Abstract
Aim:
We investigated the association between acculturation strategies and cardiometabolic risk among South Asian(SA) immigrants in the US.
Methods:
In this cross-sectional analysis of data from 849 SA participants in the Mediators of Atherosclerosis in SAs Living in America (MASALA), we performed multidimensional measures of acculturation to categorize the participants into three acculturation classes: separation(preference for SA culture), assimilation(preference for US culture), and integration(similar preference for both cultures). Differences in glycemic indices, blood pressure, lipid parameters and body composition by acculturation strategy were examined.
Results:
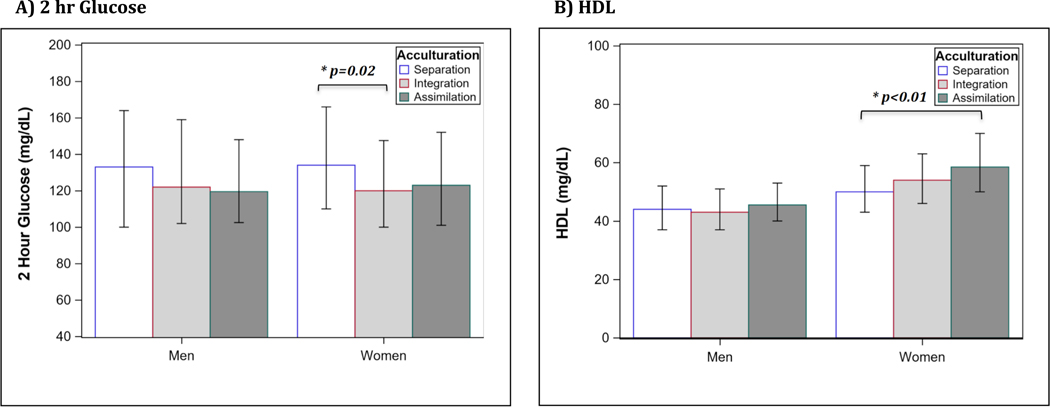
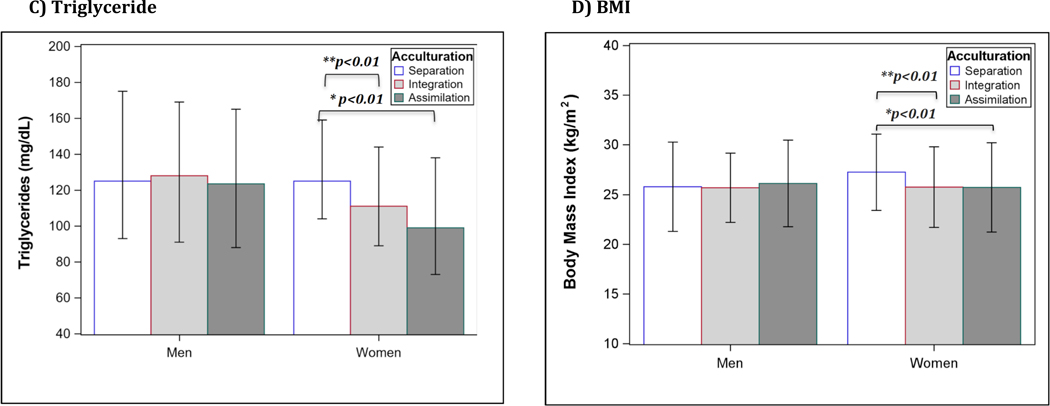
Women in the integration class had the lowest prevalence of diabetes (16.4%), prediabetes (29.7%), fasting and 2-hr glucose compared to women in the separation class with the highest prevalence of diabetes (29.3%), prediabetes (31.5%), fasting and 2-hr glucose and 2-hr insulin (all p<0.05). Women in the assimilation class had significantly lower triglycerides, BMI, and waist circumference and higher HDL compared to women in the separation class after adjusting for age, study site, and years in the US. After additionally accounting for socioeconomic/lifestyle factors, women in the assimilation class had significantly lower triglyceride and higher HDL levels compared to women in the separation class (p<0.01). There was no significant association between acculturation strategies and cardiometabolic risk in SA men.
Conclusion:
SA women who employed an assimilation or integration strategy had a more favorable cardiometabolic profile compared to women using a separation strategy. Future research should investigate the behavioral and psychosocial pathways linking acculturation strategies with cardiometabolic health to inform preventive interventions among SAs living in America.
Keywords: Acculturation, cardiovascular disease risk factors, cardiometabolic health, immigration, assimilation, integration, separation
INTRODUCTION
The prevalence of cardiovascular disease (CVD) risk factors including diabetes, hypertension, dyslipidemia, and obesity is rising at alarming rates in South Asia.1–3 Immigrants from South Asian (SA) countries (i.e. India, Pakistan, Bangladesh, Sri Lanka, and Nepal) became the fastest-growing ethnic group in the United States (US) between 2000 and 2010, and there are close to 4.9 million SAs in the US.4, 5 South Asian immigrants have a higher prevalence of CVD risk factors and greater cardiovascular mortality compared to local populations and immigrants of other ethnic groups. 6–11 Furthermore, SA immigrants develop cardiometabolic diseases at a younger age and a lower BMI than individuals of other ethnic groups.10, 12, 13
Similar to other immigrants, South Asians experience a process of acculturation whereby changes in cultural and psychosocial behaviors take place as they interact with members of different cultural groups and social structures in the host country and adapt to a new culture and environment.14 The impact of acculturation on cardiometabolic health has been examined among various ethnic groups, but prior work has been limited by its overreliance on simple unidimensional proxy measures of acculturation (e.g. English fluency and years in the US) which do not account for the multiple dimensions and complex nature of the impact of acculturation on health. Using these proxy measures, greater acculturation (i.e. assimilation) has been associated with an increased prevalence of various CVD risk factors in Japanese, Chinese, Hispanic, European, and Black immigrants in the US.15–21 The worse cardiometabolic profile in those who migrated from low-income to high-income countries compared to those who remained in their low-income home countries has been attributed to possibly adopting unhealthy behaviors related to dietary pattern (e.g. high-carbohydrate and/or fat intake), physical activity (e.g. sedentary life), psychosocial factors (e.g. depression or chronic stress), or combination of more than one of these factors that are more prevalent in most high-income countries.22–24 For example, a higher consumption of animal protein, animal and vegetable fat, and simple carbohydrates along with lower physical activity have been found in Japanese immigrants in the US compared to Japanese living in Hiroshima.21 These lifestyle changes were associated with unfavorable changes in lipids, blood pressure, BMI, and carotid intima-media thickness in this study. Acculturation, however, is widely variable among immigrants and depends in part on the differences in health behaviors between the host country and country of origin. It is possible that some immigrants may adopt healthier behaviors from the host country that would lower their risk of CVD.25–27 Hence, the use of a multidimensional model of acculturation is needed to better characterize the impact of acculturation on cardiometabolic health and capture domains of this process that may not be apparent with the use of the traditional proxy measures of acculturation. Moreover, sex differences in the degree of assimilation to the host culture after migration, as well as heterogeneity by sex in the association of acculturation and CVD risk factors have been reported in various ethnic groups.20, 28–30
In this study, we sought to examine the association between acculturation strategies, using several cultural and behavioral indicators of acculturation, and CVD risk factors among SA immigrants in the US. We used data from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study that utilized twelve indicators of acculturation to identify three acculturation strategies: assimilation, integration, and separation.31 We hypothesized that by potentially adopting unhealthy behaviors that are prevalent in the US, SA immigrants using the assimilation and integration strategies (i.e. stronger preference of US culture over SA culture) would have a higher prevalence of CVD risk factors than South Asians using the separation strategy (i.e. stronger preference of SA culture over US culture). We also hypothesized that the association between acculturation and CVD risk factors would vary by sex among SA immigrants.
METHODS
Study design and participants
We conducted a cross-sectional analysis of data from the MASALA study, a community-based cohort of SA men and women from two clinical sites (San Francisco Bay Area at the University of California, San Francisco (UCSF) and the greater Chicago area at Northwestern University (NWU)). MASALA enrolled 906 participants (98% foreign-born) between October 2010 and March 2013. The detailed study design and objectives of the MASALA study have been previously described.32 In brief, individuals were eligible for the MASALA study if they were aged 40 to 84 years, self-identified as having SA ancestry (defined as having 3 or more grandparents born in India, Pakistan, Nepal, Bangladesh, or Sri Lanka), and free from physician-diagnosed CVD. All visits were conducted by trained bilingual study staff and all consent forms were translated into Hindi and Urdu. The institutional review boards at the University of California, San Francisco (UCSF) and Northwestern University (NWU) approved the MASALA study protocol, and all study participants provided written informed consent.
For this analysis, we excluded 31 individuals who were missing data on one or more variables used in the acculturation analysis, 7 individuals with missing data on diabetes status, and 19 individuals who were born in the US (final n=849).
