Abstract
Background
The pandemic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) might be curtailed by vaccination. We assessed the safety, reactogenicity, and immunogenicity of a viral vectored coronavirus vaccine that expresses the spike protein of SARS-CoV-2.
Methods
We did a phase 1/2, single-blind, randomised controlled trial in five trial sites in the UK of a chimpanzee adenovirus-vectored vaccine (ChAdOx1 nCoV-19) expressing the SARS-CoV-2 spike protein compared with a meningococcal conjugate vaccine (MenACWY) as control. Healthy adults aged 18–55 years with no history of laboratory confirmed SARS-CoV-2 infection or of COVID-19-like symptoms were randomly assigned (1:1) to receive ChAdOx1 nCoV-19 at a dose of 5 × 1010 viral particles or MenACWY as a single intramuscular injection. A protocol amendment in two of the five sites allowed prophylactic paracetamol to be administered before vaccination. Ten participants assigned to a non-randomised, unblinded ChAdOx1 nCoV-19 prime-boost group received a two-dose schedule, with the booster vaccine administered 28 days after the first dose. Humoral responses at baseline and following vaccination were assessed using a standardised total IgG ELISA against trimeric SARS-CoV-2 spike protein, a muliplexed immunoassay, three live SARS-CoV-2 neutralisation assays (a 50% plaque reduction neutralisation assay [PRNT50]; a microneutralisation assay [MNA50, MNA80, and MNA90]; and Marburg VN), and a pseudovirus neutralisation assay. Cellular responses were assessed using an ex-vivo interferon-γ enzyme-linked immunospot assay. The co-primary outcomes are to assess efficacy, as measured by cases of symptomatic virologically confirmed COVID-19, and safety, as measured by the occurrence of serious adverse events. Analyses were done by group allocation in participants who received the vaccine. Safety was assessed over 28 days after vaccination. Here, we report the preliminary findings on safety, reactogenicity, and cellular and humoral immune responses. The study is ongoing, and was registered at ISRCTN, 15281137, and ClinicalTrials.gov, NCT04324606.
Findings
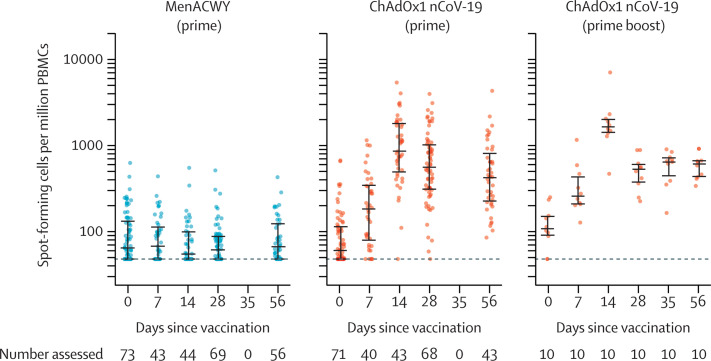
Between April 23 and May 21, 2020, 1077 participants were enrolled and assigned to receive either ChAdOx1 nCoV-19 (n=543) or MenACWY (n=534), ten of whom were enrolled in the non-randomised ChAdOx1 nCoV-19 prime-boost group. Local and systemic reactions were more common in the ChAdOx1 nCoV-19 group and many were reduced by use of prophylactic paracetamol, including pain, feeling feverish, chills, muscle ache, headache, and malaise (all p<0·05). There were no serious adverse events related to ChAdOx1 nCoV-19. In the ChAdOx1 nCoV-19 group, spike-specific T-cell responses peaked on day 14 (median 856 spot-forming cells per million peripheral blood mononuclear cells, IQR 493–1802; n=43). Anti-spike IgG responses rose by day 28 (median 157 ELISA units [EU], 96–317; n=127), and were boosted following a second dose (639 EU, 360–792; n=10). Neutralising antibody responses against SARS-CoV-2 were detected in 32 (91%) of 35 participants after a single dose when measured in MNA80 and in 35 (100%) participants when measured in PRNT50. After a booster dose, all participants had neutralising activity (nine of nine in MNA80 at day 42 and ten of ten in Marburg VN on day 56). Neutralising antibody responses correlated strongly with antibody levels measured by ELISA (R2=0·67 by Marburg VN; p<0·001).
Interpretation
ChAdOx1 nCoV-19 showed an acceptable safety profile, and homologous boosting increased antibody responses. These results, together with the induction of both humoral and cellular immune responses, support large-scale evaluation of this candidate vaccine in an ongoing phase 3 programme.
Funding
UK Research and Innovation, Coalition for Epidemic Preparedness Innovations, National Institute for Health Research (NIHR), NIHR Oxford Biomedical Research Centre, Thames Valley and South Midland's NIHR Clinical Research Network, and the German Center for Infection Research (DZIF), Partner site Gießen-Marburg-Langen.
Research in context.
Evidence before this study
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified as the causative agent of COVID-19 in January, 2020. There are currently no licensed vaccines to prevent COVID-19. ChAdOx1 nCoV-19 has previously been reported to be immunogenic and protective against pneumonia in a rhesus macaque challenge model. We searched PubMed for research articles published between database inception and July 6, 2020, using the terms “SARS-CoV-2”, “vaccine”, “clinical trial”, and “phase”. No language restrictions were applied. We identified one published clinical trial, describing a trial done in China of an adenovirus-5-vectored vaccine against SARS-CoV-2, using a single dose at three different dose levels. The vaccine was tolerated, with reactogenicity increased at the highest dose. Antibodies, neutralising antibodies in a proportion of vaccinees, and cellular responses were induced. A further clinical trial, which was done in the USA, has been reported on medRxiv. The vaccine was a lipid nanoparticle-formulated, nucleoside-modified, mRNA vaccine that encodes trimerised SARS-CoV-2 spike glycoprotein receptor binding domain administered at one or two doses of three dose levels. The vaccine was tolerated, with reactogenicity increased at the highest dose. Antibodies and neutralising antibodies were induced in a dose-dependent manner and increased after a second dose.
Added value of this study
We report the results of the first clinical study of ChAdOx1 nCoV-19 (AZD1222). The vaccine was safe and tolerated, with reduced reactogenicity when paracetamol was used prophylactically for the first 24 h after vaccination. Reactogenicity was reduced after a second dose. Humoral responses to SARS-CoV-2 spike protein peaked by day 28 post prime and cellular responses were induced in all participants by day 14. Neutralising antibodies were induced in all participants after a second vaccine dose. After two doses, potent cellular and humoral immunogenicity was present in all participants studied.
Implications of all the available evidence
A vaccine against SARS-CoV-2 could be used to prevent infection, disease, and death in the global population, with high-risk populations such as hospital workers and older adults (eg, ≥65 years of age) prioritised to receive vaccination. The immune correlates of protection against SARS-CoV-2 have not yet been determined. Immunisation with ChAdOx1 nCoV-19 results in rapid induction of both humoral and cellular immune responses against SARS-CoV-2, with increased responses after a second dose. Further clinical studies, including in older adults, should be done with this vaccine.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged as a zoonotic virus late in 2019 and is the causative agent of COVID-19. Exposure to SARS-CoV-2 can result in a range of clinical outcomes, varying from asymptomatic infection to severe acute respiratory distress and death. SARS-CoV-2 has spread globally and was declared a pandemic on March 11, 2020, by WHO. As of July 19, 2020, more than 14 million people globally have been infected with more than 597 000 deaths.1 The pandemic has placed substantial pressures on health systems delivering care for patients with COVID-19 and caused disruption of non-COVID-19 health-care provision, in addition to negative effects on the global economy. Further health consequences are anticipated.
