Abstract
Objective
The purpose of this study was to evaluate the types and the frequency of fractures, both in the pediatric and adult population during the COVID-19 pandemic and to find out the differences in comparison to the non-pandemic period.
Methods
Patients who were admitted to the hospital with a new fracture during pandemic period (March 16 to May 22, 2020) were evaluated. Control group consisted of patients with new fractures admitted to the hospital in the same date range in 2018 and 2019. The patients were divided into two groups as ≤16 years old (group 1) and >16 years old (group 2). The evaluation was based on the age and gender of the patients and localization of the fractures. Hospitalized and surgically treated patients were evaluated as well.
Results
A total of 1794, 1747, and 670 fractures were observed in 2018, 2019, and 2020, respectively. Mean age of the patients in group 1 was found to have decreased in the pandemic period (p<0.001). The most common fracture sites in the pediatric population were the distal forearm and distal arm, whereas hand, distal forearm, and foot were most common fracture sites in adults, in both pandemic and non-pandemic periods. The proportional increase in femoral and tibial shaft fractures in group 1, and toe, tibial shaft, and metacarpal fractures in group 2 was found to be statistically significantly (p<0.05). In group 1; 6.8%, 7.7%, and 14.6% of the fractures were treated surgically in 2018, 2019, and 2020, respectively (p<0.001). For group 2, these rates were 20.1%, 18.6%, and 18.1%, respectively (p=0.67). There were 48, 29, and 26 open fractures in 2018, 2019 and 2020, respectively (p=0.066). In pandemic period, duration of the hospital stay was significantly shorter for distal humerus and proximal femur fractures (p values= 0.001 and 0.017, respectively).
Conclusion
We observed that the frequency of fractures decreased by approximately one-third during the pandemic period compared with that in the non-pandemic period. The mean age of the patients with a fracture in the pediatric group was found to have decreased also. Finger fractures in pediatric patients and metatarsal fractures in adult patients were found to have significantly decreased during the pandemic.
Level of Evidence
Level III, Diagnostic study
Keywords: COVID 19, Pandemic, Fracture, Orthopedics, Hospitalization,
Introduction
A novel type of Corona virus was identified as an etiologic factor for fatal pneumonia in Wuhan-China and afterward, a global spread occurred (1). The World Health Organization declared this infection as a pandemic on 11 March 2020 (2). This date is also the date when the first case was reported in Turkey. Due to the lack of preventive vaccines and therapeutic drugs, public health measures such as isolation, social distancing, and quarantine were the only elective ways to prevent the spread of the disease (3).
Shortly after the detection of the first case in Turkey, serious measures were taken in order to reduce the spread of the disease. These measures included closing of schools and starting the online and television-based distance education, and curfew for people over and under the age of 65 and 20, respectively. Places where people meet each other, such as cinema, theater, and shopping centers, were also closed to prevent close contact. Public was warned not to go to outpatient clinics in compulsory cases in order not to create crowds in hospitals. Elective surgeries were postponed. Flexible working modalities were emphasized to public employees in order to prevent the spread of the virus. As a result of all these measures, outdoor mobility has decreased significantly.
Falls from a height, simple falls in the elderly, after-school activities of children, sport injuries, and traffic accidents are all well-known etiologic factors for the occurrence of fractures (4–6). We hypothesized that the incidence of fractures would be decreased in every part of the body during the period of COVID 19 pandemic.
The purpose of this study was to evaluate the types and incidence of fractures treated during the pandemic and compare them with the same time period without pandemic, in order to shed light on the situations that should be prepared for orthopedic trauma surgeons in extraordinary situations that may be seen in the future.
Materials and Methods
Local ethical committee approval was obtained for this retrospective cohort study (number: 2020/6-12, date:13/05/2020). The data of patients who were admitted to a tertiary care hospital, where trauma patients are frequently admitted, were gathered from the digital archive. Patients who were admitted to the hospital with a new fracture between the time period of March 16 and May 22 in 2018, 2019, and 2020 were included. Patients with a diagnosis other than fracture and re-admissions with the same fracture were excluded from the study. Pandemic period for COVID 19 was accepted as between March 16 and May 22 of 2020. The same time periods in 2018 and 2019 were accepted as non-pandemic periods.
Patients who were admitted and examined by orthopedic surgeons in both emergency departments and outpatient clinics were sought from the hospital’s digital archive. A second analysis was performed to exclude the patients with same identification number and repeated hospital admissions. Afterwards, International Statistical Classification of Diseases and Related Health Problems (ICD) 10 codes of fractures were analyzed. Patients mistakenly coded with a diagnosis of fracture were excluded as well. Finally, 1717, 1634, and 645 patients with 1794, 1747, and 670 fractures from years 2018, 2019, and 2020, respectively, were included in the study. Flowchart of the study population is shown in Table 1.
Table 1.
Flowchart of the study
| March 16–May 22 | |||
|---|---|---|---|
|
| |||
| 2018 | 2019 | 2020 | |
| Number of patients admitted to the orthopedics department | 19707 | 18224 | 5420 |
| Number of patients after excluding duplicated records | 12786 | 13086 | 2290 |
| Number of patients with an ICD code of fracture | 2906 | 3022 | 906 |
| Number of patients after excluding patients coded with the diagnosis of fracture accidentally and recurrent admission | 1717 | 1634 | 645 |
| Number of fractures | 1794 | 1747 | 670 |
The patients were divided into two groups as “less than or equal to 16 years old” and “more than 16 years old’’ in order to further analyze the fractures of pediatric and older age groups. The data in 2018, 2019, and 2020 were compared with each other.
