results from the POWER study. AIDS Behav. 2019. 10.1080/09540121.2019.1659921. [DOI] [PMC free article] [PubMed]
- 15.Matthews DD, Sang JM, Chandler CJ, Bukowski LA, Friedman MR, Eaton LA, Stall RD. Black men who have sex with men and lifetime HIV testing: characterizing the reasons and consequences of having never tested for HIV. Prev Sci. 2019. 10.1007/s11121-019-01022-4 (In press). [DOI] [PMC free article] [PubMed]
- 16.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389:1453–63. 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- 17.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Soc Sci Med. 2014;103:1–6. 10.1016/j.socscimed.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 18.Spielberg F, Branson BM, Goldbaum GM, Lockhart D, Kurth A, Celum CL, et al. Overcoming barriers to HIV testing: preferences for new strategies among clients of a needle exchange, a sexually transmitted disease clinic, and sex venues for men who have sex with men. J Acquir Immune Defic Syndr. 2003;32:318–27. [DOI] [PubMed] [Google Scholar]
- 19.Newman LM, Berman SM. Epidemiology of STD disparities in African American communities. Sex Transm Dis. 2008;35:S4–S12. [DOI] [PubMed] [Google Scholar]
- 20.Ayala G, Bingham T, Kim J, Wheeler DP, Millett GA. Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. Am J Public Health. 2012;102:S242–S249249. 10.2105/AJPH.2011.300641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in Black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–8. [DOI] [PubMed] [Google Scholar]
- 22.Brooks RA, Etzel MA, Hinojos E, Henry CL, Perez M. Preventing HIV among Latino and African American gay and bisexual men in a context of HIV-related stigma, discrimination, and homophobia: perspectives of providers. AIDS Patient Care STDS. 2005;19:737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levy ME, Wilton L, Phillips G 2nd, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014;18:972–96. 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mays VM, Cochran SD, Zamudio A. HIV prevention research: are we meeting the needs of African American men who have sex with men? J Black Psychol. 2004;30:78–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maulsby C, Millett G, Lindsey K, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18:10–25. [DOI] [PubMed] [Google Scholar]
- 26.Tempalski B, Cooper HLF, Kelley ME, Linton SL, Wolfe ME, Chen YT, et al. Identifying which place characteristics are associated with the odds of recent HIV testing in a large sample of people who inject drugs in 19 US metropolitan areas. AIDS Behav. 2018. 10.1007/s10461-018-2217-z. [DOI] [PMC free article] [PubMed]
- 27.Friedman SR, West BS, Tempalski B, et al. Do metropolitan HIV epidemic histories and programs for people who inject drugs and men who have sex with men predict AIDS incidence and mortality among heterosexuals? Annals Epidemiol. 2014;24:304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tempalski B, Flom PL, Friedman SR, Des Jarlais DC, Friedman JJ, McKnight C, et al. Social and political factors predicting the presence of syringe exchange programs in 96 US metropolitan areas. Am J Public Health. 2007;97:437–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Friedman SR, Tempalski B, Cooper H, Perlis T, Keem M, et al. Estimating numbers of injecting drug users in metropolitan areas for structural analyses of community vulnerability and for assessing relative degrees of service provision for injecting drug users. J Urban Health. 2004;81:377–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Friedman SR, Tempalski B, Brady JE, et al. Income inequality, drug-related arrests, and the health of people who inject drugs: Reflections on seventeen years of research. Int J Drug Policy. 2016;32:11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedman SR, Tempalski B, Brady J, Friedman JJ, Cooper HL, et al. Predictors of the degree of drug treatment coverage for injection drug users in 94 metropolitan areas in the United States. Int J Drug Policy. 2007;18:475–85. [DOI] [PubMed] [Google Scholar]
- 32.Tempalski B, Cooper H, Friedman SR, Des Jarlais DC, Brady J. Correlates of syringe coverage for heroin injection in 35 large metropolitan areas in the US in which heroin is the dominant injected drug. Int J Drug Policy. 2008;19:S47–S58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tempalski B, Williams LD, West BS, Cooper HLF, Beane S, Ibragimov U, Friedman SR. Predictors of historical change in drug treatment coverage among people who inject drugs in 90 large metropolitan areas in the USA, 1993–2007. Subst Abuse Treatm Prev Policy. 2020. In Press [DOI] [PMC free article] [PubMed]
- 34.Smith N Uneven development: nature, capital and the production of space. New York: Basil Blackwell; 1991. [Google Scholar]
- 35.Mitchell D The right to the city: social justice and the fight for public space in America. New York: Guilford; 2003. [Google Scholar]
