Abstract
The pandemic spread of corona virus disease 2019 (COVID-19) has become a global threat. No cure is available for this condition till date. Ayurveda, may come to rescue in these times of COVID-19 spread. In this review we have analyzed that the COVID-19 has analogy with the Rajayakshma (∼a wasting disease indicating suboptimum immune response) and the established treatment of Rajayakshma disease can be proposed for preventive as well as curative purpose.
Keywords: Ayurveda, COVID-19, Rajayakshma
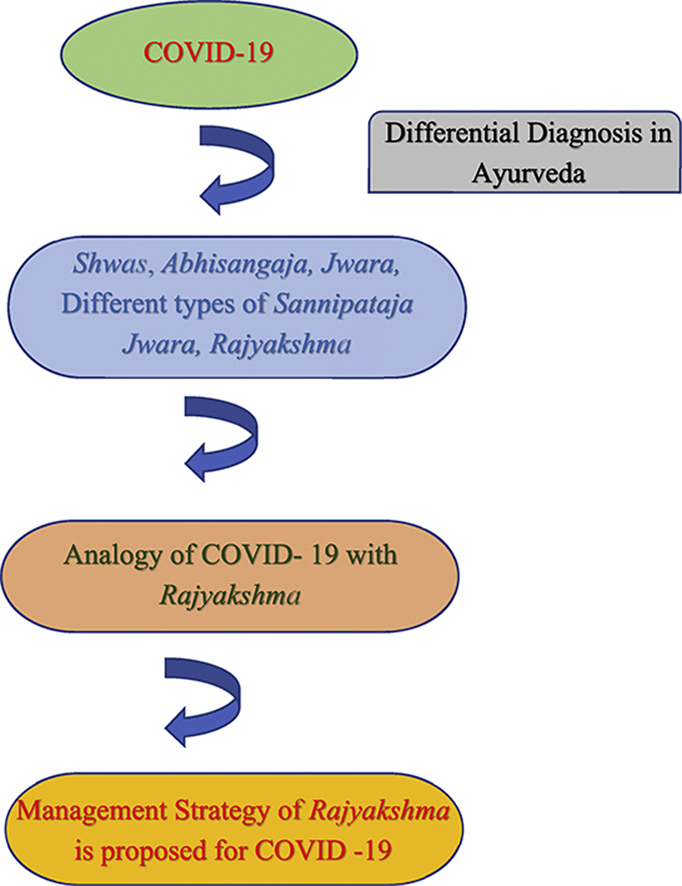
Graphical abstract
1. Introduction
Corona virus disease (COVID-19) is caused by 2019 novel coronavirus (2019-nCoV). The genome of this 2019-nCoV partially resembled severe acute respiratory syndrome-like corona virus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) MERS-CoV, which had global outbreak in the latter half of year 2019 [1]. The COVID-19 causative is closely related with the SARS-COV [2]. It is established that the spread of the disease in human is through direct contact via droplets and touching the contaminated surface before touching the eyes, nose and mouth [3]. The incubation period of the disease is between 3 and 14 days. It is observed that elderly patients and patients with co morbidities like diabetes, cardiovascular conditions, chronic respiratory diseases, malignancy, chronic kidney diseases, immune compromised patients and patients undergoing chemotherapy or radiotherapy are more prone to fatality. Symptom of the disease is flu like (lower respiratory illness) or the infected patients may remain asymptomatic also. Most of the patients (around 81%) observe mild symptoms as dry cough, fever, fatigue, sputum production, shortness of breath, muscle or joint pain, headache, diarrhea, nausea or vomiting, nasal congestion, sore throat, loss of smell and abdominal pain. In moderately affected patients, around 14% cases show symptoms of moderate pneumonia, cough and shortness of breath. In severely affected patients, around 5% exhibits severe pneumonia, dyspnea, respiratory distress, tachypnea, hypoxia and fever. Critical patients may develop Acute Respiratory Distress Syndrome, Sepsis and Septic Shock resulting in multi organ failure [4]. Presently the symptomatic management, oxygen therapy, mechanical ventilation, hemodynamic supports are used for COVID-19 patients. Even the scope of plasma therapy is being explored in the cases of COVID-19 [5]. Presently we must aim for a practical and feasible therapeutic regime for management of disease for large populations. In this review the analogy of the COVID-19 disease with the Rajayakshma (∼a wasting disease indicating suboptimum immune response) is analyzed and the use of various therapeutic measures prescribed in the Rajayakshma Chikitsa (treatment) for COVID-19 patients are discussed.
2. Differential diagnosis
Regarding differential diagnosis COVID-19 in Ayurveda, the disease have similarity with Shwasa (dyspnea), Abhisangaja Jwara (fever of infectious origin), different type of Sannipataja Jwara (∼Tridoshaja fever) and Rajayakshma. Here only some type of Jwara (fever) and Rajayakshma diseases are contagious in nature like COVID-19 [6]. All the symptoms and concerns for COVID-19 are also addressed in Rajayakshma. Furthermore treatment strategies of all these diseases are also adoptable in the management of Rajayakshma. Hence there is analogy between COVID-19 and Rajayakshma.
