Abstract
Background
National health information (HI) systems provide data on population health, the determinants of health and health system performance within countries. The evaluation of these systems has traditionally focused on statistical practices and procedures, and not on data use or reuse for policy and practice. This limits the capacity to assess the impact of HI systems on healthcare provision, management and policy-making. On the other hand, the field of Knowledge Translation (KT) has developed frameworks to guide evidence into practice.
Methods
A scoping review of the KT literature to identify the essential mechanisms and determinants of KT that could help monitor the impact of HI systems.
Results
We examined 79 publications and we identified over 100 different KT frameworks but none of these were focused on HI systems per se. There were specific recommendations on disseminating evidence to stakeholders at the institutional and organizational level, and on sustaining the use of evidence in practice and the broader community setting.
Conclusions
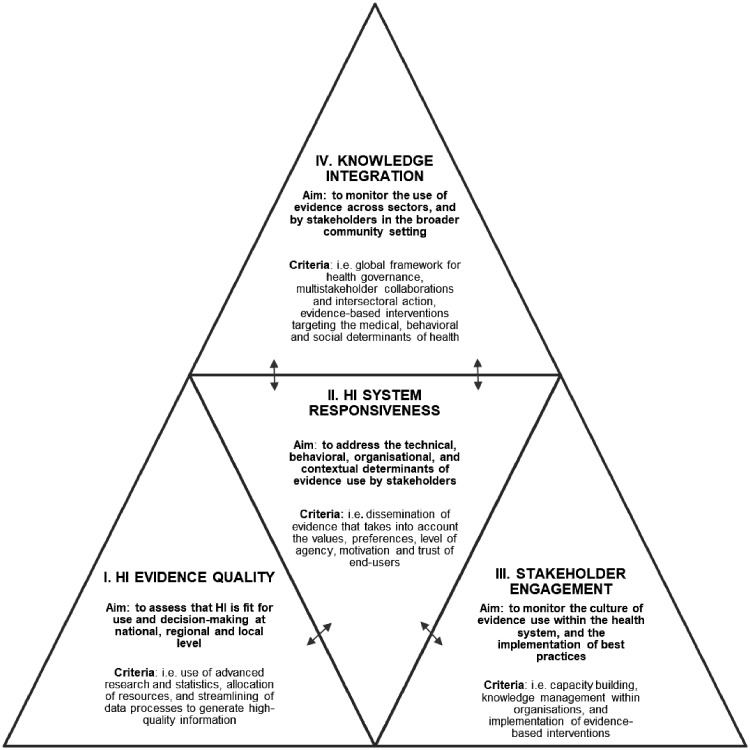
We developed a new model, the HI-Impact framework, in which four domains are essential for mapping the impact of national HI systems: (i) HI Evidence Quality, (ii) HI System Responsiveness, (iii) Stakeholder Engagement and (iv) Knowledge Integration. A comprehensive impact assessment of HI systems requires addressing the use of HI in public health decision-making, health service delivery and in other sectors which might have not been considered previously. Monitoring Stakeholder Engagement and Knowledge Integration certifies that the use of HI in all policies is an explicit point of assessment.
Introduction
National health information (HI) systems compile evidence on population health, the determinants of health and health system performance within countries (i.e. HI).1–3 HI is usually collected in routine from population health registers, health facilities, and also during national health surveys. Benchmarks of population characteristics, health and service needs are useful for research, decision-making and intervention in public health policy and practice.3,4 For example, we know that in Europe, there is up to 4-fold variation in stillbirth and infant mortality,5,6 persistent disparities in cancer mortality,7 and gender-based patterns in survival and disability8; knowledge of these inequalities has been used to inform more global frameworks that aim to ensure health for all (i.e. Sustainable Development Goal 3). In 2016, the World Health Organization (WHO) presented an action plan to strengthen the use of evidence for policy-making in the European Region.9,10 The current Joint Action on Health Information, InfAct, which gathers 40 public health institutes from 28 European countries also embodies this will for a more integrated HI strategy.3,4 Whereas the vision is clear, it requires monitoring the impact of national HI systems on reducing the evidence-to-practice gap.11 In this context, we define impact as the demonstrated use of evidence by stakeholders for decision-making and intervention in public health policy and practice.1,12–14
The Performance of Routine Information System Management (PRISM) framework was seminal in identifying the key features of efficient HI systems, including the use of information for decision-making.15 Yet, evaluations of these systems have traditionally focused more on statistical data processes and data quality, and less on how data are integrated to practice.1 On the other hand, the field of Knowledge Translation (KT) has developed frameworks that guide ‘the appropriate exchange, synthesis and ethically sound application of knowledge to interventions that strengthen the healthcare system and improve health’.16,17 Therefore, our aim with this study was to draw from the lessons learned in the field of KT in order to derive a new HI system evaluation framework—one based on monitoring the impact of national HI systems in healthcare, policy-making and service delivery, as well as in other sectors which might not have been considered previously.