No vaccines have been approved for prevention of COVID-19. There are currently more than 137 candidates undergoing preclinical development and 23 in early clinical development, according to WHO.2 An ideal vaccine against SARS-CoV-2 would be effective after one or two vaccinations; would protect target populations such as older adults and those with comorbidities, including immunocompromised individuals; would confer protection for a minimum of 6 months; and would reduce onward transmission of the virus to contacts. Replication-deficient viral vectored vaccines have been used in immunocompromised individuals with no safety concerns3, 4, 5 and ChAdOx1 vaccines are immunogenic in older adults6 and can be manufactured at large scale, making this platform technology a promising candidate to develop a vaccine for the prevention of COVID-19. Adenoviral vectors have previously been combined with DNA and poxviral vectors to attempt to improve immunogenicity, with adenovirus or modified vaccinia virus Ankara prime-boost regimens showing enhancement of both cellular and humoral immunity. Use of homologous adenoviral regimens has largely been avoided because of presumed induction of antivector immunity, inhibiting the potency of a second dose.
Coronaviruses are enveloped, positive sense single-stranded RNA viruses with a glycoprotein spike on the surface, which mediates receptor binding and cell entry during infection. The roles of the spike protein in receptor binding and membrane fusion make it an attractive vaccine antigen. We have previously shown that a single dose of ChAdOx1 MERS, a chimpanzee adenovirus-vectored vaccine that encodes the spike protein of Middle East respiratory syndrome coronavirus (MERS-CoV), protected non-human primates against MERS-CoV-induced disease,7 and data from a phase 1 clinical trial showed that ChAdOx1 MERS was safe and well tolerated at all three doses tested (5 × 109 viral particles, 2·5 × 1010 viral particles, and 5 × 1010 viral particles).8 In addition, the highest dose elicited both humoral and cellular responses against MERS-CoV in all vaccinees within 1 month of vaccination.
The ChAdOx1 nCoV-19 vaccine (AZD1222) consists of the replication-deficient simian adenovirus vector ChAdOx1, containing the full-length structural surface glycoprotein (spike protein) of SARS-CoV-2, with a tissue plasminogen activator leader sequence. ChAdOx1 nCoV-19 expresses a codon-optimised coding sequence for the spike protein (GenBank accession number MN908947).
In rhesus macaques, a single vaccination with ChAdOx1 nCoV-19 induced humoral and cellular immune responses. Protection against lower respiratory tract infection was observed in vaccinated non-human primates after high-dose SARS-CoV-2 challenge.9
We did a phase 1/2 single-blind, randomised controlled trial of ChAdOx1 nCoV-19 compared with a licensed meningococcal group A, C, W-135, and Y conjugate vaccine (MenACWY; Nimenrix, Pfizer, UK), as control vaccine, in healthy adults in the UK. In this preliminary report, we describe the immunogenicity, reactogenicity, and safety of vaccination with 5 × 1010 viral particles of ChAdOx1 nCoV-19 in single-dose and two-dose regimens.
Methods
Study design and participants
This phase 1/2, participant-blinded, multicentre, randomised controlled trial is being done at five centres in the UK (Centre for Clinical Vaccinology and Tropical Medicine, University of Oxford; NIHR Southampton Clinical Research Facility, University Hospital Southampton NHS Foundation Trust, Southampton; Clinical Research Facility, Imperial College London; St Georges University of London and University Hospital NHS Foundation Trust; and University Hospitals Bristol and Weston NHS Foundation Trust). Healthy adult participants aged 18–55 years were recruited through local advertisements. All participants underwent a screening visit where a full medical history and examination was taken in addition to blood and urine tests (HIV; hepatitis B and C serology; full blood count; kidney and liver function tests; and urinary screen for blood, protein, and glucose and a pregnancy test done in women of childbearing potential). Volunteers with a history of laboratory confirmed SARS-CoV-2 infection; those at higher risk for SARS-CoV-2 exposure pre-enrolment (ie, front-line health-care workers working in emergency departments, intensive care units, and COVID-19 wards, and close contacts of confirmed COVID-19 cases; see appendix 1 p 82 for further details); and those with a new onset of fever, cough, shortness of breath, and anosmia or ageusia since Feb 1, 2020, were excluded from the study. An amendment to the study protocol (amendment date April 21, 2020) allowed for recruitment of health-care workers with a negative SARS-CoV-2 serology at screening, once an antibody test became available. As it was not possible to screen for negative SARS-CoV-2 serology in all participants, some enrolled participants had high-level anti-spike antibodies at baseline and their data are included in all analyses. Full details of the eligibility criteria are described in the trial protocol provided in the appendix 1 (pp 80–82).
Written informed consent was obtained from all participants, and the trial is being done in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice. This study was approved in the UK by the Medicines and Healthcare products Regulatory Agency (reference 21584/0424/001-0001) and the South Central Berkshire Research Ethics Committee (reference 20/SC/0145). Vaccine use was authorised by Genetically Modified Organisms Safety Committees at each participating site.
Randomisation and masking
Participants were randomly assigned (1:1) to receive either the ChAdOx1 nCoV-19 vaccine or the MenACWY vaccine. MenACWY was used as a comparator vaccine to maintain blinding of participants who experienced local or systemic reactions, since these reactions are a known association with viral vector vaccinations. Use of saline as a placebo would risk unblinding participants as those who had notable reactions would know they were in the ChAdOx1 nCoV-19 vaccine group.
Randomisation lists, using block randomisation stratified by study group and study site, were generated by the study statistician (MV). Block sizes of two and four were chosen to align with the study group sizes and the sequence of enrolment, and varied across study groups. Computer randomisation was done with full allocation concealment within the secure web platform used for the study electronic case report form (REDCap version 9.5.22; Vanderbilt University, Nashville, TN, USA). The trial staff administering the vaccine prepared vaccines out of sight of the participants and syringes were covered with an opaque material until ready for administration to ensure blinding of participants. Clinical investigators and the laboratory team remained blinded to group allocation.
Procedures
The recombinant adenovirus for ChAdOx1 nCoV-19 was produced as previously described.10 The vaccine was manufactured according to current Good Manufacturing Practice by the Clinical BioManufacturing Facility (University of Oxford, Oxford, UK) as previously described,11 with only minor modifications, as described in the Investigational Medicinal Product Dossier and approved by the regulatory agency in the UK. ChAdOx1 nCoV-19 was administered at a dose of 5 × 1010 viral particles. The MenACWY vaccine was provided by the UK Department of Health and Social Care and administered as per summary of product characteristics at the standard dose of 0·5 mL. Vaccines were administered as a single intramuscular injection into the deltoid.
Participants were recruited and followed up according to groups. Participants were recruited first for groups 1 and 3, then group 2, and then group 4. Group 1 (the phase 1 component of the study) consisted of participants who had intensive early follow-up visits for safety and immunogenicity purposes at days 3, 7, 14, 28, and 56 after vaccination. Group 2 consisted of participants who had higher blood volumes drawn for humoral and cellular immunogenicity assessment than group 4, which consisted of participants who had a serum sample drawn for humoral immunology assessments only. Group 3 consisted of ten participants who were enrolled in a non-randomised prime-boost group and received a booster ChAdOx1 nCoV-19 administered 28 days after the first dose. These participants were not blinded and had extensive follow-up for safety and immunogenicity purposes, as per group 1, after each dose. A staggered-enrolment approach was used for the first two, six, and 90 participants recruited in groups 1 and 3 (appendix 1 p 89) and interim safety reviews with the independent Data and Safety Monitoring Board were done before proceeding with vaccinations in larger numbers of volunteers. Volunteers were considered enrolled into the trial at the point of vaccination.
Participants in all groups had blood samples drawn and clinical assessments for safety as well as immunology at days 0 and 28, and will also be followed up at days 184 and 364. A later amendment to the protocol (amendment date June 22, 2020) provided for additional testing of booster vaccinations in a subset of participants, the results of which are not yet available and are not included in this Article.
In two of the five trial sites (Oxford and Southampton), a protocol amendment (amendment date May 6, 2020) was implemented to allow prophylactic paracetamol to be administered before vaccination and participants were advised to continue with 1 g of paracetamol every 6 h for 24 h to reduce vaccine-associated reactions. All participants enrolled after the protocol amendment at these two sites were given prophylactic paracetamol and randomised equally to the vaccine or control arms of the study.