3. Analogy of COVID 19 with Rajayakshma
There is lot of similarity in COVID-19 and Rajayakshma disease. Rajayakshma disease is Tridoshaja and the epidemiology and pathogenesis of COVID-19 suggests it as Tridoshaja [7]. In Rajayakshma, spread is like Kustha (contagious disease), with Agantu Anubandhtvat (the causative factor is acquired from outside not resultant of the body’s metabolisms) and Naanurakshataha (by getting exposed to the causative) this is also true for COVID-19. [7, Chapter 8/4] Patient gets affected due to Sharira Sneha Ksheenta (loss of unctuousness), Dhatukshaya (depletion of tissues), Sukrakshaya (depletion of Sukra Dhatu), Ojakshaya (∼decreased vitality) and all these factors indicate the low immune response. [7, chapter 8/4 ] This factor may be somewhat true in the case of the COVID-19 as the immune response is the main key factor that contributes to the prognosis of the disease. There are two sets of symptoms described in the Rajayakshma first is the Shadrupa (six symptoms). [7, chapter 8/46–47] It includes Kasa (cough), Jwara (Fever), Parshva Shoola (pain in lateral), Swarabheda (hoarseness of voice), Atisaara (diarrhea), and Aruchi (loss of appetite). These symptoms are majorly present in most of the affected individuals and if the patients have Mamsa Bala Kshaya (weight and strength loss) then the disease can prove fatal. [7, chapter 8/47] The same is true for viral disease also in which such type of loss cause depletion of natural killer cells, cytotoxic T-cells and helper T-cells which make individual more prone to infection [8].The second set of the symptoms are the Ekadasharupa (eleven symptoms). [7, chapter 8/45–46] These symptoms are observed in some patients and their severity also depends upon the individual’s own response. These symptoms include Shirahashoola (headache), Jwara (Fever), Pratishyaya (cold), Praseka (running of nose, mouth, nausea), Kanthaudhvansa (sore throat), Kasa (cough), Swarabheda (hoarseness of voice) or Swarakshay (laryngitis), Parshva Shoola (pain in lateral), Shwasa (dyspnea), Urahashoola (Pain in chest) or Urahakshata (damage in lung tissues) or Raktavamana (hemoptysis), Jrimbha (indicating fatigue) or Ansavamardana (malaise in scapular region), or Angamardana (generalized malaise) or Ansasantapa (weakness or fatigue in scapular region), Aruchi (loss of appetite), Muhur – Muhur Chardi (repetitive vomiting) or Vaman (vomiting), Atisara (diarrhea) or Trilakshan Varchabheda (severe diarrhea). All of these symptoms described in Shadarupa and Ekadasharupa are observed in patients of COVID-19 [9,10]. Thus there is close resemblance between the clinical presentation of COVID-19 and Rajayakshma [9,10] (Table 1).
Table-1.
| Sno. | Variables | Rajayakshma | COVID 19 |
|---|---|---|---|
| 1. | Shirahashoola (headache) | + | Headache present in 14.0%, Dizziness (Indriya Vibhram) present in 7.6% |
| 2 | Jwara (Fever) | + | Present in 83.3% |
| 3 | Pratishayaya (cold) | + | Rhinorrhea present in 3.5%, nasal congestion present in 1.8%, Chills present in 15% |
| 4 | Kanthaudvansa (sore throat) | + | Present in 12.3% |
| 5 | Kasa (cough), Swarabheda (hoarseness of voice), Swarakshaya (laryngitis) | + | Cough present in 60.3% (increased sputum production – 26.9%) |
| 6 | Shwasa (dyspnea) | + | Present in 24.9% (shortness of breath) |
| 7 | Parshwa Shoola (pain in lateral),Urahashoola (Pain in chest) | + | Chest pain present in 14.9% |
| 8 | Urahaskshata (damage in lung tissues) | + | Ground-glass opacities present in 80%, Bilateral pneumonia present in 73.2% Acute respiratory distress syndrome present in 15.7% |
| 9 | Raktavamana (hemoptysis) | + | Present in 2.0% |
| 10 | Jrimbha (indicating fatigue) | + | Present in 38.0% |
| 11 | Ansavmardana (malaise in scapular region), Angamardana (generalized malaise), Ansasantapa (weakness or fatigue in scapular region) | Myalgia present in 28.5% | |
| 12 | Aruchi (loss of taste, appetite) | + | Presence of acute smell and taste dysfunction. Lack of appetite present in 78%, abdominal pain in 1.9% |
| 13 | Praseka (nausea), Muhur – Muhur Chardi (repetitive vomiting), Vamana (vomiting) | + | Nausea and vomiting present in 3.6% |
| 14 | Atisara (diarrhea), Trilakshana Varchabheda (severe diarrhea) | + | Present in 8.4% |
| 15 | No obvious symptoms | – | Present in 5.6% |
In Ayurveda pandemic are mentioned as Janpadodhvansha [11] or Maraka. [12] In these Pandemic one or more conditions like Kasa (cough), Shwasa (dyspnea), Vamathu (vomiting), Pratisyaya (Rhinorrhoea), Shiroruja (headache) and Jwara (fever) may be present. [12, chapter 6/21] In COVID-19 disease nearly all these symptoms are commonly found. Rajayakshma is considered as Roga Samuhanam (a condition with many disease or symptoms) [13]. As various new symptoms are also appearing in COVID-19 hence it can also be considered as Roga Samuhanam. Asymptomatic and mild symptomatic cases are more prevalent in COVID-19. Reason for this is also described in Rajayakshma as presence of optimum Bala, Mamsa and Rakta (strength, weight, blood etc.). If patients have all symptoms of disease even then it should be considered as suffering from less symptoms (asymptomatic and mild symptomatic). [11, chapter 3/15] This is responsible for the fast recovery in these types of patients. In some cases death resulted in COVID-19 from hypoxia due to cytokine storm in body [14]. The same situation is in Asadhyavastha (incurable condition) and death in Rajayakshma due to Urdhwashwas. [12, chapter 33/20] Among the four pattern of pathogenesis and occurrence of symptoms in Rajayakshma – Dhatukshayajanya (∼due to depletion of tissues and immunity) seems to be the most apt reason for COVID-19. Ayurveda advocate Panchakarma (five folds Ayurvedic purification therapy) and Rasayana Chikitsa [11, chapter 3/13, 14] in pandemic condition. Mridu Panchakarma of shorter durations may be beneficial for COVID-19 as in Rajayakshma. [7, chapter 8/87–88] The Achara Rasayana (behavioral therapy) is indicated in management of Janpadodhwansa [11, chapter 3/15–18] and Rajayakshma. [7, chapter 8/179–189] Thus it seems that COVID-19 is analogous with Rajayakshma.
