Abstract
Purpose
This study aimed to assess the effects of thermal pulsation system (TPS) treatment on astigmatism management in meibomian gland dysfunction (MGD) patients undergoing cataract surgery.
Patients and Methods
This single-center pilot study included 25 eyes of 23 patients who had visually significant cataract and concomitant MGD-associated dry eye in at least 1 eye and were willing to undergo TPS treatment and wait for at least 6 weeks for tear film stabilization prior to cataract surgery. Post-TPS keratometric readings were used for presurgical planning, and the actual postoperative residual refractive astigmatism (RRA) was recorded. Pre-TPS keratometry was used to mathematically simulate the RRA that would have been obtained from the lens choice and astigmatism management without TPS treatment.
Results
Following TPS treatment, the magnitude of astigmatism increased in 52% of eyes, decreased in 24%, and remained unchanged in 24%. Correspondingly, astigmatism treatment modality changed in 68% of eyes after tear film stabilization with TPS treatment. The type of astigmatism management increased (ie, shifted from no treatment to LRI or LRI to toric IOL) in 25% of eyes and decreased in 8%. Actual RRA ≤0.5 D was achieved in 76% of eyes, compared to simulated RRA ≤0.5 D in 40% of eyes (p=0.004).
Conclusion
Stabilization of the tear film with TPS treatment resulted in less RRA than if pre-TPS keratometric readings had been used to determine the astigmatism management method and toric IOL power and axis.
Keywords: dry eye cataract, meibomian gland dysfunction cataract, thermal pulsation treatment dry eye, astigmatism treatment cataract dry eye
Introduction
An estimated three-quarters of eyes undergoing cataract surgery have astigmatism >0.5 D1–3 and one-third have >1.0 D.1,2,4 The correction of pre-existing astigmatism is fundamental to the goal of achieving emmetropia and increased spectacle independence after cataract surgery.5 Partial-thickness arcuate incisions, corneal limbal relaxing incisions, and toric IOLs are the most commonly performed procedures to address pre-existing astigmatism at the time of cataract surgery; however, astigmatic outcomes are often suboptimal, particularly in patients with pre-existing dry eye.6
Meibomian gland dysfunction (MGD)-associated evaporative dry eye negatively affects ocular surface health through tear film instability, increased tear evaporation, hyperosmolarity, inflammation, and subsequent ocular surface damage.7,8 The unstable tear film affects the quality of optical surface reflections from the cornea on which the keratometric measurements are based, compromising keratometry readings with manual keratometry or advanced devices like placido disc/point-source color light-emitting diode topographers, slit-scan imaging, swept source OCT biometers or Scheimpflug image-based tomographers.9,10 Further, chronic ocular desiccation and deficiency of the tears have also been associated with corneal deformation, most commonly inferior corneal steepening and high astigmatism resembling keratoconus.11 This could potentially be due to dry eye-induced, prolonged inflammation or eye rubbing or other unknown mechanisms.12,13 It is therefore recommended that dry eye and MGD be diagnosed and treated prior to pre-surgical biometry and IOL power calculations. Keratometry and other measurements from a healthy cornea allow for more reliable selection of astigmatic correction approaches and identification of the accurate magnitude and axis of astigmatism.5
Thermal pulsation system (TPS) treatment for MGD has well-documented positive effects on ocular surface health and patient symptoms.14–16 However, its effect on keratometry measurements and presurgical planning for astigmatism management has not been studied. We hypothesize that TPS treatment prior to cataract surgery (in eyes with concomitant MGD) may potentially change the keratometry (magnitude and/or axis of orientation of astigmatism) and affect treatment planning. We also hypothesize that astigmatic outcomes that would be achieved after performing cataract surgery using the post-TPS keratometric measurements would be better than those based on pre-TPS keratometric measurements. Accordingly, this study aimed to compare the actual astigmatic outcomes (and astigmatic management choices, if needed) using the post-TPS keratometric measurements to the simulated astigmatic outcomes (calculated mathematically) that would have been achieved if pre-TPS keratometric measurements had been used as the basis for astigmatism management in MGD patients undergoing cataract surgery.