Participants were observed in the clinic for 30–60 min after the vaccination procedure and were asked to record any adverse events using electronic diaries during the 28-day follow-up period. Expected and protocol-defined local site reactions (injection site pain, tenderness, warmth, redness, swelling, induration, and itch) and systemic symptoms (malaise, muscle ache, joint pain, fatigue, nausea, headache, chills, feverishness [ie, a self-reported feeling of having a fever], and objective fever defined as an oral temperature of 38°C or higher) were recorded for 7 days. All other events were recorded for 28 days and serious adverse events are recorded throughout the follow-up period.
Severity of adverse events are graded with the following criteria: mild (transient or mild discomfort for <48 h, no interference with activity, and no medical intervention or therapy required), moderate (mild to moderate limitation in activity [some assistance might be needed] and no or minimal medical intervention or therapy required), severe (marked limitation in activity [some assistance usually required] and medical intervention or therapy required), and potentially life-threatening (requires assessment in emergency department or hospitalisation). Unsolicited adverse events are reviewed for causality by two clinicians blinded to group allocation, and events considered to be possibly, probably, or definitely related to the study vaccines were reported. Laboratory adverse events were graded by use of site-specific toxicity tables, which were adapted from the US Food and Drug Administration toxicity grading scale.
Cellular responses were assessed using an ex-vivo interferon-γ enzyme-linked immunospot (ELISpot) assay to enumerate antigen-specific T cells. Humoral responses at baseline and following vaccination were assessed using a standardised total IgG ELISA against trimeric SARS CoV-2 spike protein, a muliplexed immunoassay (Meso Scale Discovery multiplexed immunoassay [MIA] against spike and receptor binding domain), three live SARS-CoV-2 neutralisation assays (Public Health England [PHE] plaque reduction neutralisation test [PRNT IC50], PHE microneutralisation assay [MNA IC50, IC80, IC90], and Marburg virus neutralisation [VN IC100]), and a pseudovirus neutralisation assay (PseudoNA IC50). PHE PRNT is a live neutralisation assay and was done at PHE (Porton Down, UK). PHE MNA is a rapid microneutralisation assay, which was conducted in the same laboratory. The third assay, Marburg VN, was conducted at Marburg University (Marburg, Germany). Full details on the assays are provided in the appendix 1 (pp 31–34). Owing to the labour-intensive nature of some of these assays, we prioritised analysis of samples from the ChAdOx1 nCoV-19 group, randomly selecting more samples from ChAdOx1 nCoV-19 participants than control samples to be sent for analysis.
Convalescent plasma samples from adults (≥18 years) with PCR-positive SARS-CoV-2 infection were obtained from symptomatic patients admitted to hospital or from surveillance on health-care workers who did not have symptomatic infection. These samples were tested using standardised ELISA, MIA, PseudoNA, and Marburg VN. Different samples were analysed across the assays, dependent on sample availability, laboratory capacity, and assay-specific requirements. Where multiple longitudinal samples were available for the same participant, only one timepoint is included in the analyses in this Article and the earliest timepoint (at least 20 days after initial symptoms) was selected.
Outcomes
The co-primary outcomes are to assess efficacy as measured by cases of symptomatic virologically confirmed COVID-19 and safety of the vaccine as measured by the occurrence of serious adverse events. Secondary outcomes include safety, reactogenicity, and immunogenicity profiles of ChAdOx1 nCoV-19, and efficacy against hospital-attended COVID-19, death, and seroconversion against non-spike proteins (appendix 1 pp 72–73). Preliminary results for secondary endpoints are reported here: occurrence of local and systemic reactogenicity signs and symptoms for 7 days after vaccination; occurrence of unsolicited adverse events for 28 days after vaccination; change from day 0 (baseline) to day 28 for safety laboratory measures; and cellular and humoral immunogenicity of ChAdOx1 nCoV-19. Neutralising antibodies and laboratory adverse events were tested on participants in groups 1 and 3 only. Unsolicited adverse events are reported for group 1 only.
The convalescent sample collection of PCR-positive hospitalised patients with COVID-19 or asymptomatic health-care workers was done to characterise the immunological properties of COVID-19 and not for the purposes of the clinical trial (Gastrointestinal Illness in Oxford: COVID substudy [Sheffield Research Ethics Committee reference: 16/YH/0247], ISARIC/WHO Clinical Characterisation Protocol for Severe Emerging Infections [Oxford Research Ethics Committee C reference 13/SC/0149], and Sepsis Immunomics project [Oxford Research Ethics Committee C, reference 19/SC/0296]).
Statistical analysis
Safety endpoints are described as frequencies (%) with 95% binomial exact CIs. Medians and IQRs are presented for immunological endpoints and analyses are considered descriptive only, as the full set of samples have not yet been analysed on all platforms and therefore results reported here are preliminary. Participants were analysed according to the group to which they were randomised. To assess the effect of prophylactic paracetamol use, the occurence of adverse reactions in the first 2 days after vaccination was analysed as a binary variable using adjusted logistic regression with results presented as adjusted odds ratios. The model adjusted for age, sex, occupation (health-care worker or not), smoking, alcohol consumption, and body-mass index. To assess the relationship between responses on different assays, linear regression was used to analyse log-transformed post-baseline values. Statistical analyses were done using SAS version 9.4 and R version 3.6.1 or later.
The sample size for the study was determined by the number of doses of vaccine that were available for use after the initial clinical manufacturing process. Sample sizes for efficacy are based on the number of primary outcome events that accrue and are presented in the protocol (appendix pp 1 116–117). Efficacy analyses have not yet been done and are not included in this Article.
An independent data and safety monitoring board provided safety oversight (appendix 1 p 46). This study is registered with ClinicalTrials.gov, NCT04324606, and with ISRCTN, 15281137.
Role of the funding source
The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between April 23 and May 21, 2020, 1077 participants were enrolled into the study and assigned to vaccination with either ChAdOx1 nCoV-19 (n=543) or MenACWY (n=534; appendix 1 p 3); ten of these participants were enrolled in group 3, the prime-boost group, and thus were not randomly assigned. 88 participants were included in group 1, 412 in group 2, and 567 in group 4 (appendix 1 p 3). All randomised participants were vaccinated; one participant in the MenACWY group received the ChAdOx1 nCoV-19 vaccine (appendix 1 p 3).
The median age of participants was 35 years (IQR 28–44 years), 536 (49·8%) participants were female and 541 (50·2%) were male, and the majority of participants (979 [90·9%]) were white (appendix 1 p 4). Baseline characteristics seemed similar between randomised groups (appendix 1 p 4).
