Abstract
Introduction
Gastrointestinal (GI) symptoms are increasingly being recognized in coronavirus disease 2019 (COVID-19). It is unclear if the presence of GI symptoms is associated with poor outcomes in COVID-19. We aim to assess if GI symptoms could be used for prognostication in hospitalized patients with COVID-19.
Methods
We retrospectively analyzed patients admitted to a tertiary medical center in Brooklyn, NY, from March 18, 2020, to March 31, 2020, with COVID-19. The patients' medical charts were reviewed for the presence of GI symptoms at admission, including nausea, vomiting, diarrhea, and abdominal pain. COVID-19 patients with GI symptoms (cases) were compared with COVID-19 patients without GI symptoms (control).
Results
A total of 150 hospitalized COVID-19 patients were included, of which 31 (20.6%) patients had at least 1 or more of the GI symptoms (cases). They were compared with the 119 COVID-19 patients without GI symptoms (controls). The average age among cases was 57.6 years (SD 17.2) and control was 63.3 years (SD 14.6). No statistically significant difference was noted in comorbidities and laboratory findings. The primary outcome was mortality, which did not differ between cases and controls (41.9 vs. 37.8%, p = 0.68). No statistically significant differences were noted in secondary outcomes, including the length of stay (LOS, 7.8 vs. 7.9 days, p = 0.87) and need for mechanical ventilation (29 vs. 26.9%, p = 0.82).
Discussion
In our study, the presence of GI manifestations in COVID-19 at the time of admission was not associated with increased mortality, LOS, or mechanical ventilation.
Keywords: COVID-19, Gastrointestinal manifestations, Gastrointestinal symptoms, Severe acute respiratory syndrome coronavirus 2, Coronavirus, Outcomes, Mortality, Length of stay
Introduction
The novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was started as an epidemic in Wuhan, China. It was later declared as a global pandemic with New York as the current epicenter [1]. The SARS-CoV-2 mainly spreads through direct exposure (droplets, person to person). However, it is also assumed to be transmitted by contaminated objects, airborne transmission, and fecal-oral transmission [2]. The COVID-19 is predominantly a respiratory disease manifested by fever, fatigue, dry cough, anorexia, myalgia, and dyspnea [3]. However, gastrointestinal (GI) manifestations such as nausea, vomiting, diarrhea, and abdominal pain are increasingly being recognized as important manifestations of COVID-19 [4, 5, 6, 7, 8]. Other symptoms such as dysgeusia and anosmia are also gaining attention as important symptoms of COVID-19 [9, 10].
The spectrum of COVID-19 infection ranges from mild to critical. Most of the patients (81%) have mild disease, 14% of the patients have severe disease, and 5% of the patients have a critical disease [1, 11]. The factors associated with severe COVID-19 infection include advanced age >65 years, chronic respiratory diseases, hypertension, diabetes mellitus (DM), malignancy, and cardiovascular disease [12, 13, 14]. In a recent study published from the USA, about 12% of the patients required mechanical ventilation, and the mortality rate of patients on mechanical ventilation was 88% [15]. In a study by Pan et al. [7], the presence of GI symptoms was associated with higher liver enzymes, lower monocyte count, and longer prothrombin time. The overall pooled prevalence of GI symptoms in COVID-19 based on a systematic review was reported to be 18% [16]. The most common GI symptom reported is diarrhea (13%), followed by nausea or vomiting (10%) and abdominal pain [16]. SARS-CoV-2 has also been found in the fecal samples of COVID-19 patients even after the complete resolution of symptoms [13, 17]. Therefore, the fecal-oral transmission is also considered as a potential mode of transmission [17]. The occurrence of GI symptoms is probably from the intestinal tropism of the SARS-CoV-2 [18]. Moreover, GI symptoms can coexist or even precede respiratory manifestations [19]. Rarely, COVID-19 patients can present with only GI symptoms without respiratory symptoms [7].
Hence, there has been an increasing interest in whether GI symptoms are associated with severe disease. There are conflicting reports in terms of whether GI symptoms are associated with severe COVID-19 or not [7, 20]. Therefore, in this study, we aimed to analyze if the presence of GI symptoms at the time of hospitalization is associated with mechanical ventilation or mortality when compared to those who did not have GI symptoms.