Acculturation strategies
Using twelve indicators of acculturation, SA immigrants in the MASALA study have been previously shown to use one of the following three acculturation strategies: Separation (preference of SA culture over US culture); Integration (similar preference for SA and US cultures); and Assimilation (preference of US culture over SA culture). A detailed description of the methodology used to identify the acculturation strategies employed by MASALA participants has been previously published. 31 In brief, respondents were asked to report how much they wish the following traditions from South Asia would be practiced in America (1 = absolutely- 5 = not at all): (1) performing religious ceremonies or rituals; (2) serving SA sweets for ceremonies or rituals; (3) fasting on specific occasions; (4) living in a joint family; (5) having an arranged marriage; (6) having a staple diet of chapatis, rice, daal, vegetables, and yogurt; and (7) using spices for healing and health. Next, respondents were asked to report how often they fast (1= two or three times per week- 6= almost never or never), what foods they normally eat at home and in restaurants (1= only SA food- 6= never eat at home/in restaurants), how often their family shops at SA grocery stores or markets (1= two or three times per week- 5= almost never or never), and which country or culture most of their friends belong to (1= only SA- 5= only other ethnic groups). Latent class analysis (LCA) was used to identify acculturation strategies: “separation” having a high preference for SA culture, “assimilation” having the least preference, and “integration” having an intermediate preference.31
Assessment of CVD risk factors
Participants were assessed for traditional CVD risk factors including dysglycemia, dyslipidemia, hypertension, and obesity.
Blood samples were collected after a 12-hour overnight fast. Total cholesterol, triglyceride, and high-density lipoprotein (HDL) cholesterol levels were analyzed by enzymatic methods, and low-density lipoprotein (LDL) cholesterol concentrations were calculated. Dyslipidemia was defined as having a total cholesterol of ≥200 mg/dl, triglyceride of ≥150 mg/dl, HDL<40 mg/dl in men or <50 mg/dl in women, or using a cholesterol-lowering medication. A 75-g oral glucose tolerance test was performed for participants who were not taking glucose-lowering medications and blood samples were drawn 2 hours after the glucose challenge. Fasting plasma glucose (FPG) and 2-hour post challenge glucose were measured using a hexokinase method (Quest Labs, San Jose, CA). Fasting serum insulin was measured by the sandwich immunoassay method (Elecsys 2010, Roche Diagnostics). The homeostasis model assessment (HOMA)-IR was used to measure IR and calculated as [Insulin0 (μIU/mL)/Glucose0 (mmol/L)/ 22.5], and HOMA-b was used to measure β-cell function and was calculated as [20 x Insulin0(μIU/mL)/Glucose0(mmol/L) - 3.5].33 We excluded participants taking glucose-lowering medications from the analyses of HOMA-IR and HOMA-B. Diabetes and prediabetes were defined according to the American Diabetes Association guidelines.34
Three seated blood pressure measurements were obtained after resting in a seated position for 5 minutes as previously reported.32Hypertension was defined as a systolic blood pressure of ≥140 mmHg or diastolic blood pressure ≥90 mmHg or use of a blood pressure lowering medication.
Participant weight and waist and hip circumferences were measured and body mass index (BMI) was calculated as previously described. 32 Obesity was defined according to the WHO Asian BMI cut-off point of BMI ≥27.5 kg/m2.35
Abdominal visceral, subcutaneous, and intermuscular fat areas were calculated using abdominal computed tomography scans (CT, Philips Medical Systems, Andover, MA, USA; Toshiba Medical Systems, Tustin, CA, USA; Siemens Medical Solution, Malvern, PA, USA) as previously reported.36, 37 The relationship of hepatic fat content and hepatic attenuation is an inverse one with higher hepatic attenuation implying lower fat content.
Covariates
All participants completed a detailed questionnaire to ascertain sociodemographic information, medical history, family history, medication use, cultural practices, and behaviors. Dietary intake over the previous year was assessed using the Study of Health Assessment and Risk in Ethnic Groups (SHARE) food frequency questionnaire, which was created and validated among SAs in Canada.38 Physical activity was assessed using the Typical Week’s Physical Activity Questionnaire.39 Total physical activity included intentional exercise, occupational activities, volunteer activities, household chores, yardwork, child/adult care, transportation, and leisure activities. Intentional exercise included walking for exercise, dancing, team sports, dual sports, individual activities, moderate conditioning activities, and heavy conditioning activities. Tobacco use and alcohol consumption were determined by questionnaires. Several psychosocial scales were administered including the Center for Epidemiologic Studies Depression Scale (CES-D).40
Statistical Analyses
Variable distributions were examined for normality using the Shapiro-Wilk test and visual examination of histograms. The non-normally distributed variables of FPG, 2-hour glucose, HDL, and triglyceride were presented as medians and interquartile ranges (IQR) and HOMA-IR was appropriately transformed. Baseline characteristics were compared by acculturation class using pairwise comparison (i.e. separation vs integration and separation vs assimilation). Participant characteristics were stratified by sex and were compared using t-tests for continuous variables and chi-squared tests of homogeneity for categorical variables. Non-normally distributed variables were compared using Kruskal–Wallis test. Multivariable linear regression analyses were used to determine which acculturation strategy classes were associated with the various CVD risk factors in unadjusted models, after controlling for age and study site (Model 1), additionally adjusting for socioeconomic factors such as education level, family income, employment, country of birth, marital status, religious affiliation, years lived in the US, and medical insurance (Model 2), and after additionally adjusting for behavioral and psychosocial factors such as total physical activity, total exercise, total caloric intake, depression, smoking, and alcohol status (Model 3).
We tested the effect modification of sex on the relationship between acculturation and CVD risk factors by including an interaction term (sex × acculturation class). The unadjusted interaction terms were significant for HDL, triglyceride, and BMI; as well as the fully adjusted interaction terms for HDL and triglyceride (all p values <0.05). Therefore, all data are presented stratified by sex. In addition, we performed a sensitivity analysis to evaluate the association between length of residence in the US and prevalence of CVD risk factors as this is a commonly used proxy measure of acculturation in literature. All significance testing was 2-tailed with α of 0.05, and data were analyzed using SAS (version 9.4; SAS Institute Inc, Cary, NC).
RESULTS
Sociodemographic and lifestyle-related factors by acculturation class
The study population included 849 participants, of whom 45.8% were women and 23.0% were in the separation class, 54.4% in the integration class, and 22.6% in the assimilation class. Majority of the study participants spoke English well or very well (87.2%), were born in India (85.3%) and were employed (70.4%). Table 1 shows the characteristics of the study participants by sex and acculturation class. Compared to those in the separation class, men and women in the assimilation and integration classes had a longer residence in the US; more education and higher income; were more likely to have insurance and speak English well or very well, and had lower CES-D scores. Men and women in the assimilation class had the highest total exercise per week and lowest caloric intake; whereas those in the separation class had the lowest total exercise per week and highest caloric intake.