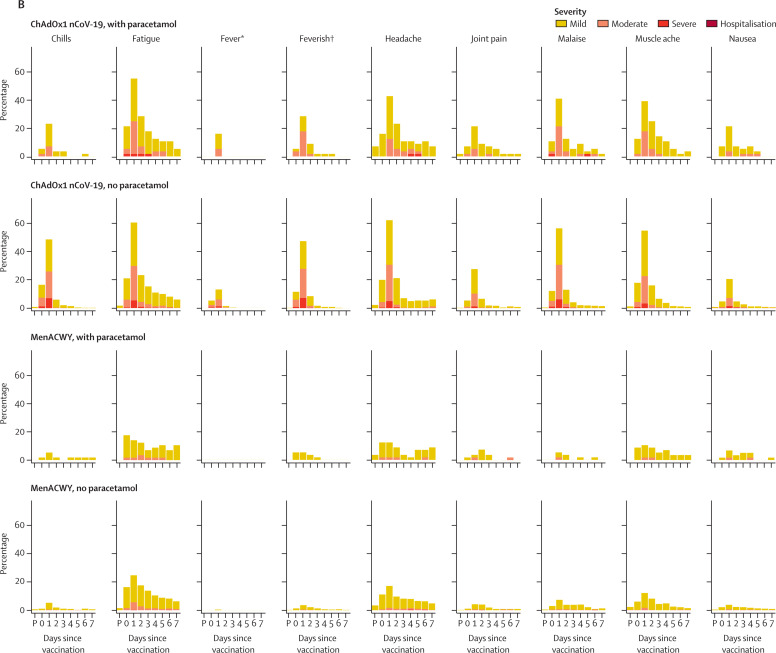
56 participants in the ChAdOx1 nCoV-19 group and 57 in the MenACWY group received prophylactic paracetamol. In those who did not receive prophylactic paracetamol, 328 (67%) of 487 participants in the ChAdOx1 nCoV-19 group and 180 (38%) of 477 participants in the MenACWY group reported pain after vaccination, which was mostly mild to moderate in intensity (appendix 1 pp 5–7). With prophylactic paracetamol, pain was reported by fewer participants: 28 (50%) in the ChAdOx1 nCoV-19 group and 18 (32%) in the MenACWY group. Tenderness of mostly mild intensity was reported in the ChAdOx1 nCoV-19 group by 403 (83%) participants without paracetamol and 43 (77%) with paracetamol, and in the MenACWY group by 276 (58%) participants without paracetamol and 26 (46%) with paracetamol (figure 1 ; appendix 1 pp 5–7).
Figure 1.
Solicited local (A) and systemic (B) adverse reactions in first 7 days after vaccination as recorded in participant symptom electronic diaries
Day 0 is the day of vaccination. P=60-min post-vaccination observation period in the clinic. MenACWY=meningococcal group A, C, W-135, and Y conjugate vaccine. *Mild: 38·0°C to <38·5°C; moderate: 38·5°C to <39·0°C; severe: ≥39·0°C. †Self-reported feeling of feverishness.
Fatigue and headache were the most commonly reported systemic reactions. Fatigue was reported in the ChAdOx1 nCoV-19 group by 340 (70%) participants without paracetamol and 40 (71%) with paracetamol and in the MenACWY group by 227 (48%) participants without paracetamol and 26 (46%) with paracetamol, whereas headaches were reported in the ChAdOx1 nCoV-19 group by 331 (68%) participants without paracetamol and 34 (61%) with paracetamol and in the MenACWY group by 195 (41%) participants without paracetamol and 21 (37%) participants with paracetamol.
Other systemic adverse reactions were common in the ChAdOx1 nCoV-19 group: muscle ache (294 [60%] participants without paracetamol and 27 [48%] with paracetamol), malaise (296 [61%] and 27 [48%]), chills (272 [56%] and 15 [27%]); and feeling feverish (250 [51%] and 20 [36%]). In the of ChAdOx1 nCoV-19 group, 87 (18%) participants without paracetamol and nine (16%) participants with paracetamol reported a temperature of at least 38°C, and eight (2%) patients without paracetamol had a temperature of at least 39°C. In comparison, two (<1%) of those receiving MenACWY reported a fever of at least 38°C, none of whom were receiving prophylactic paracetamol (figure 1; appendix 1 pp 5–7).
The severity and intensity of local and systemic reactions was highest on day 1 after vaccination (figure 1).
Adjusted analysis of the effect of prophylactic paracetamol on adverse reactions of any severity in the first 2 days after vaccination with ChAdOx1 nCoV-19 showed significant reductions in pain, feeling feverish, chills, muscle ache, headache, and malaise (appendix 1 pp 10–11).
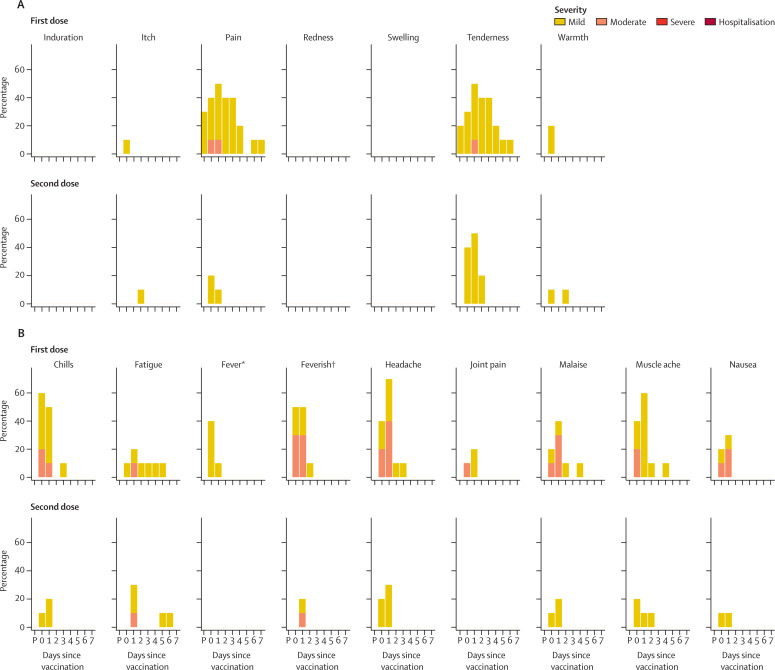
All ten participants in the prime-boost group received their booster vaccine at day 28; solicited local and systemic reactions were measured in these participants for 7 days after both the prime and booster doses. The reactogenicity profile after the second dose appeared less severe in this subset, although the small number of participants in this group led to wide CIs (figure 2 ; appendix 1 pp 8–9).
Figure 2.
Solicited local (A) and systemic (B) adverse reactions in first 7 days after priming and booster doses of ChAdOx1 nCoV-19 in the non-randomised subset of ten participants
Day 0 is the day of vaccination. P=60-min post-vaccination observation period in the clinic. *Mild: 38·0°C to <38·5°C; moderate: 38·5°C to <39·0°C; severe: ≥39·0°C. †Self-reported feeling of feverishness.
Unsolicited adverse events in the 28 days following vaccination considered to be possibly, probably, or definitely related to ChAdOx1 nCoV-19 were predominantly mild and moderate in nature and resolved within the follow-up period (appendix 1 pp 12–15). Laboratory adverse events considered to be at least possibly related to the study intervention were self-limiting and predominantly mild or moderate in severity (data not shown). Transient haematological changes from baseline (neutropenia) were observed in 25 (46%) of 54 participants in the ChAdOx1 nCoV-19 group compared with three (7%) of 44 participants in the MenACWY group. There was one serious adverse event in the MenACWY group consisting of a new diagnosis of haemolytic anaemia, occurring 9 days after vaccination. The participant was clinically well throughout the study. The event was reported as a suspected unexpected serious adverse reaction relating to the MenACWY vaccine.
In the ChAdOx1 nCoV-19 group, antibodies against SARS-CoV-2 spike protein peaked by day 28 (median 157 ELISA units [EU], IQR 96–317; n=127) and remained elevated to day 56 (119 EU, 70–203; n=43) in participants who received only one dose, and increased to a median of 639 EU (360–792) at day 56 in the ten participants who received a booster dose (figure 3 ).
Figure 3.
SARS-CoV-2 IgG response by standardised ELISA to spike protein in trial participants (A) and in 180 convalescent plasma samples from 172 patients with PCR-confirmed COVID-19 and eight asymptomatic health-care workers (B)
Error bars show median (IQR). Participants in the prime boost group received their second dose at day 28. Lower limit of quantification is 1 ELISA unit. Red stars in panel B show five samples also tested on the Marburg VN assay (see figure 4). MenACWY=meningococcal group A, C, W-135, and Y conjugate vaccine. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
Similar increases in serum antibody levels to both the spike protein and the receptor binding domain by day 28 and after a booster dose were observed when measured by MIA (appendix 1 p 16). Immunogenicity among those who were advised to take paracetamol prophylactically was similar to that seen among those who were not advised to use it prophylactically (data not shown).