- 36.Blomley NK. Unsettling the city: urban land and the politics of property. New York: Routledge; 2004. [Google Scholar]
- 37.Stoller NE. Lessons from the damned: queers, whores, and junkies respond to AIDS. New York, NY: Routledge; 1998. [Google Scholar]
- 38.Risse GB. Epidemics and history: ecological perspectives and social responses In: Fee E, Fox DM, editors. AIDS: the burdens of history. Berkeley: University of California Press; 1988. p. 33–66. [Google Scholar]
- 39.Keith M, Pile S, editors. Geographies of resistance. London: Routledge; 1997. [Google Scholar]
- 40.Rogers E Diffusion of innovations. New York: The Free Press; 2003. [Google Scholar]
- 41.Barker K Diffusion of innovations: a world tour. Journal of Communication. 2004;9:131–7. [DOI] [PubMed] [Google Scholar]
- 42.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ. 1998;317:465–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Des Jarlais DC, Sloboda Z, Friedman SR, Tempalski B, McKnight C, Braine N. Comparing the diffusion of D.A.R.E and syringe exchange programs. Am J Public Health. 2006;96:1354–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rosser BRS, Horvath KJ. Predictors of success in HIV prevention in rural America: a state level structural factor analysis of HIV prevention targeting men who have sex with men. AIDS Behav. 2008;12:159–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mahnaz RC, Crepaz N, Guenther-Gray C, Henny K, Liau A, Willis LA, Lyles CM. Efficacy of structural-level condom distribution interventions: a meta-analysis of U.S. and International Studies, 1998–2007. AIDS Behav. 2011;15(7):1283–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abdul-Quader AS, Feelemyer J, Modi S, Stein ES, Briceno A, Semaan S, et al. Effectiveness of structural-level needle/syringe programs to reduce HCV and HIV infection among people who inject drugs: a systematic review. AIDS Behav. 2013;17(9):2878–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Des Jarlais DC, Paone D, Friedman SR, Peyser N, Newman RG. Public health then and now: regulating controversial programs for unpopular people: methadone maintenance and syringe-exchange programs. Am J Public Health. 1995;85:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kresina TF, Lubran R. Improving public health through access to and utilization of medication assisted treatment. Int J Environ Res Public Health. 2011;8:4102–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Downing M, Riess TH, Vernon K, Mulia N, Hollinquest M, McKnight C, et al. It takes a community: successful implementation of syringe exchange programs. AIDS Educ Prev. 2005;17:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bluthenthal RN. Syringe exchange as a social movement: a case study of harm reduction in Oakland. Calif Subst Use Misuse. 1998;33:1147–71. [DOI] [PubMed] [Google Scholar]
- 51.Shaw SJ. Public citizens, marginalized communities: The struggle for syringe exchange in Springfield, Massachusetts. Med Anthropol. 2006;25:31–633. [DOI] [PubMed] [Google Scholar]
- 52.Beatty PW, Hagglund KJ, Neri MT, Dhont KR, Clark MJ, Hilton SA. Access to health care services among people with chronic or disabling conditions: patterns and predictors. Arch Phys Med Rehab. 2003;84:1417–25. [DOI] [PubMed] [Google Scholar]
- 53.Drainoni ML, Lee-Hood E, Tobia C, Bachman S, Andrew J, Maisels L. Cross-disability experiences of barriers of health-care access. J Disabil Policy Stud. 2006;17:101–15. [Google Scholar]
- 54.Latkin C, Weeks MR, Glasman L, Galletly C, Albarracin D. A dynamic social systems model for considering structural factors in HIV prevention and detection. AIDS Behav. 2010;14:S222–S23838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sheppard VB, Hannon M, Barbosa CE, Pestian JP. From research to community action: an assessment of child and adolescent hospitalizations. Fam Commun Health. 1999;22:1. [Google Scholar]
- 56.Hoffman B Health care reform and social movements in the United States. Am J Public Health. 2003;93:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brown P, Zavestoski S, McComiick S, Mayer B, Morello-Frosch R, Gasior R. Embodied health movements: new approaches to social movements in health. Soc Health Illness. 2004;26:50–80. [DOI] [PubMed] [Google Scholar]
- 58.DeMarco R, Johnsen C. Taking action in communities: women living with HIV/AIDS lead the way. J Comm Health Nursing. 2003;20:1. [DOI] [PubMed] [Google Scholar]
- 59.Chiotti QP, Joseph AE. Casey house: interpreting the location of a Toronto AIDS hospice. Soc Sci Med. 1995;41:131–40. [DOI] [PubMed] [Google Scholar]
- 60.Barnett R, Barnett P. If you want to sit on your butts you’ll get nothing!: community activism in response to threats of rural hospital closure in southern New Zealand. Health Place. 2003;9:2. [DOI] [PubMed] [Google Scholar]
- 61.Poland B, Boutilier M, Tobin S, Badgley R. The policy context for community development practice in public health: a Canadian case study. J Public Health Policy. 2000;21:1. [PubMed] [Google Scholar]
