To the Editor:
We fully agree with Dr Guerini et al regarding how challenging the differentiation between lung toxicity and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in patients with lung cancer (LC) can be.1 However, we would like to comment on the management complexity of patients with LC (both for new tumor diagnoses and for known patients with cancer) during the COVID-19 pandemic beyond lung toxicity. There are few publications that address the clinical management of patients with LC in the current SARS-CoV-2 pandemic.2, 3, 4, 5 The clinical and radiologic manifestations of COVID-19 can mimic pulmonary toxicity or progression of tumor disease in patients with LC.6 Some extrapulmonary complications of SARS-CoV-2 pneumonia may also simulate progression of cancer disease.7 On the other hand, some treatment-related complications of patients with LC can radiologically mimic SARS-CoV-2 pneumonia.8 , 9 Finally, the management of some diagnostic interventional procedures can be difficult in COVID-19 patients with LC.10 In this letter, we describe our experience in the management of several patients with LC during the COVID-19 pandemic that affected our region, and which required close multidisciplinary collaboration between different specialists.
Case 1. Incidental Detection of Lung Tumor in a Patient With Confirmed COVID-19
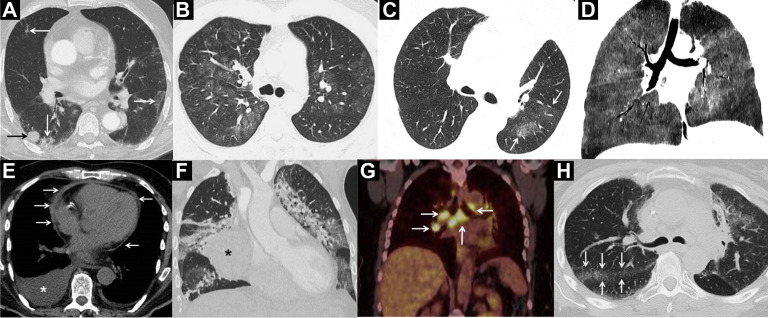
Chest radiograph in an 84-year-old man with fever, cough, and dyspnea revealed bilateral opacities. The SARS-CoV-2 reverse transcriptase polymerase chain reaction (RT-PCR) test was positive. A chest computed tomography (CT) was performed a few days later which incidentally detected a peripheral pulmonary nodule (Figure 1A ). Positron emission tomography/CT confirmed its likely malignant nature and the absence of distant metastases. A treatment with curative intention was decided with stereotaxic radiotherapy.
Figure 1.
A, Computed Tomography (CT) Image Shows a Solid Lung Tumor Nodule (black arrow) and Several Peripheral Sub-segmental Ground-Glass Attenuation Opacities of Infectious Nature (white arrows). B, CT Image Shows Ground-Glass Attenuation Opacities Consistent With COVID-19 Infection. C, CT Image Shows Ground-Glass Attenuation Opacities in the Left Lung (arrows) Highly Suggestive of COVID- 19. In This Case, the Radiologic Findings Contributed to the Correct Management of the Patient. D, CT Image Shows Extensive Ground-Glass Opacities. The Absence of Infectious Symptoms Suggested a Pulmonary Toxicity. E, CT Image (Staging Study) Shows a New Pericardial Thickening (arrows) and a Bilateral Pleural Effusion (asterisk), and an Empirical Diagnosis of Post-COVID Acute Pericarditis was Made. F, CT Image Shows an Incidentally Detected Mass in the Right Hemithorax (asterisk); Note the Presence of Bilateral Pulmonary Consolidations. A Percutaneous CT-Guided Biopsy was Performed. G, Positron Emission Tomography/CT Image Shows the Appearance of Hypermetabolic Lymph Nodes in the Mediastinum and Both Pulmonary Hila (arrows), Suggesting the Diagnosis of Sarcoid Reaction. H, CT Image (Same Patient as G) Shows the Appearance of Multiple Small Perilymphatic Nodules Adjacent to the Greater Fissure (arrows), a Typical Finding of Pulmonary Sarcoidosis
Case 2. Confirmed COVID-19 in a Patient With LC on Follow-up
This is a 36-year-old man with known LC (with ALK translocation) on crizotinib who consulted for fever, cough, and dyspnea. The SARS-CoV-2 RT-PCR test was positive, and a chest radiograph showed bilateral pulmonary opacities. A chest CT scan confirmed the presence of bilateral ground-glass attenuation opacities (Figure 1B). The patient improved after the administration of specific treatment against SARS-CoV-2 2 (hydroxychloroquine and lopinavir/ritonavir).
Case 3. Suspicion of COVID-19 in a Patient With LC on Follow-up
A 64-year-old woman with known LC (with KRAS mutation) who was being treated with chemotherapy presented with high fever, dry cough, myalgia, and ageusia. A chest CT revealed infectious-looking left lung opacities (Figure 1C). Despite 2 consecutive RT-PCR tests negative for SARS-CoV-2, an empirical diagnosis of COVID-19 was issued, and the patient improved with the specific treatment for this infection (hydroxychloroquine, azithromycin, and corticosteroids). Determination of SARS-CoV-2 IgG and IgM antibodies was positive.
Case 4. Lung Toxicity (Secondary to Everolimus) in a Patient With LC Mimicking COVID-19
A 54-year-old man with a metastatic pulmonary neuroendocrine tumor treated with everolimus presented with dyspnea (no fever or cough). The SARS-CoV-2 RT-PCR test was negative on 2 occasions, as well as the determination of antibodies. Chest CT detected a striking mosaic pattern (Figure 1D). Everolimus was suspended and corticosteroids were added, improving the patient’s symptoms and lung opacities.
