Abstract
Background
Various factors associated with vaccination uptake in children have been identified, but no study has examined their overall immunization status and individual vaccine coverage at 1, 2 and 5 years in the UK.
Methods
Data from 6977 participants in the Born in Bradford cohort were linked to primary care records. Overall immunization status and individual vaccine uptake of the UK routine childhood vaccination schedule was estimated in White British and Pakistani children born between 2007 and 2011, and factors associated with partial uptake in each ethnic group were identified using Poisson regression.
Results
Vaccine uptake was greater in Pakistani compared with White British children at all ages and for each year examined in this study. Children of foreign-born White British women were more likely to be partially immunized and those of foreign-born Pakistani women were more likely to be fully immunized. Socio-economic factors were strongly associated with uptake, especially among White British women.
Conclusions
Vaccination uptake is influenced by social and economic environment, ethnicity and maternal country of birth. This suggests that current health education and service delivery may not be effective for some families, including those from different cultural and ethnic backgrounds, who may require targeted interventions to improve immunization uptake.
Introduction
Immunization is important for protection against disease at both the individual and the population levels. The World Health Organisation considers that a 95% vaccination uptake of the measles vaccine is necessary to achieve herd immunity, which is defined as ‘the reduction of infection or disease in the unimmunized segment as a result of immunizing a proportion of the population’.1 The UK immunization schedule of childhood vaccinations is routinely offered to all children free of charge via the National Health Service (NHS). The schedule consists of a number of vaccinations given at recommended ages, which are guided by the age-specific risk of a disease, the risk of disease complications and the ability to respond to the vaccine.2 However, not all children receive the full series of immunizations. Previous research has identified a number of factors associated with poor vaccination uptake, including lone parenthood,3,4 younger or older mothers,3,4 a low socio-economic status,4,5 smoking during pregnancy,4 employment status3,4 and living in a household where there are other children.3–5 Other studies have reported higher uptake in children from ethnic minority populations,6,7 but lower uptake in children of foreign-born mothers.8,9 Most existing studies have examined uptake of single vaccines or antigens; those that examined uptake of all vaccinations were either limited to the first year of life or non-UK studies, and all were cross-sectional. The aims of this study were to (i) estimate overall immunization status and the coverage of individual vaccines included in the child immunization schedule in a longitudinal birth cohort at 1, 2 and 5 years of age, (ii) examine whether uptake differed by year of birth and (iii) identify factors associated with partial uptake of immunizations at 1, 2 and 5 years of age.
Methods
Participants
The sample comprised participants enrolled in the Born in Bradford (BiB) cohort, details of which have been reported previously.10 Briefly, women were recruited to the study at around 26 weeks gestation when they attended their oral glucose tolerance test appointment, a routine procedure offered to all women booked for delivery at Bradford Royal Infirmary, Bradford, UK. A total of 12 453 women were recruited across 13 776 pregnancies between March 2007 and December 2010, resulting in 13 858 births. Participants gave their consent for access to their own and their child’s General Practitioner (GP) primary care records via SystmOne, a clinical computer system used by all GP practices in Bradford. Cohort participants were matched deterministically to SystmOne using NHS number, surname and date of birth. Ethics approval was granted by Bradford National Health Service Research Ethics Committee (ref 07/H1302/112).
Supplementary figure S1 shows the flow of participants through the study. Of the 13 858 children participating in the BiB study, 74 could not be matched to primary care records, 2864 were not registered with a GP for the entire first 5 years of life, and 1256 did not have a baseline questionnaire or had missing data on the predictors under consideration. Ethnicity was self-defined by the mother in the baseline questionnaire and was used to define the ethnicity of her child. The majority of BiB participants is of White British and Pakistani ethnicity; therefore, due to low numbers and heterogeneity of other ethnic groups, a further 1844 children were excluded from the analysis. Also excluded were children who were registered at GP practices where there were less than 20 children in each ethnic group (443 White British and 381 Pakistani) to avoid level 1 sparseness of data (see Statistical Analysis section), and children born after 31 March 2011 (n = 19) to enable year-by-year comparison with national figures (which are calculated yearly from 1 April to 31 March). Our final sample size was 6977 (3060 White British and 3917 Pakistani).
Outcome measures
We assessed overall immunization status (none, partial and full) at 1, 2 and 5 years of age and uptake of individual vaccines that were not subject to changes in schedules or policy during the time-period under observation (see Supplementary table S1):
- 1 year:
- Diphtheria, tetanus, pertussis, polio and haemophilus influenzae type b vaccine (DTaP/IPV/Hib).