Methods
Strategy
This article builds on the work done on the evaluation of HI systems by the WHO and the United States Agency for International Development (USAID).18–20 HI systems contribute to sound decision-making at all levels of the health system.2 End-users have different roles ranging from providing care, implementing screening programmes, planning interventions and policy-making. Therefore, the scope of our study bridges across different fields of practice which warranted a system-wide approach, and a broad search strategy. We conducted a scoping review of KT frameworks; this methodology answers far-reaching questions, and is more amenable than systematic reviews to explore the conceptual boundaries of a given topic.21 We investigated PubMed, Medline and the Cochrane Database of Systematic Reviews between August and December 2018, using common terms used to define KT in the literature. Straus et al.22 note that ‘the terms implementation science or research utilization are common in Europe, while in the United States, the terms dissemination and diffusion, research use, knowledge transfer, and uptake are often used. In Canada, the terms knowledge transfer and exchange and knowledge translation are employed’. We built our search using the following terms combined and truncated*: knowledge*, translation, health data*, dissemination, implementation, adaptation, evidence informed*, evidence based*, public health, health policy, healthcare, impact, health system*, performance, health information*, tool, framework, monitoring, evaluation (Supplementary annexe S1). We further examined the grey literature and websites of public health knowledge brokers (i.e. the Canadian National Collaborating Centre for Methods and Tools, the US Agency for Healthcare research and Quality, and Knowledge Translation Australia). Reference tracking was applied, and our bibliography was managed in RefManager 12.
Eligibility criteria
We focused on reviews of KT frameworks and interventions published between 2008 and December 2018. We used Nilsen’s taxonomy of KT frameworks for screening publications23 according to process-based (i.e. on the mechanisms and stages of evidence-use), or determinant-based frameworks (i.e. on the barriers and facilitators to evidence-use) operating at organizational and/or institutional level. Per standard scoping review methodology, we included publications even when the risk of bias was not explicitly assessed.21 We excluded, however, study protocols, commentaries, editorials and opinion pieces, or when the full-text article could not be retrieved (Flow chart in Supplementary annexe S1).
Data charting and analysis
Publications were essentially screened by the first author based on the title, the abstract and the full text. Inclusions and charting were independently compared for accuracy and completeness by the co-authors (D.I., F.T., H.V.O., and L.A.A.). From each source, we extracted the following:
Characteristics: author and citation; country of origin; publication year; and the number of studies/frameworks included in the review.
Content: Type of framework (e.g. KT processes/determinants), socio-ecological level (e.g. organization, community, systems); KT stage (e.g. dissemination and/or implementation), and field-use (e.g. community health, health policy and healthcare).
We conducted a thematic content analysis which consisted in examining (i) the mechanisms, and (ii) the determinants underpinning the use of evidence in practice. We defined practice as the act of intervening (directly or conceptually) in healthcare provision, service planning and delivery, policy-making and evaluation.
Results
In total, we screened 533 publications, and we included 79 publications on the mechanisms and determinants of KT. Reviews came primarily from the USA, Canada, Australia (65%) and the UK (22%). Across publications there were large differences in the terminology that was used—with respect to how evidence is defined (e.g. data, knowledge, research, innovations and ideas), or embedded into practice (e.g. knowledge uptake, transfer, exchange, circulation and brokering). Although our search spanned the last 10 years, most reviews were published in the last 5 (67%). There were many more KT publications in healthcare (53 studies), versus policy (16) or community health (8), and two reviews in public health in general. We saw an evolution in the publications, with a greater emphasis on KT in healthcare in the beginning of the study period, and over time an increasing focus on the use of evidence in health policy, and ultimately at the level of health system. This could indicate a growing trend in recognizing the importance of interdisciplinary interventions in KT, as also noted by Vollmar et al.24
The studies we included examined between 425 and 15926 different KT frameworks, and as shown in table 1, there were 45 reviews on the process of KT.17,22,23,25–65 In general, KT can be summarized as a dynamic and iterative cycle in which data-providers ‘push’9 information into the hands of a target audience—which is known as the dissemination stage.28 In turn, data-users can choose to ‘pull’9 this evidence for intervention in a particular setting (i.e. health facility, local community)—which is known as the implementation stage.28 Feedback from the field guides further practice changes, and informs future data needs thereby completing the process. In our study, there were 19 reviews on the dissemination of evidence to stakeholders, 26 on the implementation of evidence into practice. Another 34 reviews were focused on both aspects of dissemination and implementation highlighting their interdependency in the KT process. Some KT frameworks were applied in specific areas of health, namely: cancer research,48,49,58,66,67 child health and welfare,38,57,63,68,69 chronic illness,26,53,70,71 cardiovascular health,72 healthy aging,41,54,73 immunization,74 acute and primary care,27,71,75 mental health,37,38,51,68,73 nursing,76 physiotherapy,61 chiropractic,77 rehabilitation,39 renal replacement therapy53 and genomics.47
Table 1.