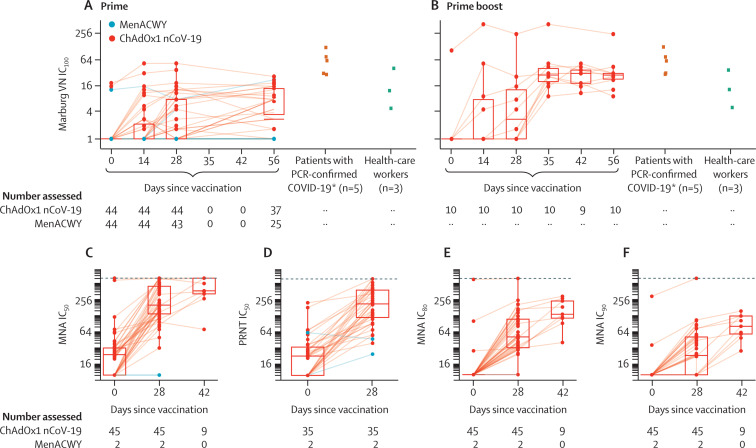
In the PHE PRNT50 assay, which determined the extent to which serum can be diluted and still reduce SARS-CoV-2 plaque formation by 50%, 35 (100%) of 35 participants achieved neutralising titres with a median titre of 218 (IQR 122–395) at day 28 and similar results were obtained with the PHE MNA80 assay, with titres inducing 80% virus neutralisation achieved in 32 (91%) of 35 participants after one dose (median titre 51, 32–103), and in nine (100%) of nine participants after the booster dose (median titre 136, 115–241; figure 4 ; appendix 1 pp 17–19). In the Marburg VN assay, 23 (62%) of 37 recipients had neutralising antibodies that induced complete inhibition of the cytopathic effect caused by SARS-CoV-2 by day 56 after one dose, as did ten (100%) of ten participants after a booster dose, with a median titre of 29 (24–32; figure 4).
Figure 4.
Live SARS-CoV-2 neutralisation assays (Marburg VN and PHE PRNT50) and microneutralisation assays (PHE MNA)
Panels A and B show live SARS-CoV-2 neutralisation (Marburg VN) in prime (A) and prime boost (B) trial participants (boosted at day 28) and convalescent plasma from patients with PCR-confirmed COVID-19 and asymptomatic health-care workers. Panels C, E, and F show the PHE MNA (at IC50, IC80, and IC90, respectively) and panel D the PHE PRNT50. The day 42 timepoint was only measured in participants who received a booster dose at day 28. Solid lines connect samples from the same participant. Boxes show median (IQR). Dotted lines show upper limits of detection. MenACWY=meningococcal group A, C, W-135, and Y conjugate vaccine. PHE=Public Health England. MNA=microneutralisation assay. PRNT=plaque reduction neutralisation test. VN=virus neutralisation. IC=inhibitory concentration. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2. *ELISA results for these five convalescent plasma samples are shown in figure 3 as red stars.
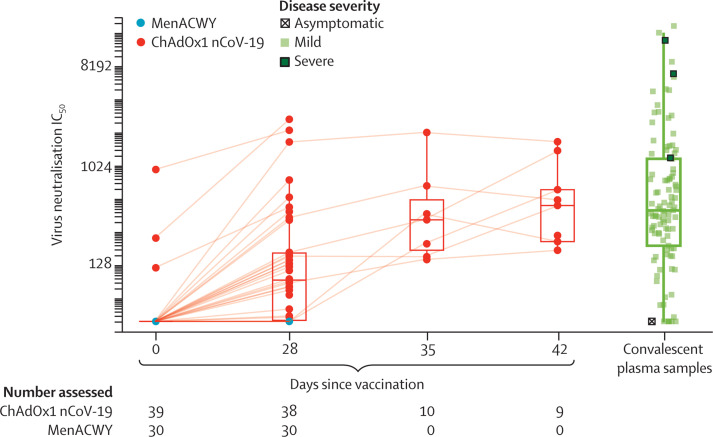
Titres from the PseudoNA assay and the Marburg VN assay correlated positively with other live virus neutralisation assay titres and with ELISA (PseudoNA R 2=0·53 and Marburg VN R 2=0·67; both p<0·001; Figure 4, Figure 5 ; appendix 1 pp 20–21). We included responses following natural exposure as a point of reference for vaccine response data, and found that vaccine-induced responses were in a similar range (figure 5). Interferon-γ ELISpot responses against SARS-CoV-2 spike peptides peaked at 856 spot-forming cells per million peripheral blood mononuclear cells (IQR 493–1802; n=43) at day 14, declining to 424 (221–799; n=43) by day 56 after vaccination (figure 6 ).
Figure 5.
PseudoNA results in trial participants and in convalescent plasma samples from 146 patients with PCR-confirmed COVID-19 and 24 asymptomatic health-care workers
Solid lines connect samples from the same participant. Boxes show median (IQR). Results for days 35 and 42 are samples from participants who received a booster dose at day 28. IC=inhibitory concentration. MenACWY=meningococcal group A, C, W-135, and Y conjugate vaccine.
Figure 6.
Interferon-γ ELISpot response to peptides spanning the SARS-CoV-2 spike vaccine insert
Error bars show median (IQR). The lower limit of detection, indicated with the dotted line, is 48 spot-forming cells per million PBMCs. PBMC=peripheral blood mononuclear cell. SARS-CoV-2=severe acute respiratory syndrome coronavirus 2. ELISpot=enzyme linked immunospot. MenACWY=meningococcal group A, C, W-135, and Y conjugate vaccine.
A small number (four [4%] of 98) participants had neutralising antibody titres greater than 8 against SARS-CoV-2 spike protein before vaccination (Marburg VN) and 11 (4%) of 270 participants had high ELISA titres at baseline, representing possible prior asymptomatic infection.
Before vaccination, only one (1%) of 98 participants who were tested had high titre (>200) neutralising antibodies against ChAdOx1. Antibodies were detectable at a lower level in a further 18 (18%) participants, and in 79 (81%) participants there were no detectable anti-ChAdOx1 antibodies. We found no relationship between presence of low-level antibodies to ChAdOx1 on the day of vaccination and the ELISA titre to SARS-CoV-2 spike protein in those randomly assigned to receive ChAdOx1 nCoV-19 (appendix 1 p 22).
Discussion
Our preliminary findings show that the candidate ChAdOx1 nCoV-19 vaccine given as a single dose was safe and tolerated, despite a higher reactogenicity profile than the control vaccine, MenACWY. No serious adverse reactions to ChAdOx1 nCoV-19 occurred. The majority of adverse events reported were mild or moderate in severity, and all were self-limiting. The profile of adverse events reported here is similar to that for other ChAdOx1-vectored vaccines and other closely related simian adenoviruses, such as ChAdOx2, ChAd3, and ChAd63, expressing multiple different antigens8, 12, 13, 14 at this dose level, as well as to some licensed vaccines.15 A dose of 5 × 1010 viral particles was chosen on the basis of our previous experience with ChAdOx1 MERS, where despite increased reactogenicity, a dose–response relationship with neutralising antibodies was observed.8 The protocol was written when the pandemic was accelerating in the UK and a single higher dose was chosen to provide the highest chance of rapid induction of neutralising antibody. In the context of a pandemic wave where a single higher, but more reactogenic, dose might be more likely to rapidly induce protective immunity, the use of prophylactic paracetamol appears to increase tolerability and would reduce confusion with COVID-19 symptoms that might be caused by short-lived vaccine-related symptoms without compromising immunogenicity.
We show that a single dose of ChAdOx1 nCoV-19 elicits an increase in spike-specific antibodies by day 28 and neutralising antibody in all participants after a booster dose. High levels of neutralising antibody at baseline seen in a small number of participants probably indicates prior asymptomatic infection, as potential participants with recent COVID-19-like symptoms or with a history of positive PCR test for SARS-CoV-2 were excluded from the study. Individuals with high titres on the day of vaccination who received ChAdOx1 nCoV-19 were boosted by vaccination.