4. Principles for the management of COVID 19 in Ayurveda
In Janpadodhvansha Panchakarma and uses of Rasayana are indicated. In Rajayakshma Mridu Panchakarma, treatment strategy of Jwara and Khataksheena is advisable. [7, chapter 8/117,183] In the treatment of Abhisangaja Jwara, Visha Chikitsa (anti-poisonous treatment) is advised. [7, chapter 3 /117–118].Thus as per the principles of Ayurveda the diet and drug formulation with Snigdha (unctuous), Sukravardhaka (∼aphrodisiac), Ojovardhaka (increasing the vitality), Jwaraghna (antipyretic), Vishanashaka (anti-poisonous), Rasayana (immune modulation), Tridoshasamyakara (balancing the harmony of body humors), Manaprasadana (psychotropic), Sarvsatmya (homologous to body) qualities and Satvaavajaya Chikitsa (behavioral therapy and psycho-somatic management) will be useful in managing the COVID-19 cases. It prescribes the use of medicated decoctions and liquids, protein based diet for rapid recovery. The main concern of COVID-19 is dyspnea (Shwasa). In this condition Mridu Swedana [7, chapter 17/83] Mridu Vamana with Lavanambu (salty water) [7, chapter 17 /85], Mridu Virechana [7, chapter 17/87], and Nasya [7, chapter 17/131] are useful and this is also according to the Rajayakshma treatment. The Swedana (heat therapy) is used for relieving painful conditions, congestion and accelerate healing (as Sankara, Nadi, Upanaha, Parisheka and Avgahana Swedana). [7, chapter 8/65] Snehana (lipid replacement therapy) is used in various form [orally after meals with milk, Nasya (nasal instillation), Abhyanga (massage), Avgahana (tub bath), Lepa (topical application of herbal paste), Udvartana (topical application of Ayurvedic powder or paste), Bastikarma (rectal administration)] as per requirement and condition of the patients. [7, chapter 8/65] If required mild forms of Bloodletting (Shringa, Jaloka and Alabu) is also employed. [7, chapter 8/82] An important aspect of Nidan Parivarjana (avoiding causative) is also employed in COVID-19 by limiting exposure [15].
5. Treatment approach of Rajayakshma for COVID-19 management
5.1. Preventive measures
It is extreme important for survival at this time to develop a body status with a good immune response for prevention and limiting severity of the disease. For this purpose the principle of daily regime, night regime and seasonal regime are to be followed. Special emphasis is to be given to healthy and nutritious diet, and immune boosting drugs should be incorporated as a part of life style in forms of various formulations like juice, lickables, decoctions, teas, tonics etc. The various examples of such immunoboosting formulations for general population are Chyawanprasha [16] Tulsi (Ocimum basilicum L.) [17], green tea [18], Ginger tea [19], Cinnamon tea [20], Turmeric milk [21] etc. Uses of Rasayana after Panchakarma procedures is also helpful.
5.2. Non infected but exposed population (quarantine)
For these types of population a bit advanced strategy is to be planned since they are exposed to the virus and may cause disease later. Thus certain medication is to be added for general protection along with the rigorous following of the preventive measures. In this condition Ojovardhaka (immunomodulation) Vishaghna (anti-toxic) and Krimighna (anti-histaminic, anti-allergic, and anti-viral) drugs are useful. Sitopaladi Churna which is an anti-allergic compound [22,23], Tulsi Patra Swarasa, [17] Guduchi Swarasa [7, chapter 8/72] or Guduchi Ghan Vati can be prescribed for immunomodulation.
5.3. Infected but asymptomatic population (quarantine)
In these types of patients precautions should be taken since the symptoms may develop few days later. Patient should take optimum rest and he should be advised for plenty of intake of plain warm water or Shadanga Paniya- ∼2 L in a day, [7, chapter 3/145–146] and Draksharista-15 to 20 mL [23, chapter 14/73-76] with equal amount of water after meals, in addition to therapeutic regime prescribed above for quarantine population.
5.4. Mild symptomatic population (non-pneumonia)
In mild symptomatic population with absence of pneumonia. There is presence of primary symptoms like dry cough, fever, body ache, sore throat, nasal congestion, headache and diarrhea. The additional medication could be prescribed for various symptoms as per individual need.
5.4.1. Fever
For the management of febrile condition the treatment guidelines for Jwara Chikitsa can be adopted as described in Rajayakshma Chikitsa. [7, chapter 8/117]
5.4.2. Body ache
In body ache water bottle fomentation or Swedana with salt may be applied to relieve the pain.
5.4.3. Sore throat
In sore throat gargling with warm salt water could ease symptom. Even the use of Yashtimadhu (Glycyrrhiza glabra L. var. Violace) or ginger (Zingiber officinale Rosc.) slice coated in rock salt can also soothe sore throat.