Age, gender, and fracture areas were recorded. Patients who were hospitalized and operated in central operating theaters were scanned from the clinical archive. Patients operated due to a fracture were investigated. As most common operated fractures, distal humeral and proximal femoral fractures were additionally analyzed and compared for their length of hospital stays and time to operations. If the patients need hospitalization, they were examined to rule out COVID 19 infection. When there is a suspicious situation, Polymerase Chain Reaction test was performed, and the management was performed accordingly.
Statistical analysis
Statistical package for Social Sciences version 24 (IBM SPSS Corp, Armonk, NY, USA) was used for the statistical analysis. The Shapiro-Wilk test was used to evaluate the normality of groups. For the normally distributed data, t and ANOVA tests were used to compare two and more than two groups, respectively. If the distribution of data was not normal, Mann–Whitney U and Kruskal–Wallis tests were used to compare two and more than two groups, respectively. Categorical data were analyzed by using Fisher exact or chi-squared tests. Proportion comparisons of fracture and surgical treatment rates between years were made with Fisher’s exact test developed for rXc tables with Bonferroni-corrected two-rate z test. A p value below than 0.05 was accepted as statistically significant.
Results
A total of 1794, 1747, and 670 fractures were observed in 2018, 2019, and 2020 year periods, respectively. Fractures were observed more commonly in the patients of group 1 in 2018, 2019, and 2020 year periods, respectively (56.4%, 55.4%, and 52.2%, respectively) (Figure 1). A total of 1011, 967, and 350 of the fractures were observed in group 1 patients in 2018, 2019, and 2020, respectively (Figures 2–4 and table 2). The mean age of the patients in group 1 was 8.2±4.3 (range, 0–16), 8.6±4.2 (range, 0–16) and 7.1±4.4 (0–16) years for three periods, respectively. When the age values of these three years were compared with each other, there was a statistically significant difference (p<0.001). The mean age of the patients in group 2 was 45.3±17.8 (range 17–91), 45.5±17.9 (range 17–98), and 45.2±19.5 (range 17–91), respectively. There was no statistically significant difference (p=0.92). Three hundred fifty-four (34.8%), 331 (34.2%), and 132 (37.7) of group 1 patients of three periods were female, respectively (p=0.82). Three hundred fifty-six (45.5%), 348 (44.6%), and 131 (40.9%) of group 2 patients of three periods were female, respectively (p=0.58) (Table 3). The number of the fractures was observed to be decreased significantly in the pandemic period (37.3% and 38.4% of fractures in the period between 2018 and 2019, respectively). The most common locations of the fractures were distal forearm and distal arm in group 1 and hand, distal forearm, and foot in group 2 (Figures 2–4 and Tables 4a and 4b). There was a statistically significantly proportional increase in femoral and tibial shaft fractures in the pandemic period in group 1. Finger fractures were found to be statistically significantly decreased in group 1 in the pandemic period (Table 4a). In group 2, the proportion of toe, tibia shaft, and metacarpal fractures were found to be increased and as opposed to this, proportion of metatarsal fractures were found to be statistically significantly decreased in the pandemic period (Table 4b). No statistically significant difference was observed in the proportion of surgical treatments, except for metacarpal fractures (Table 4b). Five hundred and thirty-six, 542, and 155 fractures were observed in the hospitalized patients in 2018, 2019, and 2020 periods, respectively. Four hundred and four, 464, and 138 patients were operated in the central operation theatres in years 2018, 2019, and 2020, respectively. Two hundred and twenty-six, 219, and 102 of these operations were performed because of fractures in 2018, 2019, and 2020 periods, respectively (Table 2 and Table 4b). It was apparent that the number of operations other than for fracture etiology had decreased statistically significantly in the pandemic period (44.1%, 52.8%, and 26.1%, respectively) (p<0.001). The diagnosis of the patients who were operated for a reason other than a fracture were mostly musculoskeletal infections or peripheral complication of diabetes. None of the elective surgeries such as foot surgery, hand surgery, and arthroplasty were performed during the pandemic period.
Figure 1.
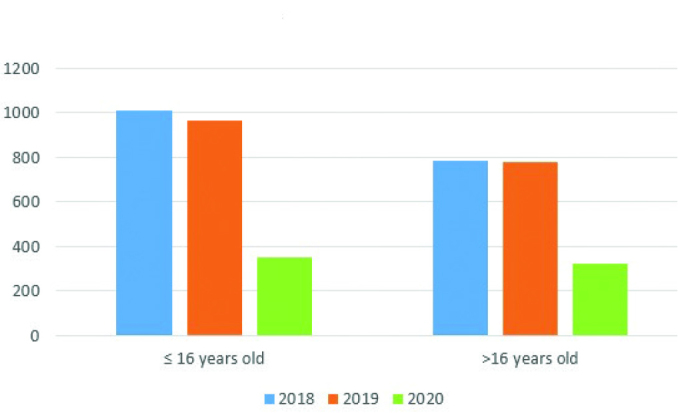
Chart of the number of fractures observed in pediatric and older groups in 2018, 2019, and 2020 periods
Figure 2.
