Abstract
Coronavirus disease-2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and represents a potentially fatal disease. COVID-19 is associated with a hypercoagulable state leading to increased incidence of venous thromboembolism. Arterial thrombosis has been reported, but the prevalence is not known. Herein, we report an unusual presentation of a 77-year-old male who presented with dyspnea and pain in left leg and was found to have acute limb ischemia. Our case adds to the limited literature regarding arterial thrombosis in COVID-19.
Keywords: covid-19, acute limb ischemia, arterial thrombosis, thrombosis, sars-cov-2 (severe acute respiratory syndrome coronavirus 2
Introduction
At the end of 2019, a novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China. On March 11, 2020, WHO declared coronavirus disease 2019 (COVID-19) as pandemic [1]. Droplets and contact are the main means of transmission [2]. Patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection mainly present with upper and lower respiratory tract symptoms, with complications related to cytokine storm syndrome and acute respiratory distress syndrome (ARDS) [3]. We report an unusual presentation of a 77-year-old male who presented with dyspnea and pain, swelling in the left leg, and was found to have acute limb ischemia (ALI).
Case presentation
A 77-year-old male patient presented to emergency department with complaints of shortness of breath and pain, discoloration, and swelling of the left leg. Vital signs on presentation were heart rate 110 per minute, blood pressure 155/85 mmHg, oxygen saturation 96% on room air, and temperature 36 degree Celsius. The patient had bilateral crackles on lung exam and absent left dorsalis pedis and posterior tibial pulses and foot was swollen, discolored, and cold. Electrocardiogram showed sinus tachycardia 110 per minute.
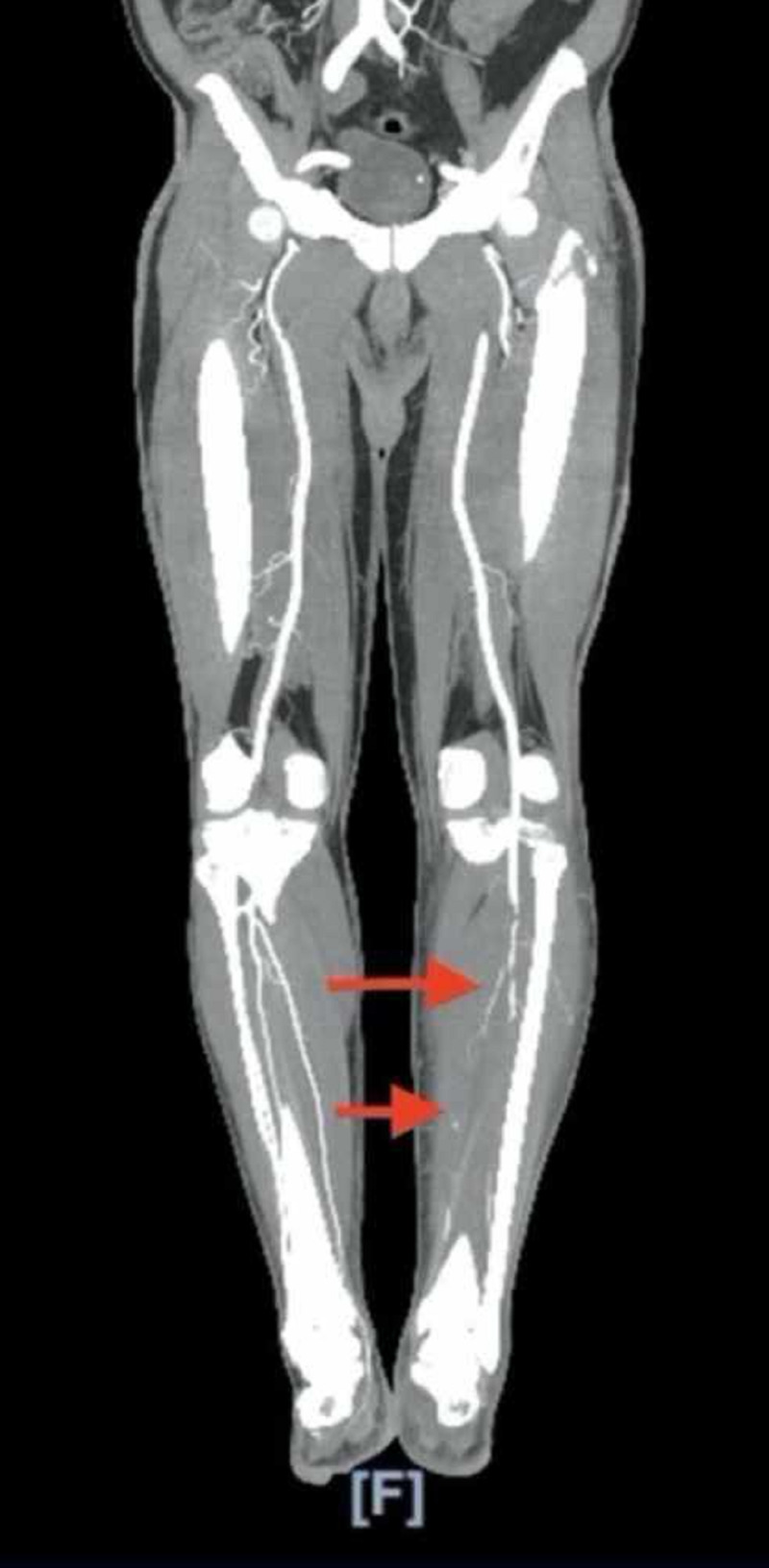