5.4.4. Nasal congestion
The nasal congestion can be relieved by Swedana (fomentation) and Dhuma (steam inhalation). [7, chapter 8/67] eatables made from barley are useful. Uses of mutton and chicken soup, high protein diet are recommended. [7, chapter 8/66-68] Shirahaparisheka with decoction of Bala (Sida cordifolia L.), Guduchi (Tinospora cordifolia (Willd.) Hook.F. & Thoms) and Madhuyasti can be done. [7, chapter 8/72] Nasya (nasal therapy) with Madhuyashti Ghrita is also useful. [7, chapter 8/90]
5.4.5. Headache
For headache Nasya, Dhumpana (inhalation of fume), Vasti (medicated enema), Raktavsechana (bloodletting) and various Lepa (topical application) can be done according to the need. [7, chapter 8/81–84] Dashmooladi Ghrit is useful in this condition. [7, chapter 8/93]
5.4.6. Diarrhea
Here Agnideepaka (appetizer), Atisarnashaka (anti-diarrheal) Mukhasudhikaraka (mouth refreshing) and Aruchinashaka (anti-anorexia) treatment should be adopted. Pathadi Churna, Jambvadi Churna, sour soup, sour Sthiradi Panchamool Kwatha can be prescribed. [7, chapter 8/126-133] The diarrhea can be managed with use of Yavanishadhava Churna [7, chapter 8/145–148], and Talishadi Churna [7, chapter 8/145–148].
5.4.7. Abdominal discomfort
In Abdominal discomfort, nausea and vomiting- Kaphapraseka Nashak (anti-vitiated Kapha Dosha) treatment should be done. [7, chapter 8/118-120] Talishadi Churna or Karpooradi Churna [23, chapter 14/35–36] can be used.
5.4.8. Loss of taste and loss of smell sensation
Two time tooth brushing, Kaval (medicated gargling and holding the paste or fluid in the mouth for certain time), Dhumpana (medicated fumes/smoking), and Mukhavairasya Nashaka Yoga (medication for ageusia) should be given for loss of taste. [7, chapter 8/135-140] In loss of taste Yavanisadava Churna [7, chapter 8/141–144] and Talishadi Churna [7, chapter 8/145–148] are effective. For loss of smell sensation- Pratimarsha Nasya (administration of oil based nasal drops in doses of 0.5 –1 mL), Prayogika or Snehika Dhuma Nasya (inhalation of medicated fume) may be used.
In Kasa (cough), Swarabheda (hoarseness of voice) or Swarakshaya (laryngitis), Shwasa (dyspnea),Ansavmardana (malaise in scapular region), Angamardana (generalized malaise), Ansasantapa (weakness or fatigue in scapular region) and headache- Kharjuradi Ghrita, Dashmool Ghrita, Sitopaladi Churna, Vasa Ghrita, Shatavari Ghrita, Duralabhadya Ghrita, Jivantyadi Ghrita, [7, chapter 8/96–105] Yavanisadava Churna and Talishadi Churna can be used according to the individual patient condition.
5.5. Moderate pneumonia population
In the cases of moderate pneumonia-line of management of Shwasa (respiratory disorders) may be adopted. Shati Pushakar Mool Yoga, [7, chapter 8/101] Sringarabhra Rasa, [23, chapter 14/101–110] Chandamrita Rasa [23, chapter 14/214-218] can also be added in above line of management. Regular monitoring is necessary in for prognosis of these cases.
5.6. Severe pneumonia population
In this condition Rasoushadhi (herbo-mineral compounds), preparation of Manahshila (As2O3) – an Arsenic ore, considered as Rasayana and Vishaghna (anti-toxic) [24] and preparation of gold are needed.Rasmanikya and Lakshmi Vilas Rasa which also have anti oxidative property are useful in this condition [25].These drugs are having Rasayana (immunomodulation) property. In cases of severe pneumonia the patients should be hospitalized and should be under regular monitoring. Karpooradi Churna, [23, chapter 14/35–36] Vasavleha [23, chapter 14/37–39] Lakshmi Vilas Rasa [23, chapter 14/214-218], Hemagarbha Pottali Rasa [23, chapter 14/186–188] could be prescribed for various symptoms as per individual need.
5.7. COVID-19 patient with associated comorbidities
COVID-19 patient with various comorbidities – Diabetes mellitus-2 (Madhumeha), cardiovascular complications (Hrida Roga), respiratory disorders (Shwasa Roga), chronic kidney disease (Mutrakriccha or Mutra Vikara) and immune compromised patients undergoing chemotherapy or radiotherapy (Ojo Kshaya/Bala Kshaya) needs special attention. In this condition, line of management of these specific comorbidities should also be added in COVID-19 treatment. Some medicine which are described in Rajayakshma Chikitsa are also useful in these comorbidities. Herbs used in Rajayakshma Chikitsa and having Rasayan or anti-oxidative properties may also be useful in this Vyadhishankara (comorbidities) condition. Raktachandana (Pterocarpus santalinusL.F.) [26], Bala (S. cordifolia L.), [27] Madhuyasti (G. glabra L. var. Violace), [28] Vidarikanda (Pueraria tuberosa (ROXB. EX. WILLD.) DC.), [29,30] Shigru (Moringa oleifera Lam), [31] Manjistha (Rubia cordifolia L.), [32,33] Shatavari (Asparagus racemosus WILLD.), [34] Punarnava (Boerhavia diffusa L.), [35] Pippali (Piper longum L.), [36] Dashmool [37] Kharjura (Phoenix dactylifera L.), [38] Mridwika (Vitis vinifera L.), [39,40] Shati (Hedychium spicatum BUCH.-HAM.), [41] Pushkarmoola (Inula racemosa HOOK. F.), [42] Vasa (Adhatoda vasica NEES), [43] Gokshuru (Tribulus terrestris L), [44] Arjuna (Terminalia Arjuna (ROXB.) WIGHT & ARN.), [45] Tulsi (O. basilicum L.) [17], and Aswagandha (Withania somnifera DUNAL) [46] are suitable for this purpose (Table 2). These herbs or their compound may be helpful in combating the COVID-19 and all the associated comorbidities. Sringa-Arjunadi Churna, [23, chapter 14/26] Lavangadi Churna, [23,chapter 14/23-25] Eladi Churna, [23, chapter 14/34] Kakubhadi Ksheera [23, chapter 14/12],Trayodashanga Kwatha [23, chapter 14/21], Aswagandhadi Kwatha [23, chapter 14/20] can be used in these comorbidities associated COVID-19.