Reviews of knowledge translation process frameworks and interventions, in public health policy and practice, from 2008 to 2018
| Authors, ref | Title | Country | Year | Type of framework | KT stagea | Field | Socio-ecological levelb | No. of studies | No. of frameworks |
|---|---|---|---|---|---|---|---|---|---|
| Armstrong et al.25 | Knowledge translation strategies to improve the use of evidence in public health decision making in local government: intervention design and implementation plan | Australia | 2013 | Process | I | Public health; policy | Systems | 4 | |
| Ben et al.27 | Effective strategies for scaling up evidence-based practices in primary care: a systematic review | Canada, Australia | 2017 | Process | I | Healthcare primary care | Organizations | 14 | |
| Best et al.65 | Building knowledge integration systems for evidence-informed decisions. | Canada | 2009 | Process | D&I | Healthcare; policy | Organizations | 5 | |
| Brown et al.28 | An Overview of Research and Evaluation Designs for Dissemination and Implementation. | USA | 2017 | Process | D&I | Research; policy; healthcare | Systems | 8 | |
| Brownson et al.29 | Fostering more-effective public health by identifying administrative evidence-based practices: a review of the literature. | USA | 2012 | Process | I | Policy; administrative | Systems | 144 | |
| Burchett et al.30 | How do we know when research from one setting can be useful in another? A review of external validity, applicability and transferability frameworks. | UK | 2011 | Process | I | Public health | Systems | 38 | 35 |
| Contandriopoulos et al.31 | Knowledge exchange processes in organisations and policy arenas: a narrative systematic review of the literature | Canada | 2010 | Process | D&I | Organizations and policy-makers | Organizations, systems | 205 | |
| Darzi et al.32 | A methodological survey identified eight proposed frameworks for the adaptation of health related guidelines. | Lebanon, USA, Canada | 2017 | Process | D | Healthcare | Organizations | 8 | |
| Damschroder et al.56 | Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. | USA | 2009 | Process/Determinants | I | Healthcare | Systems | 19 | |
| Davison et al.34 | Critical examination of knowledge to action models and implications for promoting health equity | Canada | 2015 | Process | D&I | Healthcare; policy | Organizations, systems | 48 | |
| Davies et al.33 | Mobilising knowledge to improve UK health care: learning from other countries and other sectors – a multimethod mapping study. | UK | 2015 | Process/Determinants | D&I | Healthcare; social care and education | Systems | 71 | |
| Escoffery et al.35 | A systematic review of adaptations of evidence-based public health interventions globally | USA | 2018 | Process/Determinants | I | Community health | Systems | 42 | |
| Gagnon et al.57 | A Systematic Review of Knowledge Translation (KT) in Pediatric Pain: Focus on Health Care Providers. | Canada | 2016 | Process/Determinants | D&I | Healthcare | Organizations | 98 | |
| Gardois et al.36 | Health promotion interventions for increasing stroke awareness in ethnic minorities: a systematic review of the literature. | UK | 2014 | Process | I | Healthcare | Systems | 18 | |
| Goldner et al.37 | A narrative review of recent developments in knowledge translation and implications for mental health care providers | Canada | 2014 | Process/determinants | D&I | Healthcare: child mental health | Organizations | 61 | |
| Hack et al.58 | Facilitating the implementation of empirically valid interventions in psychosocial oncology and supportive care | Canada | 2011 | Process/Determinants | I | Healthcare: cancer | Systems | 3 | 28 |
| Hanson et al.38 | The what, when, and why of implementation frameworks for evidence-based practices in child welfare and child mental health service systems | USA | 2016 | Process/Determinants | I | Healthcare: child welfare and mental health | Systems | 9 | |
| Jones et al.39 | Translating knowledge in rehabilitation: systematic review | USA | 2015 | Process/Determinants | I | Healthcare: rehabilitation | Organizations | 26 | |
| Kneale et al.59 | The use of evidence in English local public health decision-making: a systematic scoping review. | UK | 2017 | Process/Determinants | D&I | Public health; policy | Systems | 23 papers from 21 studies | |
| Leeman et al.40 | What strategies are used to build practitioners' capacity to implement community-based interventions and are they effective?: a systematic review | UK | 2015 | Process | I | Healthcare, community health | Systems | 42 papers from 29 studies | |
| Leeman et al.131 | Developing Theory to Guide Building Practitioners' Capacity to Implement Evidence-Based Interventions. | USA | 2017 | Process | I | Public health | Systems | 24 | |
| Lourida et al.41 | Dissemination and implementation research in dementia care: a systematic scoping review and evidence map. | UK | 2017 | Process/Determinants | D&I | Healthcare: geriatrics | Organizations | 88 | |
| Mairs et al.42 | Online strategies to facilitate health-related knowledge transfer: a systematic search and review. | Canada | 2013 | Process/Determinants | D | Community health | Systems | 45 | |
| Matus et al.43 | Research capacity building frameworks for allied health professionals - a systematic review. | Australia | 2018 | Process | D | Healthcare: allied health professionals | Organizations | 6 | |
| Meyers et al.44 | The quality implementation framework: a synthesis of critical steps in the implementation process. | USA | 2012 | Process | I | Healthcare; community health | Systems, organizations | 25 | |
| Milat et al.45 | Narrative review of frameworks for translating research evidence into policy and practice | Australia | 2017 | Process | D&I | Healthcare and policy | Systems | 41 | |
| Moullin et al.46 | A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. | Australia | 2015 | Process | I | Research, policy, healthcare | Systems | 49 | |
| Nilsen et al.23 | Making sense of implementation theories, models and frameworks | Sweden | 2015 | Process | I | Public health | Systems | 38 | |
| Payne et al.47 | Translational informatics: enabling high-throughput research paradigms. | USA | 2009 | Process | D&I | Healthcare: genomics | Organizations, systems | ||
| Rajan et al.48 | Critical appraisal of translational research models for suitability in performance assessment of cancer centers. | The Netherlands | 2012 | Process | D&I | Healthcare: cancer | Organizations | 12 | |
| Senore et al.49 | How to enhance physician and public acceptance and utilisation of colon cancer screening recommendations | Italy | 2010 | Process/Determinants | D&I | Healthcare: cancer, community health | Organizations, systems | NA | |
| Slade et al.50 | Frameworks for embedding a research culture in allied health practice: a rapid review | Australia | 2018 | Process | D&I | Healthcare | Organizations | 16 | |
| Stander et al.61 | Training programmes to improve evidence uptake and utilisation by physiotherapists: a systematic scoping review. | South Africa, Australia | 2018 | Process | D&I | Healthcare: physiotherary | Organizations | 10 | |
| Stirman et al.51 | Bridging the Gap Between Research and Practice in Mental Health Service Settings: An Overview of Developments in Implementation Theory and Research. | USA | 2016 | Process | I | Healthcare: mental health setting | Organizations | 73 | |