Neutralising antibodies targeting different epitopes of the spike glycoprotein have been associated with protection from COVID-19 in early preclinical rhesus macaque studies.16 Although a correlate of protection has not been defined for COVID-19, high levels of neutralising antibodies have been shown in convalescent individuals, with a wide range, as confirmed in our study.17, 18
Antibodies capable of neutralising live SARS-CoV-2 were induced by day 28 with titres of 51 (PHE MNA80) and 218 (PHE PRNT50), and with titres of 29 (Marburg VN) or 136 (PHE MNA80) after a booster dose, as measured using different assays. In a non-human primate study where primary SARS-CoV-2 infection elicited at least short-term protection against reinfection, neutralising antibody titres of the magnitude found in our study after boosting appeared sufficient to confer protection using the Marburg VN assay methodology.19 Neutralising antibody titres were increased by a two-dose regimen, and further investigation of this approach is underway. The correlation of neutralisation assays with IgG quantitation indicates that, if confirmed, a standardised ELISA might be sufficient to predict protection, should neutralising antibody also be shown to be protective in humans. We have presented data from three different live neutralising antibody assays and a pseudo-neutralisation assay, which show tight correlation with each other but give very different neutralising antibody titres. This issue highlights the urgent need for centralised laboratory infrastructure to allow bridging between vaccine candidates and accelerate the availability of multiple products to provide the global capacity to end the pandemic. If any one candidate demonstrates efficacy, bridging this result to other candidate vaccines through rigorously conducted laboratory assays will become a crucial issue for global health.
Importantly, there are accumulating data to suggest T-cell responses play an important role in COVID-19 mitigation; individuals who were exposed but asymptomatic developed a robust memory T-cell response without symptomatic disease in the absence of a measurable humoral response.20, 21, 22 Adenovirus-vectored vaccines are known to induce strong cellular immunity and ChAdOx1 nCoV-19 vaccination resulted in marked increases in SARS-CoV-2 spike-specific effector T-cell responses as early as day 7, peaking at day 14 and maintained up to day 56 as expected with adenoviral vectors. However, a boost in cellular responses was not observed following the second ChAdOx1 nCoV-19 dose. This is consistent with previous findings on viral vectored vaccines given as part of a homologous prime-boost regimen.12
Severe and fatal cases of COVID-19 disproportionally affect older individuals. Therefore, it is important that vaccines developed to reduce or prevent COVID-19 are suitable for administration in older age groups. Immunogenicity of a ChAdOx1-vectored vaccine against influenza has been shown in older adults (50–78 years of age).6 As previously reported,10 anti-vector immunity was low before vaccination in UK adults aged 18–55 years, with no relationship between the presence of antibodies to ChAdOx1 and immune response to the vaccine antigen. Future studies will address the potential effect of anti-vector antibodies on homologous boosting, although in the subgroup reported on here, who received two vaccinations 28 days apart, there was clear evidence of boosting of antibody response to SARS-CoV-2 spike protein.
Limitations of this study include the short follow-up reported to date, the small number of participants in the prime-boost group, and single-blinded design, although staff undertaking clinical evaluation and laboratory staff all remained blinded. Additionally, the study findings are not easily generalisable, as this is a first-in-human study of fairly young and healthy volunteers, the majority of whom were white. Further studies are required to assess the vaccine in various population groups including older age groups, those with comorbidities, and in ethnically and geographically diverse populations. The participants recruited in this study will be followed up for at least 1 year and further safety, tolerability, and immunogenicity (in addition to efficacy) results will be reported when data are available.23, 24, 25
In conclusion, ChAdOx1 nCoV-19 was safe, tolerated, and immunogenic, while reactogenicity was reduced with paracetamol. A single dose elicited both humoral and cellular responses against SARS-CoV-2, with a booster immunisation augmenting neutralising antibody titres. The preliminary results of this first-in-human clinical trial supported clinical development progression into ongoing phase 2 and 3 trials. Older age groups with comorbidities, health-care workers, and those with higher risk for SARS-CoV-2 exposure are being recruited and assessed for efficacy, safety, and immunogenicity of ChAdOx1 nCoV-19 given as a single-dose or two-dose administration regimen in further trials conducted in the UK and overseas. We will also evaluate the vaccine in children, once sufficient safety data have been accumulated in adult studies. Phase 3 trials are now underway in Brazil, South Africa, and the UK and will evaluate vaccine efficacy in diverse populations.
This online publication has been corrected. The corrected version first appeared at thelancet.com on August 13, 2020, and further correction has been made on November 19, 2020
Data sharing
The study protocol is provided in the appendix 1 (pp 49–130). Individual participant data will be made available when the trial is complete, upon requests directed to the corresponding author; after approval of a proposal, data can be shared through a secure online platform.
Acknowledgments
Acknowledgments
This work is funded by UK Research and Innovation (MC_PC_19055), Engineering and Physical Sciences Research Council (EP/R013756/1), Coalition for Epidemic Preparedness Innovations (CEPI), the National Institute for Health Research (NIHR), the NIHR Oxford Biomedical Research Centre, and the German Center for Infection Research (DZIF), Partner site Gießen-Marburg-Langen. Additional resources for study delivery were provided by NIHR Southampton Clinical Research Facility and NIHR Southampton Biomedical Research Centre, University Hospital Southampton NHS Foundation Trust; the NIHR Imperial Clinical Research Facility; and NIHR North West London, South London, Wessex, and West of England Local Clinical Research Networks and NIHR Oxford Health Biomedical Research Centre. PMF received funding from the Coordenacao de Aperfeicoamento de Pessoal de Nivel Superior, Brazil (finance code 001). Development of SARS-CoV-2 reagents was partially supported by the US National Institute of Allergy and Infectious Diseases Centers of Excellence for Influenza Research and Surveillance contract HHSN272201400008C. The research reagent for SARS-CoV-2 RNA (NIBSC 20/130) was obtained from the National Institute for Biological Standards and Control, UK. The control vaccine was provided free of charge by the UK Department of Health and Social Care. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK Department of Health and Social Care. The University of Oxford has entered into a partnership with AstraZeneca on vaccine development; the authors are grateful to the senior management at AstraZeneca for facilitating and funding the pseudovirus neutralisation assays and Meso Scale antibody assay included in this Article. AstraZeneca reviewed the data from the study and the final manuscript before submission, but the authors retained editorial control. The investigators express their gratitude for the contribution of all the trial participants, the invaluable advice of the international Data Safety Monitoring Board (appendix 1 p 46) and the independent members of the Trial Steering Committee. We additionally acknowledge the broader support from the various teams within the University of Oxford including Medical Sciences Division, Nuffield Department of Medicine and Department of Paediatrics, the Oxford Immunology Network COVID Consortium, Clinical Trials Research Governance, Research Contracts, Public Affairs Directorate and the Clinical Biomanufacturing Facility, as well as the Oxford University Hospitals NHS Foundation Trust and Oxford Health NHS Foundation Trust and the trial sites (appendix 1 pp 46–48). We are grateful for the input of the protein production team at the Jenner Institute and the team at the Pirbright Institute.
Contributors
SCG and AJP conceived and designed the trial and AJP is the chief investigator. AJP, PMF, DJ, HR, and MV contributed to the protocol and design of the study. AF, PH, RL, KMP, SNF, BA, and AVSH were the study site principal investigators. DB, MB, CD, SBi, SBe, EAC, TL, KJE, ALF, BH, RM, and SB-R were responsible for laboratory testing and assay development. PKA, DJ, HR, PMF, AMM, MR, and MS contributed to the implementation of the study. MV conducted the statistical analysis. CG, ADD, and RT were responsible for vaccine manufacturing. TL and SCG were responsible for vaccine development. AVSH and SCG developed the ChAdOx1 vector. TL, KJE, MV, SCG, AVSH, PMF, and AJP contributed to the preparation of the report. All other authors contributed to the implementation of the study and data collection. All authors critically reviewed and approved the final version.