- Meningococcal C vaccine (MenC).
- Pneumococcal conjugate vaccine (PCV).
-
2 years:
Diphtheria, tetanus, pertussis and polio and haemophilus influenzae type B vaccine (DTaP/IPV/Hib).
Haemophilus influenzae type B/meningococcal C booster (Hib/MenC).
Pneumococcal conjugate booster (PCV).
Measles, mumps and rubella, first dose (MMR 1); doses are given below age of 1 year were discounted.2
-
5 years:
Diphtheria, tetanus, pertussis and polio booster (DTaP/IPV).
Measles, mumps and rubella, first dose (MMR 1).
Measles, mumps and rubella, first and second dose (MMR 1 and 2).
Co-variables
We examined the following factors that have previously been associated with vaccination uptake: maternal age, marital status, smoking during pregnancy, highest maternal educational attainment, receipt of means-tested benefits (as a proxy for socio-economic status), number of other children aged under 15 years in the household and mother’s place of birth. Information for all of the above was obtained from the baseline questionnaire administered at recruitment.
Statistical analysis
The distributions of the outcomes and co-variables were examined overall and separately for White British and Pakistani ethnic groups, and the differences between the ethnic groups were compared using chi-squared tests. Immunization status overall and for individual vaccines at 1, 2 and 5 years (none, partial and full) is presented as frequency (%). As very few participants were unimmunized, we examined factors associated with partial immunization status only [defined as a child not receiving one or more of their routine vaccinations by each time point (1, 2 and 5 years)]. Two multi-level Poisson regression analyses with robust error variances were performed (univariable and backwards stepwise regression), with child as the first level and GP practice as the second level to account for clustering within GP practice. Variables with a likelihood ratio test P-value <0.2 in the univariable model were included in the stepwise regression model, and those where P < 0.05 were retained in the final model. Results are presented as risk ratios with 95% confidence intervals. All analyses were conducted using STATA/SE software (Stata/SE 13.1, StataCorp, College Station, TX, USA).
Results
Characteristics of the sample overall and by ethnic group are presented in table 1. Compared with White British mothers, Pakistani mothers were older, less likely to be a single parent or smoke during pregnancy, more likely to be educated to degree level, be in receipt of means-tested benefits, born outside the UK and have more children under the age of 15 living in their household. The immunization status of children for all vaccines at 1, 2 and 5 years of age is presented in table 2. At 1 year of age, 9% of White British children and 1% of Pakistani children had not received any vaccinations. This fell to 3.5 and 0.5%, respectively, at 2 years of age and by age 5 less than five White British child remained unimmunized. The percentage of children fully immunized at each age was around 10% higher in Pakistani children compared with White British children. A similar pattern was also observed for individual vaccinations (see Supplementary table S2), with the exception of the DTaP/IPV booster at 5 years, for which 96.3% Pakistani and 94.5% White British children were vaccinated, and to a lesser extent the Hib/MenC booster at 2 years (95.5% vs. 89.8% for Pakistani and White British children, respectively). The proportion of children unimmunized for each vaccine was consistently higher in White British compared with Pakistani children.
Table 1.