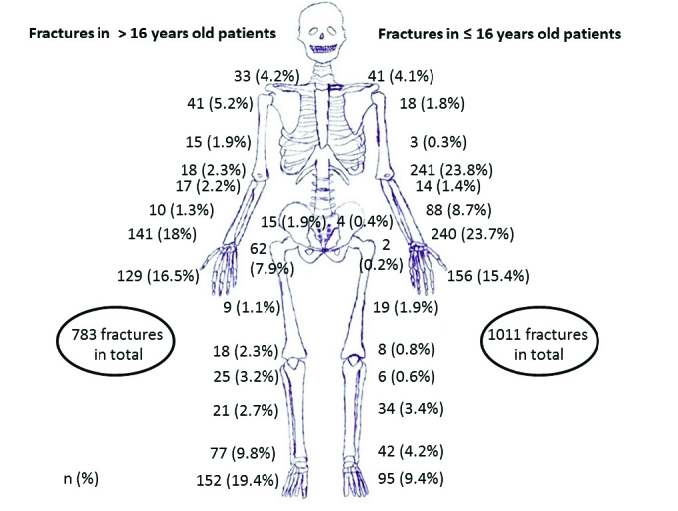
Numbers and locations of fractures between March 16 and May 22 of 2018
Figure 3.
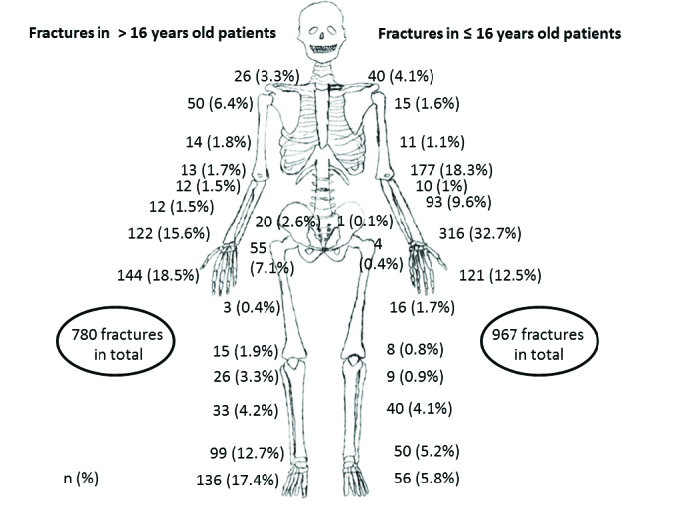
Numbers and locations of fractures between March 16 and May 22 of 2019
Figure 4.
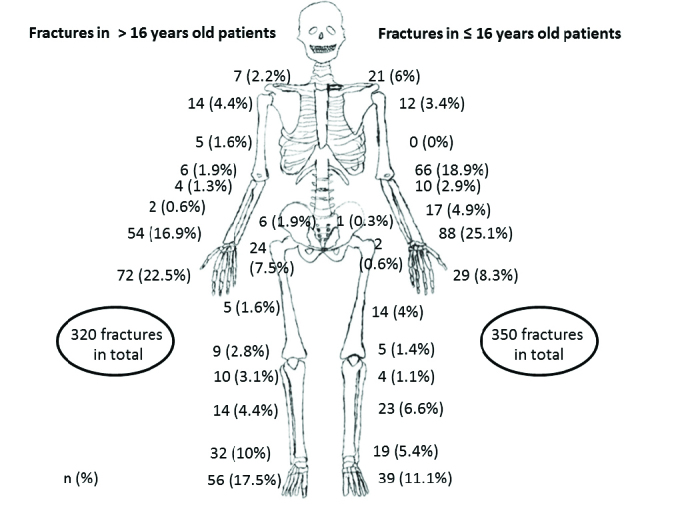
Numbers and locations of fractures between March 16 and May 22, 2020 (pandemic)
Table 2.
Detailed information about the studied population in terms of fractures and treatments according to the years, *total number of cases who were operated by Orthopedics and Traumatology Department
| March 16–May 22 | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| 2018 | 2019 | 2020 | ||||
| Total patients (n) | 12786 | 13086 | 2290 | |||
| Age | ≤16 y.o. |
>16 y.o. |
≤16 y.o. |
>16 y.o. |
≤16 y.o. |
>16 y.o. |
| Number | 4042 | 8744 | 4307 | 8779 | 838 | 1452 |
| Patients with | ||||||
| fracture(s) (n:) | 973 | 744 | 902 | 732 | 341 | 304 |
| Fracture (n:) | 1011 | 783 | 967 | 780 | 350 | 320 |
| Number of fractures in hospitalized fractures(n:) | 252 | 284 | 226 | 316 | 76 | 79 |
| Surgical treatment(n:)* | 162 | 242 | 181 | 283 | 68 | 74 |
| Surgery for fracture(n:) | 69 | 157 | 74 | 145 | 51 | 58 |
Table 3.