| Straus et al.22 | Knowledge translation is the use of knowledge in health care decision making | Canada | 2011 | Process/determinants | D&I | Healthcare | Organizations | NA | |
| Strifler et al.26 | Scoping review identifies significant number of knowledge translation theories, models, and frameworks with limited use. | Canada | 2018 | Process | D&I | Healthcare: cancer and chronic diseases | Organizations | 596 | 159 |
| Tabak et al.52 | Bridging research and practice: models for dissemination and implementation research. | USA | 2012 | Process | D&I | Research | Systems | 61 | |
| Van der Veer et al.53 | Translating knowledge on best practice into improving quality of RRT care: a systematic review of implementation strategies. | Netherlands | 2011 | Process | I | Healthcare: renal placement therapy; chronic care | Organizations | 93 | |
| Van Eerd et al.54 | Knowledge brokering for healthy aging: a scoping review of potential approaches. | Canada | 2016 | Process | D&I | Healthcare: healthy aging | Organizations | 19 | |
| Ward et al.62 | Developing a framework for transferring knowledge into action: a thematic analysis of the literature. | UK | 2009 | Process | D&I | Public health | Organizations, systems | 28 | |
| Whitney et al.27 | Evaluation of health information outreach: theory, practice, and future direction. | USA | 2014 | Process/determinants | D | Public health | Systems | 33 | |
| Welch et al.55 | Health equity: evidence synthesis and knowledge translation methods | Canada | 2013 | Process | D | Research | Systems | 34 | |
| Wilson et al.64 | Disseminating research findings: what should researchers do? A systematic scoping review of conceptual frameworks. | UK | 2010 | Process | D | Research | Systems | 33 | |
| Wilson et al.63 | Knowledge translation studies in paediatric emergency medicine: A systematic review of the literature. | Canada | 2016 | Process | D | Healthcare: child health | Organizations | 15 | |
| Yost et al.17 | Knowledge translation strategies for enhancing nurses' evidence-informed decision making: a scoping review. | Canada | 2014 | Process | I | Healthcare: nursing | Organizations | 274 |
Notes: In Table 1, we are only listing publications focused on KT processes (45 out of 79); publications focused on KT determinants are included in tables 2 and 3.
D: Dissemination (targeted outreach to stakeholders with evidence): I: Implementation (use of evidence for intervention in a specific setting).
Socio-ecological level: “systems”, if more than one organizational level is involved: that is health policy and health care.
A common starting point in the KT frameworks we reviewed was the generation of high-quality data.9,22,28–31,33,34,36,37,45,52,54–56,64,78–80 We identified three main attributes of data quality: statistical accuracy, content relevance and coverage.9,11 Standardized methodological approaches, data innovations and advanced statistical methods can improve the accuracy of evidence provided to stakeholders.67 On the other hand, content relevance is ensured by providing the data needed by stakeholders for planning, care or service delivery (i.e. information on the burden of disease, or on cost effectiveness and feasibility).33,81 Adequate coverage in the data provides for more equity in the interventions.9,30,36,82 For instance, disaggregated data by age, gender or socio-economic status are needed to plan actions that target vulnerable segments of the population, diverse communities or subgroups at the highest health risk.67,83,84
We found that although data production initiates the KT process, dissemination carries it through. Jones et al.39 note that strategies range from passive methods such as printed educational material to more active multicomponent strategies involving audit and feedback from local opinion leaders, while only relying on printed material is regarded as a ‘reasonably ineffective KT strategy’. Two methods, however, have been recognized by Blessing et al.9,39 as particularly useful: (i) Exchange methods in which data-providers and policy-makers for instance work in partnership, as well as (ii) Integrated methods ‘where a knowledge translation platform is institutionalized in an organization or in the broader health system’. When stakeholders have access to evidence, this can spearhead problem recognition and the development of meaningful solutions in the field.9,24 These include actions whether legal, financial or political that align with national and international health targets.25,38,59,81,85–88
During the implementation stage, Davies et al.33 emphasize that there are three broad types of knowledge use: instrumental (i.e. for direct application in the field), conceptual (i.e. for problem-solving and agenda setting) and symbolic (i.e. in support of predetermined positions or after the decision has already been made). Donaldson et al. suggest monitoring intermediate shifts in stakeholders’ knowledge, attitude and skills89 as proof that evidence has been accessed and used,90 granted few frameworks provide specific KT outcome or impact measures.91,92
Although in general, KT frameworks share the aforementioned characteristics, we found notable differences in the intricacy of the data-provider/data-user interaction across publications.45,52 For instance in the prominent Re-aim framework, there are five dimensions to consider: reach (R) and effectiveness (E), operate essentially at individual-level; whereas adoption (A), implementation (I) and maintenance (M) are focused on organizational and community-level change.45 Another highly cited model, the Knowledge-to-Action framework is based on two components: (i) the Knowledge creation funnel in which research data is generated, synthesized and contextualized to become more useful, and (ii) the Action cycle which includes a range of actions targeting changes in stakeholders’ level of understanding, behaviours and attitudes.45 Other models explicitly rely on the latest developments in health information technology for the dissemination and implementation stages. For instance, in the Learning Healthcare Systems framework, electronic health records and data mining facilitate exchanges between data-users and data-providers; this model also puts emphasis on shared decision-making between patients and care providers with the aim to bring quality improvements in clinical care.93
There were 58 reviews which explored the determinants of the use of evidence in healthcare, public health policy-making and service delivery. Among which, six were focused on the tools (i.e. checklists and guidelines) which have been developed to facilitate the access to, and the use of evidence.9,16,17,80,94,95 We have summarized KT determinants by field of practice (e.g. healthcare, policy-making and community health) in tables 2 and 3. Studies insisted on lifting technical (i.e. availability and access to evidence), behavioural (i.e. motivation and competence), organizational (i.e. culture of evidence-use) and contextual KT barriers (i.e. political and social)11,15,33,35,41,54,59,66,81,87,88,96–98 as shown in table 2. Whereas in table 3, we identified attributes that promote KT and the successful dissemination of evidence such as: (i) clarity of the data/evidence, (ii) timeliness, (iii) a tailored reporting format based on stakeholders’ preferences and (iv) the use of tools to facilitate access to research (i.e. packaging, application, dissemination and communication tools).9,41,42,54,56,59,64,67,80,81,96,99–101
Table 2.