Participant characteristics overall and by ethnic group
| Maternal characteristics | All (N = 6977) | White British (N = 3060) | Pakistani (N = 3917) | P-value* |
|---|---|---|---|---|
| Age (years) | ||||
| <20 | 512 (7.3) | 383 (12.5) | 129 (3.3) | <0.001 |
| 20–24 | 1897 (27.2) | 851 (27.8) | 1046 (26.7) | |
| 25–29 | 2247 (32.2) | 887 (29.0) | 1360 (34.7) | |
| 30–34 | 1472 (21.1) | 568 (18.6) | 904 (23.1) | |
| 35+ | 849 (12.2) | 371 (12.1) | 478 (12.2) | |
| Single parent | ||||
| No | 5820 (83.4) | 2144 (70.1) | 3676 (93.9) | <0.001 |
| Yes | 1157 (16.6) | 916 (29.9) | 241 (6.2) | |
| Maternal education | ||||
| Less than degree level | 5513 (79.0) | 2515 (82.2) | 2998 (76.5) | <0.001 |
| Degree level | 1464 (21.0) | 545 (17.8) | 919 (23.5) | |
| Smoked during pregnancy | ||||
| No | 5786 (82.9) | 1996 (65.2) | 3790 (96.8) | <0.001 |
| Yes | 1191 (17.1) | 1064 (34.8) | 127 (3.2) | |
| In receipt of means-tested benefits | ||||
| No | 3847 (55.1) | 1833 (59.9) | 2014 (51.4) | <0.001 |
| Yes | 3130 (44.9) | 1227 (40.1) | 1903 (48.6) | |
| Number of other children in household | ||||
| 0 | 2055 (29.4) | 1293 (42.2) | 762 (19.5) | <0.001 |
| 1 | 2145 (30.8) | 1091 (35.7) | 1054 (26.9) | |
| 2–3 | 2271 (32.6) | 613 (20.1) | 1658 (42.3) | |
| 4+ | 506 (7.2) | 63 (2.1) | 443 (11.3) | |
| Mother’s place of birth | ||||
| Born in UK | 4622 (66.3) | 2991 (97.8) | 1631 (41.6) | <0.001 |
| Born outside UK | 2355 (33.7) | 69 (2.2) | 2286 (58.4) | |
| Child’s year of birth | ||||
| 2007–08 | 1335 (19.1) | 519 (17.0) | 816 (20.8) | <0.001 |
| 2008–09 | 1550 (22.2) | 618 (20.2) | 932 (23.8) | |
| 2009–10 | 2096 (30.0) | 943 (30.8) | 1153 (29.4) | |
| 2010–11 | 1996 (28.6) | 980 (32.0) | 1016 (25.9) |
Values are expressed as n (%).
P values for difference between White British and Pakistani participants tested using chi-squared test.
Table 2.
Overall immunization status at 1, 2 and 5 years of age
| White British (N = 3060) | Pakistani (N = 3917) | |
|---|---|---|
| 1 year of age | ||
| Not immunized | 268 (8.8) | 36 (0.9) |
| Partially immunized | 199 (6.5) | 184 (4.7) |
| Fully immunized | 2593 (84.7) | 3697 (94.4) |
| 2 years of age | ||
| Not immunized | 103 (3.4) | 19 (0.5) |
| Partially immunized | 550 (18.0) | 378 (9.7) |
| Fully immunized | 2407 (78.7) | 3520 (89.9) |
| 5 years of age | ||
| Not immunized | <5 (0.0) | 0 (0.0) |
| Partially immunized | 718 (23.5) | 491 (12.5) |
| Fully immunized | 2341 (76.5) | 3426 (87.5) |
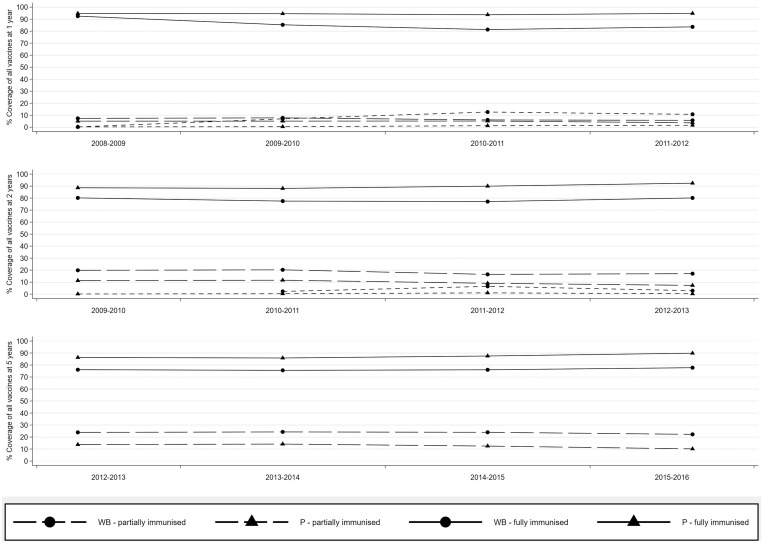
Vaccination uptake varied by year (see figure 1). The proportion of children fully immunized at age 1 was similar in both ethnic groups in 2008–09 at around 94% but fell in White British children in 2009–10 resulting in a 10% disparity between the ethnic groups. By age 2, in 2009–10, 89% of Pakistani children were fully immunized compared with 80% of White British children, and this ethnic difference increased over subsequent years. Similar patterns were observed at 5 years of age. Uptake of individual vaccines by year is presented in Supplementary figure S2a (coverage at 1 year), figure S2b (coverage at 2 years) and figure S2c (coverage at 5 years). A similar trend was seen for the majority of vaccines with uptake being consistently lower in White British children compared with Pakistani children, with the exception of the DTaP/IPV booster at 5 years, whereby 2014–15 uptake in the two ethnic groups was comparable.