Methods
This pilot retrospective study included 25 dry eyes of 23 patients (12 female and 11 male), who underwent cataract surgery at least 6 weeks after TPS treatment at Matossian Eye Associates in Doylestown, PA and Hopewell, NJ, USA. The mean age of the included patients meeting the recruitment criteria was 73.4±7.5 years (range 59 to 86 years).
Patients were assessed by the surgeon to have visually significant cataract and concomitant MGD-associated dry eye in at least 1 eye. Patients were educated about their co-existing disease entities and given the option to pay for TPS and wait 6 weeks for their pre-operative measurements for cataract surgery. As part of routine clinical protocol, the risks, benefits, and alternatives to TPS treatment were explained to all patients prior to surgery and signed informed consent was obtained. Patients who agreed were administered the 12-minute LipiFlow treatment. The patients were directed to continue the use of any artificial lubricants they were already using, in the same manner as before. No new dry eye treatments other than LipiFlow were initiated. Since the data were previously collected, de-identified, and compliant with the Health Insurance Portability and Accountability Act, approval from an Institutional Review Board was not required.
Patients with complicated cataracts or ocular disorders other than MGD likely to affect the keratometry readings (eg, corneal scar, post-LASIK) were excluded, as were those with a need for additional corneal or filtering surgery, those likely to have an unpredictable response to surgery due to systemic conditions (eg, collagen vascular disease, undergoing chemo treatments), patients with posterior segment pathology that could affect refractive assessment, and patients allergic to any perioperative drug. Patients on topical immunomodulators, such as cyclosporine or lifitegrast, for dry eye disease were also excluded.
Study Parameters and Outcome Measures
Initial keratometry readings were obtained via the OPD-Scan III wavefront aberrometer (Nidek and Marco, Jacksonville, FL, USA). TPS treatment (LipiFlow; Johnson & Johnson Vision) was performed on the same day as the initial keratometry measurements. Keratometry was repeated approximately 6 weeks (±2 weeks) after TPS treatment, prior to planned cataract surgery.
The outcome measures were post-TPS versus pre-TPS keratometry assessed using single angle vector plots, change in magnitude of astigmatism and axis of orientation (WTR, ATR, oblique), and astigmatism management modality. Astigmatism management decisions were based on the following criteria: toric IOL for eyes with keratometric astigmatism ≥1.00 D, limbal relaxing incisions (LRIs) for eyes with keratometric astigmatism ranging from 0.5D to 0.99 D, and no intervention for eyes with keratometric astigmatism <0.5 D. The applicable management approach was determined for pre-TPS keratometry as well as post-TPS keratometry. Patients were treated based on the calculations using post-TPS keratometry measurements.
Residual refractive astigmatism (RRA) was measured at 4–5 weeks after cataract surgery (actual RRA). Hill et al’s method17 was adapted to vectorially calculate the simulated RRA that would have been obtained had treatment been based on pre-TPS keratometry.
Vector plots, mean±standard deviation (magnitude), and frequency distribution of change in the magnitude of RRA were used to compare the actual and simulated RRA. The change in astigmatism management approach from pre-TPS to post-TPS was also analyzed.
Statistical Methods
Statistical analysis was performed using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA). Normality of the scale data was tested using the Shapiro–Wilk test and quantile–quantile (Q–Q) plots. For normally distributed scale data, means were compared using the paired t-test; its non-parametric counterpart, the Wilcoxon signed-rank test, was used for not-normally-distributed scale data. McNemar’s test was used for paired nominal data; All p-values were two-sided and were considered statistically significant when less than 0.05.