Genders and mean ages of the both ≤16 years old and >16 years old patients
| Patients with a fracture | Patients who were treated surgically for a fracture | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| ≤16 years old (group 1) | >16 years old (group 2) | ≤16 years old (group 1) | >16 years old (group 2) | |||||
|
| ||||||||
| Girl (n:) mean age±std. dev. (min–max) | Boy (n:) mean age±std. dev. (min–max) | Female (n:) mean age±std. dev. (min–max) | Male (n:) mean age±std. dev. (min–max) | Girl (n:) mean age±std. dev. (min–max) | Boy (n:) mean age±std. dev. (min–max) | Female (n:) mean age±std. dev. (min–max) | Male (n:) mean age±std. dev. (min–max) | |
| 2018 | (n:354) 7.1±4.3 (0–16) | (n:657) 8.7±4.2 (0–16) | (n:356) 51.2±17.4 (17–90) | (n:427) 40.3±16.6 (17–91) | (n:28) 6.2±3.4 (1–16) | (n:41) 8.4±3.9 (2–16) | (n:66) 61.6±19.4 (19–90) | (n:91) 44.7±20.2 (17–91) |
| 2019 | (n:331) 7.6±4.1 (0–16) | (n:636) 9.1±4.2 (0–16) | (n:348) 52.7±17.3 (17–94) | (n:432) 39.8±16.4 (17–98) | (n:28) 6.1±3.3 (2–15) | (n:46) 8.9±4.4 (2–16) | (n:61) 62.4±20.2 (20–94) | (n:84) 48.1±20.9 (17–94) |
| 2020 | (n:132) 5.8±3.8 (0–16) | (n:218) 7.8±4.7 (0–16) | (n:131) 55.2±19.6 (17–91) | (n:189) 38.2±16.3 (17–88) | (n:20) 5.9±3.7 (1–14) | (n:31) 6.1±4.6 (1–15) | (n:24) 64.1±18.6 (26–87) | (n:34) 43.9±22.4 (18–87) |
Table 4a.
Number of fractures, surgically treated fractures and percentages of surgical treatments according to the body regions in ≤ 16 years old patients (group 1)
| Year 2018 (16 March to 22 May) | Year 2019 (16 March to 22 May) | Year 2020 (16 March to 22 May) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Fractures [n (%)] | Surgically treated [n (%)] | Surgical treatment percentage (%) | Fractures [n (%)] | Surgically treated [n (%)] | Surgical treatment percentage (%) | Fractures [n (%)] | Surgically treated [n (%)] | Surgical treatment percentage (%) | |
|
|
|
|
|||||||
| Toe | 46 (4.5) | 0 (0) | 0 | 19 (2) | 0 (0) | 0 | 17 (4.9) | 0 (0) | 0 |
| Metatarsal | 48 (4.7) | 0 (0) | 0 | 37 (3.8) | 0 (0) | 0 | 20 (5.7) | 0 (0) | 0 |
| Calcaneus/talus | 1 (0.1) | 0 (0) | 0 | 0 (0) | 0 (0) | 0 | 2 (0.6) | 0 (0) | 0 |
| Ankle | 42 (4.2) | 2 (2.9) | 4.8 | 50 (5.2) | 3 (4.1) | 6 | 19 (5.4) | 4 (7.8) | 21 |
| Tibia shaft* | 34 (3.4) | 1 (1.4) | 2.9 | 40 (4.1) | 3 (4.1) | 7.5 | 23 (6.6) | 0 (0) | 0 |
| Proximal tibia | 6 (0.6) | 2 (2.9) | 33.3 | 9 (0.9) | 0 (0) | 0 | 4 (1.1) | 0 (0) | 0 |
| Distal femur | 5 (0.5) | 1 (1.4) | 20 | 5 (0.5) | 0 (0) | 0 | 4 (1.1) | 0 (0) | 0 |
| Patella | 3 (0.3) | 0 (0) | 0 | 3 (0.3) | 1 (1.4) | 33.3 | 1 (0.3) | 1 (2) | 100 |
| Femur shaft* | 19 (1.9) | 5 (7.2) | 26.3 | 16 (1.7) | 4 (5.4) | 25 | 14 (4) | 7 (13.7) | 50 |
| Proximal femur | 2 (0.2) | 1 (1.4) | 50 | 4 (0.4) | 0 (0) | 0 | 2 (0.6) | 0 (0) | 0 |
| Pelvic ring | 3 (0.3) | 0 (0) | 0 | 1 (0.1) | 0 (0) | 0 | 1 (0.3) | 0 (0) | 0 |
| Acetabulum | 1 (0.1) | 0 (0) | 0 | 0 (0) | 0 (0) | 0 | 0 (0) | 0 (0) | 0 |
| Finger* | 128 (12.7) | 1 (1.4) | 0.7 | 100 (10.3) | 1 (1.4) | 1 | 15 (4.3) | 1 (2) | 6.7 |
| Metacarpal | 26 (2.6) | 0 (0) | 0 | 18 (1.9) | 1 (1.4) | 5.55 | 12 (3.4) | 0 (0) | 0 |
| Carpal | 2 (0.2) | 0 (0) | 0 | 3 (0.3) | 0 (0) | 0 | 2 (0.6) | 0 (0) | 0 |
| Distal radius-ulna | 240 (23.7) | 2 (2.9) | 0.8 | 316 (32.7) | 2 (2.7) | 0.6 | 88 (25.1) | 0 (0) | 0 |
| Radius-ulna shaft | 88 (8.7) | 3 (4.3) | 3.4 | 93 (9.6) | 5 (6.8) | 5.4 | 17 (4.9) | 2 | 0 |
| Proximal radius-ulna | 14 (1.4) | 2 (2.9) | 14.3 | 10 (1) | 1 (1.4) | 10 | 10 (2.9) | 0 (0) | 0 |
| Distal humerus | 241 (23.8) | 48 (69.6) | 19.9 | 177 (18.3) | 50 (67.6) | 28.2 | 66 (18.9) | 36 (70.6) | 54.5 |
| Humerus shaft | 3 (0.3) | 0 (0) | 0 | 11 (1.1) | 0 (0) | 0 | 0 (0) | 0 (0) | 0 |
| Proximal humerus | 18 (1.8) | 1 (1.4) | 5.5 | 15 (1.6) | 2 (2.7) | 13.3 | 12 (3.4) | 0 (0) | 0 |
| Clavicle | 39 (3.9) | 0 (0) | 0 | 40 (4.1) | 1 (1.4) | 2.5 | 20 (5.7) | 0 (0) | 0 |
| Scapula | 2 (0.2) | 0 (0) | 0 | 0 (0) | 0 (0) | 0 | 1 (0.3) | 0 (0) | 0 |
| Total | 1,011 (100) | 69 (100) | 6.8a | 967 (100) | 74 (100) | 7.7b | 350 (100) | 51 (100) | 14.6c |
statistically significantly different in the pandemic period in terms of proportional fracture frequency
p<0.001 for the comparison of a, b, and c
Table 4b.