Table 1:
Participant Characteristics by Acculturation Class and Sex (n=849)
| All n=849 | Men (n=460) | Women (n=389) | |||||
|---|---|---|---|---|---|---|---|
| Characteristic | Separation n=103 (22%) | Integration n=267 (58%) | Assimilation n =90 (20%) | Separation n=92 (24%) | Integration n=195 (50%) | Assimilation n=102 (26%) | |
| Sociodemographic Characteristics | |||||||
| Age, mean (SD), years | 55.4 (9.3) | 56.7 (9.7) | 56.1 (9.8) | 55.7 (10.3) | 54.4 (9.2) | 54.2 (8.2) | 54.9 (8.8) |
| NWU study site | 382 (45.0) | 63 (61.2) | 127 (47.6) a | 31 (34.4) b | 48 (52.2) | 78 (40.0) | 35 (34.3) b |
| Married, n (%) | 780 (91.9) | 103 (100) | 259 (97.0) | 83 (92.2) b | 77 (83.7) | 174 (89.2) | 84 (82.4) |
| Religion, n (%) | |||||||
| Hinduism/Jainism | 633 (74.6) | 72 (69.9) | 212 (79.4) a | 59 (65.6) b | 60 (65.2) | 163 (83.6) a | 67 (65.7) b |
| Other religion | 168 (19.8) | 30 (29.1) | 47 (17.6) a | 12 (13.3) b | 32 (34.8) | 31 (15.9) a | 16 (15.7) b |
| No religious affiliation | 48 (5.7) | 1 (1.0) | 8 (3.0) a | 19 (21.1) b | 0 | 1 (0.5) a | 19 (18.6) b |
| Birthplace, n (%) | |||||||
| India | 724 (85.3) | 81 (78.6) | 232 (86.9) a | 80 (88.9) b | 73 (79.3) | 171 (87.7) a | 87 (85.3) b |
| Other | 125 (14.7) | 22 (21.4) | 35 (13.1) a | 10 (11.1) b | 19 (20.7) | 24 (12.3) a | 15 (14.7) b |
| Years lived in the US, mean (SD) | 27.0 (10.8) | 24.5 (11.3) | 27.0 (10.4) a | 31.8 (10.4) b | 22.6 (10.7) | 26.8 (10.4) a | 29.9 (10.5) b |
| Percent of life in US, mean (SD), % | 48.5 (16.5) | 43.4 (18.6) | 47.8 (15.1) a | 56.9 (15.4) b | 41.7 (17.5) | 48.8 (15.8) a | 53.6 (15.0) b |
| English language proficiency, n (%) | |||||||
| Speak English poorly or fairly | 109 (12.8) | 30 (29.1) | 17 (6.4) a | 1 (1.1) b | 38 (41.3) | 20 (10.3) a | 3 (2.9) b |
| Speak English well or very well | 740 (87.2) | 73 (70.9) | 250 (93.6) a | 89 (98.9) b | 54 (58.7) | 175 (89.7) a | 99 (97.1) b |
| Education, n (%) | |||||||
| Less than bachelor’s degree | 97 (11.4) | 19 (18.4) | 22 (8.2) a | 5 (5.5) b | 32 (34.8) | 11 (5.6) a | 8 (7.8) b |
| Bachelor’s degree | 247 (29.1) | 39 (37.9) | 60 (22.5) a | 16 (17.8) b | 30 (32.6) | 77 (39.5) a | 25 (24.5) b |
| More than bachelor’s degree | 505 (59.5) | 45 (43.7) | 185 (69.3) a | 69 (76.7) b | 30 (32.6) | 107 (54.9) a | 69 (67.7) b |
| Annual family income, n (%) | |||||||
| <$100,000 | 314 (37.0) | 63 (61.2) | 93 (34.8) a | 15 (16.7) b | 61 (66.3) | 55 (28.2) a | 27 (26.5) b |
| $100,000 to $200,000 | 291 (34.3) | 21 (20.4) | 107 (40.1) a | 35 (38.9) b | 18 (19.6) | 79 (40.5) a | 31 (30.4) b |
| >$200,000 | 244 (28.7) | 19 (18.4) | 67 (25.1) a | 40 (44.4) b | 13 (14.1) | 61 (31.3) a | 44 (43.1) b |
| Insurance status, n (%) | |||||||
| Insured | 780 (91.9) | 83 (80.6) | 249 (93.3) a | 90 (100) b | 75 (81.5) | 183 (93.8) a | 100 (98.0) b |
| Not Insured | 69 (8.1) | 20 (19.4) | 18 (6.7) a | 0 b | 17 (18.5) | 12 (6.2) a | 2 (2.0) b |
| Occupation, n (%) | |||||||
| Unemployed | 135 (15.9) | 7 (6.8) | 11 (4.1) | 2 (2.2) | 35 (38.0) | 58 (29.7) | 22 (21.6) b |
| Employed | 598 (70.4) | 78 (75.7) | 215 (80.5) | 75 (83.3) | 49 (53.3) | 118 (60.5) | 63 (61.8) b |
| Retired | 116 (13.7) | 18 (17.5) | 41 (15.4) | 13 (14.4) | 8 (8.7) | 19 (9.7) | 17 (16.7) b |
| CES-D depression scale, mean (SD) | 7.7 (7.1) | 8.8 (7.4) | 7.1 (6.6) a | 5.1 (4.5) b | 9.9 (8.7) | 8.1 (7.3) | 7.1 (6.8) b |
| Lifestyle and Behavioral Factors | |||||||
| Total physical activity, mean (SD), MET-min/week | 10057 (4031) | 10396 (4658) | 9518 (3410) | 9410 (2848) | 10680 (4706) | 10452 (4317) | 10382 (4353) |
| Total exercise, median (IQR), MET-min/week | 945 (1523) | 705 (1620) | 1020 (1418) | 1365 (1755) b | 630 (1076) | 825 (1605) a | 1260 (1845) b |
| Total caloric intake, median (IQR), Kcal | 1613 (654) | 1747 (583) | 1705 (700) | 1513 (642) b | 1573 (537) | 1527 (564) | 1454 (627) |
| Smoking, n (%) | |||||||
| Never | 701 (82.6) | 76 (73.8) | 188 (70.4) | 61 (67.8) | 91 (98.9) | 191 (97.9) | 94 (92.2) |
| Former | 119 (14.0) | 24 (23.3) | 63 (23.6) | 23 (25.6) | 1 (1.1) | 2 (1.0) | 6 (5.9) |
| Current | 29 (3.4) | 3 (2.9) | 16 (6.0) | 6 (6.7) | 0 | 2 (1.0) | 2 (2.0) |
| Alcohol use ≥1 drink/week, n (%) | 277 (32.6) | 23 (22.3) | 116 (43.4) a | 64 (71.1) b | 5 (5.4) | 32 (16.4) a | 37 (36.3) b |
Abbreviations: NWU, Northwestern University.
Differences by acculturation class were examined using t tests and pairwise comparison (i.e. separation vs integration and separation vs assimilation); categorical variables were examined using chi-squared tests of homogeneity. Testing was performed on log transformed variables when necessary to achieve normality.
Statistically significant difference (p value<0.05) between integration and separation classes.
Statistically significant difference (p value<0.05) between assimilation and separation classes.
Cardiovascular disease risk factors by acculturation class
Glycemic indices:
Women in the integration class had the lowest prevalence of diabetes (16.4%) and prediabetes (29.7%) compared to women in the separation class who had the highest prevalence of diabetes (29.3%) and prediabetes (31.5%). Similarly, women in the integration class had significantly lower 2-hr glucose and insulin, compared to women in the separation class. Men, however, had no significant differences in any of the glycemic indices by acculturation class (Table 1, Figure 1 A, and Supplementary Figure 1).
Figure 1:
A) 2-hour glucose levels were similar in women in the assimilation class [median (IQR): 123 (51) mg/dl, p=0.09] compared to women in the separation class [134 (56) mg/dl]. *Women in the integration class had significantly lower levels of 2-hour glucose [median (IQR): 120 (47.5) mg/dl, p=0.02] compared to women in the separation class. 2-hour glucose levels were similar in men in the separation, integration, and assimilation classes [median (IQR): 133 (64), 122 (57), and 119.5 (45.5) mg/dl, respectively; all p>0.05]. B) *HDL levels were higher in women in the assimilation group [median (IQR): 58.5 (20) mg/dl, p<0.01] compared to women in the separation class [50 (16) mg/dl]. Women in the integration class had a slightly higher HDL level [median (IQR): 54 (17) mg/dl, p=0.05] compared to women in the separation class. HDL levels were similar in men in the separation, integration, and assimilation classes [median (IQR): 44 (15), 43 (14), and 45.5 (13) mg/dl, respectively; all p>0.05]. C) *Triglyceride levels were lower in women in the assimilation group [median (IQR): 99 (65) mg/dl, p<0.01] compared to women in the separation class [125 (55) mg/dl]. **Women in the integration class also had a lower triglyceride level [111 (55) mg/dl, p<0.01] compared to women in the separation class. Triglyceride levels were similar in men in the separation, integration, and assimilation classes [median (IQR): 125 (82), 128 (78), and 123.5 (77) mg/dl, respectively; all p>0.05]. D) *Significantly lower BMI in women in the assimilation group [mean (SD) 25.7 (4.5) kg/m2, p<0.01] compared to women in the separation class [27.3 (3.8) kg/m2]. **Significantly lower BMI in women in the integration class [25.8 (4.1) kg/m2, p<0.01] compared to women in the separation class. Similar BMI in men in the separation, integration, and assimilation classes [25.8 (4.5), 25.7 (3.5), and 26.1 (4.3) kg/m2, respectively].
Blood pressure:
There were no significant differences in systolic or diastolic blood pressure by acculturation class among men or women (Supplementary Figures 2 A and B).
Lipid parameters:
Triglycerides were significantly lower in women in the assimilation class versus the separation class (median(IQR): 99(65) versus 125(55) mg/dl, p<0.01) and HDL was significantly higher in the assimilation class versus the separation class (median(IQR): 58.5(20) versus 50(16) mg/dl, p<0.01). Similarly, women in the integration class had lower triglyceride and slightly higher HDL levels compared to those in the separation class (p<0.01 and 0.05, respectively). Overall, no significant differences were noted in any of the lipid parameters by acculturation class in men (Figure 1 B, 1 C, and Supplementary Figure 2 C).
Weight and body composition:
The prevalence of obesity was lowest among women in the assimilation class (26.5%), followed by the integration class (28.4%) and the separation class (48.9%) (P<0.01 for both: assimilation versus separation and integration versus separation) (Table 1). Similarly, BMI was significantly lower in women in the assimilation class versus the separation class (p<0.01); and in women in the integration class versus the separation class (p<0.01) (Figure 1 D). Furthermore, women in the assimilation and integration classes had significantly lower hip girth and pericardial fat compared to those in the separation class (Table 1 and Supplementary Figure 3 C). Men, however, had no significant differences in the prevalence of obesity, BMI, hip girth, or body fat composition by acculturation class (Figure 1 D and Supplementary Figure 3 B -D).