Table-2.
Useful plants in COVID-19 patient with associated comorbidities.
| S.No. | Plant name | Properties |
|---|---|---|
| 1 | Raktachandana (Pterocarpus santalinusL.F.) | Anti-oxidative, anti- diabetic, antimicrobial, anticancer, and anti-inflammatory properties and protective effects on the nervous system, liver and gastric mucosa [26] |
| 2 | Bala (Sida cordifolia L.) | Has anti-diabetic, antioxidant, hepatoprotective, analgesic and antihelmintic properties [27] |
| 3 | Madhuyasti (Glycyrrhiza glabra L. var. Violace) | Effective as anticoagulant, antiviral, antioxidant, anti-inflammatory and having immunomodulation activity [28] |
| 4 | Vidarikanda (Pueraria tuberosa (ROXB. EX. WILLD.) DC.) | Useful in cardiovascular diseases and diabetic nephropathy and also is a potent antihypertensive and antioxidant [29,30] |
| 5 | Shigru (Moringa oleifera Lam) | Diuretic, anti-diabetic, antihypertensive, cholesterol lowering, antitumor, and antipyretic activities [31] |
| 6 | Manjistha (Rubia cordifolia L.) | Potent antioxidant and having cardio protective, metal chelant and anti-inflammatory properties [32,33] |
| 7 | Shatavari (Asparagus racemosus WILLD.) | Anti-carcinogenic, antioxidant, immunomodulation, antitussive and antiulcer drug [34] |
| 8 | Punarnava (Boerhavia diffusa L.), | Having immunomodulation, anticancer, anti-diabetic, anti-fibrinolysis, hepatoprotection, and diuresis properties [35] |
| 9 | Pippali (Piper longum L.) | It is a proved herbal bio enhancer and has immunomodulation, cardio protective, antioxidant, anticancer, radio protective and antiviral activities [36] |
| 10 | Dashmool(roots of ten plants) | Act as analgesic and anti-inflammatory drug and shows anti-platelet effects [37] |
| 11 | Kharjura (Phoenix dactylifera L.) | Considered as anti-diabetic, antioxidant, immunostimulant antimutagenic, anticancer, anti-inflammatory, hepatoprotective, gastro protective and nephroprotective [38] |
| 12 | Mridwika (Vitis vinifera L.), | Effective in metabolic syndrome such as hypertension, hyperlipidemia and hyperglycemia and has hepatoprotective, antioxidative, anti-inflammatory, cardio protective, neuroprotective effects and antiviral effect [39,40] |
| 13 | Shati (Hedychium spicatum BUCH.-HAM.), | Useful in asthama, bronchitis,vomitting, diarrhea and blood disorders and having antimicrobial, anti-inflammatory and anti-oxidant activities [41] |
| 14 | Pushkarmool (Inula racemosa HOOK. F.) | Cardioprotective in nature [42] |
| 15 | Vasa (Adhatoda vasica NEES) | Widely used in respiratory disorders and having antimicrobial and antioxidant properties [43] |
| 16 | Gokshuru (Tribulus terrestris L) | Has cardio protective, anti-diabetic, antioxidant, antitumor and antiurolithic properties [44] |
| 17 | Arjuna (Terminalia Arjuna (ROXB.) WIGHT & ARN.) | Can protect the cardiovascular system and also having the anti-hypertensive, antioxidant, anti-carcinogenic, anti-mutagenic and gastro-protective effect [45] |
| 18 | Aswagandha (Withania somnifera DUNAL) | Immunomodulation, anti-microbial, anti-arthritic,anti-inflammatory, anti-tumor, anti-oxidant, neuroprotective, cardio-protective, and anti-diabetic properties [46] |
5.8. Specialized dietary modifications
A viral disease causes a metabolic crisis in the body. Thus it becomes necessary to plan a diet that is rich in protein and calories to replenish the loss and maintain the physiological function of the body. The few example of the protein calorie rich diet suitable in the condition are Barley water, Barley recipes [47], warm liquid lentils recipes [48] flesh soup [49]etc. Study on chicken soup showed that is effective in viral symptomatic upper respiratory diseases. Additionally there is always a need of cleansing of the body which can decrease the toxic load of the body. The plain warm water or medicated water like Lavangajala (water processed with fruits of Syzygium aromaticum (L.) Merrill & Perry) should be used in plenty. The fruits like pomegranate (Punica granatum L.), grapes [50], dates, coconut (Cocos nucifera L.) [51] intake should be encouraged. Use of functional foods like garlic (Allium sativum L.) [52], onion (Allium cepa L.), basil, ginger, turmeric (Curcuma longa L.), black pepper (Piper nigrum L.), cardamom (Elettaria cardamomum MATON var. miniscula), cinnamon (Cinnamomum aromaticum NEES), bay leaves (Cinnamomum tamala NEES & EBERM.), curry leaves (Murraya koenigii (L.) SPR.), fennel (Foeniculum vulgare GAERTN), Rock salt etc. are also helpful. Emphasis should be given on maintenance of optimum weight. Individual should avoid complex diet (containing preservatives and unnatural compounds, empty calories). Overeating, excessive eating, fasting or experimentation with various types of diets should not be done at this stage.