Number of fractures, surgically treated fractures and percentages of surgical treatments according to the body regions in patients older than 16 years old (group 2)
| Year 2018 (16 March to 22 May) | Surgical treatment percentage (%) | Year 2019 (16 March to 22 May) | Surgical treatment percentage (%) | Year 2020 (16 March to 22 May) | Surgical treatment percentage (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Fractures [n (%)] | Surgically treated [n (%)] | Fractures [n (%)] | Surgically treated [n (%)] | Fractures [n (%)] | Surgically treated [n (%)] | ||||
|
|
|
|
|
|
|
||||
| Toe* | 57 (7.3) | 0 (0) | 0 | 43 (5.5) | 0 (0) | 0 | 42 (13.1) | 0 (0) | 0 |
| Metatarsal* | 77 (9.8) | 3 (1.9) | 3.9 | 69 (8.8) | 2 (1.4) | 2.9 | 10 (3.1) | 2 (3.4) | 20 |
| Calcaneus/talus | 18 (2.3) | 2 (1.3) | 11.1 | 24 (3.1) | 2 (1.4) | 8.3 | 4 (1.3) | 1 (1.7) | 25 |
| Ankle | 77 (9.8) | 17 (10.8) | 22.1 | 99 (12.7) | 15 (10.3) | 15.1 | 32 (10) | 7 (12.1) | 21.9 |
| Tibia shaft* | 21 (2.7) | 18 (11.5) | 85.7 | 33 (4.2) | 21 (14.5) | 63.6 | 14 (4.4) | 6 (10.3) | 42.9 |
| Proximal tibia | 25 (3.2) | 8 (5.1) | 32 | 26 (3.3) | 5 (3.4) | 19.2 | 10 (3.1) | 4 (6.9) | 40 |
| Distal femur | 5 (0.6) | 3 (1.9) | 60 | 4 (0.5) | 3 (2.1) | 75 | 4 (1.3) | 1 (1.7) | 25 |
| Patella | 13 (1.7) | 3 (1.9) | 23.1 | 11 (1.4) | 2 (1.4) | 18.2 | 5 (1.6) | 2 (3.4) | 40 |
| Femur shaft | 9 (1.1) | 8 (5.1) | 88.9 | 3 (0.4) | 3 (2.1) | 100 | 5 (1.6) | 5 (8.6) | 100 |
| Proximal femur | 62 (7.9) | 49 (31.2) | 79 | 55 (7.1) | 47 (32.4) | 85.4 | 24 (7.5) | 14 (24.1) | 58.3 |
| Pelvic ring | 8 (1) | 0 (0) | 0 | 14 (1.8) | 0 (0) | 0 | 3 (0.9) | 2 (3.4) | 66.6 |
| Acetabulum | 7 (0.9) | 1 (0.6) | 14.3 | 6 (0.8) | 1 (0.7) | 16.7 | 3 (0.9) | 0 (0) | 0 |
| Finger | 75 (9.6) | 1 (0.6) | 1.3 | 88 (11.3) | 2 (1.4) | 2.3 | 36 (11.3) | 3 (5.2) | 8.3 |
| Metacarpal*x | 36 (4.6) | 0 (0) | 0 | 27 (3.5) | 5 (3.4) | 18.5 | 32 (10) | 3 (5.2) | 9.4 |
| Carpal | 18 (2.3) | 7 (4.5) | 38.9 | 29 (3.7) | 3 (2.1) | 10.3 | 4 (1.3) | 0 (0) | 0 |
| Distal radius-ulna | 141 (18) | 7 (4.5) | 4.9 | 122 (15.6) | 9 (6.2) | 7.4 | 54 (16.9) | 4 (6.9) | 7.4 |
| Radius-ulna shaft | 10 (1.3) | 9 (5.7) | 90 | 12 (1.5) | 10 (6.9) | 83.3 | 2 (0.6) | 0 (0) | 0 |
| Proximal radius-ulna | 17 (2.2) | 2 (1.3) | 11.8 | 12 (1.5) | 2 (1.4) | 16.7 | 4 (1.3) | 3 (5.2) | 75 |
| Distal humerus | 18 (2.3) | 12 (7.6) | 66.6 | 13 (1.7) | 5 (3.4) | 38.5 | 6 (1.9) | 1 (1.7) | 16.7 |
| Humerus shaft | 15 (1.9) | 1 (0.6) | 6.7 | 14 (1.8) | 3 (2.1) | 21.4 | 5 (1.6) | 0 (0) | 0 |
| Proximal humerus | 41 (5.2) | 6 (3.8) | 14.6 | 50 (6.4) | 4 (2.8) | 8 | 14 (4.4) | 0 (0) | 0 |
| Clavicle | 29 (3.7) | 0 (0) | 0 | 23 (2.9) | 1 (0.7) | 4.3 | 6 (1.9) | 0 (0) | 0 |
| Scapula | 4 (0.5) | 0 | 0 | 3 (0.4) | 0 | 0 | 1 (0.3) | 0 | 0 |
| Total | 783 (100) | 157 (100) | 20.1a | 780 (100) | 145 (100) | 18.6b | 320 (100) | 58 (100) | 18.1c |
statistically significantly different in the pandemic period in terms of proportional fracture frequency
statistically significantly different in the pandemic period in terms of proportional surgical treatment p=0,67 for the comparison of a, b, and c