Technical, behavioural, organizational and contextual barriers to KT in public health policy and practice
| Decision-makers | Technical | Behavioural | Organizational | Contextual |
|---|---|---|---|---|
| Community health managers |
|
|||
| Health policy-makers |
|
|||
| Clinicians and allied health professionals |
|
a Patient needs, preferences and adherence to treatment when these interfere with evidence-based recommendations22,56,72 |
Notes: KT determinants are categorized by themes (technical, behavioural, organizational and contextual).
Field specific determinant.
Table 3.
Technical, behavioural, organizational and contextual solutions for promoting KT in public health policy and practice
| Decision-makers | Technical | Behavioural | Organizational | Contextual |
|---|---|---|---|---|
| Community health managers |
|
|
|
|
| Health policy-makers |
|
|
|
|
| Clinicians and allied health professionals |
|
|
|
|
Notes: KT determinants are categorized by themes (technical, behavioural, organizational and contextual) and subthemes which are underlined.
Field specific determinant.
In table 3, we have listed further recommendations for engaging stakeholders at the organizational and institutional level in using evidence, and adopting best practices.56 In policy, a setting that has a ‘stable, clear and decentralized decision-making authority’ is said to have a greater capacity to adopt innovations.102 When leaders commission or champion evidence themselves this can facilitate the KT process.9,100 Inter-sectorial structures (i.e. the EU Joint Research Centre) and institutionalized knowledge brokers can also play a role in disseminating evidence in a whole-of-government approach.33 A common understanding between data-providers and data-users, a sense of trust, a shared vision among stakeholders and the provision of resources also facilitate KT (table 3). Nonetheless, we also found that there are many competing sources of information which can interfere with KT. At the level of the decision-maker, testimonials and narratives can sometimes be considered more convincing for policy-making,103 as well as advice from personal contacts, sometimes mid-level managers with no direct expertise in public health.104,105
In medical facilities, Reschovsky et al.106 state that the extent to which KT occurs can vary by clinical indication, specialty and health service setting (i.e. operational size, structure: private vs. public). We found that engaging frontline staff and health managers in improving data collection and its use is crucial for team transformation and quality improvement107; capacity building and workforce development also.31,43,61,70,72,81,95,108 A culture of evidence-use can also be supported by health information technology to facilitate a rapid access to evidence (i.e. e-journals, clinical decision support systems).41,68,80,94,109 Local opinion leaders,85 greater social cohesion in medical facilities,41,80,106,110 performance rankings,14 providing resources and financial incentives further contribute to KT at organizational level.9,14,43,59,79,100,106
There were additional determinants related to the sustainability of the KT process. Fifteen reviews highlighted that embedding evidence within social contexts is essential for achieving system level change within organizations and local communities25,30,31,35,40,42,59,65,66,67,69,85,97,110,111; although Davies et al.33 noted that very few KT strategies targeted the general public. In a study of adaptations in evidence-based interventions, the most cited concern was the need for cultural appropriateness, and acceptability.35 Common adaptations included content (100%), context (95.2%), cultural modifications (73.8%) and delivery (61.9%).35 This relies on the consolidation of partnerships for health, and outreach to key players in the communities where the interventions would take place. Haynes et al.112 note that platforms for cross-sectoral collaborations can increase decision-makers’ capacity to use evidence. This highlights the importance of appraising potential conflicts of interests across stakeholder groups113 when KT is the aim.
Finally, we have synthesized our finding into four domains that are relevant for capturing the mechanisms and determinants that drive KT. The domains of ‘HI Evidence Quality’, ‘HI System Responsiveness’, ‘Stakeholder Engagement’ and ‘Knowledge Integration’ constitute the building blocks of the HI-Impact framework shown in figure 1. These conceptual domains could serve to monitor the impact of national HI systems on reducing the evidence-to-practice gap. More specific evaluation criteria could be developed in each domain to address the quality of the evidence provided by HI systems, the extent of the dissemination efforts (i.e. evaluating ‘Responsiveness’), and how this evidence has influenced decision-making and intervention (i.e. the level of ‘Stakeholder Engagement’ and ‘Knowledge Integration’ across practice fields). We develop further the relevance of these domains for HI systems evaluation in the discussion.
Figure 1.