5.9. Specialized Yoga intervention
Yoga can prove an additional asset in the management of COVID-19. Individual should indulge in regular physical exercises incorporating Mindful breathing and appropriate Yogic postures. In these cases only mild Yoga practices which promotes healing of the body is permissible that too for a very short time (the individual should not feel any fatigue in these efforts). Individual should prefer mindful breathing practices that promote the physical and mental wellbeing.
5.10. Behavioral modifications
The various behavioral modifications have to be adopted by in this time of crisis. One should refrain from smoking, tobacco and alcohol intake. Certain stress managing activity should be taken up like Agri-gym, gardening, reading. The individual should try to follow the biological rhythm of the body. Try to avoid going to sleeping late at night or sleeping for long hours at day time. The individual should try to have optimum sleep and wake up early. Special emphasis should be given to oral hygiene and upper respiratory tract cleaning though (brushing, tongue scrapping, gum massage, gargling with warm salt water or medicated herbs water). The individual should avoid all sorts of physical and mental and emotional stress till the complete strength is regained. The examples of the physical stress are rigorous exercise, travelling etc. Individual should refrain from excessive talking, excessive walking, being in a posture for too long time. Excessive strain on sense organs like (eyes, ears) should also be avoided. Individual should stay in moderate temperature. Exposure to excessive cold temperature (Air conditioners, intake of cold food like cold drinks, cold juices, milk shakes, ice creams should be avoided). Natural urges of defecation, flatus, urination, coughing, sneezing, yawing, sleep, hunger, thirst etc. should be respected and forceful expulsion or withholding should be avoided to maintain the body harmony. Utmost importance is given to Bahirmarjana (sanitizations, disinfection procedures like hand washing, bath with medicated water, rubbing of medicated powder on body) and uses of Madhya (alcoholic preparations) in prophylaxis of Rajayakshma [7, chapter 8/164] which is also the major prophylaxis in the COVID-19. The habit of Bahirmarjana should be adopted. Madhya and Sugandhit Dravya Dhupana (fumigation with fragrant herbs and compounds) can be used in sanitization process.
6. Discussion
COVID-19 is a very new disease with age less than a year and not much is known about it and every day something new is added about it. In these times our main focus should be to maximally utilize the time tested knowledge present at our dispose rather than experimenting with the valuable lives. This principle is also mentioned in Ayurveda in dealing with a new disease. It is stated that in emergence of new disease it is not wise to worry about the naming of the disease or search for the standard treatment instead in times of emergency the conditions of Dosha (body humors), Dhatu (∼tissues) and Mala (excretory waste products),Prakriti (individual body constitution),Adhisthan (site of disease) and Samutthan (site of body for origin of disease) are analyzed and the available standard line of treatment should be adopted accordingly.[13, Chapter18/44–46] Same approach is advocated here by using the present available knowledge about COVID-19 and analyzing it under the light of Ayurveda. In this review the COVID-19 was found analogous with Rajayakshma and an attempt was made to develop an applicable approach of management guidelines of Rajayakshma in COVID-19. In this approach various symptom present at varied stages of the COVID-19 are discussed with a rationale and formulation are also suggested appropriately as needed.
7. Conclusion
In the present state of emergency across the global time tested knowledge of Ayurveda may come to rescue in both preventing and managing the cases of the COVID-19. There is analogy between Rajayakshma and COVID-19. The management strategy of Rajayakshma which also follow the management strategy of Janpadodhvansa is useful in COVID-19. This management strategy might be helpful in managing the pandemic with the least resources and most economical way in large populations.
Sources of Funding
None declared.
Conflict of interest
None.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
Contributor Information
Sarvesh Kumar Singh, Email: sarveshksingh21@gmail.com.
Kshipra Rajoria, Email: kshiprarajoria@gmail.com.
Sanjeev Sharma, Email: profsanjeevhp@gmail.com.
References
- 1.Xie M., Chen Q. Insight into 2019 novel coronavirus — an updated interim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis. 2020;94:119–124. doi: 10.1016/j.ijid.2020.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. 2020;26(6):734–792. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu R., Cui B., Duan X., Zhang P., Zhou X., Yuan Q. Saliva: potential diagnostic value and transmission of 2019-nCoV. Int J Oral Sci. 2020;12(11) doi: 10.1038/s41368-020-0080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cascella M., Rajnik M., Cuomo A., Dulebohn Scott C., Napoli R.D. StatPearls [Internet] StatPearls Publishing; Treasure Island (FL): 2020. Features, evaluation and treatment coronavirus (COVID-19) [updated 2020 Apr 6]https://www.ncbi.nlm.nih.gov/books/NBK554776/ Available from: [PubMed] [Google Scholar]