Cardiovascular disease risk factors by duration of residence in the US
With the exception of HDL and waist circumference, none of the differences seen in the CVD risk factors by acculturation class was seen when length of residence in the US was used as a proxy measure of acculturation (Supplementary Table 1). There were no significant differences in any of the glycemic indices, triglyceride or LDL levels, blood pressure, BMI, or body composition by length of residence in the US. However, women and men who lived in the US for 20 or more years had higher HDL levels (57±14mg/dl and 46±11mg/dl; respectively) compared to women and men who lived in the US for 10 to 19 years (52±14mg/dl, p<0.01 and 44±11mg/dl, p=0.02; respectively) and compared to those who lived in the US for less than 10 years (52±11mg/dl, p=0.04 and 42±5mg/dl, p=0.21; respectively). The differences in HDL by length of residence in the US were not statistically significant when adjusted for age in men; and only women lived in the US for 20 or more years had a significantly higher age-adjusted HDL levels compared to those who lived in the US for less than 10 years (data not shown).
Multivariable regression analyses
The results of the multivariable regression analyses examining the relationship between the acculturation classes and various CVD risk factors are shown in Tables 2 and 3. Compared to women in the separation class, women in the integration class had significantly lower FPG (−8.9±2.9mg/dl, p<0.01) and 2-hr glucose (−20.3±7.1mg/dl, p<0.01) in the unadjusted model. These differences were attenuated and became non-significant after adjusting for age, study site, years lived in the US, education level, family income, country of birth, marital status, religious affiliation, medical insurance, and employment (Model 2, Table 2). Compared to women in the separation class, women in the assimilation class had significantly lower triglyceride levels [−29.2±7.2 mg/dl, p<0.01] and higher HDL levels [9±1.9mg/dl, p<0.01] in the unadjusted model. These differences remained significant in the fully adjusted Model 3 (Table 2). Finally, compared to women in the separation class, women in the assimilation class had significantly lower waist circumference [−2.9±1.4cm, p=0.04] and BMI [−1.5±0.6 kg/m2, p=0.01] in the unadjusted model. No significant differences by acculturation class were noted in any of the CVD risk factors among men (Table 3).
Table 2:
Cardiovascular Risk Factors and Body Composition by Acculturation Class and Sex (n=849)*
| All n=849 | Men (n=460) | Women (n=389) | |||||
|---|---|---|---|---|---|---|---|
| Characteristic | Separation n=103 (22%) | Integration n=267 (58%) | Assimilation n =90 (20%) | Separation n=92 (24%) | Integration n=195 (50%) | Assimilation n=102 (26%) | |
| Cardiovascular Risk Factors | |||||||
| Glycemic status, n (%) | |||||||
| Normal | 348 (41.0) | 31 (30.1) | 93 (34.8) | 37 (41.1) | 36 (39.1) | 105 (53.8) a | 46 (45.1) |
| Prediabetes | 282 (33.2) | 40 (38.8) | 95 (35.6) | 28 (31.1) | 29 (31.5) | 58 (29.7) a | 32 (31.4) |
| Diabetes | 219 (25.8) | 32 (31.1) | 79 (29.6) | 25 (27.8) | 27 (29.3) | 32 (16.4) a | 24 (23.5) |
| Fasting glucose, median (IQR), mg/dl | 101 (24) | 99 (20) | 97 (26) | 94 (18) | 94 (12) | 95 (15) | |
| Hemoglobin A1C, mean (SD), % | 6.1 (0.9) | 6.3 (1.0) | 6.1 (0.9) | 6.2 (1.0) | 6.2 (1.2) | 5.9 (0.5) | 6.0 (0.7) |
| HOMA-B, mean (SD) | 123.3 (90.2) | 149.4 (151.0) | 117.6 (84.4) | 127.6 (95.6) | 120.1 (68.9) | 122.2 (65.0) | 111.1 (65.5) |
| Fasting insulin, mean (SD), pmol/L | 76.0 (85.0) | 95.2 (117.7) | 82.1 (117.1) | 78.0 (49.4) | 71.1 (41.3) | 63.3 (36.9) | 65.9 (50.8) |
| 2-hr insulin, mean (SD), pmol/L | 721.9 (628.3) | 831.5 (518.1) | 766.1 (643.0) | 841.9 (956.1) b | 805.0 (692.5) | 619.4 (504.7) a | 507.0 (340.9) b |
| Hypertension, n (%) | 339 (39.9) | 50 (48.5) | 115 (43.1) | 40 (44.4) | 33 (35.9) | 70 (35.9) | 31 (30.4) |
| Dyslipidemia, n (%) | 557 (65.6) | 69 (67.0) | 189 (70.8) | 65 (72.2) | 64 (69.6) | 112 (57.4) | 58 (56.9) |
| Total Cholesterol, mean (SD), mg/dl | 187.2 (37.1) | 181.8 (35.4) | 181.4 (37.1) | 182.5 (39.1) | 195.0 (38.3) | 192.4 (34.6) | 194.8 (37.1) |
| Cholesterol-lowering medications, n (%) | 254 (29.9) | 35 (34.0) | 88 (33.0) | 40 (44.4) | 24 (26.1) | 37 (19.0) | 30 (29.4) |
| Glucose-lowering medications, n (%) | 142 (16.7) | 25 (24.3) | 51 (19.1) | 18 (20.0) | 15 (16.3) | 17 (8.7) | 16.(15.7) |
| Blood pressure-lowering medications, n (%) | 253 (31.7) | 42 (42.0) | 83 (33.3) | 34 (38.6) | 23 (25.8) | 45 (25.0) | 26 (28.0) |
| Weight and Body Composition | |||||||
| Obesity, n (%)† | 250 (29.6) | 32 (31.1) | 67 (25.3) | 24 (26.7) | 45 (48.9) | 55 (28.4) a | 27 (26.5) b |
| Weight, mean (SD), Kg | 69.9 (12.5) | 73.7 (14.0) | 74.4 (11.1) | 76.1 (10.9) | 66.1 (10.4) | 63.8 (11.1) a | 64.2 (11.7) b |
| Hip girth, mean (SD), cm | 102.8 (8.4) | 101.9 (8.6) | 102.5 (7.4) | 101.7 (6.9) | 105.6 (8.7) | 103.4 (9.6) a | 102.1 (8.4) b |
| Waist-Hip ratio, mean (SD) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) |
| Subcutaneous fat, mean (SD), cm2 | 234.8 (91.5) | 208.0 (90.6) | 217.4 (83.8) | 210.3 (76.3) | 274.5 (113.2) | 256.1 (85.8) | 253.3 (91.0) |
| Inter-muscular fat, mean (SD), cm2 | 21.3 (8.6) | 21.0 (8.6) | 21.4 (9.7) | 20.6 (8.2) | 21.8 (8.4) | 20.9 (7.3) | 22.4 (8.5) |
Differences by acculturation class were examined using t tests and pairwise comparison (i.e. separation vs integration and separation vs assimilation); categorical variables were examined using chi-squared tests of homogeneity. Testing was performed on log transformed variables when necessary to achieve normality.
Obesity was defined using the WHO Asian BMI cut-off point of BMI ≥27.5 kg/m2.
Statistically significant difference (p value<0.05) between integration and separation classes.
Statistically significant difference (p value<0.05) between assimilation and separation classes.