Results
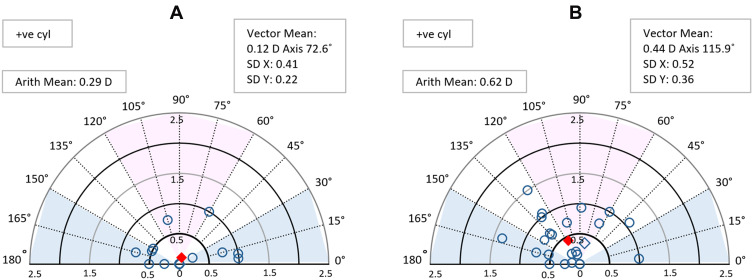
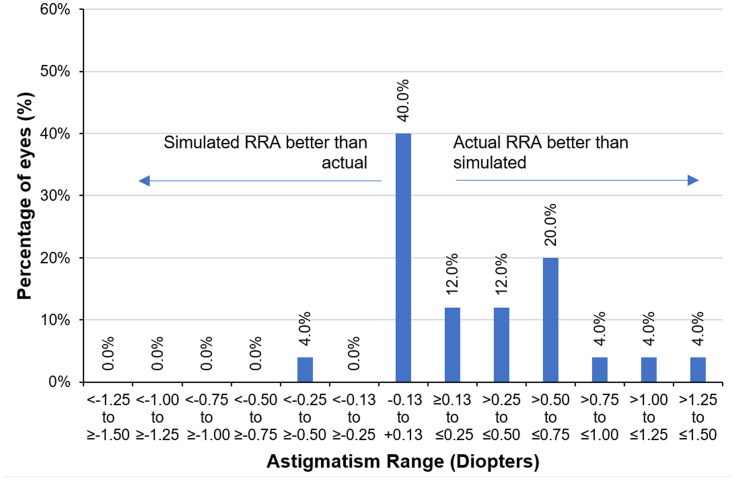
Figure 1 presents single angle vector plots of actual and simulated RRA. The simulated RRA values are more broadly dispersed, particularly beyond 0.5 D, than the actual RRA values (Figure 1A and B). The mean arithmetic positive cylinder of simulated RRA (0.62 D±0.43) was statistically significantly higher (p=0.001) than the actual RRA (0.30 D±0.37). In 56% of eyes, the actual RRA was better than the simulated RRA (Figure 2). In 40% of eyes, the values were comparable. Actual RRA ≤0.5 D was achieved in 76% of eyes, while simulated RRA ≤0.5 D was achieved in only 40% of eyes (p=0.004).
Figure 1.
Single angle vector plot for actual (A) versus simulated (B) residual refractive astigmatism.
Figure 2.
Frequency distribution histograms of difference between actual versus simulated residual refractive astigmatism.
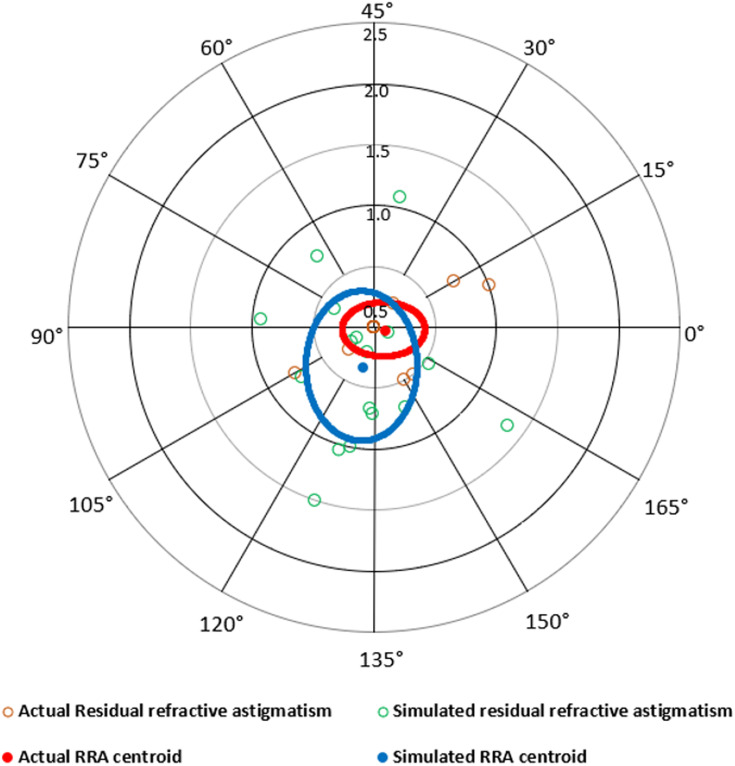
Among the 17 eyes (68%) with a change in astigmatism management, the centroid of actual RRA was closer to 0.0 D and had a smaller vectoral standard deviation (within 0.5 D; represented by eclipse) than the corresponding analyses for simulated RRA (Figure 3).