The Health Information (HI)-Impact framework: evaluation domains for monitoring the impact of national health information systems in public health policy and practice. Notes: I. Health Information (HI) Evidence Quality relates to data production, accuracy and content relevance; II. HI System Responsiveness reflects the attributes of the wider data infrastructure that enhance the likelihood of information to be used—by improving the end-user experience and addressing expectations on how to access and work with the data; this domain mediates the interaction between the HI systems that generate evidence and the decision-makers in public health policy and practice as represented by the double arrows; III. Stakeholder Engagement relates to the use of HI for training, decision-making and the implementation of interventions in public health policy and practice; IV. Knowledge Integration relates to the use of HI by community partners, in multi-stakeholder coalitions, and for cross-sectoral actions with a broader reach on the determinants of health. This domains builds on the other three domains and furthers the use of HI in all policies for a greater societal impact
Discussion
Securing evidence for policy development and intervention is not a strictly linear process. KT relies on feedback and exchange mechanisms between data-providers and data-users working in government, clinics, health agencies and in the broader community. To our knowledge, this study is the first to propose an original framework for monitoring the impact of national HI systems based on lessons from the field of KT. However, we experienced several methodological limitations during the scoping review. As stated by Goldner et al.37 and Straus et al.,22 the concept of KT is an umbrella term and inconsistencies in the terminology made it more difficult to screen eligible publications. There is a lack of guidance in choosing one KT framework over another, many KT frameworks have not been evaluated, and consensual outcome measures of KT are lacking.102,114–116 Nevertheless, a strength of this scoping review is the breadth of our research, we have examined 79 reviews of KT frameworks encompassing 3916 studies. Furthermore, a new HI systems evaluation framework focusing on impact is highly relevant for Europe given that PRISM was originally intended for strengthening systems in low- and middle-income countries,15 and the KT tools from other high-income countries such as the USA or Canada were not intended for the evaluation of national HI systems.
National HI systems and the data they produce are needed to respond to complex health and health system challenges.24,117 However, ensuring that routinely collected data are fit-for-use and decision-making can be a challenge. HI systems collect dispersed data from various sources, including systems which were not initially established for public health surveillance purposes (i.e. administrative and health insurance registries). The quality of routinely collected HI can also vary, and there are noted issues with the ascertainment of causes-of-death statistics for instance across countries. Despite these limitations, routinely collected data are often the best evidence available at population level for decision-makers. Therefore, ensuring that robust and timely evidence is generated and accessed by stakeholders is important, and this is why we have included ‘HI Evidence Quality’ as one of our domains (see figure 1) in line with traditional HI system evaluation frameworks.1
The cycle of evidence-informed public health starts with data.24 Without it, decision-makers cannot assess the problem or act on it effectively. Yet, the quality of information alone cannot guarantee that it will be used for decision-making.118,119 In public health, there is a lack of global operational guidelines for data sharing.120 Therefore, it is also relevant to consider what can be done to facilitate the access to evidence for intervention. ‘Responsiveness’ is a term originally used to describe the quality of the patient–provider dyad and interaction; it encompasses attributes which promote the best patient experience that are linked to quality of care and outcomes (i.e. dignity, respect and autonomy).121 Given the importance of dissemination in the KT process, we propose an original application of the concept of ‘Responsiveness’ to HI systems. A responsive HI system would aim to facilitate the access to, and use of HI by lifting the technical, behavioural, organizational and contextual barriers to evidence-use (those listed in table 2).
In our framework, monitoring ‘HI Evidence Quality’, and ‘HI System Responsiveness’ would provide insight on the availability and accessibility of robust and credible evidence. This could entail monitoring whether the evidence provided to stakeholders adheres to the FAIR: findable, accessible, interoperable and reusable data principles.122 Anell et al.123 also noted that the reporting format has an influence on decision-making, and with ‘league tables, decision-makers tended to suggest more actions compared to funnel plots’ which could be another point of evaluation. Since community mobilization and social marketing approaches have also been recognized as effective KT strategies,37 new types of data capture methods (i.e. real-world data from sensors, mobile phones and social media) might also play a role in the evaluation of ‘Responsiveness’. When data are presented in international conferences and high-impact journals, synthesized for decision-makers,124 and also presented in plain language summaries, and in social media,125 this can increase the impact of HI systems. For example, Euro-Peristat, a European maternal and child health information network uses a wide array of dissemination strategies to reach their stakeholders in 31 countries. Euro-Peristat results are published in comprehensive reports for clinicians and policy-makers, presented in international scientific conferences and peer-reviewed journals, on their project website and in a quarterly newsletter.
Our review of KT determinants also highlighted the importance of organizational readiness for evidence-based practice. Therefore, monitoring HI system use within healthcare facilities, and institutions is the third domain in our framework (figure 1) which we refer to as ‘Stakeholder Engagement’. The increasing use of multidimensional and composite indicators such as the Healthy Life Years,13 and the Disability Adjusted Life Years illustrate the need for HI systems to provide data that resonate with the complex problems that policy-makers face in health.126 Yet, the lack of joint understanding can negatively influence the KT process, and the sustainability of evidence-based interventions in the field.59,98 For example in 2018, the French Government pushed for the reduction of the speed limitation from 90 to 80 km/h−1 (50 mph) on two-lane highways. Despite data on the number of avoidable deaths (300–400 per year), and an increasing trend in road mortality since 2014, this measure was met with significant resistance from local authorities. Ultimately, national enforcement was amended to voluntary implementation by the regions. (https://www.theguardian.com/world/2018/jan/10/france-cuts-speed-limit-rise-deaths). Politics and external actors with vested interests also influence policies—this can lead to dissonance when objectives across sectors do not align to improve health.12,127 In Europe, the Joint Research Centre, EVIPnet and the European Health Observatory facilitate the continued use of evidence in policy development.