Table 3:
Multivariable regression models of the relationship between cardiovascular disease risk factors and acculturation class in Women*
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Beta | P-value | Beta | P-value | Beta | P-value | Beta | P-value |
| Fasting Glucose | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −8.9 (±2.9) | <0.01 | −7.0 (±2.9) | 0.02 | −4.7 (±3.2) | 0.14 | −2.8 (±2.8) | 0.31 |
| Assimilation | −4.9 (±3.3) | 0.14 | −2.5 (±3.4) | 0.46 | 0.8 (±3.8) | 0.84 | 0.8 (±3.4) | 0.80 |
| 2 hr Glucose | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −20.3 (±7.1) | <0.01 | −20.3 (±7.1) | <0.01 | −12.4 (±8.0) | 0.12 | −7.9 (±7.5) | 0.29 |
| Assimilation | −14.2 (±8.1) | 0.08 | −15.0 (±8.3) | 0.07 | −5.6 (±9.5) | 0.55 | 2.5 (±9.1) | 0.78 |
| Systolic Blood Pressure | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | 0.3 (±2.1) | 0.88 | 1.0 (±2.0) | 0.61 | 3.0 (±2.2) | 0.19 | 3.0 (±2.2) | 0.16 |
| Assimilation | −2.7 (±2.4) | 0.26 | −2.2 (±2.3) | 0.35 | 1.6 (±2.6) | 0.53 | 1.2 (±2.6) | 0.63 |
| Diastolic Blood Pressure | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | 1.1 (±1.2) | 0.37 | 1.6 (±1.2) | 0.21 | 1.9 (±1.4) | 0.18 | 2.2 (±1.4) | 0.12 |
| Assimilation | −1.0 (±1.4) | 0.48 | −0.1 (±1.4) | 0.92 | 1.3 (±1.6) | 0.43 | 0.9 (±1.7) | 0.60 |
| Total cholesterol | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −2.6 (±4.6) | 0.56 | −4.0 (±4.6) | 0.39 | 2.7 (±5.2) | 0.61 | −2.2 (±4.9) | 0.65 |
| Assimilation | −0.2 (±5.2) | 0.97 | −2.4 (±5.4) | 0.65 | 3.9 (±6.0) | 0.52 | 1.7 (±5.8) | 0.77 |
| Triglycerides† | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −20.5 (±6.4) | <0.01 | −19.4 (±6.5) | <0.01 | −19.3 (±7.5) | 0.01 | −18.2 (±7.5) | 0.02 |
| Assimilation | −29.2 (±7.2) | <0.01 | −27.8 (±7.6) | <0.01 | −25.4 (±8.7) | <0.01 | −24.2 (±8.8) | <0.01 |
| LDL | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −1.5 (±4.0) | 0.71 | −2.4 (±4.1) | 0.57 | 3.6 (±4.6) | 0.44 | −0.4 (±4.3) | 0.93 |
| Assimilation | −3.2 (±4.6) | 0.48 | −4.4 (±4.8) | 0.36 | 0.7 (±5.4) | 0.89 | −0.2 (±5.2) | 0.96 |
| HDL† | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | 3.1 (±1.7) | 0.07 | 2.4 (±1.7) | 0.16 | 3.2 (±1.9) | 0.09 | 2.5 (±1.9) | 0.18 |
| Assimilation | 9.0 (±1.9) | <0.01 | 7.7 (±2.0) | <0.01 | 8.4 (±2.2) | <0.01 | 7.3 (±2.2) | <0.01 |
| Visceral Fat | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −8.9 (±5.6) | 0.11 | −8.3 (±5.6) | 0.14 | −6.1 (±6.4) | 0.34 | −5.2 (±6.3) | 0.41 |
| Assimilation | −11.4 (±6.4) | 0.07 | −11.3 (±6.5) | 0.08 | −8.1 (±7.4) | 0.28 | −5.6 (±7.4) | 0.45 |
| Waist Circumference | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −2.4 (±1.2) | 0.05 | −2.7 (±1.3) | 0.03 | −1.6 (±1.4) | 0.26 | −1.5 (±1.4) | 0.28 |
| Assimilation | −2.9 (±1.4) | 0.04 | −3.5 (±1.5) | 0.02 | −1.8 (±1.7) | 0.28 | −1.6 (±1.7) | 0.35 |
| BMI † | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −1.5 (±0.5) | <0.01 | −1.5 (±0.5) | <0.01 | −1.0 (±0.6) | 0.09 | −0.9 (±0.6) | 0.12 |
| Assimilation | −1.5 (±0.6) | <0.01 | −1.5 (±0.6) | 0.01 | −1.0 (±0.7) | 0.16 | −0.8 (±0.7) | 0.23 |
Beta coefficient ±SD except as indicated. The regression models compare levels of various cardiometabolic risk factors in women in the integration and assimilation classes to those in the separation class. All results are from linear regression models. Unadjusted model; Model 1: adjusted for age, study site, and years lived in the US; Model 2 (socioeconomic factors): Model 1+ adjustment for education level, family income, country of birth, marital status, religious affiliation, medical insurance, and employment; Model 3 (behavioral and psychosocial factors): Model 2+ adjustment for total physical activity, total exercise, total caloric intake, depression, smoking and alcohol status. Additional adjustment for the use of glucose-lowering, blood pressure-lowering, and lipid-lowering medications was performed in Model 3 when examining the relationship between acculturation class and (fasting and 2 hr glucose), (systolic and diastolic blood pressure), and (total cholesterol, triglycerides, LDL, and HDL); respectively.
p-value for interaction by sex is <0.05
DISCUSSION
In contrast to prior studies, we found a relatively higher degree of preference for US culture over SA culture– represented by the integration and assimilation classes– to be associated with an overall healthier cardiometabolic profile among SA women in the US; but the differences in CVD risk factors by acculturation strategy were not significant in men. Furthermore, we identified healthier behaviors and psychosocial factors in men and women who employ the assimilation strategy compared to those who employ the separation strategy that include less caloric intake, more total exercise, and less depression symptoms. However, the differences in these behavioral and psychosocial factors across acculturation classes did not completely explain the healthier cardiometabolic profile among SAs who expressed a stronger preference for US culture over SA culture. The differences by acculturation class in HDL and triglyceride levels among women, for example, remained significant even after adjusting for demographic, socioeconomic, behavioral, and psychosocial factors that include caloric intake, total exercise, and depression symptoms. It is possible that unmeasured lifestyle, psychosocial factors, and contextual factors among women in the different acculturation classes may explain these findings.
The sex differences in the association between acculturation and CVD risk factors in our study is an important finding that warrants further attention. Only among women, did we find that a relatively higher degree of preference for US culture over SA culture was associated with lower prevalence of CVD risk factors. Similarly, another study reported that maintaining the original culture was associated with a greater BMI and waist circumference in immigrant women in the US from the former Soviet Union.42 However, the association between acculturation and diabetes has been shown to be stronger in men than women in other studies in Latinos and other ethnic groups.15, 28 It has been postulated that the negative impact of health-compromising behaviors, highly prevalent in high-income countries, may be offset by the Western social norms on body shape which endorse slim body shape and fitness especially among women.17 In support of this idea, one study reported that Mexican Americans who were overweight and less acculturated were less likely to perceive themselves as overweight and to have tried to lose weight compared to those who were more acculturated.43 Therefore, it is possible that SA women may adopt healthier behaviors and improved health knowledge and attitude as they integrate or assimilate in the US. It has also been proposed that women tend to adapt to the cultural norm of the host country more quickly than men; and it is possible that SA women may be influenced by some of the health-promoting behaviors in the US such as leisure-time physical activity more quickly than men52. It is also possible that differences in health beliefs and perception, knowledge about disease risk and prevention, and attitudes towards CVD risk factors, and psychosocial factors may exist across acculturation classes and could potentially explain the differences in CVD risk factors observed in our study. Future research should explore these potential pathways linking acculturation strategies with CVD risk factors in SA women.
Previous studies examining the association of acculturation and CVD risk factors have been inconclusive. For example, assimilation to the US has been associated with poorer health behaviors and increased risk of diabetes, hypertension, and coronary artery disease in many studies of other immigrant groups.16–18, 44–47 Duration of residence in the US and/or English language proficiency have been used as surrogate markers of acculturation in many of these studies. In contrast, a smaller number of studies linked higher degree of acculturation with positive health behaviors and lower risk of diabetes, obesity, and other CVD risk factors.29, 42, 48–50 The inconsistency in these results is partly due to differences in country of origin and ethnicity, reasons for and context of migration, and, importantly, reliance on surrogate markers of acculturation that do not account for the multidimensional nature of acculturation. In fact, the use of length of residence in the US as a proxy measure of acculturation in our study failed to capture most of the differences in CVD risk factors observed with the use of the multidimensional acculturation model. Furthermore, participants in the assimilation and integration classes in our study had a healthier cardiometabolic profile despite having more years of residence in the US compared to those in the separation class. These findings highlight the advantage of using an expanded model of acculturation when studying the impact of acculturation on cardiometabolic health. This is especially true for SAs in the MASALA study because over 70% of them have been in the US for more than 20 years and speak English well or very well. Similar findings have been recently shown in Ghanaian and Nigerian-born African immigrants in the US; where those who employ an integration strategy were found to have lower CVD risk, despite having a longer duration of residence in the US, compared to those who had more traditional beliefs and behaviors.29
A major strength of our study is that instead of relying on traditional proxy measures of acculturation such as years in the US or English language proficiency, we used a multidimensional model of acculturation that accounts for attitude about the practice of SA traditions in the US, frequency of fasting, food normally eaten at home and in restaurants, frequency of shopping in SA markets, and ethnic composition of friendship networks. Furthermore, the large community-based sample along with the comprehensive assessment of acculturation, CVD risk, lifestyle and behavioral factors in our study allowed us to identify the potential impact of acculturation strategies on CVD risk factors that is not apparent with the use of traditional proxy measures of acculturation. The latter finding has implications for future studies examining the health consequences of acculturation in SA immigrants, as well as immigrants of other racial/ethnic groups, living in high-income countries as our multidimensional model of acculturation can be adopted in those studies.
The limitations of our study include the cross-sectional nature that precludes us from making causal inferences as we are unable to ascertain temporal order between acculturation strategies and CVD risk factors. The MASALA study recruited participants from two specific geographic regions, the San Francisco Bay and great Chicago areas, which may not represent all SAs immigrants in the US. However, similarity of the MASALA population to the US Census 2010 South Asians data has been reported.32 Consistent with waves of SA immigration to the US, a majority of the MASALA study participants were Asian Indians, have lived in the US for over 20 years, speak English well or very well, and had a high socioeconomic status which limits the generalizability of our results. These, and other contextual factors, influence how immigrants acculturate into US society.51 It is possible that we have not captured residual confounding factors that may explain the linkage between acculturation strategies and CVD risk factors in SA immigrants. Finally, we treated latent class membership as an observed variable where respondents were assigned to a single acculturation class based on their most likely class assignment. This approach does not account for uncertainty in latent class assignment.