Figure 3.
Double angle vector plot for actual versus simulated residual refractive astigmatism in eyes with change in treatment type (17 eyes).
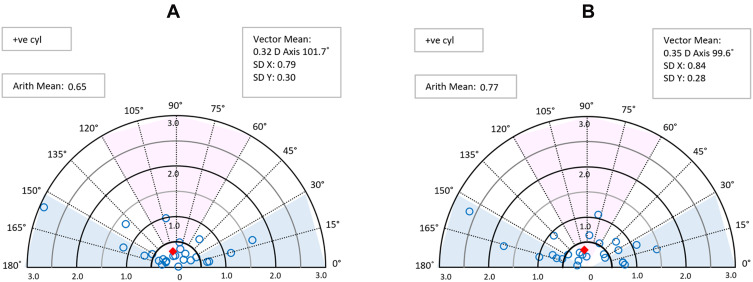
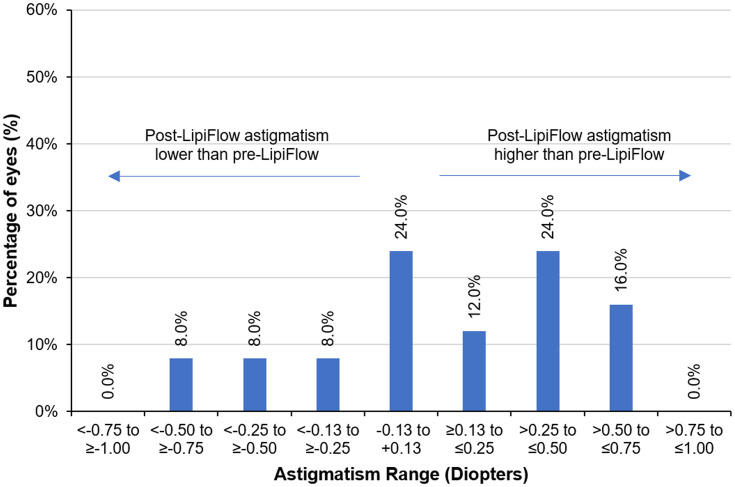
Figure 4 presents single angle vector plots of pre-TPS and post-TPS keratometric astigmatism. The post-TPS keratometric astigmatism values are more broadly dispersed than the pre-TPS keratometric values (Figure 4A and B). The mean arithmetic cylinder after TPS treatment (0.77±0.54) was higher than the pre-TPS treatment (0.65±0.62) (p=0.110). When analyzed by eye, the magnitude of astigmatism post-TPS treatment was higher in 52% eyes, unchanged (±0.125 D) in 24% and lower in 24% of eyes (Figure 5). TPS treatment also changed the axis of orientation of cylinder in 7 eyes (WTR, ATR, oblique; based upon 30° definition) as shown in Table 1.
Figure 4.
Single angle vector plot for pre-TPS (A) versus post-TPS (B) keratometric astigmatism.
Abbreviation: TPS, thermal pulsation system.
Figure 5.
Frequency distribution histogram of difference between pre-TPS and post-TPS keratometric astigmatism.
Abbreviation: TPS, thermal pulsation system.
Table 1.