Declaration of interests
SCG is co-founder and board member of Vaccitech (collaborators in the early development of this vaccine candidate) and named as an inventor on a patent covering use of ChAdOx1-vectored vaccines and a patent application covering this SARS-CoV-2 vaccine. TL is named as an inventor on a patent application covering this SARS-CoV-2 vaccine and consultant to Vaccitech. PMF is a consultant to Vaccitech. AJP is Chair of the UK Department of Health and Social Care's Joint Committee on Vaccination & Immunisation (JCVI), but does not participate in policy advice on coronavirus vaccines, and is a member of the WHO Strategic Advisory Group of Experts (SAGE). AVSH is a co-founder of and consultant to Vaccitech and is named as an inventor on a patent covering design and use of ChAdOx1-vectored vaccines. AF is a member of JCVI, Chair of the WHO European Technical Advisory Group of Experts on Immunisation, an ex-officio member of WHO SAGE working group on COVID-19 vaccines, and acting director of National Institute for Health Research West of England Local Clinical Research Network. KMP reports grants from the NIHR Imperial Biomedical Research Centre and Gilead Sciences, and personal fees from Sanofi Pasteur, outside of the submitted work. MS reports grants from Janssen, GlaxoSmithKline, Medimmune, Novavax, and MCM and grants and non-financial support from Pfizer, outside of the submitted work. CG reports personal fees from the Duke Human Vaccine Institute, outside of the submitted work. ADD reports grants and personal fees from AstraZeneca, outside of the submitted work. In addition, ADD has a patent manufacturing process for ChAdOx vectors with royalties paid to AstraZeneca, and a patent ChAdOx2 vector with royalties paid to AstraZeneca. The other authors declare no competing interests.
Contributor Information
Oxford COVID Vaccine Trial Group:
Jeremy Aboagye, Kelly Adams, Aabidah Ali, Elizabeth Allen, Jennifer L. Allison, Rachel Anslow, Edward H. Arbe-Barnes, Gavin Babbage, Kenneth Baillie, Megan Baker, Natalie Baker, Philip Baker, Ioana Baleanu, Juliana Ballaminut, Eleanor Barnes, Jordan Barrett, Louise Bates, Alexander Batten, Kirsten Beadon, Rebecca Beckley, Eleanor Berrie, Lisa Berry, Amy Beveridge, Kevin R. Bewley, Else Margreet Bijker, Tracey Bingham, Luke Blackwell, Caitlin L. Blundell, Emma Bolam, Elena Boland, Nicola Borthwick, Thomas Bower, Amy Boyd, Tanja Brenner, Philip D. Bright, Charlie Brown-O'Sullivan, Emily Brunt, Jamie Burbage, Sharon Burge, Karen R. Buttigieg, Nicholas Byard, Ingrid Cabera Puig, Anna Calvert, Susana Camara, Michelangelo Cao, Federica Cappuccini, Melanie Carr, Miles W. Carroll, Victoria Carter, Katrina Cathie, Ruth J. Challis, Sue Charlton, Irina Chelysheva, Jee-Sun Cho, Paola Cicconi, Liliana Cifuentes, Helen Clark, Elizabeth Clark, Tom Cole, Rachel Colin-Jones, Christopher P. Conlon, Aislinn Cook, Naomi S. Coombes, Rachel Cooper, Catherine A. Cosgrove, Karen Coy, Wendy E.M. Crocker, Christina J. Cunningham, Brad E. Damratoski, Lynne Dando, Mehreen S. Datoo, Hannah Davies, Hans De Graaf, Tesfaye Demissie, Claudio Di Maso, Isabelle Dietrich, Tao Dong, Francesca R. Donnellan, Naomi Douglas, Charlotte Downing, Jonathan Drake, Rachael Drake-Brockman, Ruth Elizabeth Drury, Susanna Jane Dunachie, Nick J. Edwards, Frances D.L. Edwards, Chris J. Edwards, Sean C. Elias, Michael J. Elmore, Katherine R.W. Emary, Marcus Rex English, Susanne Fagerbrink, Sally Felle, Shuo Feng, Samantha Field, Carine Fixmer, Clare Fletcher, Karen J. Ford, Jamie Fowler, Polly Fox, Emma Francis, John Frater, Julie Furze, Michelle Fuskova, Eva Galiza, Diane Gbesemete, Ciaran Gilbride, Kerry Godwin, Giacomo Gorini, Lyndsey Goulston, Caroline Grabau, Lara Gracie, Zoe Gray, Lucy Belle Guthrie, Mark Hackett, Sandro Halwe, Elizabeth Hamilton, Joseph Hamlyn, Brama Hanumunthadu, Irasha Harding, Stephanie A. Harris, Andrew Harris, Daisy Harrison, Clare Harrison, Thomas C. Hart, Louise Haskell, Sophia Hawkins, Ian Head, John Aaron Henry, Jennifer Hill, Susanne H.C. Hodgson, Mimi M. Hou, Elizabeth Howe, Nicola Howell, Cecilia Hutlin, Sabina Ikram, Catherine Isitt, Poppy Iveson, Susan Jackson, Frederic Jackson, Sir William James, Megan Jenkins, Elizabeth Jones, Kathryn Jones, Christine E. Jones, Bryony Jones, Reshma Kailath, Konstantinos Karampatsas, Jade Keen, Sarah Kelly, Dearbhla Kelly, David Kerr, Simon Kerridge, Liaquat Khan, Uzma Khan, Annabel Killen, Jasmin Kinch, Thomas B. King, Lloyd King, Jade King, Lucy Kingham-Page, Paul Klenerman, Francesca Knapper, Julian C. Knight, Daniel Knott, Stanislava Koleva, Alexandra Kupke, Colin W. Larkworthy, Jessica P.J. Larwood, Anna Laskey, Alison M. Lawrie, Arlene Lee, Kim Yee Ngan Lee, Emily A Lees, Helen Legge, Alice Lelliott, Nana-Marie Lemm, Amelia M. Lias, Aline Linder, Samuel Lipworth, Xinxue Liu, Shuchang Liu, Raquel Lopez Ramon, May Lwin, Francesca Mabesa, Meera Madhavan, Garry Mallett, Kushal Mansatta, Ines Marcal, Spyridoula Marinou, Emma Marlow, Julia L. Marshall, Jane Martin, Joanne McEwan, Lorna McInroy, Gretchen Meddaugh, Alexander J. Mentzer, Neginsadat Mirtorabi, Maria Moore, Edward Moran, Ella Morey, Victoria Morgan, Susan Jane Morris, Hazel Morrison, Gertraud Morshead, Richard Morter, Yama F. Mujadidi, Jilly Muller, Tatiana Munera-Huertas, Claire Munro, Alasdair Munro, Sarah Murphy, Vincent J. Munster, Philomena Mweu, Andrés Noé, Fay L. Nugent, Elizabeth Nuthall, Katie O'Brien, Daniel O'Connor, Blanché Oguti, Jennifer L. Oliver, Catarina Oliveira, Peter John O'Reilly, Mairead Osborn, Piper Osborne, Cathy Owen, Daniel Owens, Nelly Owino, Mihaela Pacurar, Kaye Parker, Helena Parracho, Maia Patrick-Smith, Victoria Payne, Jennifer Pearce, Yanchun Peng, Marco Polo Peralta Alvarez, James Perring, Katja Pfafferott, Dimitra Pipini, Emma Plested, Helen Pluess-Hall, Katrina Pollock, Ian Poulton, Laura Presland, Samuel Provstgaard-Morys, David Pulido, Kajal Radia, Fernando Ramos Lopez, Jade Rand, Helen Ratcliffe, Thomas Rawlinson, Sarah Rhead, Amy Riddell, Adam John Ritchie, Hannah Roberts, Joanna Robson, Sophie Roche, Cornelius Rohde, Christine S. Rollier, Rossana Romani, Indra Rudiansyah, Stephen Saich, Sara Sajjad, Stephannie Salvador, Lidia Sanchez Riera, Helen Sanders, Katherine Sanders, Shari Sapaun, Chloe Sayce, Ella Schofield, Gavin Screaton, Beatrice Selby, Calum Semple, Hannah R. Sharpe, Imam Shaik, Adam Shea, Holly Shelton, Sarah Silk, Laura Silva-Reyes, Donal T. Skelly, Heather Smee, Catherine C. Smith, David J. Smith, Rinn Song, Alexandra J. Spencer, Elizabeth Stafford, Amy Steele, Elena Stefanova, Lisa Stockdale, Anna Szigeti, Abdessamad Tahiri-Alaoui, Moira Tait, Helen Talbot, Rachel Tanner, Iona Jennifer Taylor, Victoria Taylor, Rebecca Te Water Naude, Nazia Thakur, Yrene Themistocleous, Andreas Themistocleous, Merin Thomas, Tonia M. Thomas, Amber Thompson, Samantha Thomson-Hill, Jennifer Tomlins, Susan Tonks, James Towner, Nguyen Tran, Julia A. Tree, Adam Truby, Kate Turkentine, Cheryl Turner, Nicola Turner, Sally Turner, Toby Tuthill, Marta Ulaszewska, Rachel Varughese, Neeltje Van Doremalen, Kristin Veighey, Marije K. Verheul, Iason Vichos, Elia Vitale, Laura Walker, Marion E.E. Watson, Benjamin Welham, Julie Wheat, Caroline White, Rachel White, Andrew T. Worth, Danny Wright, Suzie Wright, Xin Li Yao, and Yasmine Yau