Monitoring the impact of HI systems within the broader social context could provide valuable information on the extent of HI system use. This is because health is largely influenced by determinants outside the health sector as recognized in Dahlgren and Whitehead’s128 model of the layers of influence on health, and the more recent focus on ‘Health in all policies’.86 Therefore, we have included ‘Knowledge Integration’ in civil society and across sectors as the fourth domain in the HI-Impact framework. This domains relates to the effective incorporation of knowledge into the decisions, practices and policies of organizations and systems.65 With the Sustainable Development Goals, countries have been encouraged to build alliances for health in all policies; yet these integrated approaches are currently not reflected in the way national HI systems are being evaluated.86 In their review of HI system evaluation frameworks, Eslami et al.1 stressed that the role of context has been largely neglected thus far, and requires more attention.
Together, the domains of ‘Stakeholder engagement’ and ‘Knowledge integration’ aim to ensure that HI systems are providing data that are used in coherent interventions on the medical, social and commercial determinants of health. These domains expand the scope of existing HI system evaluation frameworks, by examining the contextual impact of HI systems in areas which might not have been considered before (i.e. across sectors and by the general public). In a recent study, commissioned by the European Parliament, it was noted that ‘faced with emerging threats relating to the spread of disinformation and pseudo-science (…) fostering scientific literacy can provide people with tools to navigate (…) the vast amounts of information exchanged in public debate.’ The inefficient use of healthcare services and poorer health also depends on the level of health knowledge, socio-demographic characteristics and education.129,130 Therefore, increasing scientific and health literacy could constitute another important lever of impact for HI systems.
In conclusion, the field of KT could serve to secure current and future investments in HI systems, by drawing attention to the mechanisms and determinants of evidence-based public health practice and policy-making. In this study, we have answered how we might want to evaluate the impact of national HI systems, and why the HI-Impact framework domains could be relevant. However, input from public health professionals and policy-makers will be critical to operationalize what specifically should be evaluated in each domain. To this aim, we have conducted an online DELPHI exercise with experts in 38 countries, and the development of an evaluation tool based on the HI-Impact framework is currently underway. Further piloting in European public health agencies could contribute to a more balanced assessment of HI systems in each country—one that takes into account the quality of the evidence, as well as the health and societal impact of the systems generating these data.
Funding
M.D. is funded by a Marie Skłodowska-Curie Action Individual Fellowship, GA No 795051; D.I. is funded by HealthPros, a Marie Skłodowska-Curie Innovative Training Network, and GA No 765141.
Conflicts of interest: None declared.
Key points
Creating a culture of accountability for evidence-based decision-making requires close monitoring of health information (HI) use in policy, at the points of care and service delivery, and in the broader community.
Current frameworks used to evaluate the performance of HI systems focus on data production; we however, encourage giving increased attention to the dissemination, relevance and use of HI in all policies, and by new actors in civil society.
There should be a deliberate strategy to provide HI to stakeholders within and outside the health system for a greater societal impact.
Supplementary Material
References
- 1. Eslami AA, Scheepers H, Rajendran D, Sohal A. Health information systems evaluation frameworks: a systematic review. Int J Med Inform 2017;97:195–209. [DOI] [PubMed] [Google Scholar]
- 9. Blessing V, Davé A, Varnai A Evidence on Mechanisms and Tools for Use of Health Information for Decision-Making. Health Evidence Network Synthesis Report 54, Copenhagen. 2017. Available at: http://www.euro.who.int/en/publications/abstracts/evidence-on-mechanisms-and-tools-for-use-of-health-information-for-decision-making-2017 (December 2018, date last accessed). [PubMed]
- 11. Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. Int J Qual Health Care 2014;26:321–9. [DOI] [PubMed] [Google Scholar]
- 13. Bogaert P, Van Oyen H, Beluche I, et al. The use of the global activity limitation Indicator and healthy life years by member states and the European Commission. Arch Public Health 2018;76:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Levesque JF, Sutherland K. What role does performance information play in securing improvement in healthcare? A conceptual framework for levers of change. BMJ Open 2017;7:e014825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aqil A, Lippeveld T, Hozumi D. PRISM framework: a paradigm shift for designing, strengthening and evaluating routine health information systems. Health Policy Plan 2009;24:217–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Peirson L, Catallo C, Chera S. The Registry of Knowledge Translation Methods and Tools: a resource to support evidence-informed public health. Int J Public Health 2013;58:493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Straus SE, Tetroe JM, Graham ID. Knowledge translation is the use of knowledge in health care decision making. J Clin Epidemiol 2011;64:6–10. [DOI] [PubMed] [Google Scholar]
- 26. Strifler L, Cardoso R, McGowan J, et al. Scoping review identifies significant number of knowledge translation theories, models, and frameworks with limited use. J Clin Epidemiol 2018;100:92–102. [DOI] [PubMed] [Google Scholar]
- 31. Contandriopoulos D, Lemire M, Denis JL, Tremblay E. Knowledge exchange processes in organisations and policy arenas: a narrative systematic review of the literature. Milbank Q 2010;88:444–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Davies HTO, Powell AE, Nutley SM. Mobilising knowledge to improve UK health care: learning from other countries and other sectors—a multimethod mapping study. Health Serv Delivery Res 2015;3:1. [PubMed] [Google Scholar]