The rate of operations for the fractures in group 1 were 6.8%, 7.7%, and 14.6% in 2018, 2019, and 2020 periods, respectively (p<0.001) (Table 4a). For group 2, these rates were 20.1%, 18.6%, and 18.1%, respectively (p=0.67) (Table 4b). The fractures that needed surgery were most commonly located in the distal humerus (most of them were supracondylar humerus fractures in pediatric patients) and proximal femur (most of them in the femoral neck) in all three periods (Tables 4.a, b). When the times to operation and hospitalization times for these two most commonly operated locations were evaluated, the shortest time was observed in the pandemic period (Table 5). Time to operation was shorter in the pandemic period; however, there was no statistically significant difference for both localizations (p values of 0.26 and 0.72, respectively). Hospitalization time was statistically significantly shorter in the pandemic period for both fracture localizations (p values of 0.001 and 0.017, respectively) (Table 5). There were 48, 29, and 26 open fractures in 2018, 2019, and 2020 periods, respectively. The rate of open fractures was apparently higher in male patients (87.5%, 79.3%, and 88.4%, respectively). There was not a statistically significant difference between the periods in terms of open fracture rates (p=0.066). The most common location of open fractures was fingers for all three periods (43.8%, 44.8%, and 50%, respectively). The second common location was tibia shaft (Table 6).
Table 5.
Comparison of time to operation and hospitalization times of patients who were treated surgically for distal humerus and proximal femur fractures
| Distal humerus fractures time to operation (days) (mean±SD) (min–max) | Distal humerus fractures hospitalization time (days) (mean±SD) (min–max) | Proximal femur fractures time to operation (days) (mean±SD) (min–max) | Proximal femur fractures hospitalization time (days) (mean±SD) (min–max) | |
|---|---|---|---|---|
| 2018 | 0.41±0.77 (0.13–5) | 2.66±1.8 (1–12) | 3.7±2.8 (0.13–10) | 8.5±5.9 (1–28) |
| 2019 | 0.38±0.65 (0.13–3) | 2.85±1.6 (1–7) | 2.9±2.6 (0.13–8) | 7.2±3.8 (1–16) |
| 2020 | 0.22±0.1 (0.13–0.38) | 1.55±0.5 (1–2) | 1.7±1.1 (0.33–4) | 4.5±2.1 (2–8) |
| p valuea | 0.26 | 0.001 | 0.07 | 0.017 |
SD: standard deviation; min: minimum; max: maximum
Kruskal-Wallis test
Table 6.
Open fractures; localizations, mean age and genders of the patients
| 2018 (16 March to 22 May) [(n, mean±SD), (min–max), (gender)] | 2019 (16 March to 22 May) [(n, mean±SD), (min–max), (gender)] | 2020 (16 March to 22 May) [(n, mean±SD), (min–max), (gender)] | |
|---|---|---|---|
| Hand finger | n:21, 18.8±16.2 (3–46), (5F-16M) | n:13 (29.3±19.9 (2–58), (5F-8M) | n:13, 36±21.3 (6–74), (2F-11M) |
| Metacarpal | n:3, 51.3±32.3 (3M) | 0 | n:1, 45, (M) |
| Forearm | 0 | 1, 47, (M) | 1, 30, (M) |
| Humerus | 0 | 0 | 1, 30, (M) |
| Foot finger | n:2, 13±16.9 (1–25), (2M) | n:3, 32.7±3.5 (29–36), (3M) | n:2, 9.5±7.7 (4–15), (2M) |
| Talus | n:1, 13, (M) | 0 | 0 |
| Metatarsal | n:3, 34.7±30.5 (5–66), (3M) | 0 | n:2, 23.5±0.7 (23–34), (2M) |
| Distal tibia | n:6, 25.6±17 (6–56), (6M) | n:3, 39±24.5 (18–66), (3M) | 0 |
| Tibia shaft | n:9, 33.8±21.1 (3–59), (9M) | n:8, 29.8±15.9 (8–50), (1F-7M) | n:4, 38±15.8 (19–56), (1F- 3M) |
| Proximal tibia | n:1, 60, (M) | n:1, 26, (M) | n:1, 26, (M) |
| Femur | n:2, 24±11.3 (16–32), (1F- 1M) | 0 | n:1, 41, (M) |
| Total (p:0.19) | n:48, 26.2±20.7 (1–77), (6F- 42M) | n:29, 31.3±17.2 (2–66), (6F-23M) | n:26, 33± 17.9 (4–74), (3F-23M) |
SD: standard deviation; min: minimum; max: maximum; F: female; M: male
There were 4, 3, and 3 multi-traumatized patients in need of treatment in the intensive care unit in 2018, 2019, and 2020 periods, respectively. Corona virus infection was never encountered in any patient and healthcare team member who was treated and treated for fracture in the pandemic process.