In conclusion, our findings suggest that SA immigrant women who employ an assimilation or integration strategy have a more favorable cardiometabolic profile compared to women using a separation strategy. Therefore, programs targeting the prevention and management of CVD risk factors among SA immigrants should be culturally tailored to account for differences in acculturation strategy and sex; and focus on promoting the adoption and retention of healthy lifestyle and behaviors after arrival in the US. Future research should investigate the behavioral, psychosocial, and contextual pathways linking acculturation strategies with cardiometabolic health among SA immigrants and further explore the differences in the impact of acculturation strategies in women versus men and the potential incorporation into prevention interventions.
Supplementary Material
A) Fasting glucose levels were similar in women in the assimilation class [median (IQR): 95 (15) mg/dl, p=0.79] compared to women in the separation class [94 (18) mg/dl]. Similarly, women in the integration class had similar levels of fasting glucose [median (IQR): 94 (12) mg/dl, p=0.11] compared to women in the separation class. Fasting glucose levels were similar in men in the separation, integration, and assimilation classes [median (IQR):101 (24), 99 (20), and 97 (26) mg/dl, respectively, all p>0.05]. B) Log HOMA-IR levels were slightly lower in women in the assimilation class [mean (SD): 0.68 (0.74), p=0.08] compared to women in the separation class [0.82 (0.63)]. Women in the integration class had log HOMA-IR of [0.72 (0.56), p=0.07] compared to women in the separation class. Log HOMA-IR levels were similar in men in the separation, integration, and assimilation classes [1.05 (0.68), 0.95 (0.61), and 0.95 (0.71), respectively; all p>0.05].
A) Systolic blood pressure levels were similar in women in the separation, integration, and assimilation classes [mean (SD): 122.4 (15.1), 122.7 (18.6), and 119.7 (13.5) mmHg, respectively; all p>0.05]. Systolic blood pressure levels were similar in men in the separation, integration, and assimilation classes [124.7 (14.6), 126.1 (14.4), and 125.3 (13.7) mmHg, respectively; all p>0.05]. B) Diastolic blood pressure levels were similar in women in the separation, integration, and assimilation classes [mean (SD): 69.3 (9.7), 70.4 (10.1), and 68.3 (8.9) mmHg, respectively; all p>0.05]. Diastolic blood pressure levels were similar in men in the separation, integration, and assimilation classes [75.2 (9.0), 77.1 (8.5), and 75.6 (9.2) mmHg, respectively; all p>0.05]. C) LDL levels were similar in women in the separation, integration, and assimilation classes [mean (SD): 115.7 (32), 114.2 (30.6), and 112.5 (34.1) mg/dl, respectively; all p>0.05]. LDL levels were similar in men in the separation, integration, and assimilation classes [108.4 (30.3), 109.5 (32.8), and 105.2 (33.2) mg/dl, respectively; all p>0.05].
A) Slightly smaller waist circumference in women in the assimilation group [mean (SD) 88.3 (10.5) cm, p=0.06] compared to women in the separation class [91.2 (10.2) cm]. Slightly smaller waist circumference in women in the integration class [88.8 (9.1) cm, p=0.05] compared to women in the separation class. Similar waist circumferences in men in the separation, integration, and assimilation classes [96.5 (11.4), 95.6 (8.9), and 95.3 (8.7) cm, respectively; all p>0.05]. B) Slightly smaller Visceral fat areas in women in the assimilation group [mean (SD) 110.4 (49.3) cm2, p=0.08] compared to women in the separation class [121.7 (40.4) cm]. Similar visceral area in the integration class [112.8 (42.9) cm, p=0.10] compared to women in the separation class. Similar visceral fat areas in men in the separation, integration, and assimilation classes [160.2 (73.7), 149.4 (53.6), and 149 (56) cm, respectively; all p>0.05]. C) *Pericardial fat volumes were smaller in women in the assimilation group [median (IQR) 42 (26.3) cm2, p=0.01] compared to women in the separation class [49.4 (24.9) cm2]. **Women in the integration class also had a smaller pericardial fat volume of [43.6 (23.1) cm2, p=0.02] compared to women in the separation class. Pericardial fat volumes were similar in men in the separation, integration, and assimilation classes [62.6 (32.8), 62.1 (44.3), and 64.9 (32) cm, respectively; all p>0.05]. D) Hepatic fat attenuation was similar in women in the separation, integration, and assimilation classes [median (IQR) 59.5 (9.5), 61.0 (11.0), and 59.5 (13.0) HU, respectively; all p>0.05]. Hepatic fat attenuation was similar in men in the separation, integration, and assimilation classes [52 (13.5), 55.0 (12.0), and 54.0 (13.0) HU, respectively; all p>0.05].
Table 4:
Multivariable regression models of the relationship between cardiovascular disease risk factors and acculturation class in men*
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | Beta | P-value | Beta | P-value | Beta | P-value | Beta | P-value |
| Fasting Glucose | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −1.6 (±3.0) | 0.59 | −0.8 (±3.0) | 0.80 | −0.1 (±3.1) | 0.98 | 1.2 (±2.6) | 0.65 |
| Assimilation | −1.9 (±3.7) | 0.61 | −0.3 (±3.8) | 0.94 | 0.4 (±4.1) | 0.92 | 1.0 (±3.6) | 0.77 |
| 2 hr Glucose | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −2.4 (±7.2) | 0.74 | −0.4 (±7.2) | 0.96 | 9.3 (±7.7) | 0.23 | 7.9 (±7.7) | 0.31 |
| Assimilation | −8.9 (±8.9) | 0.32 | −4.8 (±9.3) | 0.60 | 6.9 (±10.1) | 0.49 | 4.0 (±10.4) | 0.70 |
| Systolic Blood Pressure | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | 1.5 (±1.7) | 0.37 | 1.4 (±1.6) | 0.39 | 1.2 (±1.7) | 0.46 | 1.9 (±1.7) | 0.27 |
| Assimilation | 0.6 (±2.1) | 0.77 | 0.2 (±2.0) | 0.93 | −0.2 (±2.2) | 0.93 | 0.1 (±2.3) | 0.98 |
| Diastolic Blood Pressure | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | 1.9 (±1.0) | 0.06 | 1.7 (±1.0) | 0.10 | 2.0 (±1.0) | 0.05 | 2.4 (±1.0) | 0.02 |
| Assimilation | 0.3 (±1.3) | 0.79 | −0.3 (±1.3) | 0.80 | −0.1 (±1.4) | 0.96 | −0.1 (±1.4) | 0.93 |
| Total cholesterol | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −0.4 (±4.3) | 0.93 | −0.3 (±4.3) | 0.94 | −0.3 (±4.5) | 0.95 | 0.1 (±4.0) | 0.97 |
| Assimilation | 0.7 (±5.3) | 0.90 | 1.0 (±5.5) | 0.86 | 1.4 (±5.9) | 0.81 | 8.7 (±5.6) | 0.12 |
| Triglycerides† | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −7.8 (±8.7) | 0.37 | −8.1 (±8.6) | 0.35 | −7.9 (±9.0) | 0.38 | −7.4 (±9.1) | 0.42 |
| Assimilation | 3.2 (±10.8) | 0.76 | 3.6 (±11.1) | 0.74 | 6.9 (±11.9) | 0.57 | 10.2 (±12.5) | 0.41 |
| LDL | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | 1.1 (±3.8) | 0.76 | 1.2 (±3.8) | 0.76 | 0.9 (±3.9) | 0.82 | 2.1 (±3.5) | 0.56 |
| Assimilation | −3.2 (±4.7) | 0.50 | −2.8 (±4.9) | 0.57 | −2.9 (±5.2) | 0.58 | 5.3 (±4.9) | 0.27 |
| HDL† | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −0.9 (±1.2) | 0.48 | −0.8 (±1.2) | 0.51 | −0.2 (±1.3) | 0.89 | −0.6 (±1.3) | 0.66 |
| Assimilation | 2.0 (±1.5) | 0.19 | 2.0 (±1.6) | 0.21 | 2.1 (±1.7) | 0.21 | 1.8 (±1.7) | 0.30 |
| Visceral Fat | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −10.8 (±7.1) | 0.13 | −11.2 (±7.1) | 0.12 | −7.4 (±7.4) | 0.32 | −7.5 (±7.4) | 0.31 |
| Assimilation | −11.2 (±8.7) | 0.20 | −12.3 (±9.1) | 0.17 | −6.4 (±9.7) | 0.51 | −4.8 (±10.0) | 0.63 |
| Waist Circumference | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −0.9 (±1.1) | 0.40 | −0.9 (±1.1) | 0.39 | −0.2 (±1.2) | 0.86 | −0.2 (±1.1) | 0.88 |
| Assimilation | −1.2 (±1.4) | 0.38 | −1.3 (±1.4) | 0.37 | −0.1 (±1.5) | 0.97 | 0.3 (±1.6) | 0.87 |
| BMI† | ||||||||
| Separation | Ref | Ref | Ref | Ref | ||||
| Integration | −0.1 (±0.5) | 0.81 | −0.2 (±0.5) | 0.67 | 0.0 (±0.5) | 0.96 | 0.0 (±0.5) | 0.93 |
| Assimilation | 0.3 (±0.6) | 0.56 | 0.2 (±0.6) | 0.79 | 0.5 (±0.6) | 0.41 | 0.4 (±0.7) | 0.50 |
Beta coefficient ±SD except as indicated. The regression models compare levels of various cardiometabolic risk factors in men in the integration and assimilation classes to those in the separation class. All results are from linear regression models. Unadjusted model; Model 1: adjusted for age, study site, and years lived in the US; Model 2 (socioeconomic factors): Model 1+ adjustment for education level, family income, country of birth, marital status, religious affiliation, medical insurance, and employment; Model 3 (behavioral and psychosocial factors): Model 2+ adjustment for total physical activity, total exercise, total caloric intake, depression, smoking and alcohol status. Additional adjustment for the use of glucose-lowering, blood pressure-lowering, and lipid-lowering medications was performed in Model 3 when examining the relationship between acculturation class and (fasting and 2 hr glucose), (systolic and diastolic blood pressure), and (total cholesterol, triglycerides, LDL, and HDL); respectively.