- 62.Tempalski B, Friedman R, Keem M, Cooper HLF, Friedman SR. NIMBY localism and national inequitable exclusion alliances: the case of syringe exchange programs in the United States. Geoforum. 2007;38:1250–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tempalski B Placing the dynamics of syringe exchange programs in the United States. Health Place. 2007;13:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Friedman SR, Cooper HLF, Tempalski B, Keem M, Friedman R, Flom PL, et al. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in U.S.A. Metropolitan Areas. AIDS. 2006;20:93–9. [DOI] [PubMed] [Google Scholar]
- 65.Friedman SR, Pouget ER, Chatterjee S, Cleland CM, Tempalski B, Brady JE, et al. Do drug arrests deter injection drug use? Am J Public Health. 2011;101:344–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cooper HLF, Des Jarlais DC, Tempalski B, Bossak B, Ross Z, Friedman SR. Drug-related arrest rates and spatial access to syringe exchange programs in New York City health districts: combined effects on the risk of injection-related infections among injectors. Health Place. 2012;18:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Des Jarlais DC, Pinkerton S, Hagan H, Guardino V, Feelemyer J, Cooper HL, et al. 30 years on selected issues in the prevention of HIV among persons who inject drugs. Adv Prev Med. 2013. 10.1155/2013/346372. [DOI] [PMC free article] [PubMed]
- 68.Dear M, Wilton R, Gaber SL, Takahashi LM. Seeing people differently: the sociospatial construction of disability. Society Space Environ Planning. 1997;15:455–80. [Google Scholar]
- 69.Law R. Communities, citizens, and the perceived importance of AIDS-related services in West Hollywood, California. Health Place. 2003;9:7–22. [DOI] [PubMed] [Google Scholar]
- 70.Law RM, Takahashi LM. HIV, AIDS and human services: Exploring public attitudes in West Hollywood. Calif Health Social Care Commun. 2000;8:90–108. [DOI] [PubMed] [Google Scholar]
- 71.Lyon-Callo V Making sense of NIMBY: poverty, power and community opposition to homeless shelters. City Comm. 2001;13:183–209. [Google Scholar]
- 72.Petchey R, Williams J, Farnsworth B, Starkey K. A tale of two (low prevalence) cities: social movement organizations and the local policy response to HIV/AIDS. Soc Sci Med. 1998;47:9. [DOI] [PubMed] [Google Scholar]
- 73.Takahashi LM. Homelessness, AIDS, and stigmatization. Oxford: Clarendon Press; 1998. [Google Scholar]
- 74.Centers for Disease Control and Prevention. HIV/AIDS Surveillance Branch. National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Expanded Testing Program Initiative (ETP) data 2011–2016.
- 75.Newport F In U.S., Estimate of LGBT Population Rises to 4.5%. Gallup News. https://news.gallup.com/poll/234863/estimate-lgbt-population-rises.aspx. Accessed 22 May 2018.
- 76.Intercensal estimates of the resident population by sex, race, and Hispanic origin for counties Intercensal Estimates of the Resident Population. Washington, DC: US Census Bureau; 2011–2016 [Google Scholar]
- 77.Singer JD, Willett JB. Applied longitudinal data analysis: modeling change and event occurrence. Oxford: Oxford University Press; 2003. [Google Scholar]
- 78.Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods, vol. 1 Thousand Oaks: Sage; 2002. [Google Scholar]
- 79.Greenland S, Senn SJ, Rothman KJ, et al. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Euro J Epidemiol. 2016;31:337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Figueiredo Filho DB, Paranhos R, Rocha EC, et al. When is statistical significance not significant? Braz Polit Sci Rev. 2013;7(1):31–55. [Google Scholar]
- 81.Cooper HLF, West B, Linton S, et al. Contextual predictors of injection drug use among black adolescents and adults in US Metropolitan Areas, 1993–2007. Am J Public Health. 2016;106:517–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.SAS Institute Inc. SAS 9.4. Cary, NC: SAS Institute Inc. [Google Scholar]
- 83.SAS Institute I. SAS/STAT(R) 9.2 User’s Guide. Collinearity diagnostics. 2010. https://support.sas.com/documentation/cdl/en/statug/63033/HTML/default/viewer.htm#statug_reg_sect038.htm.
- 84.Yang J Interpreting coefficients in regression with log-transformed variables. Ithaca: Cornell University; 2012. [Google Scholar]
- 85.Brown MP. Replacing citizenship: AIDS activism and radical democracy. New York: Guilford Press; 1997. [Google Scholar]
- 86.Epstein S Impure science: AIDS, activism, and the politics of knowledge. Berkeley: University of California Press; 1996. [PubMed] [Google Scholar]
- 87.National Black Leadership Commission on AIDS. https://nblca.org/mission-history/. Accessed August 2019.
- 88.Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103:813–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Centers for Disease Control & Prevention. Press release: lifetime risk of HIV diagnosis. 2016.
- 90.Centers for Disease Control & Prevention. Pre-exposure prophylaxis (PrEP). Accessed July 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.