Change in Treatment Type (None, LRI, or Toric IOL) Determined from Pre-TPS vs Post-TPS Keratometry
| Post-TPS Treatment Type | ||||||
|---|---|---|---|---|---|---|
| None | LRI | Toric IOL | Total | |||
| Pre-TPS treatment plan | None | n | 7 | 6 | 2 | 15 |
| % | 28 | 24 | 8 | 60 | ||
| LRI | n | 1 | 4 | 0 | 5 | |
| % | 4 | 16 | 0 | 20 | ||
| Toric IOL | n | 0 | 1 | 4 | 5 | |
| % | 0 | 4 | 16 | 20 | ||
| Total | n | 8 | 11 | 6 | 25 | |
| % | 32 | 44 | 24 | 100 | ||
Notes:
 , increase in treatment type;
, increase in treatment type;  , decrease in treatment type;
, decrease in treatment type;  , no change in treatment type.
, no change in treatment type.
The planned astigmatism management approach changed in 10 eyes based on the change in keratometry following TPS treatment (Table 2). Two eyes requiring no astigmatism correction based on pre-TPS keratometry were found to require toric IOL implantation according to post-TPS keratometry; 6 eyes shifted from no astigmatism correction to LRI, 1 eye shifted from toric to LRI, and 1 eye shifted from LRI to no treatment required.
Table 2.
Change in the Axis of Keratometric Astigmatism from Pre-TPS to Post-TPS
| Post-TPS K axis | ||||||
|---|---|---|---|---|---|---|
| WTR (60–120) | ATR (0–30, 150–180) | OBL (30–60, 120–150) | Total | |||
| Pre-TPS K axis | WTR (60–120) | n | 3 | 1 | 2 | 6 |
| % | 12.0 | 4.0 | 8.0 | 24.0 | ||
| ATR (0–30, 150–180) | n | 1 | 12 | 1 | 14 | |
| % | 4.0 | 48.0 | 4.0 | 56.0 | ||
| OBL (30–60, 120–150) | n | 1 | 1 | 3 | 5 | |
| % | 4.0 | 4.0 | 12.0 | 20.0 | ||
| Total | n | 5 | 14 | 6 | 25 | |
| % | 20.0 | 56.0 | 24.0 | 100.0 | ||
Notes:
 , axis of orientation changed;
, axis of orientation changed;  , no change in axis of orientation.
, no change in axis of orientation.
Discussion
Increasing awareness of the impact of dry eye and MGD on keratometry has led to the recommendation that patients undergoing refractive cataract surgery with premium IOLs be treated for dry eye; however, it has not been studied systematically.
Due to the widely held belief that dry eye induces corneal steepening, it was our expectation that improving ocular surface health with TPS would reduce post-TPS keratometric astigmatism. Instead, we were surprised to find that the magnitude of post-TPS astigmatism was actually higher than pre-TPS astigmatism in the majority of eyes (52%), and lower in 24% of eyes (Figure 5). In addition, a change in the axis of orientation of the cylinder was also observed in 7 eyes (WTR/ATR/oblique).
With the changes in astigmatism magnitude and axis of orientation, the planned astigmatism management modality also changed in 10 eyes (Table 1), with 8 of those eyes requiring a higher level of astigmatism management than anticipated before TPS treatment and 2 shifting to a lower level of astigmatism management. In 7 other eyes, although the management approach did not change, there were still changes in astigmatism magnitude and/or axis that led to adjustments to the surgical management plan (ie, a different power toric IOL). Among the 17 eyes with a change in the planned astigmatism management approach, double angle vector plots (Figure 3) show that actual RRA was lower than the simulated RRA that would have been obtained using the pre-TPS keratometry and astigmatism management plan.
While a larger study population would help to further delineate the proportion of eyes likely to experience an increase or decrease in astigmatism following dry eye therapy, this pilot study clearly shows that an unhealthy corneal surface leads to unpredictable measurement of astigmatism. Contrary to common belief, the measured astigmatism may be more or less than the actual corneal astigmatism, potentially leading the surgeon to over- or under-correct astigmatism. Not only could this yield suboptimal outcomes for patients who desire spectacle independence, but the selection of less suitable methods of astigmatism management could also have a negative financial impact on the practice or the patient.