Methods
Study Design and Data Source
This is a retrospective cohort study conducted in a cohort of COVID-19 patients who were admitted to the Brookdale University Hospital Medical Center (BHMCNY), a tertiary care academic medical center in Brooklyn, New York. BHMCNY is a non-profit medical service provider servicing almost 1 million residents of Eastern Brooklyn. The BHMCNY's Institutional Review Board approved this study as minimal-risk research while utilizing anonymized and de-identified retrospective data collection and waived the requirement for informed consent. We included consecutive patients who were admitted to the hospital with a confirmed diagnosis of COVID-19 on nasopharyngeal polymerase chain reaction testing for SARS-CoV-2 from March 18, 2020, to March 31, 2020. Patients were excluded if they were younger than 18 years, who were not hospitalized and managed on an ambulatory basis, pregnant patients, unavailability of results of SARS-CoV-2 nasopharyngeal testing, and missing data on mortality or disposition.
Data related to patients' demographics, clinical symptoms, comorbidities, home medications, vitals at presentation, admission laboratory tests, inpatient medications, and outcomes were collected (Table 1). Demographic variables such as age, sex, race, smoking status, and BMI were obtained. Data on multiple comorbid conditions such as the history of hypertension, dyslipidemia, coronary artery disease, DM, history of any cancer, chronic obstructive pulmonary disease, and asthma were obtained. Medication history of the use of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, non-steroidal anti-inflammatory drugs, aspirin, or statin use was collected. Furthermore, initial laboratory data such as hemoglobin level, WBC, absolute lymphocyte count, platelet count, ferritin, C-reactive protein (CRP), d-dimer, lactic acid, aspartate aminotransferase, and alanine aminotransferase were noted. If a particular laboratory test was not performed at the time of admission, then the first laboratory values within 24 h of the admission were used.
Table 1.
Prevalence of gastrointestinal (GI) system in the entire cohort
| GI symptoms | N (%) |
|---|---|
| No gastrointestinal symptoms | 119 (79.3) |
| Nausea/vomiting | 6 (4) |
| Diarrhea | 15 (10) |
| Nausea/vomiting + diarrhea | 7 (4.7) |
| Nausea/vomiting + abdominal pain | 3 (2) |
Stratification of Study Cohort and Outcomes
In our study, the GI symptoms were defined as the presence of nausea, vomiting, diarrhea, or abdominal pain at the time of admission. The study cohort was stratified into 2 groups based on the presence of GI symptoms: COVID-19 with GI symptoms (cases) and COVID-19 without GI symptoms (controls). The primary outcome was death from any cause. Secondary outcomes were identified as total hospital length of stay (LOS) and need for mechanical ventilation during that hospitalization.
Statistical Analysis
Statistical analysis was performed using IBM SPSS software version 26 (SPSS Inc., Armonk, NY, USA). Descriptive summary statistics are presented as means and SD for continuous variables and frequencies with percentages for categorical variables. Categorical and continuous variables were tested for statistical significance using χ2 tests and t tests, respectively. If the continuous variable is not normally distributed, we utilized the nonparametric test such as the Mann-Whitney U test to compare the groups.
Results
Study Population and Baseline Demographics
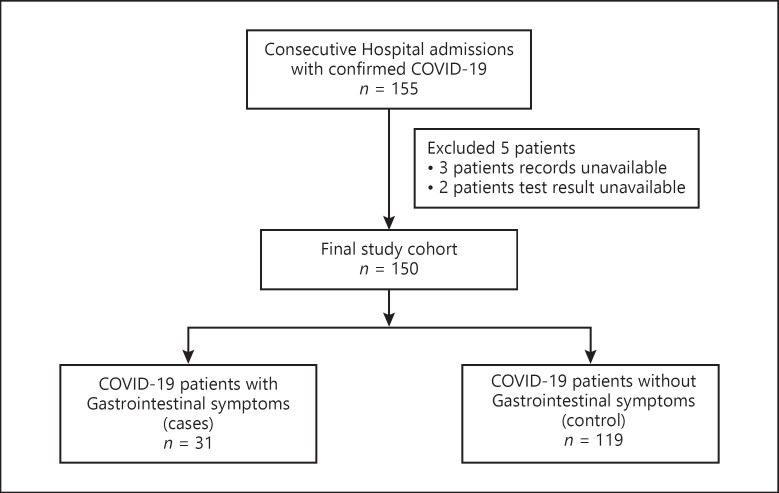
A total of 155 patients were hospitalized with confirmed COVID-19 during the study period. Five patients were excluded based on the exclusion criteria. A total of 150 patients met the inclusion criteria and formed our final study population (Fig. 1). Of these, 31 (20.6%) patients had GI symptoms (cases), and 119 patients had no GI symptoms (controls) (Table 1). Diarrhea was the most common GI symptom, which was reported in 14.7% of the cohort, followed by nausea or vomiting, reported in 10.7% of the patients, and only 2% of the patients had abdominal pain (Table 2). Demographic variables are noted in Table 3. The mean age was 57 years (SD ± 17) in cases as compared to 63 years (SD ± 15 years) in controls. The mean BMI was 31.7 and 30.7 in cases and controls, respectively. Comorbidities such as hypertension, dyslipidemia, chronic obstructive pulmonary disease, asthma, coronary artery disease, DM, and cancer were similarly distributed between 2 groups (Table 3). There was no difference in the presence of other symptoms such as fever, cough, dyspnea, fatigue, and myalgia between the 2 groups.