On initial laboratory evaluation, the following values were noted: hemoglobin 12.1 g/dl (reference: 12-16 g/dl), hematocrit 38.2% (reference: 36%-46%), white blood cells 41 K/mm3 (reference: 4.5-11 K/mm3), platelets 534 K/mm3 (reference: 140-440 K/mm3), potassium 4.1 meq/L (reference: 3.5-5 meq/L), glucose 126 mg/dl (reference: 70-105 mg/dl), creatinine 0.61 mg/dl (reference: 0.6-1.30 mg/dl), blood urea nitrogen 8 mg/dl (reference: 7-23 mg/dl), lactic acid 1.1 mmol/L (reference: 0.5-2.2 mmol/L), troponin 0.136 ng/ml (reference: less than 0.03 ng/ml), D-dimer 2.77 (reference: less than 0.5), prothrombin time 14.8 seconds (reference: 12.2-14.9 seconds), international normalized ratio (INR) 1.2 (reference: less than 1), partial thromboplastin time 39.8 seconds (reference: 21.3-35.1 seconds), lactate dehydrogenase (LDH) 392 U/L (reference: 140-271 U/L), C-reactive protein (CRP) 301 mg/L (reference: less than 10 mg/L), ferritin 1,396 ng/mL (reference: 12-300 ng/ml), procalcitonin 0.60 ng/ml (reference: less than 2 ng/ml), aspartate transaminase 134 U/L (reference: 13-39 U/L), calcium 8.5 mg/dl (reference: 8.6-10.3 mg/dl), and albumin 2.7 mg/dl (reference: 3.5-5.0 mg/dl). Chest X ray showed bilateral hazy infiltrates. CT angiography of the abdomen and aorta with Iliofemoral runoff showed thrombus within the mid left superficial femoral artery and occluded left anterior tibial artery, left posterior tibial artery, and left peroneal artery with no flow to the foot (Figure 1).
Figure 1. CT angiography of aorta with iliofemoral runoff showing occluded left anterior tibial artery and left peroneal artery.
Covid-19 was diagnosed on the basis of reverse transcription polymerase chain reaction (RT-PCR) testing. Echocardiogram showed an ejection fraction of 60%. The patient was placed on air-borne precautions and was started on ceftriaxone, azithromycin, hydroxychloroquine, and therapeutic anticoagulation with heparin. He underwent thrombectomy of left common femoral artery, profunda femoris, superficial femoral artery, popliteal artery, anterior tibial artery, posterior tibial artery, and peroneal artery.