A clinical threshold of 0.50 D astigmatism is commonly used to assess the efficacy of astigmatic treatment modalities. Actual RRA within 0.50 D was achieved in 76% of eyes compared to 40% eyes with simulated RRA (p=0.004). Thus, using post-TPS astigmatism measurement to plan for astigmatic management allowed 36% more eyes to achieve the clinical target of ≤0.50 D for good uncorrected distance vision. In fact, 7 eyes (28%) had simulated RRA ≥1.00 D, which would be likely to significantly degrade uncorrected vision.
Astigmatism correction is fundamental to the optimal functioning of presbyopia-correcting IOLs; as little as 0.50 D of astigmatism may degrade visual quality and may leave a patient symptomatic with visual blur, ghosting, and halos. It is reasonable to assume that treatment decisions based on post-TPS keratometry would help improve the performance of presbyopia-correcting IOLs, as well.
Optimal refractive outcomes in eyes with astigmatism depend on a number of factors other than accurate measurement of cylinder. These include the use of modern IOL power calculation formulae, consideration of posterior corneal astigmatism, good estimation of surgically induced astigmatism, cyclotorsion compensation, and precise alignment of the toric IOL on the intended treatment axis.
TPS treatment was used based on its reported efficacy for MGD. In the present study, the number of functioning meibomian glands and the quality and quantity of meibum were not recorded, which may be considered a limitation of the study. The retrospective study design and small sample size of the present study are other limitations. Future studies with a prospective study design and larger data set are needed to validate the findings of this pilot study. In patients with aqueous deficient or combination forms of dry eye, other treatments may be needed to stabilize the ocular surface, instead of or in conjunction with TPS.18
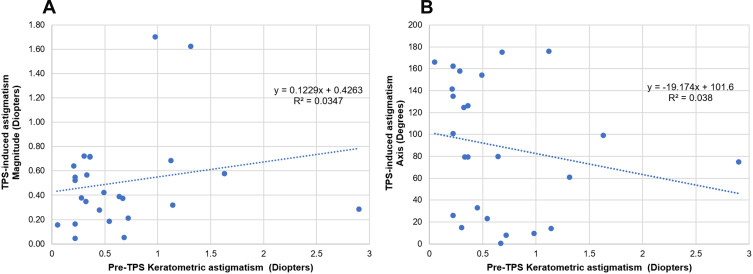
Of note, it is not possible to predict the expected change in astigmatism following dry eye therapy based on any of the preoperative characteristics we studied. While astigmatism increased or decreased following TPS in 76% of eyes, there was no change in astigmatism in 24% eyes. We ran a post-hoc correlation analysis between the magnitude of pre-TPS astigmatism and magnitude of the vectoral change in astigmatism (following TPS treatment) and found no correlation (Figure 6A). A similar comparison of the magnitude of pre-TPS astigmatism and axis of the vectoral change in astigmatism also revealed no correlation between the studied parameters (Figure 6B). The current study seems to suggest that all eyes presenting with cataract and concomitant dry eye must be carefully examined and, if needed, treated for dry eye prior to performing keratometry and determining the surgical plan for astigmatism management.
Figure 6.
Scatter plots (A) between TPS-induced change in astigmatism magnitude and pre-TPS keratometric astigmatism;, and(B) between change in astigmatism axis and pre-TPS keratometric astigmatism.
Abbreviation: TPS, thermal pulsation system.
Acknowledgments
Raman Bedi, MD (IrisARC – Analytics, Research & Consulting, Chandigarh, India) and Jan Beiting (Wordsmith Consulting, Cary, NC, USA) provided research, statistics, and editorial assistance in the preparation of this manuscript.
Disclosure
The financial support for biostatistical analysis, medical writing, and manuscript preparation was provided by J&J Vision, but they provided no support for the study itself. CM is a consultant to J&J Vision and reports no other possible conflicts of interest in this work.