- 5.Duan K., Liu B., Li C., Zhang H., Yu T., Qu J., et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. PNAS. 2020;117(17):9490–9496. doi: 10.1073/pnas.2004168117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shastri A., editor. Commentary Ayurveda tatva sandeepika on susruta samhita Nidan Sthan, chapter 5, verse 33. Chaukumba Sanskrit Sansthan; Varanasi: 2003. p. 251. [Google Scholar]
- 7.Gaur B.L. Rastriya Ayurveda Vdyapeeth; New Delhi: 2014. Commentator. Commentary Esana Hindi translation of Ayurvedadipika commentary of Caraka Samhita of Agnivesa. 3rd volume, Chikitsa Sthana Rajyakshama Chikitsa Adhyaya. [Google Scholar]
- 8.Thimmapuram R., Lanka S., Esswein A., Dall L. Correlation of nutrition with immune status in human immunodeficiency virus outpatients. Mo Med. 2019;116(4):336–339. [PMC free article] [PubMed] [Google Scholar]
- 9.Fu L., Wang B., Yuan T., Chen X., Ao Y., Fitzpatrick T., et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80(6):656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pan L., Mu M., Yang P., Sun Y., Wang R., Yan J., et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115(5):766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandey G., editor. Commentary vidhyotini of caraka samhita of agnivesa-1st volume, Viman Sthan Janpadodhwansiya Vimanadhyaya. Chaukumba Sanskrit Sansthan; Varanasi: 2006. [Google Scholar]
- 12.Shastri A., editor. Commentary Ayurveda Tatva Sandeepika on Susruta Samhita Sutra Sthan. Chaukumba Sanskrit Sansthan; Varanasi: 2003. [Google Scholar]
- 13.Pandey G., editor. Commentary Vidhyotini of Caraka Samhita of Agnivesa-1st volume, Sutra Sthan. Chaukumba Sanskrit Sansthan; Varanasi: 2006. [Google Scholar]
- 14.Sultan S., Sultan M. COVID-19 cytokine storm and novel truth [published online ahead of print, 2020 may 22] Med Hypotheses. 2020:109875. doi: 10.1016/j.mehy.2020.109875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tay K., Kamarul T., Lok W.Y., Li X., Wong J., Saw A. COVID-19 in Singapore and Malaysia: rising to the challenges of orthopaedic practice in an evolving pandemic. Malays Orthop J. 2020;14(2) doi: 10.5704/MOJ.2007.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma R., Martins N., Kuca K., Chaudhary A., Kabra A., Rao M.M., et al. Chyawanprash: a traditional Indian bioactive health supplement. Biomolecules. 2019;9(5):161. doi: 10.3390/biom9050161. Published 2019 Apr 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen M.M. Tulsi - ocimum sanctum: a herb for all reasons. J Ayurveda Integr Med. 2014;5(4):251–259. doi: 10.4103/0975-9476.146554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chacko S.M., Thambi P.T., Kuttan R., Nishigaki I. Beneficial effects of green tea: a literature review. Chin Med. 2010;5:13. doi: 10.1186/1749-8546-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prasad S., Tyagi A.K. Ginger and its constituents: role in prevention and treatment of gastrointestinal cancer. Gastroenterol Res Pract. 2015;2015:142979. doi: 10.1155/2015/142979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ranasinghe P., Pigera S., Premakumara G.A., Galappaththy P., Constantine G.R., Katulanda P. Medicinal properties of ’true’ cinnamon (Cinnamomum zeylanicum): a systematic review. BMC Complement Altern Med. 2013;13:275. doi: 10.1186/1472-6882-13-275. Published 2013 Oct 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hewlings S.J., Kalman D.S. Curcumin: a review of its’ effects on human health. Foods. 2017;6(10):92. doi: 10.3390/foods6100092. Published 2017 Oct 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makhija I.K., Shreedhara C.S., Ram H.N. Mast cell stabilization potential of Sitopaladi churna: an ayurvedic formulation. Pharmacognosy Res. 2013;5(4):306–308. doi: 10.4103/0974-8490.118824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mishra S. Chaukhamba Surbharati Prakashan; Varanasi: 2007. Bhaisajyaratnavali. Sidhiprada Hindi commentary. [Google Scholar]
- 24.Walker A.M., Stevens J.J., Ndebele K., Tchounwou P.B. Evaluation of arsenic trioxide potential for lung cancer treatment: Assessment of apoptotic mechanisms and oxidative damage. J Canc Sci Ther. 2016;8(1):1–9. doi: 10.4172/1948-5956.1000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaur G., Gupta V., Bansal P. Innate antioxidant activity of some traditional formulations. J Adv Pharm Technol Res. 2017;8(1):39–42. doi: 10.4103/2231-4040.197393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bulle S., Reddyvari H., Nallanchakravarthula V., Vaddi D.R. Therapeutic potential of pterocarpus santalinus L.: an update. Pharmacogn Rev. 2016;10(19):43–49. doi: 10.4103/0973-7847.176575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanth V.R., Diwan P.V. Analgesic, antiinflammatory and hypoglycaemic activities of Sida cordifolia. Phytother Res. 1999;13(1):75–77. doi: 10.1002/(SICI)1099-1573(199902)13:1<75::AID-PTR387>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 28.Sharma V., Katiyar A., Agrawal R.C. Glycyrrhiza glabra: chemistry and pharmacological activity. Sweeteners. 2017:87–100. doi: 10.1007/978-3-319-27027-2_21. [DOI] [Google Scholar]
- 29.Verma S.K., Jain V., Singh D.P. Effect of Pueraria tuberosa DC. (Indian Kudzu) on blood pressure, fibrinolysis and oxidative stress in patients with stage 1 hypertension. Pak J Biol Sci. 2012;15(15):742–747. doi: 10.3923/pjbs.2012.742.747. [DOI] [PubMed] [Google Scholar]