- 34. Davison CM, Ndumbe-Eyoh S, Clement C. Critical examination of knowledge to action models and implications for promoting health equity. Int J Equity Health 2015;14:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Escoffery C, Lebow-Skelley E, Haardoerfer R, et al. A systematic review of adaptations of evidence-based public health interventions globally. Implement Sci 2018;13:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mairs K, McNeil H, McLeod J, et al. Online strategies to facilitate health-related knowledge transfer: a systematic search and review. Health Info Libr J 2013;30:261–77. [DOI] [PubMed] [Google Scholar]
- 45. Milat AJ, Li B. Narrative review of frameworks for translating research evidence into policy and practice. Public Health Res Pract 2017;27:pii2711704. [DOI] [PubMed] [Google Scholar]
- 49. Senore C, Malila N, Minozzi S, Armaroli P. How to enhance physician and public acceptance and utilisation of colon cancer screening recommendations. Best Pract Res Clin Gastroenterol 2010;24:509–20. [DOI] [PubMed] [Google Scholar]
- 52. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med 2012;43:337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Van Eerd D, Newman K, DeForge R, et al. Knowledge brokering for healthy aging: a scoping review of potential approaches. Implement Sci 2016;11:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Sci 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gagnon MM, Hadjistavropoulos T, Hampton AJ, Stinson J. A systematic review of knowledge translation (KT) in pediatric pain: focus on health care providers. Clin J Pain 2016;32:972–90. [DOI] [PubMed] [Google Scholar]
- 67. Rabin BA, Glasgow RE, Kerner JF, et al. Dissemination and implementation research on community-based cancer prevention: a systematic review. Am J Prev Med 2010;38:443–56. [DOI] [PubMed] [Google Scholar]
- 69. van der Kleij R, Coster N, Verbiest M, et al. Implementation of intersectoral community approaches targeting childhood obesity: a systematic review. Obes Rev 2015;16:454–72. [DOI] [PubMed] [Google Scholar]
- 70. Attieh R, Gagnon MP, Estabrooks CA, et al. Organizational readiness for knowledge translation in chronic care: a review of theoretical components. Implement Sci 2013;8:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Baatiema L, Otim ME, Mnatzaganian G, et al. Health professionals' views on the barriers and enablers to evidence-based practice for acute stroke care: a systematic review. Implement Sci 2017;12:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kastner M, Bhattacharyya O, Hayden L, et al. Guideline uptake is influenced by six implementability domains for creating and communicating guidelines: a realist review. J Clin Epidemiol 2015;68:498–509. [DOI] [PubMed] [Google Scholar]
- 81. Oliver K, Innvar S, Lorenc T, et al. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res 2014;14:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Flodgren G, Parmelli E, Doumit G, et al. Local opinion leaders: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2011;CD000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Guglielmin M, Muntaner C, O’Campo P, Shankardass K. A scoping review of the implementation of health in all policies at the local level. Health Policy 2018;122:284–92. [DOI] [PubMed] [Google Scholar]
- 87. Orton L, Lloyd-Williams F, Taylor-Robinson D, et al. The use of research evidence in public health decision making processes: systematic review. PLoS One 2011;6:e21704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Donaldson NE, Rutledge DN, Ashley J. Outcomes of adoption: measuring evidence uptake by individuals and organisations. Worldviews Evid Based Nurs 2004;1(Suppl. 1):S41–51. [DOI] [PubMed] [Google Scholar]
- 92. Lewis CC, Fischer S, Weiner BJ, et al. Outcomes for implementation science: an enhanced systematic review of instruments using evidence-based rating criteria. Implement Sci 2015;10:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Tricco AC, Cardoso R, Thomas SM, et al. Barriers and facilitators to uptake of systematic reviews by policy makers and health care managers: a scoping review. Implement Sci 2016;11:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Lorenc T, Tyner EF, Petticrew M, et al. Cultures of evidence across policy sectors: systematic review of qualitative evidence. Eur J Public Health 2014;24:1041–7. [DOI] [PubMed] [Google Scholar]
- 98. van de Goor I, Hamalainen RM, Syed A, et al. Determinants of evidence use in public health policy making: results from a study across six EU countries. Health Policy 2017;121:273–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Quinn E, Huckel-Schneider C, Campbell D, et al. How can knowledge exchange portals assist in knowledge management for evidence-informed decision making in public health? BMC Public Health 2014;14:443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Reschovsky JD, Rich EC, Lake TK. Factors contributing to variations in physicians' use of evidence at the point of care: a conceptual model. J Gen Intern Med 2015;30(Suppl. 3):S555–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Huckel SC, Campbell D, Milat A, et al. What are the key organisational capabilities that facilitate research use in public health policy? Public Health Res Pract. 2014;25:e2511406. [DOI] [PubMed] [Google Scholar]
- 120. van Panhuis WG, Paul P, Emerson C, et al. A systematic review of barriers to data sharing in public health. BMC Public Health 2014;14:1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Malekinejad M, Horvath H, Snyder H, Brindis CD. The discordance between evidence and health policy in the United States: the science of translational research and the critical role of diverse stakeholders. Health Res Policy Syst 2018;16:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Gellert P, Tille F. What do we know so far? The role of health knowledge within theo-ries of health literacy. Eur Health Psychol 2018;17:266–74. [Google Scholar]
- Missing references are listed online in the Supplementary material.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.