Figure 1.
Coverage of all vaccinations at 1, 2 and 5 years of age
The unadjusted analyses of factors examined for association with partial immunization at 1, 2 and 5 years are presented in Supplementary table S3 and results of the final models are in table 3. Factors associated with an increased risk of partial immunization were mostly related to social and economic environment including: smoking during pregnancy at 2 and 5 years in White British children only; single parenthood at all ages in Pakistani children and at 1 year in White British children; receipt of means-tested benefits for Pakistani children at age 5, and increasing number of children in the household for all ages and in both ethnic groups, although this varied by the number of children. Pakistani children were more likely to be fully immunized if their mother was born outside the UK, whereas the converse was observed in the children of foreign-born White British mothers.
Table 3.
Backward stepwise multi-level Poisson regression for factors associated with partial immunization at 1, 2 and 5 years of age by ethnic group
| 1 year | 2 years | 5 years | ||||
|---|---|---|---|---|---|---|
| ARR (95% CI) | ARR (95% CI) | ARR (95% CI) | ||||
| White British (%) | Pakistani (%) | White British (%) | Pakistani (%) | White British (%) | Pakistani (%) | |
| Smoking during pregnancy | ||||||
| No | NS | NS | 1.00 | NS | 1.00 | NS |
| Yes | 1.25 (1.05–1.50) | 1.22 (1.04–1.43) | ||||
| In receipt of means-tested benefits | ||||||
| No | NS | NS | NS | NS | NS | 1.00 |
| Yes | 1.25 (1.03–1.51) | |||||
| Single parent | ||||||
| No | 1.00 | 1.00 | NS | 1.00 | NS | 1.00 |
| Yes | 1.41 (1.05–1.89) | 1.99 (1.24–3.17) | 1.71 (1.21–2.42) | 1.56 (1.13–2.14) | ||
| No. children in household | ||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1 | 1.58 (1.04–2.12) | 1.01 (0.54–1.61) | 1.35 (1.10–1.65) | 1.06 (0.76–1.47) | 1.26 (1.05–1.50) | 0.97 (0.72–1.29) |
| 2–3 | 2.43 (1.45–3.01) | 1.21 (0.80–1.83) | 1.96 (1.58–2.43) | 1.34 (1.00–1.80) | 1.86 (1.54–2.24) | 1.17 (0.90–1.52) |
| 4 | 5.87 (2.90–9.92) | 1.76 (1.06–2.92) | 3.34 (2.06–5.41) | 1.77 (1.23–2.54) | 2.80 (1.74–4.50) | 1.42 (1.02–1.98) |
| UK born | ||||||
| No | NS | 0.70 (0.52–0.94) | 1.65 (1.06–2.57) | 0.77 (0.63–0.95) | 1.55 (1.02–2.36) | 0.80 (0.67–0.97) |
| Yes | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
Values are adjusted risk ratios (ARRs) with 95% confidence intervals (95% CI). Fully immunized is the baseline.
Discussion
Main findings of the study
We found that compared with White British children, vaccination uptake was greater in Pakistani children at all ages and for each year examined in this study. Children of foreign-born Pakistani mothers were more likely to be fully immunized than Pakistani children whose mothers were born in the UK but children of foreign-born White British women were more likely to be partially immunized compared with UK-born White British women. Partial immunization was associated with social and economic factors including smoking during pregnancy (White British only), receipt of means-tested benefits, single parenthood and increasing number of children living in the household in both ethnic groups, though the risk differed according to the age of child and ethnicity, being especially strong in White British children. We found no association between maternal education with vaccination uptake.
What is already known on this topic
Our findings support other UK studies that have found higher immunization rates in Asian children6,11,12 compared with white children. Several UK studies have also found that the children of lone parents were less likely to be fully immunized but as these did not consider ethnicity it is not known if this association is present across different ethnic groups.3,4,13 Smoking was significantly associated with partial immunization in White British women when their children were 2 and 5 years old, supporting findings from a previous UK study.4 Smoking is more prevalent among lower socio-economic groups thus this finding may reflect the lower socio-economic status of some participants.14 A number of other studies have reported an association between larger family size and lower vaccine uptake,3,4,6 including one UK study which examined vaccine uptake amongst different ethnicities and observed a lower uptake of DTaP at 16 weeks and MMR at 2 years in White British women with increasing parity that was not evident in Pakistani or Black ethnic groups.7 Uptake according to maternal place of birth has been examined by studies in the USA and Netherlands which have found that foreign-born women were less likely to complete their vaccination schedule.8,9
What this study adds
To our knowledge, this is the first UK study to assess longitudinal immunization status during the first 5 years of life in a bi-ethnic cohort. The key strengths of our study are its large size and linkage of research data with primary care records, which has enabled us to accurately examine vaccination uptake through recorded clinic visits rather than rely on parental report.