- 30.Shukla R., Banerjee S., Tripathi Y.B. Antioxidant and Antiapoptotic effect of aqueous extract of Pueraria tuberosa (Roxb. Ex Willd.) DC. On streptozotocin-induced diabetic nephropathy in rats. BMC Complement Altern Med. 2018;18(1):156. doi: 10.1186/s12906-018-2221-x. Published 2018 May 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Anwar F., Latif S., Ashraf M., Gilani A.H. Moringa oleifera: a food plant with multiple medicinal uses. Phytother Res. 2007;21(1):17–25. doi: 10.1002/ptr.2023. [DOI] [PubMed] [Google Scholar]
- 32.Chandrashekar B.S., Prabhakara S., Mohan T., Shabeer D., Bhandare B., Nalini M., et al. Characterization of Rubia cordifolia L. root extract and its evaluation of cardioprotective effect in Wistar rat model. Indian J Pharmacol. 2018;50(1):12–21. doi: 10.4103/ijp.IJP_418_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tripathi Y.B., Singh A.V. Role of Rubia cordifolia Linn. in radiation protection. Indian J Exp Biol. 2007;45(7):620–625. [PubMed] [Google Scholar]
- 34.Negi J.S., Singh P., Joshi G.P., Rawat M.S., Bisht V.K. Chemical constituents of Asparagus. Pharmacogn Rev. 2010 Jul;4(8):215–220. doi: 10.4103/0973-7847.70921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mishra S., Aeri V., Gaur P.K., Jachak S.M. Phytochemical, therapeutic, and ethnopharmacological overview for a traditionally important herb: boerhavia diffusa Linn. BioMed Res Int. 2014;2014:808302. doi: 10.1155/2014/808302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumar S., Kamboj J., Suman Sharma S. Overview for various aspects of the health benefits of Piper longum linn. fruit. J Acupunct Meridian Stud. 2011;4(2):134–140. doi: 10.1016/S2005-2901(11)60020-4. [DOI] [PubMed] [Google Scholar]
- 37.Parekar R.R., Bolegave S.S., Marathe P.A., Rege N.N. Experimental evaluation of analgesic, anti-inflammatory and anti-platelet potential of Dashamoola. J Ayurveda Integr Med. 2015 Jan-Mar;6(1):11–18. doi: 10.4103/0975-9476.146565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tang Z.X., Shi L.E., Aleid S.M. Date fruit: chemical composition, nutritional and medicinal values, products. J Sci Food Agric. 2013;93(10):2351–2361. doi: 10.1002/jsfa.6154. [DOI] [PubMed] [Google Scholar]
- 39.Akaberi M., Hosseinzadeh H. Grapes (Vitis vinifera) as a potential candidate for the therapy of the metabolic syndrome. Phytother Res. 2016;30(4):540–556. doi: 10.1002/ptr.5570. [DOI] [PubMed] [Google Scholar]
- 40.Nassiri-Asl M., Hosseinzadeh H. Review of the pharmacological effects of Vitis vinifera (Grape) and its bioactive compounds. Phytother Res. 2009;23(9):1197–1204. doi: 10.1002/ptr.2761. [DOI] [PubMed] [Google Scholar]
- 41.Rawat S., Jugran A.K., Bhatt I.D., Rawal R.S. Hedychium spicatum: a systematic review on traditional uses, phytochemistry, pharmacology and future prospectus. J Pharm Pharmacol. 2018;70(6):687–712. doi: 10.1111/jphp.12890. [DOI] [PubMed] [Google Scholar]
- 42.Kalachaveedu M., Raghavan D., Telapolu S., Kuruvilla S., Kedike B. Phytoestrogenic effect of Inula racemosa Hook f - a cardioprotective root drug in traditional medicine. J Ethnopharmacol. 2018;210:408–416. doi: 10.1016/j.jep.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 43.Duraipandiyan V., Al-Dhabi N.A., Balachandran C., Ignacimuthu S., Sankar C., Balakrishna K. Antimicrobial, antioxidant, and cytotoxic properties of vasicine acetate synthesized from vasicine isolated from Adhatoda vasica L. BioMed Res Int. 2015;2015:727304. doi: 10.1155/2015/727304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stefănescu R., Tero-Vescan A., Negroiu A., Aurică E., Vari C.E. A comprehensive review of the phytochemical, pharmacological, and toxicological properties of Tribulus terrestris L. Biomolecules. 2020;10(5):752. doi: 10.3390/biom10050752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Amalraj A., Gopi S. Medicinal properties of Terminalia arjuna (Roxb.) Wight & Arn.: a review. J Tradit Complement Med. 2016 Mar 20;7(1):65–78. doi: 10.1016/j.jtcme.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dar N.J., Hamid A., Ahmad M. Pharmacologic overview of Withania somnifera, the Indian Ginseng. Cell Mol Life Sci. 2015;72(23):4445–4460. doi: 10.1007/s00018-015-2012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zeng Y., Pu X., Yang J., Du J., Yang X., Li X., et al. Preventive and therapeutic role of functional ingredients of barley grass for chronic diseases in human beings. Oxid Med Cell Longev. 2018;2018:3232080. doi: 10.1155/2018/3232080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rennard B.O., Ertl R.F., Gossman G.L., Robbins R.A., Rennard S.I. Chicken soup inhibits neutrophil chemotaxis in vitro. Chest. 2000;118(4):1150–1157. doi: 10.1378/chest.118.4.1150. [DOI] [PubMed] [Google Scholar]
- 49.Su X., D’Souza D.H. Grape seed extract for control of human enteric viruses. Appl Environ Microbiol. 2011;77(12):3982–3987. doi: 10.1128/AEM.00193-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ganesan K., Xu B. Polyphenol-rich lentils and their health promoting effects. Int J Mol Sci. 2017;18(11):2390. doi: 10.3390/ijms18112390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.DebMandal M., Mandal S. Coconut (Cocos nucifera L: arecaceae): in health promotion and disease prevention. Asian Pac J Trop Med. 2011;4:241–247. doi: 10.1016/S1995-7645(11)60078-3. [DOI] [PubMed] [Google Scholar]
- 52.Shastri A., editor. Commentary Ayurveda Tatva Sandeepika on Susruta Samhita Uttar Tantra, chapter 41, verse 59. Chaukumba Sanskrit Sansthan; Varanasi: 2003. p. 25. [Google Scholar]