p-value for interaction by sex is <0.05
ACKNOWLEDGMENT:
The authors thank the MASALA staff and participants for their valuable contributions. They also thank Dr. Diane M. Becker from the Division of General Internal Medicine at Johns Hopkins University for providing critical analysis and insightful comments on early versions of the manuscript.
Financial Support: The MASALA study was supported by NIH grants R01HL093009 and K24HL112827. Data collection at the University of California, San Francisco, was supported by NIH/NCRR grant UL1 RR024131. The Saudi Government Scholarship from King Saud University, Riyadh, Saudi Arabia provided fellowship training support to Dr. Al-Sofiani. None of the funders were involved in the design, conduct, or analysis of the study; collection, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Disclosure Summary: No conflicts of interest relevant to this article were reported by the authors.
REFERENCES
- 1.Geldsetzer P, Manne-Goehler J, Theilmann M, et al. Diabetes and Hypertension in India: A Nationally Representative Study of 1.3 Million Adults. JAMA Intern Med. 2018;178(3):363–372. doi: 10.1001/jamainternmed.2017.8094 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anjana RM, Deepa M, Pradeepa R, et al. Prevalence of diabetes and prediabetes in 15 states of India: results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5(8):585–596. doi: S2213-8587(17)30174-2 [pii]. [DOI] [PubMed] [Google Scholar]
- 3.Prabhakaran D, Jeemon P, Ghosh S, et al. Prevalence and incidence of hypertension: Results from a representative cohort of over 16,000 adults in three cities of South Asia. Indian Heart J. 2017;69(4):434–441. doi: S0019-4832(17)30228-6 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Census Bureau U.S. 2010 Census--Demographic Profile Data.2010. [Google Scholar]
- 5.LÓPEZ G, RUIZ N, PATTEN E. Key facts about Asian Americans, a diverse and growing population. . Accessed 2/12/, 2019. [Google Scholar]
- 6.Jose PO, Frank AT, Kapphahn KI, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64(23):2486–2494. doi: 10.1016/j.jacc.2014.08.048 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Creatore MI, Moineddin R, Booth G, et al. Age- and sex-related prevalence of diabetes mellitus among immigrants to Ontario, Canada. CMAJ. 2010;182(8):781–789. doi: 10.1503/cmaj.091551 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhopal R, Unwin N, White M, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999;319(7204):215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wium C, Gulseth HL, Eriksen EF, Birkeland KI. Characteristics of glucose metabolism in Nordic and South Asian subjects with type 2 diabetes. PLoS One. 2013;8(12):e83983. doi: 10.1371/journal.pone.0083983 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kanaya AM, Herrington D, Vittinghoff E, et al. Understanding the high prevalence of diabetes in U.S. south Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37(6):1621–1628. doi: 10.2337/dc13-2656 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement From the American Heart Association. Circulation. 2018;138(1):e34. doi: 10.1161/CIR.0000000000000580 [doi]. [DOI] [PubMed] [Google Scholar]
- 12.Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet. 2000;356(9226):279–284. doi: S0140673600025022 [pii]. [DOI] [PubMed] [Google Scholar]
- 13.Misra R, Patel T, Kotha P, et al. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: results from a national study. J Diabetes Complications. 2010;24(3):145–153. doi: 10.1016/j.jdiacomp.2009.01.003 [doi]. [DOI] [PubMed] [Google Scholar]
- 14.Clark L, Hofsess L. Handbook of Immigrant Health. New York, NY: Plenum Press; 1998. [Google Scholar]
- 15.Commodore-Mensah Y, Ukonu N, Obisesan O, et al. Length of Residence in the United States is Associated With a Higher Prevalence of Cardiometabolic Risk Factors in Immigrants: A Contemporary Analysis of the National Health Interview Survey. J Am Heart Assoc. 2016;5(11): 10.1161/JAHA.116.004059. doi: e004059 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Brien MJ, Alos VA, Davey A, Bueno A, Whitaker RC. Acculturation and the prevalence of diabetes in US Latino Adults, National Health and Nutrition Examination Survey 2007–2010. Prev Chronic Dis. 2014;11:E176. doi: 10.5888/pcd11.140142 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Delavari M, Sonderlund AL, Swinburn B, Mellor D, Renzaho A. Acculturation and obesity among migrant populations in high income countries--a systematic review. BMC Public Health. 2013;13:458. doi: 10.1186/1471-2458-13-458 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kandula NR, Diez-Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA). Diabetes Care. 2008;31(8):1621–1628. doi: 10.2337/dc07-2182 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oza-Frank R, Narayan KM. Overweight and diabetes prevalence among US immigrants. Am J Public Health. 2010;100(4):661–668. doi: 10.2105/AJPH.2008.149492 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese-Americans. Am J Epidemiol. 1976;104(3):225–247. [DOI] [PubMed] [Google Scholar]
- 21.Egusa G, Watanabe H, Ohshita K, et al. Influence of the extent of westernization of lifestyle on the progression of preclinical atherosclerosis in Japanese subjects. J Atheroscler Thromb. 2002;9(6):299–304. [DOI] [PubMed] [Google Scholar]
- 22.Patel JV, Vyas A, Cruickshank JK, et al. Impact of migration on coronary heart disease risk factors: comparison of Gujaratis in Britain and their contemporaries in villages of origin in India. Atherosclerosis. 2006;185(2):297–306. doi: S0021-9150(05)00378-3 [pii]. [DOI] [PubMed] [Google Scholar]
- 23.Bhatnagar D, Anand IS, Durrington PN, et al. Coronary risk factors in people from the Indian subcontinent living in west London and their siblings in India. Lancet. 1995;345(8947):405–409. doi: S0140-6736(95)90398-4 [pii]. [DOI] [PubMed] [Google Scholar]
- 24.Shah BM, Shah S, Kandula NR, Gadgil MD, Kanaya AM. Psychosocial Factors Associated with Subclinical Atherosclerosis in South Asians: The MASALA Study. J Immigr Minor Health. 2016;18(6):1317–1327. doi: 10.1007/s10903-016-0367-5 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernando E, Razak F, Lear SA, Anand SS. Cardiovascular Disease in South Asian Migrants. Can J Cardiol. 2015;31(9):1139–1150. doi: 10.1016/j.cjca.2015.06.008 [doi]. [DOI] [PubMed] [Google Scholar]
- 26.Kolt GS, Schofield GM, Rush EC, Oliver M, Chadha NK. Body fatness, physical activity, and nutritional behaviours in Asian Indian immigrants to New Zealand. Asia Pac J Clin Nutr. 2007;16(4):663–670. [PubMed] [Google Scholar]
- 27.Venkatesh S, Weatherspoon LJ, Kaplowitz SA, Song WO. Acculturation and glycemic control of Asian Indian adults with type 2 diabetes. J Community Health. 2013;38(1):78–85. doi: 10.1007/s10900-012-9584-6 [doi]. [DOI] [PubMed] [Google Scholar]
- 28.Arcia E, Skinner M, Bailey D, Correa V. Models of acculturation and health behaviors among Latino immigrants to the US. Soc Sci Med. 2001;53(1):41–53. doi: S0277953600003105 [pii]. [DOI] [PubMed] [Google Scholar]
- 29.Commodore-Mensah Y, Ukonu N, Cooper LA, Agyemang C, Himmelfarb CD. The Association Between Acculturation and Cardiovascular Disease Risk in Ghanaian and Nigerian-born African Immigrants in the United States: The Afro-Cardiac Study. J Immigr Minor Health. 2018;20(5):1137–1146. doi: 10.1007/s10903-017-0644-y [doi]. [DOI] [PubMed] [Google Scholar]
- 30.Lee SK, Sobal J, Frongillo EA. Acculturation and health in Korean Americans. Soc Sci Med. 2000;51(2):159–173. doi: S0277953699004463 [pii]. [DOI] [PubMed] [Google Scholar]
- 31.Needham BL, Mukherjee B, Bagchi P, et al. Acculturation Strategies Among South Asian Immigrants: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. J Immigr Minor Health. 2017;19(2):373–380. doi: 10.1007/s10903-016-0372-8 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kanaya AM, Kandula N, Herrington D, et al. Mediators of Atherosclerosis in South Asians Living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol. 2013;36(12):713–720. doi: 10.1002/clc.22219 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. [DOI] [PubMed] [Google Scholar]