This study has demonstrated important ethnic differences in vaccination uptake in UK White British and Pakistani ethnic groups. Whilst White British women tended to have a poorer socio-economic profile, single parenthood and increasing number of children in the household were associated with uptake in both ethnic groups. However, we did find that country of birth had opposite effects in the ethnic groups, with children of foreign-born Pakistani women more likely to be fully immunized and those of foreign-born White British women more commonly partially immunized. Although information on place of birth was not available for a third of women in the foreign-born White British group, almost all foreign-born Pakistani women were born in Pakistan. One possible explanation for higher uptake in South Asian children is that parents, families and friends with links to South Asia may have seen first-hand the serious consequences of vaccine preventable diseases in their country of origin.12 A further explanation may be that there is a sizeable Pakistani community in Bradford which now comprises third and fourth generation UK Pakistani families; as such, access to and use of services is well established.15
We found that vaccination uptake differed by year, particularly in White British children, and it is important that this is recognized in monitoring and responding to changes in vaccine coverage by those overseeing immunization programmes. Acceptability of vaccinations can be profoundly influenced by misleading or incorrect scientific findings and subsequent media coverage, e.g. the 1998 article which reported findings linking the MMR vaccination to autism and bowel disorders,16 resulting in a dramatic decline in MMR uptake. However, we are not aware of any adverse reports regarding scheduled vaccinations during the time-period under study. Change in practice is often associated with variation in vaccine uptake. For example, we observed a decline in full coverage of DTaP/IPV/Hib, MenC and PCV between 2008–09 and 2010–11, followed by an increase in 2011–12. Previous to November 2011, the Hib/MenC vaccine was given separately to MMR and PCV, but this subsequently changed to all three vaccines being given in at the same visit. In addition, there may be individual practice or local service level factors that have affected individual years in this study but we have no clear explanation for the difference.
Overall, these analyses indicate there are social differentials in vaccination uptake, and that the factors influencing non-compliance vary by ethnic group, particularly according to the mother’s country of birth and the age of the child. White British women experiencing deprivation and white foreign-born mothers appear to be particularly affected, implying that current population-wide health promotion strategies and service delivery may not be appropriate for some population groups. It is, therefore, important to better understand the factors that prevent or encourage immunization in those from different cultural and ethnic backgrounds so that targeted interventions to improve childhood immunization rates can be developed and delivered to those families and communities where uptake is generally lower.
Limitations of this study
A possible limitation of our study is that the primary care records may be incomplete or not of sufficient quality; in particular, trends in vaccination coverage may reflect changes in data quality. However, we observed consistently higher uptake rates in Pakistani children in Bradford, suggesting good quality coding, and it is unlikely that this would have been any different for White British children. We could not link 74 children to their primary care record and also excluded children for whom we did not have complete primary care records from birth to 5 years of age to ensure completeness of data. The reasons for gaps in GP registration are unknown but it may reflect address changes, which in turn may be driven by socio-economic circumstances that could influence vaccination uptake in either direction. Further, we found that some characteristics of children for whom we had baseline information for but who were excluded from the analysis due to incomplete GP records differed from those who were included (see Supplementary table S4). In both ethnic groups, those excluded were more likely to have mothers who were educated to degree level and less likely to be in receipt of means-tested benefits. Mothers of excluded White British children were less likely to be single parent’s and less likely to smoke than those included, whereas mothers of Pakistani children were more likely to smoke and to have fewer other children in their household. As socio-economic factors are known to be associated with vaccination uptake, it is possible that these exclusions underestimated vaccination uptake, particularly in White British women, though it is unlikely that this accounts for the wide differences. There were no differences in mother’s place of birth between those excluded and included in either ethnic group.
We did not undertake any qualitative research and therefore do not have information for individuals on other factors known to affect vaccination uptake, e.g. health promotions, safety concerns etc. A qualitative study of individuals from different ethnic backgrounds in parallel with a quantitative analysis of current vaccination uptake would enable a more holistic exploration of these differences and could contribute to a better understanding of the reasons behind these ethnic disparities. As we looked at two distinct ethnic groups, our findings may not be generalizable to other South Asian or white European populations.