Fig. 1.
Study flowchart.
Table 2.
Prevalence of individual gastrointestinal (GI) symptoms in the COVID-19 cohort with GI symptoms (cases)
| GI symptoms | N (%) |
|---|---|
| Nausea/vomiting | 6 (19.4) |
| Diarrhea | 15 (48.4) |
| Nausea/vomiting + diarrhea | 7 (22.6) |
| Nausea/vomiting + abdominal pain | 3 (9.7) |
Table 3.
Baseline demographics of the study population
| Characteristic | COVID-19 patients with GI symptoms (N = 31) | COVID-19 patients without GI symptoms (N = 119) | p value |
|---|---|---|---|
| Age, mean (SD) | 57.6 (17.2) | 63.3 (14.6) | 0.06 |
| Age >60 years, n (%) | 16 (53.3) | 74 (64.3) | 0.29 |
| Female gender, n (%) | 12 (38.7) | 55 (46.2) | 0.54 |
| BMI, mean (SD) | 31.7 (8.8) | 30.7 (7.6) | 0.57 |
| Race, n (%) | |||
| White | 3 (9.7) | 3 (2.5) | |
| African American | 23 (74.2) | 90 (75.6) | |
| Hispanic | 1 (3.2) | 12 (10.1) | 0.29 |
| Asian | 1 (3.2) | 6 (5) | |
| Unknown | 3 (9.7) | 8 (6.7) | |
| Comorbidities, n (%) | |||
| Hypertension | 22 (14.7) | 79 (66.4) | 0.67 |
| Dyslipidemia | 10 (32.3) | 44 (37) | 0.68 |
| CAD | 7 (22.6) | 20 (16.8) | 0.44 |
| DM | 12 (38.7) | 52 (43.7) | 0.69 |
| Cancer | 4 (12.9) | 11 (9.2) | 0.51 |
| COPD | 1 (3.2) | 13 (10.9) | 0.30 |
| Asthma | 6 (19.4) | 17 (14.4) | 0.58 |
| Smoker | 4 (12.9) | 13 (10.9) | 0.75 |
| Medications, n (%) | |||
| ACEI/ARB | 11 (35.5) | 38 (31.9) | 0.83 |
| NSAID | 6 (19.4) | 28 (23.5) | 0.81 |
| Aspirin | 6 (19.4) | 42 (35.3) | 0.13 |
| Statin | 12 (38.7) | 58 (48.7) | 0.42 |
| Symptoms, n (%) | |||
| Cough | 23 (74.2) | 76 (63.9) | 0.39 |
| Fever | 22 (71) | 79 (66.4) | 0.67 |
| Dyspnea | 17 (54.8) | 82 (68.9) | 0.20 |
| Fatigue | 19 (61.3) | 61 (51.3) | 0.42 |
| Myalgia | 12 (38.7) | 47 (39.5) | 1.00 |
| Pneumonia | 29 (93.5) | 119 (100) | 0.04 |
COVID-19, coronavirus disease 2019; GI, gastrointestinal; CAD, coronary artery disease; DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; ACEI/ARB, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker; NSAID, non-steroidal anti-inflammatory drug.