- 34.American Diabetes Association. 2. Classification and diagnosis of diabetes: Standard of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(Suppl.1):S27. [DOI] [PubMed] [Google Scholar]
- 35.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: S0140-6736(03)15268-3 [pii]. [DOI] [PubMed] [Google Scholar]
- 36.Center for Information Technology and National Institutes of Health. 1999. “MIPAV(Medical Image Processing, Analysis, and Visualization) 4.1.2 software” Bethesda, Maryland. [Google Scholar]
- 37.Shah AD, Kandula NR, Lin F, et al. Less favorable body composition and adipokines in South Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes (Lond). 2016;40(4):639–645. doi: 10.1038/ijo.2015.219 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelemen LE, Anand SS, Vuksan V, et al. Development and evaluation of cultural food frequency questionnaires for South Asians, Chinese, and Europeans in North America. J Am Diet Assoc. 2003;103(9):1178–1184. doi: 10.1053/jada.2003.50578 [doi]. [DOI] [PubMed] [Google Scholar]
- 39.Ainsworth BE, Irwin ML, Addy CL, Whitt MC, Stolarczyk LM. Moderate physical activity patterns of minority women: the Cross-Cultural Activity Participation Study. J Womens Health Gend Based Med. 1999;8(6):805–813. doi: 10.1089/152460999319129 [doi]. [DOI] [PubMed] [Google Scholar]
- 40.Radloff L The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 41.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: S0140-6736(03)15268-3 [pii]. [DOI] [PubMed] [Google Scholar]
- 42.Miller AM, Chandler PJ, Wilbur J, Sorokin O. Acculturation and cardiovascular disease risk in midlife immigrant women from the former Soviet Union. Prog Cardiovasc Nurs. 2004;19(2):47–55. [DOI] [PubMed] [Google Scholar]
- 43.Ahluwalia IB, Ford ES, Link M, Bolen JC. Acculturation, weight, and weight-related behaviors among Mexican Americans in the United States. Ethn Dis. 2007;17(4):643–649. [PubMed] [Google Scholar]
- 44.Mainous AG, Majeed A, Koopman RJ, et al. Acculturation and diabetes among Hispanics: evidence from the 1999–2002 National Health and Nutrition Examination Survey. Public Health Rep. 2006;121(1):60–66. doi: 10.1177/003335490612100112 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kaplan MS, Chang C, Newsom JT, McFarland BH. Acculturation status and hypertension among Asian immigrants in Canada. J Epidemiol Community Health. 2002;56(6):455–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dodani S, Dong L. Acculturation, coronary artery disease and carotid intima media thickness in South Asian immigrants--unique population with increased risk. Ethn Dis. 2011;21(3):314–321. [PubMed] [Google Scholar]
- 47.Stern MP, Knapp JA, Hazuda HP, Haffner SM, Patterson JK, Mitchell BD. Genetic and environmental determinants of type II diabetes in Mexican Americans. Is there a “descending limb” to the modernization/diabetes relationship?. Diabetes Care. 1991;14(7):649–654. [DOI] [PubMed] [Google Scholar]
- 48.Mainous AG, Diaz VA, Geesey ME. Acculturation and healthy lifestyle among Latinos with diabetes. Ann Fam Med. 2008;6(2):131–137. doi: 10.1370/afm.814 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shi L, Zhang D, van Meijgaard J, MacLeod KE, Fielding JE. The Interaction Between an Individual’s Acculturation and Community Factors on Physical Inactivity and Obesity: A Multilevel Analysis. Am J Public Health. 2015;105(7):1460–1467. doi: 10.2105/AJPH.2014.302541 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hazuda HP, Haffner SM, Stern MP, Eifler CW. Effects of acculturation and socioeconomic status on obesity and diabetes in Mexican Americans. The San Antonio Heart Study. Am J Epidemiol. 1988;128(6):1289–1301. [DOI] [PubMed] [Google Scholar]
- 51.Florez KR, Abraido-Lanza A. Segmented Assimilation: An Approach to Studying Acculturation and Obesity Among Latino Adults in the United States. Fam Community Health. 2017;40(2):132–138. doi: 10.1097/FCH.0000000000000143 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.An N, Cochran SD, Mays VM, McCarthy WJ. Influence of american acculturation on cigarette smoking behaviors among asian american subpopulations in california. Nicotine Tob Res. 2008;10(4):579–587. doi: 10.1080/14622200801979126 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A) Fasting glucose levels were similar in women in the assimilation class [median (IQR): 95 (15) mg/dl, p=0.79] compared to women in the separation class [94 (18) mg/dl]. Similarly, women in the integration class had similar levels of fasting glucose [median (IQR): 94 (12) mg/dl, p=0.11] compared to women in the separation class. Fasting glucose levels were similar in men in the separation, integration, and assimilation classes [median (IQR):101 (24), 99 (20), and 97 (26) mg/dl, respectively, all p>0.05]. B) Log HOMA-IR levels were slightly lower in women in the assimilation class [mean (SD): 0.68 (0.74), p=0.08] compared to women in the separation class [0.82 (0.63)]. Women in the integration class had log HOMA-IR of [0.72 (0.56), p=0.07] compared to women in the separation class. Log HOMA-IR levels were similar in men in the separation, integration, and assimilation classes [1.05 (0.68), 0.95 (0.61), and 0.95 (0.71), respectively; all p>0.05].
A) Systolic blood pressure levels were similar in women in the separation, integration, and assimilation classes [mean (SD): 122.4 (15.1), 122.7 (18.6), and 119.7 (13.5) mmHg, respectively; all p>0.05]. Systolic blood pressure levels were similar in men in the separation, integration, and assimilation classes [124.7 (14.6), 126.1 (14.4), and 125.3 (13.7) mmHg, respectively; all p>0.05]. B) Diastolic blood pressure levels were similar in women in the separation, integration, and assimilation classes [mean (SD): 69.3 (9.7), 70.4 (10.1), and 68.3 (8.9) mmHg, respectively; all p>0.05]. Diastolic blood pressure levels were similar in men in the separation, integration, and assimilation classes [75.2 (9.0), 77.1 (8.5), and 75.6 (9.2) mmHg, respectively; all p>0.05]. C) LDL levels were similar in women in the separation, integration, and assimilation classes [mean (SD): 115.7 (32), 114.2 (30.6), and 112.5 (34.1) mg/dl, respectively; all p>0.05]. LDL levels were similar in men in the separation, integration, and assimilation classes [108.4 (30.3), 109.5 (32.8), and 105.2 (33.2) mg/dl, respectively; all p>0.05].
A) Slightly smaller waist circumference in women in the assimilation group [mean (SD) 88.3 (10.5) cm, p=0.06] compared to women in the separation class [91.2 (10.2) cm]. Slightly smaller waist circumference in women in the integration class [88.8 (9.1) cm, p=0.05] compared to women in the separation class. Similar waist circumferences in men in the separation, integration, and assimilation classes [96.5 (11.4), 95.6 (8.9), and 95.3 (8.7) cm, respectively; all p>0.05]. B) Slightly smaller Visceral fat areas in women in the assimilation group [mean (SD) 110.4 (49.3) cm2, p=0.08] compared to women in the separation class [121.7 (40.4) cm]. Similar visceral area in the integration class [112.8 (42.9) cm, p=0.10] compared to women in the separation class. Similar visceral fat areas in men in the separation, integration, and assimilation classes [160.2 (73.7), 149.4 (53.6), and 149 (56) cm, respectively; all p>0.05]. C) *Pericardial fat volumes were smaller in women in the assimilation group [median (IQR) 42 (26.3) cm2, p=0.01] compared to women in the separation class [49.4 (24.9) cm2]. **Women in the integration class also had a smaller pericardial fat volume of [43.6 (23.1) cm2, p=0.02] compared to women in the separation class. Pericardial fat volumes were similar in men in the separation, integration, and assimilation classes [62.6 (32.8), 62.1 (44.3), and 64.9 (32) cm, respectively; all p>0.05]. D) Hepatic fat attenuation was similar in women in the separation, integration, and assimilation classes [median (IQR) 59.5 (9.5), 61.0 (11.0), and 59.5 (13.0) HU, respectively; all p>0.05]. Hepatic fat attenuation was similar in men in the separation, integration, and assimilation classes [52 (13.5), 55.0 (12.0), and 54.0 (13.0) HU, respectively; all p>0.05].