Case 5. Acute Pericarditis (Post-COVID-19) in a Patient With LC Mimicking Tumor Progression
This is a 74-year-old man with a recent simultaneous diagnosis of LC and COVID-19. On a CT staging study, a thickening of the pericardium and the appearance of bilateral pleural effusions were observed (not present 3 weeks before when the diagnosis of COVID-19 and lung mass was made) (Figure 1E). The patient stated that, after improving from the COVID-19 symptoms, he presented an episode of low-grade fever and chest pain that changed with posture variation. An empirical retrospective diagnosis of acute post-COVID-19 pleuropericarditis was made, and the symptoms improved after the administration of colchicine. A follow-up chest CT demonstrated resolution of the pericardial thickening and the pleural effusions.
Case 6. CT-guided Percutaneous Biopsy in a Patient With COVID-19 With a Lung Mass
This is a 50-year-old male with a simultaneous diagnosis of a lung mass and COVID-19 (Figure 1F). In spite of the active SARS-CoV-2 infection, it was decided to perform a CT-guided core needle biopsy of the lung mass (the staff involved followed the infection control protocol of our hospital and used personal protective equipment during the biopsy procedure).
Case 7. Sarcoid Reaction in a Patient With LC Being Treated With Immunotherapy and Mimicking COVID-19
On a follow-up study, an asymptomatic 47-year-old woman with locally advanced LC that was being treated with immunotherapy (durvalumab) showed the appearance of pulmonary ground-glass attenuation opacities and hypermetabolic bilateral mediastinal and hilar lymphadenopathies (Figure 1G, H). Physical examination revealed erythematous plaques in her lower limbs, suggestive of erythema nodosum. Although imaging suggested a sarcoid reaction, the possibility of COVID-19 was also considered. Finally, the empirical clinical diagnosis of sarcoid reaction secondary to immunotherapy was made.
These 7 cases reflect the complexity of clinical management and radiologic interpretation of patients with LC during the COVID-19 pandemic, both in patients with new LC diagnoses and in patients being followed-up. The clinical and radiologic manifestations (both pulmonary and extrapulmonary) of COVID-19 may simulate oncologic disease progression or adverse drug reactions; on the contrary, some complications of LC treatment (pulmonary toxicities, sarcoid reactions, etc) can mimic infectious pulmonary opacities on imaging tests and suggest SARS-CoV-2 pneumonia. Although the results of the SARS-CoV-2 diagnostic tests (RT-PCR and/or antibody detection) are useful for the management of these patients, their diagnostic accuracy is suboptimal, making close multidisciplinary collaboration and integration of other diagnostic tests (particularly of imaging studies) crucial.
Disclosure
The authors have stated that they have no conflicts of interest.
References
- 1.Guerini A.E., Borghetti P., Filippi A.R. Differential diagnosis and clinical management of a case of COVID-19 in a patient with stage III lung cancer treated with radio-chemotherapy and durvalumab [e-pub ahead of print] Clin Lung Cancer. 2020 doi: 10.1016/j.cllc.2020.05.027. accessed september 9, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banna G., Curioni-Fontecedro A., Friedlaender A., Addeo A. How we treat patients with lung cancer during the SARS-CoV-2 pandemic: primum non nocere. ESMO Open. 2020;5:e000765. doi: 10.1136/esmoopen-2020-000765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar S., Chmura S., Robinson C. Alternative multidisciplinary management options for locally advanced non-small cell lung cancer during the COVID-19 global pandemic. J Thorac Oncol. 2020;15:1137–1146. doi: 10.1016/j.jtho.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mazzone P.J., Gould M.K., Arenberg D.A. management of lung nodules and lung cancer screening during the COVID-19 pandemic: CHEST Expert Panel report. Chest. 2020;158:406–415. doi: 10.1016/j.chest.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao Z., Bai H., Duan J., Wang J. Recommendations of individualized medical treatment and common adverse events management for lung cancer patients during the outbreak of COVID-19 epidemic. Thorac Cancer. 2020;11:1752–1757. doi: 10.1111/1759-7714.13424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Calabrò L., Peters S., Soria J.C. Challenges in lung cancer therapy during the COVID-19 pandemic. Lancet Respir Med. 2020;8:542–544. doi: 10.1016/S2213-2600(20)30170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu J., Zhang Y., Gao X.H., Xi E.P. COVID-19 or lung cancer: a differential diagnostic experience and management model from Wuhan. J Thorac Oncol. 2020;15:e141–e142. doi: 10.1016/j.jtho.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis A.P., Boyer M., Lee J.H., Kao S.C. COVID-19: the use of immunotherapy in metastatic lung cancer. Immunotherapy. 2020;12:545–548. doi: 10.2217/imt-2020-0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaverdian N., Shepherd A., Rimner A. Need for caution in the diagnosis of radiation pneumonitis in the COVID-19 pandemic. Adv Radiat Oncol. 2020;5:617–620. doi: 10.1016/j.adro.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spiess P.E., Greene J., Keenan R.J., Paculdo D., Letson G.D., Peabody J.W. Meeting the challenge of the 2019 novel coronavirus disease in patients with cancer. Cancer. 2020;126:3174–3175. doi: 10.1002/cncr.32919. [DOI] [PMC free article] [PubMed] [Google Scholar]