Laboratory Data
There was no statistical difference between the 2 groups in values of laboratory data such as mean hemoglobin, WBC, lymphocyte, and platelet counts. The mean ferritin level was lower in the cases than in controls but did not reach statistical significance (777 vs. 951 ng/mL, p = 0.61). Mean CRP, creatinine, and lactic acid levels were higher but not statistically significant in both groups, as noted in Table 4.
Table 4.
Laboratory data of both cohorts at the time of admissiona
| Laboratory test | COVID-19 patients with GI symptoms (N = 31) | COVID-19 patients without GI symptoms (N = 119) | p value |
|---|---|---|---|
| Hemoglobin | 12.6 (2.2) | 13 (1.8) | 0.28 |
| Ferritin | 776.9 (961) | 951.8 (1,253.1) | 0.61 |
| d-dimer | 901.6 (1,380) | 10,661.9 (22,910.3) | 0.36 |
| WBC | 7,200 (2,100) | 7,400 (3,700) | 0.78 |
| Lymphocyte count | 1,000 (617) | 1,168 (681.5) | 0.22 |
| Platelet count | 211,870 (60,531) | 202,190 (76,669) | 0.52 |
| Creatinine | 2.5 (3.7) | 1.8 (2.1) | 0.28 |
| Albumin | 3.9 (0.5) | 3.7 (0.5) | 0.07 |
| CPK | 391.8 (602.8) | 924.5 (3,143.9) | 0.48 |
| Lactate | 2.1 (2.2) | 1.99 (1.7) | 0.78 |
| LDH | 1,134.4 (702.9) | 1,208.1 (734.8) | 0.65 |
| CRP | 13.7 (8.1) | 10.8 (8.1) | 0.15 |
| AST | 71.4 (77.3) | 70.9 (64.1) | 0.97 |
| ALT | 52.1 (63.3) | 51.8 (44.4) | 0.98 |
COVID-19, coronavirus disease 2019; GI, gastrointestinal; CRP, C-reactive protein; AST, aspartate aminotransferase; ALT, alanine aminotransferase. a All the laboratory values are represented as mean (SD).
Outcomes
The outcomes of the study are outlined in Table 5. The patients with the GI symptoms (cases) had higher mortality of 41.9% (13/31 patients) when compared to controls, 37.8% (45/119 patients), but it did not reach statistical significance (p = 0.68). No significant differences were noted in the secondary outcomes − mean LOS (7.8 [SD 4.4] vs. 7.9 days [SD 4.7 days], p = 0.87) and need for mechanical ventilation (29 vs. 26.9%, p = 0.82).
Table 5.
Outcome data of both cohorts at the time of admission
| Characteristic | COVID-19 patients with GI symptoms (N = 31) | COVID-19 patients without GI symptoms (N = 119) | p value |
|---|---|---|---|
| Mortality, n (%) | 13 (41.9) | 45 (37.8) | 0.68 |
| Length of stay, mean (SD) | 7.8 (4.4) | 7.9 (4.7) | 0.87 |
| Mechanical ventilation, n (%) | 9 (29) | 32 (26.9) | 0.82 |
COVID-19, coronavirus disease 2019; GI, gastrointestinal.
Discussion
In this study, we found that 20.6% of the patients hospitalized with COVID-19 presented with at least 1 GI symptom such as diarrhea, nausea, vomiting, or abdominal pain. Diarrhea was the most common GI symptom, followed by nausea/vomiting and abdominal pain. There were no significant differences in terms of patient demographics, comorbid conditions, and presenting laboratory evaluations between patients with and without GI symptoms. Furthermore, there was no association between the GI symptoms and other symptoms such as fever, cough, fatigue, and myalgia.
Our study shows that the prevalence of GI symptoms in COVID-19 patients is 20.6%, which is lower than the prevalence of GI symptoms reported by other studies in the USA and China in the range of 50.5–61.3% [7, 21]. The higher reported rate of GI symptoms in those studies could probably be due to the inclusion of anorexia as one of the GI symptoms. Anorexia is a nonspecific symptom that could be related to an overall infectious or inflammatory process and hence was not included as a specific GI symptom in our study. In a US study by Redd et al. [20], the prevalence of GI symptoms in COVID-19 patients was reported to be as high as 61.3%. In that study, anorexia was reported in 34.8% cases, diarrhea in 33.7%, and nausea in 26.4% cases. In a study by Pan et al. [7] from Wuhan, China, even though about 50% reported having GI symptoms, the majority of these patients had anorexia (78.6%). When anorexia was excluded from the analysis, only 18.6% had specific GI symptoms. A trend of increasing recognition of GI manifestations among COVID-19 patients is noted since its outbreak in Wuhan, China. During the original outbreak in Wuhan, diarrhea was reported in only 3% of the cases [1]. This number increased to 10% in a subsequent study from Wuhan and 25% in a study from Singapore [3, 22]. As awareness is increasing among the health-care workers about the GI manifestations in COVID-19 patients, the reports of the presence of GI symptoms increased in the studies.