Discussion
During the COVID 19 pandemic period, there were changes in the field of health, as in many areas of life, on both employee and patient fronts. The practice of orthopedics was also very affected by the pandemic (6–9). As a result of decreased human mobility outside the home in order to prevent the spread of the virus, it should not be surprising to predict a decrease in trauma cases. This study aimed to analyze this idea with data. The most important findings of this study were the frequency of fractures in the pandemic period decreased to approximately one-third of the pre-pandemic period’s rates while the most common fracture localizations remained the same. It was found that the number of operations performed except for the fracture etiology decreased significantly. Hospitalization times were found to be decreased significantly, both for distal humeral and proximal femoral fractures.
Currently, there is only one study which evaluates and compares the fracture rates during the COVID 19 pandemic and non-pandemic periods in the previous years (6). Bram et al. concluded that the pediatric fracture volume had decreased 2.5-fold during the COVID 19 pandemic (6). The authors evaluated the new pediatric fractures that were admitted between March 15 and April 15 of years 2018, 2019, and 2020. The authors accepted the period of year 2020 as “pandemic’’ and years 2018 and 2019 together as a single group of “pre-pandemic’’ period. In the current study, the data of 2018 and 2019 were included, considering that comparing the data of a single pandemic year with the data of the pandemic year would be insufficient. Our data showed that in the pandemic period, the frequency of the fracture decreased to approximately one third of the non-pandemic periods, similar to that in the study by Bram et al. Another similar finding was that the mean age of the pediatric patients with a fracture was found to be decreased probably due to the closing of the schools and restrictions about going out to the streets and a resulting decrease in sports activity, especially contact sports which are directly related with adolescent fractures (6, 10–14). In both studies, it was found that there was no change in gender distribution, and fractures were mostly observed in boys during the pandemic. Rates of open fractures were found to be unchanged during the pandemic in the study by Bram et al. (6). Although it did not increase statistically significantly, a proportional increase in open fractures was observed during the pandemic period in our study group. In the pandemic period, the fact that the surrounding hospitals limited patient acceptance and the fractures requiring intervention were directed to our hospital may have caused this increase. In contrast to the study results by Bram et al., the rate of surgically treated fractures was found to be increased in our study group. Our hospital, which is already a reference center for pediatric and adult fractures, has become more important for the fractures requiring surgery during the pandemic, which may have contributed to the increased surgery rates. In this study, the time interval in which fractures were evaluated was longer compared with that in the study by Bram et al. (6). This can be considered an advantage of our study as more precise information about fracture numbers could be obtained in a wider time in the ongoing pandemic process. Furthermore, the fractures of the adult population were also evaluated. The strength of the study by Bram et al. is that the epidemiology of the fractures was evaluated in detail.
Although our hospital is a center where patients are extensively referred during the pandemic period, the number of fractures decreased significantly. This situation is probably due to the decrease in mobility in the streets. The areas where fractures were most common in pediatric patients in our study population were the wrist and elbow circumference both before and during the pandemic period. The frequency of distal radius fractures in the pediatric age group has been previously reported in many studies (13,14). Finger and clavicle fractures were reported to be second most frequent sites of pediatric fractures (13, 14). However, in our study it was observed that the distal humerus was the second most common location for pediatric fractures. The reason of the increased number of pediatric distal humerus fractures admitted to our hospital, both before and during the pandemic period, is probably that our center works like a pediatric trauma center, and pediatric trauma treatments in our region are performed mostly in our center. There was a statistically significant proportional increase in the pediatric femoral and tibial shaft fractures in the pandemic period, again probably due to the increased referrals from surrounding hospitals. The fracture frequency in the hand, foot, and wrist areas in adult patients was consistent with the literature data (5, 15). Proportion of toe, metacarpal, and tibial shaft fractures was found to be increased statistically significantly in the adult population. The reason for the increase of toe and metacarpal fractures may be due to increased home accidents, and the proportional increase of tibial shaft fractures may be due to referrals from surrounding hospitals. Since patients over 65 years of age had to stay at home in our country, fractures of the hip and pelvic ring (pubic ramus), which could occur at home in those with low energy, would be expected to increase proportionally, but this did not observed (16, 17).
In the pandemic period, it was observed that the operations performed for the fracture increased proportionally, the reason for this was that all elective surgeries were postponed. In the pediatric age group, the rate of operation of the fractures encountered during the pandemic period was twice as compared with that of other years. The reason for this could be that the families did not want to go to the hospital for minor injuries because they were afraid that their children would probably be exposed to COVID 19 infection. Additionally, the increased referrals for pediatric fracture surgery from other hospitals can be another reason for this.
Although it was not statistically significant, the time to operation of hip fractures and distal humerus fractures was found to be decreased. The reason for this situation is that the patient crowd of the central operating room decreased due to the high possibility of delaying elective surgeries. The hospitalization times of both distal humerus and hip fractures were significantly reduced. This may be due to the shortening of the time to surgeries and the patient and the treating physician to be concerned that the risk of transmission of COVID infection will increase with prolonged hospital stay.