Supplementary Material
Acknowledgements
Born in Bradford is only possible because of the enthusiasm and commitment of all the children and parents in Born in Bradford. We thank all the participants, health professionals and researchers who have made Born in Bradford happen. We gratefully acknowledge the contribution of TPP and the TPP ResearchOne team in completing study participant matching to GP primary care records and in providing ongoing informatics support.
Funding
BiB receives core infrastructure funding from the Wellcome Trust (WT101597MA) and a joint grant from the UK Medical Research Council (MRC) and Economic and Social Science Research Council (ESRC) (MR/N024397/1).
Conflict of interest: None declared.
Key points
Children of Pakistani origin had a greater uptake of childhood vaccinations at 1, 2 and 5 years of age compared with White British children.
Children of foreign-born White British women were more likely to be partially immunized compared with UK-born White British women.
Children of foreign-born Pakistani women were more likely to be fully immunized compared with Pakistani women born in the UK.
Poorer socio-economic circumstances were risk factors for partial immunization.
Targeted interventions to improve childhood immunization rates should be developed for populations with different cultural and ethnic backgrounds.
References
- 1. John TJ, Samuel R. Herd immunity and herd effect: new insights and definitions. Eur J Epidemiol 2000;16:601–6. [DOI] [PubMed] [Google Scholar]
- 2. Public Health England The Green Book: Immunisation Against Infectious Disease, 2013. https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book.
- 3. Pearce A, Law C, Elliman D, et al. Factors associated with uptake of measles, mumps, and rubella vaccine (MMR) and use of single antigen vaccines in a contemporary UK cohort: prospective cohort study. BMJ 2008;336:754–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Samad L, Tate AR, Dezateux C, et al. Differences in risk factors for partial and no immunisation in the first year of life: prospective cohort study. BMJ 2006;332:1312–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hardelid P, Rait G, Gilbert R, et al. Factors associated with influenza vaccine uptake during a universal vaccination programme of preschool children in England and Wales: a cohort study. J Epidemiol Community Health 2016;70:1082–7. [DOI] [PubMed] [Google Scholar]
- 6. Mixer RE, Jamrozik K, Newsom D. Ethnicity as a correlate of the uptake of the first dose of mumps, measles and rubella vaccine. J Epidemiol Community Health 2007;61:797–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Baker D, Garrow A, Shiels C. Inequalities in immunisation and breast feeding in an ethnically diverse urban area: cross-sectional study in Manchester, UK. J Epidemiol Community Health 2011;65:346–52. [DOI] [PubMed] [Google Scholar]
- 8. van Lier A, van de Kassteele J, de Hoogh P, et al. Vaccine uptake determinants in The Netherlands. Eur J Public Health 2014;24:304–9. [DOI] [PubMed] [Google Scholar]
- 9. Buelow VH, Van Hook J. Timely immunization series completion among children of immigrants. J Immigrant Minority Health 2008;10:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wright J, Small N, Raynor P, et al. ; Born in Bradford Scientific Collaborators Group. Cohort profile: The Born in Bradford multi-ethnic family cohort study. Int J Epidemiol 2013;42:978–91. [DOI] [PubMed] [Google Scholar]
- 11. Bhopal RS, Samim AK. Immunization uptake of Glasgow Asian children: paradoxical benefit of communication barriers? Community Med 1988;10: 215–20. [DOI] [PubMed] [Google Scholar]
- 12. Hawker JI, Olowokure B, Wood AL, et al. Widening inequalities in MMR vaccine uptake rates among ethnic groups in an urban area of the UK during a period of vaccine controversy (1994-2000). Vaccine 2007;25:7516–9. [DOI] [PubMed] [Google Scholar]
- 13. Sharland M, Atkinson P, Maguire H, et al. Lone parent families are an independent risk factor for lower rates of childhood immunisation in London. Commun Dis Rep CDR Rev 1997;7: R169–72. [PubMed] [Google Scholar]
- 14.ONS. Adult Smoking Habits in the UK:2018. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2018#characteristics-of-current-cigarette-smokers-in-the-uk (19 December 2019, date last accessed).
- 15. Wagner KS, van Wijgerden JCJ, Andrews N, et al. Childhood vaccination coverage by ethnicity within London between 2006/2007 and 2010/2011. Arch Dis Child 2014;99:348–53. [DOI] [PubMed] [Google Scholar]
- 16. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998;351:637–41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.