In our study, there was no association between the GI symptoms and poor outcomes in COVID-19 patients. Previous studies have reported conflicting findings concerning the presence of GI symptoms and poor outcomes. In the study by Pan et al. [7] from Wuhan, China, patients with digestive symptoms had longer LOS (9 vs. 7.3 days, p = 0.013). Furthermore, this study noted that as the severity and duration of COVID-19 increase, GI symptoms increase as well. In a multicenter study of 191 patients by Zhou et al. [14], the presence of GI symptoms was associated with elevated CRP (7.3 vs. 3.8 mg/L, p = 0.021), elevated alanine aminotransferase (64.1 vs. 46.6 units/L, p = 0.049), and lower hemoglobin levels when compared to patients without GI symptoms. However, in the study by Redd and colleagues [20], there were no differences in clinical outcomes in patients with or without GI symptoms. Also, they reported no significant differences in the leukocyte count, hemoglobin, platelets, coagulation, or liver tests in groups with or without GI symptoms.
Although the specific mechanisms causing GI manifestations in COVID-19 are not entirely known, there are several proposed theories. Intestinal tropism has been noted with SARS-CoV-2, which could be due to its strong affinity to angiotensin-converting enzyme-2 receptors, and angiotensin-converting enzyme-2 receptors are highly expressed in the esophagus and intestinal epithelial cells [23]. Hence, there is a strong possibility of direct small bowel involvement, resulting in direct cytopathic effects causing GI symptoms. Furthermore, Redd et al. [20] noted that loss of smell (anosmia) and loss of taste (ageusia) were commonly associated with nausea (adjusted OR 2.71, 95% CI: 1.21–6.20; p = 0.015) and anorexia (adjusted OR 3.70, 95% CI: 1.49–9.16; p = 0.0048) after controlling for potential confounders. While the exact cause of this association is unclear, it could be due to damage to olfactory and gustatory receptors during viral entry through nasal and oral routes [24]. Additionally, in a study from Hong Kong, patients with diarrhea on presentation had higher rates of stool RNA positivity when compared to those without diarrhea (38.5 vs. 8.7%, p = 0.02). This is suggestive of the direct effects of the SARS-CoV-2 on the GI tract [16]. Also, the viral infection can cause altered intestinal permeability, resulting in malabsorption [25]. Finally, the inflammatory response from a cytokine storm in severe COVID-19 patients can cause hypoxia-induced bowel ischemia and contribute to diarrhea.
Specific limitations to this study include the retrospective design, relatively small sample, single-center hospital-based study, and lack of validated symptom instruments. This could introduce selection bias and limit the reliability and generalizability of the results. We could not correlate the presence of SARS-CoV-2 RNA with GI symptoms since this test was not routinely performed in our institution. Despite these limitations, the main strengths of this study are that it has validated the findings of another US study by Redd et al. [20] on GI manifestations in COVID-19. Our study also presents data from New York with a significantly higher proportion of African American patients. We also included data on home medications such as non-steroidal anti-inflammatory drugs and angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, which has not been presented in previous studies.
Conclusion
GI symptoms are commonly encountered in hospitalized COVID-19 patients. In our study, GI symptoms were not associated with poorer outcomes such as increased mortality, longer hospital LOS, and increased mechanical intubation in COVID-19 patients. It appears that the GI symptoms could potentially be a bystander in patients with COVID-19. Further, more extensive studies are needed to evaluate the effects of GI symptoms on outcomes in COVID-19.
Statement of Ethics
The BHMCNY's Institutional Review Board approved this study as minimal-risk research while utilizing anonymized and de-identified retrospective data collection and waived the requirement for informed consent.
Conflict of Interest Statement
All authors have no conflicts of interest or financial ties to disclose.
Funding Sources
The authors did not receive any funding.