This study has several limitations. Designing the study retrospectively is an important limitation. The use of ICD 10 codes while investigating patients from the archive may cause some fractures not to be detected due to incorrect coding, which is another very important limitation.
In conclusion, we observed that the frequency of fractures decreased by approximately one third during the pandemic period compared with non-pandemic periods. The mean age of the patients in the pediatric group was found to have decreased probably due to the closure of schools and reduced mobility on the play grounds which resulted in decreased adolescent fracture rates. The hospitalization time for frequently seen distal humerus and hip fractures was decreased significantly. Distribution of fractures in terms of gender did not change during the pandemic period. It can be concluded that the decreased mobility on streets directly affects the fracture frequency. In this study, only patients who applied to one large center were examined. Analysis of more centers’ data can yield more general results.
HIGHLIGHTS.
The frequency of fractures decreased by approximately one third during the pandemic period compared with non-pandemic periods.
The mean age of the patients in the pediatric group was found to be decreased probably due to the closure of schools and reduced mobility on the playgrounds which resulted in decreased adolescent fracture rates.
The decreased mobility on the streets directly affects the fracture frequency.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Committee of Tepecik Training and Research Hospital (number: 2020/6-12, date:13/05/2020).
Informed Consent: N/A.
Author Contributions: Concept - A.T.; Design - A.T., H.A.; Supervision - A.T., Ö.K.; Materials - A.T., H.A., Ü.A., S.H., E.E., Ö.K.; Data Collection and/or Processing - A.T., H.A., Ü.A., S.H., E.E.; Analysis and/or Interpretation - A.T., Ö.K.; Literature Search - A.T., H.A., S.H., E.E.; Writing Manuscript - A.T.; Critical Review - A.T., Ö.K.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Özdin S, Özdin ŞB. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020 doi: 10.1177/0020764020927051. doi: 10.1177/0020764020927051. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neher RA, Dyrdak R, Druelle V, Hodcroft EB, Albert J. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med Wkly. 2020 doi: 10.4414/smw.2020.20224. https://doi.org/10.4414/smw.2020.20224. https://doi.org/10.4414/smw.2020.20224. [DOI] [PubMed] [Google Scholar]
- 3.Nussbaumer-Streit B, Mayr V, Dobrescu AL, et al. Quarantine alone or in combination with other public health measures to control COVID-19: A rapid review. Cochrane Database Syst Rev. 2020;4:CD013574. doi: 10.1002/14651858.CD013574. doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6:79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006;37:691–7. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 6.Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020 doi: 10.1097/BPO.0000000000001600. doi: 10.1097/BPO.0000000000001600. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 7.Wong JS, Cheung KM. Orthopaedic surgeons and orthopaedic surgery in the era of COVID-19. Acta Orthop Traumatol Turc. 2020;54:221–2. doi: 10.5152/j.aott.2020.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cakmak G, Ceyhan E, Demirtas Y, Berk H. The management of orthopedics and traumatology patients during SARS-CoV-2 pandemic. Acta Orthop Traumatol Turc. 2020;54:223–7. doi: 10.5152/j.aott.2020.20166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ozturk K, Unkar EA, Ozturk AA. Perioperative management recommendations to resume elective orthopaedic surgeries for post-COVID-19 “new normal”: Current vision of the Turkish Society of Orthopaedics and Traumatology. Acta Orthop Traumatol Turc. 2020;54:228–33. doi: 10.5152/j.aott.2020.20183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ergun M, Denerel HN, Binnet MS, Ertat KA. Injuries in elite youth football players: A prospective three-year study. Acta Orthop Traumatol Turc. 2013;47:339–46. doi: 10.3944/AOTT.2013.3177. [DOI] [PubMed] [Google Scholar]
- 11.Bombaci H, Ulku K, Adiyeke L, Kara S, Gorgec M. Childhood injuries, their etiologies, and preventive measures. Acta Orthop Traumatol Turc. 2008;42:166–73. doi: 10.3944/AOTT.2008.166. [DOI] [PubMed] [Google Scholar]
- 12.Ergen E. Sports injuries in children and adolescents: etiology, epidemiology, and risk factors. Acta Orthop Traumatol Turc. 2004;38(Suppl 1):27–31. [PubMed] [Google Scholar]
- 13.Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38:913–22. doi: 10.1016/j.injury.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 14.Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81:148–53. doi: 10.3109/17453671003628780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singer BR, McLauchlan GJ, Robinson CM, Christie J. Epidemiology of fractures in 15 000 adults: the influence of age and gender. J Bone Joint Surg Br. 1998;80:243–8. doi: 10.1302/0301-620X.80B2.0800243. [DOI] [PubMed] [Google Scholar]
- 16.Turgut A, Kalenderer O, Akan I, Ilyas G, Kumbaracı M, Karapinar L. Do patients with acute isolated pubic ramus fractures have to be hospitalized? Acta Orthop Belg. 2017;83:574–80. [PubMed] [Google Scholar]
- 17.Krappinger D, Kammerlander C, Hak DJ, Blauth M. Low-energy osteoporotic pelvic fractures. Arch Orthop Trauma Surg. 2010;130:1167–75. doi: 10.1007/s00402-010-1108-1. [DOI] [PubMed] [Google Scholar]