References
- 1.Michelitsch M, Ardjomand N, Vidic B, Wedrich A, Steinwender G. [Prevalence and age-related changes of corneal astigmatism in patients before cataract surgery]. Ophthalmologe. 2017;114(3):247–251. doi: 10.1007/s00347-016-0323-8 German. [DOI] [PubMed] [Google Scholar]
- 2.Mohammadi M, Naderan M, Pahlevani R, Jahanrad A. Prevalence of corneal astigmatism before cataract surgery. Int Ophthalmol. 2016;36(6):807–817. doi: 10.1007/s10792-016-0201-z [DOI] [PubMed] [Google Scholar]
- 3.Day AC, Dhariwal M, Keith MS, et al. Distribution of preoperative and postoperative astigmatism in a large population of patients undergoing cataract surgery in the UK. Br J Ophthalmol. 2019;103(7):993–1000. doi: 10.1136/bjophthalmol-2018-312025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miyake T, Kamiya K, Amano R, Shimizu K. [Corneal astigmatism before cataract surgery]. Nippon Ganka Gakkai Zasshi. 2011;115(5):447–453. Japanese. [PubMed] [Google Scholar]
- 5.Chantra S, Jamtubtim S. Effects of dry eyes on corneal keratometry measured by VERIONTM image guided system. J Med Assoc Thai. 2018;101(2):115. [Google Scholar]
- 6.Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The prospective health assessment of cataract patients’ ocular surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423–1430. doi: 10.2147/OPTH.S120159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276–283. doi: 10.1016/j.jtos.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 8.Doğan AŞ, Gürdal C, Köylü MT. Does dry eye affect repeatability of corneal topography measurements? Turk J Ophthalmol. 2018;48(2):57. doi: 10.4274/tjo.10179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015;41(8):1672–1677. doi: 10.1016/j.jcrs.2015.01.016 [DOI] [PubMed] [Google Scholar]
- 10.Núñez MX, Henriquez MA, Escaf LJ, et al. Consensus on the management of astigmatism in cataract surgery. Clin Ophthalmol. 2019;13:311. doi: 10.2147/OPTH.S178277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zemova E, Eppig T, Seitz B, et al. Interaction between topographic/tomographic parameters and dry eye disease in keratoconus patients. Curr Eye Res. 2014;39(1):1–8. doi: 10.3109/02713683.2013.798667 [DOI] [PubMed] [Google Scholar]
- 12.Galvis V, Sherwin T, Tello A, Merayo J, Barrera R, Acera A. Keratoconus: an inflammatory disorder? Eye. 2015;29(7):843. doi: 10.1038/eye.2015.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMonnies CW. Eye rubbing type and prevalence including contact lens ‘removal‐relief’rubbing. Clin Exp Optom. 2016;99(4):366–372. doi: 10.1111/cxo.12343 [DOI] [PubMed] [Google Scholar]
- 14.Kim MJ, Stinnett SS, Gupta PK. Effect of thermal pulsation treatment on tear film parameters in dry eye disease patients. Clin Ophthalmol. 2017;11:883–886. doi: 10.2147/OPTH.S136203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Satjawatcharaphong P. Effects of LipiFlow treatment on dry eye symptoms, tear film stability, and meibomian gland expression 1Pam Satjawatcharaphong, 1Yixiu Zhou, 1, 2Meng C. Lin 1. UC Berkeley, School of Optometry, Clinical Research Center 2. UC Berkeley, Vision Science Graduate Group. Invest Ophthalmol Vis Sci. 2014;55(13):32. [Google Scholar]
- 16.Greiner JV. A single LipiFlow(R) Thermal Pulsation System treatment improves meibomian gland function and reduces dry eye symptoms for 9 months. Curr Eye Res. 2012;37(4):272–278. doi: 10.3109/02713683.2011.631721 [DOI] [PubMed] [Google Scholar]
- 17.Hill W, Osher R, Cooke D, et al. Simulation of toric intraocular lens results: manual keratometry versus dual-zone automated keratometry from an integrated biometer. J Cataract Refract Surg. 2011;37(12):2181–2187. doi: 10.1016/j.jcrs.2011.06.028 [DOI] [PubMed] [Google Scholar]
- 18.Greiner JV. Long-term (3 Year) effects of a single thermal pulsation system treatment on meibomian gland function and dry eye symptoms. Eye Contact Lens. 2016;42(2):99–107. doi: 10.1097/ICL.0000000000000166 [DOI] [PubMed] [Google Scholar]