Author Contributions
P.R., A.P., and H.G.: Conception and design. P.R., I.O., and S.G.: Data collection. A.P. and M.G.: Drafting manuscript. P.R., I.O., S.G., M.G., A.A., H.G., and A.A.: Literature review, critical revision, and final approval of the manuscript.
Availability of Data and Material
This own work has been deposited in a pre-print repository [26].
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395((10223)):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santarpia JL, Rivera DN, Herrera V, Morwitzer MJ, Creager H, Santarpia GW, et al. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center
- 3.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 Feb 7;323((11)):1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aloysius M, Thatti A, Gupta A. COVID-19 presenting as acute pancreatitis. Pancreatology. 2020;S1424–3903((20)):30154. doi: 10.1016/j.pan.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gao QY, Chen YX, Fang JY. 2019 novel coronavirus infection and gastrointestinal tract. J Dig Dis. 2020 Mar;21((3)):125–6. doi: 10.1111/1751-2980.12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kopel J, Perisetti A, Gajendran M, Boregowda U, Goyal H. Clinical insights into the gastrointestinal manifestations of COVID-19. Dig Dis Sci. 2020 Jul;65((7)):1932–9. doi: 10.1007/s10620-020-06362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020 Apr 14;115((5)):766–73. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perisetti A, Gajendran M, Goyal H. Putative mechanisms of diarrhea in COVID-19. Clin Gastroenterol Hepatol. 2020 Jun 11;S1542–3565((20)):30708–1. doi: 10.1016/j.cgh.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aziz M, Perisetti A, Lee-Smith W, Gajendran M, Bansal P, Goyal H. Taste changes (dysgeusia) in COVID-19: a systematic review and metaanalysis. Gastroenterology. 2020 May 5;S0016–5085((20)):30595–3. doi: 10.1053/j.gastro.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giacomelli A, Pezzati L, Conti F, Bernacchia D, Siano M, Oreni L, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis. 2020 Mar 26;:ciaa330. doi: 10.1093/cid/ciaa330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 Feb 15;395((10223)):507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Worldometer-age, sex, existing conditions of COVID-19 cases and deaths. Available from: https://www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/
- 13.Perisetti A, Gajendran M, Boregowda U, Bansal P, Goyal H. COVID-19 and gastrointestinal endoscopies: current insights and emergent strategies. Dig Endosc. 2020 Apr 13; doi: 10.1111/den.13693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395((10229)):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323((20)):2052–9. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheung KS, Hung IF, Chan PP, Lung KC, Tso E, Liu R, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong cohort and systematic review and meta-analysis. Gastroenterology. 2020 Apr 3;S0016–5085((20)):30448–0. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perisetti A, Garg S, Inamdar S, Tharian B. Role of face mask in preventing bacterial exposure to the endoscopist's face. Gastrointest Endosc. 2019 Nov;90((5)):859. doi: 10.1016/j.gie.2019.06.016. [DOI] [PubMed] [Google Scholar]
- 18.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Apr 30;382((18)):1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang W, Feng Z, Rao S, Xiao C, Xue X, Lin Z, et al. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. Gut. 2020 Jun;69((6)):1141–3. doi: 10.1136/gutjnl-2020-320832. [DOI] [PubMed] [Google Scholar]
- 20.Redd WD, Zhou JC, Hathorn KE, McCarty TR, Bazarbashi AN, Thompson CC, et al. Prevalence and characteristics of gastrointestinal symptoms in patients with SARS-CoV-2 infection in the United States: a multicenter cohort study. Gastroenterology. 2020 Apr 22;S0016–5085((20)):30564–3. doi: 10.1053/j.gastro.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han C, Duan C, Zhang S, Spiegel B, Shi H, Wang W, et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020 Jun;115((6)):916–23. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020 Mar 3;323((15)):1488–94. doi: 10.1001/jama.2020.3204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zou X, Chen K, Zou J, Han P, Hao J, Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med. 2020 Apr;14((2)):185–92. doi: 10.1007/s11684-020-0754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaira L, Salzano G, Deiana G, De Riu G. Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope. 2020 Jul;130((7)):1787. doi: 10.1002/lary.28692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020 Mar 3;158((6)):1518–9. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramachandran P, Onukogu I, Ghanta S, Gajendran M, Perisetti A, Goyal H, et al. Gastrointestinal Symptoms and outcomes in hospitalized COVID-19 patients. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This own work has been deposited in a pre-print repository [26].