Discussion
The clinical spectrum of COVID19 continues to evolve. The most common symptoms being reported are fever, myalgia, cough, and dyspnea, and less frequently headache, diarrhea, nausea, and vomiting [4]. Severity of infection could be varied from asymptomatic infection to critical disease. Smell and taste disorders (e.g., anosmia and dysgeusia) have also been reported as common symptoms in patients with COVID-19 [5]. Although in COVID-19 respiratory symptoms predominate, thrombosis can occur with COVID-19 [6]. Among patients with advanced age and medical comorbidities (cardiovascular disease, diabetes mellitus, hypertension, chronic lung disease, cancer, chronic kidney disease, obesity, and smoking), COVID-19 is frequently severe [7].
Patients with severe COVID-19 infection can develop a disseminated coagulopathy characterized by increases in procoagulant factors like fibrinogen and D-dimer leading to widespread microvascular thrombosis. This state has been termed thromboinflammation or COVID-19-associated coagulopathy [8]. Bellosta et al. evaluated 20 patients with ALI who were positive for COVID-19 and concluded that revascularization was lower than expected, which was hypothesized was due to a virus-related hypercoagulable state; however, the use of prolonged systemic heparin may improve surgical treatment efficacy as well as improve limb salvage and overall mortality [9]. Zhang et al. reported three COVID- 19 patients with cerebral infarcts. One of the patients had thrombosis in the bilateral lower limbs as well as in digits 2 and 3 of the left hand. In all the three cases, serologic tests were positive for anticardiolipin IgA antibodies as well as anti-β2-glycoprotein IgA and IgG antibodies. Lupus anticoagulant was not detected in any of the patients. These antibodies can arise transiently in patients with critical illness and various infections [10]. In our patient, antiphospholipid antibody testing was not done.
All hospitalized patients with COVID-19 should receive pharmacologic thromboprophylaxis with low molecular weight heparin (LMWH) or fondaparinux unless bleeding risk and full therapeutic-intensity anticoagulation in the appropriate clinical scenario [11]. Anticoagulant therapy mainly with LMWH appears to be associated with better prognosis in severe COVID-19 patients meeting sepsis-induced coagulopathy criteria or with markedly elevated D-dimer [12].
Conclusions
We report an unusual presentation of a 77-year-old male patient who presented with dyspnea and acute pain in left leg and was found to have ALI and underwent thrombectomy. Our case and review of literature reveals that health care providers should be aware of this unusual life-threatening manifestation of COVID 19 so that appropriate measures can be taken for the vascular emergency.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.The COVID-19 epidemic. Velavan TP, Meyer CG. Trop Med Int Health. 2020;25:278–280. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Jin Y-H, Cai L, Cheng Z-S, et al.; Zhongnan Hospital of Wuhan University Novel Coronavirus Management and Research Team, Evidence-Based Medicine Chapter of China International Exchange and Promotive Association for Medical and Health Care (CPAM) Mil Med Res. 2020;7:4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.COVID- 19: what has been learned and to be learned about the novel coronavirus disease. Yi Y, Lagniton PNP, Ye S, Li E, Xu R-H. Int J Biol Sci. 2020;16:1753–1766. doi: 10.7150/ijbs.45134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clinical characteristics of coronavirus disease 2019 in China. Guan WJ, Ni ZY, Hu Y, et al. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID- 19) a multicenter European study. Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Eur Arch Otorhinolaryngol. 2020;277:2251–2261. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.COVID-19 presenting as acute limb ischaemia. Kaur P, Posimreddy S, Singh B, Qaqa F, Habib HA, Maroules M, Shamoon F. Eur J Case Rep Intern Med. 2020;7:1724. doi: 10.12890/2020_001724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. Driggin E, Madhavan MV, Bikdeli B, et al. J Am Coll Cardiol. 2020;75:2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thromboinflammation and the hypercoagulability of COVID-19. Connors JM, Levy JH. J Thromb Haemost. 2020;18:1559–1561. doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acute limb ischemia in patients with COVID-19 pneumonia [Epub ahead of print] Bellosta R, Luzzani L, Natalini G, et al. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coagulopathy and antiphospholipid antibodies in patients with Covid-19. Zhang Y, Xiao M, Zhang S, et al. N Engl J Med. 2020;382:0. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. Paranjpe I, Fuster V, Lala A, et al. J Am Coll Cardiol. 2020;76:122–124. doi: 10.1016/j.jacc.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. J Thromb Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]