Supplementary Materials
References
- 1.WHO . World Health Organization; Geneva: 2020. Coronavirus disease (COVID-19) situation report—181. [Google Scholar]
- 2.WHO Draft Landscape of COVID-19 candidate vaccines. July 14, 2020. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
- 3.Fidler S, Stöhr W, Pace M. Antiretroviral therapy alone versus antiretroviral therapy with a kick and kill approach, on measures of the HIV reservoir in participants with recent HIV infection (the RIVER trial): a phase 2, randomised trial. Lancet. 2020;395:888–898. doi: 10.1016/S0140-6736(19)32990-3. [DOI] [PubMed] [Google Scholar]
- 4.Hanke T. Aiming for protective T-cell responses: a focus on the first generation conserved-region HIVconsv vaccines in preventive and therapeutic clinical trials. Expert Rev Vaccines. 2019;18:1029–1041. doi: 10.1080/14760584.2019.1675518. [DOI] [PubMed] [Google Scholar]
- 5.Mothe B, Manzardo C, Sanchez-Bernabeu A. Therapeutic vaccination refocuses T-cell responses towards conserved regions of HIV-1 in early treated individuals (BCN 01 study) EClinicalMedicine. 2019;11:65–80. doi: 10.1016/j.eclinm.2019.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coughlan L, Sridhar S, Payne R. Heterologous two-dose vaccination with simian adenovirus and poxvirus vectors elicits long-lasting cellular immunity to influenza virus A in healthy adults. EBioMedicine. 2018;29:146–154. doi: 10.1016/j.ebiom.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Doremalen N, Haddock E, Feldmann F. A single dose of ChAdOx1 MERS provides protective immunity in rhesus macaques. Sci Adv. 2020;6 doi: 10.1126/sciadv.aba8399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Folegatti PM, Bittaye M, Flaxman A. Safety and immunogenicity of a candidate Middle East respiratory syndrome coronavirus viral-vectored vaccine: a dose-escalation, open-label, non-randomised, uncontrolled, phase 1 trial. Lancet Infect Dis. 2020;20:816–826. doi: 10.1016/S1473-3099(20)30160-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Doremalen N. ChAdOx1 nCoV-19 vaccination prevents SARS-CoV-2 pneumonia in rhesus macaques. BioRxiv. 2020 doi: 10.1101/2020.05.13.093195. published online May 13. (preprint) [DOI] [PubMed] [Google Scholar]
- 10.Dicks MD, Spencer AJ, Edwards NJ. A novel chimpanzee adenovirus vector with low human seroprevalence: improved systems for vector derivation and comparative immunogenicity. PLoS One. 2012;7 doi: 10.1371/journal.pone.0040385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morris SJ, Turner AV, Green N, Warimwe GM. Laboratory-scale production of replication-deficient adenovirus vectored vaccines. Methods Mol Biol. 2016;1349:121–135. doi: 10.1007/978-1-4939-3008-1_8. [DOI] [PubMed] [Google Scholar]
- 12.Bliss CM, Bowyer G, Anagnostou NA. Assessment of novel vaccination regimens using viral vectored liver stage malaria vaccines encoding ME-TRAP. Sci Rep. 2018;8 doi: 10.1038/s41598-018-21630-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Folegatti PM, Bellamy D, Roberts R. Safety and immunogenicity of a novel recombinant simian adenovirus ChAdOx2 as a vectored vaccine. Vaccines (Basel) 2019;7:40. doi: 10.3390/vaccines7020040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ewer K, Rampling T, Venkatraman N. A monovalent chimpanzee adenovirus ebola vaccine boosted with MVA. N Engl J Med. 2016;374:1635–1646. doi: 10.1056/NEJMoa1411627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hesse EM, Shimabukuro TT, Su JR. Postlicensure safety surveillance of recombinant zoster vaccine (Shingrix)—United States, October 2017–June 2018. MMWR Morb Mortal Wkly Rep. 2019;68:91–94. doi: 10.15585/mmwr.mm6804a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yu J, Tostanoski LH, Peter L. DNA vaccine protection against SARS-CoV-2 in rhesus macaques. Science. 2020 doi: 10.1126/science.abc6284. published online May 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robbiani DF, Gaebler C, Muecksch F. Convergent antibody responses to SARS-CoV-2 in convalescent individuals. Nature. 2020 doi: 10.1038/s41586-020-2456-9. published online June 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang X, Guo X, Xin Q. Neutralizing antibodies responses to SARS-CoV-2 in COVID-19 inpatients and convalescent patients. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa721ciaa721. published online June 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deng W, Bao L, Liu J. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Science. 2020 doi: 10.1126/science.abc5343. published online July 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grifoni A, Weiskopf D, Ramirez SI. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181:1489. doi: 10.1016/j.cell.2020.05.015. 501.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sekine T, Perez-Potti A, Rivera-Ballesteros O. Robust T cell immunity in convalescent individuals with asymptomatic or mild COVID-19. bioRxiv. 2020 doi: 10.1101/2020.06.29.174888. published online June 29. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weiskopf D, Schmitz KS, Raadsen MP. Phenotype and kinetics of SARS-CoV-2-specific T cells in COVID-19 patients with acute respiratory distress syndrome. Sci Immunol. 2020;5 doi: 10.1126/sciimmunol.abd2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bolles M, Deming D, Long K. A double-inactivated severe acute respiratory syndrome coronavirus vaccine provides incomplete protection in mice and induces increased eosinophilic proinflammatory pulmonary response upon challenge. J Virol. 2011;85:12201–12215. doi: 10.1128/JVI.06048-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu L, Wei Q, Lin Q. Anti-spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI Insight. 2019;4 doi: 10.1172/jci.insight.123158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weingartl H, Czub M, Czub S. Immunization with modified vaccinia virus Ankara-based recombinant vaccine against severe acute respiratory syndrome is associated with enhanced hepatitis in ferrets. J Virol. 2004;78:12672–12676. doi: 10.1128/JVI.78.22.12672-12676.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The study protocol is provided in the appendix 1 (pp 49–130). Individual participant data will be made available when the trial is complete, upon requests directed to the corresponding author; after approval of a proposal, data can be shared through a secure online platform.