Abstract
Introduction
Many dermatological conditions require extraction of material from the lesion followed by visualization under a microscope. However, visualization of the extracted material can be done using a dermoscope instead. We propose “extraction dermoscopy” as an addition to the already existing treasury that dermoscopy holds.
Methods
After approval from the institutional ethics committee, a cross-sectional study was carried out in a tertiary care hospital. Polarized and non-polarized versions of in vivo dermoscopy, as well as extraction dermoscopy, were performed on a total of 77 lesions, including 5 eruptive vellus hair cysts, 2 cilia incarnata externum, 10 trichostasis spinulosa, 20 keratosis pilaris, 20 molluscum contagiosum, and 20 lesions of milia. Heine Delta 20T and Dino-Lite Premier AM4113T were employed for dermoscopic examination.
Results
A total of 77 lesions were selected, including 5 eruptive vellus hair cysts, 2 cilia incarnata externum, 10 trichostasis spinulosa, 20 keratosis pilaris, 20 molluscum contagiosum, and 20 lesions of milia. Extraction dermoscopy of the eruptive vellus cysts revealed skin color to brownish colored cysts with a bunch of pigmented hair. Similarly, findings of all other lesions were described and recorded post-extraction.
Conclusion
Extraction dermoscopy helps confirm the diagnosis without visualization under a microscope. Its application in recent times makes the explanation of the nature of many disorders to patients easier, and demonstration of extracted lesions may further improve doctor-patient communication.
Keywords: Extraction dermoscopy, Epiluminescence microscopy, Eruptive vellus hair cyst, Cilia incarnata, Keratosis pilaris, Trichostasis spinulosa, Molluscum contagiosum, Milia
Introduction
The dynamic nature of the dermatoscope has expanded its use exponentially across various classes of dermatology. Newer patterns and findings continue to be described regularly. Furthermore, the art of dermoscopy has been made more specific with the use of terminologies that are used to describe specific indications, such as pigmentaroscopy, trichoscopy (dermoscopy of scalp and hair), onychoscopy (nails), inflammoscopy (inflammatory dermatosis), and entomodermoscopy (skin infestations and infections) [1, 2]. Many dermatological conditions require extraction of material from the lesion followed by visualization under a microscope. However, visualization of the extracted material can be done using a dermoscope instead. We propose “extraction dermoscopy” as an addition to the already existing treasury that dermoscopy holds.
Methods
After approval from the institutional ethics committee, a cross-sectional study was carried out in a tertiary care hospital. Demographic data and clinical variables were recorded after obtaining written informed consent. Polarized and non-polarized versions of in vivo dermoscopy, as well as extraction dermoscopy, were performed on a total of 30 patients, with a total of 77 lesions selected for extraction dermoscopy for the following conditions (eruptive vellus hair cyst, cilia incarnata externum, trichostasis spinulosa, keratosis pilaris, molluscum contagiosum, and milia), and the findings were recorded respectively. Heine Delta 20T and Dino-Lite Premier AM4113T were employed for dermoscopic examination.
Results
A total of 77 lesions from 30 patients (17 males and 13 females) were selected. The age of the patients ranged from 6 to 45 years. The 77 lesions included 5 eruptive vellus hair cysts, 2 cilia incarnata externum, 10 trichostasis spinulosa, 20 keratosis pilaris, 20 molluscum contagiosum, and 20 lesions of milia.
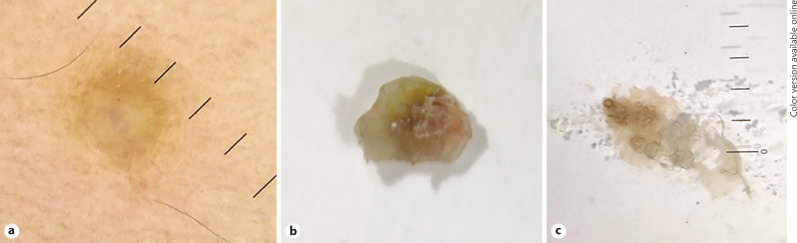
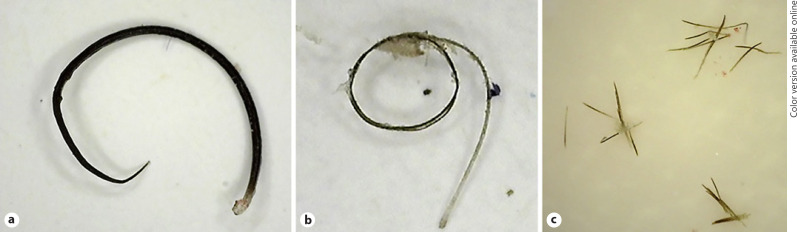
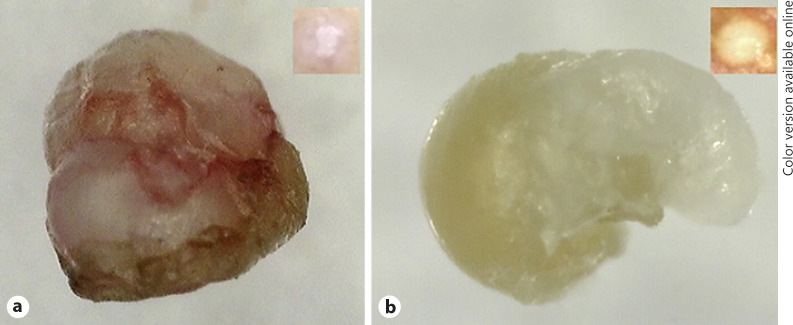
In vivo dermoscopy of eruptive vellus hair cysts showed bluish dome-shaped papules surrounded by a hyperpigmented halo. Needling of the papules followed by extraction of its contents revealed skin color to brownish colored cysts with a bunch of pigmented hair when seen under a dermoscope (Fig. 1). In case of cilia incarnata externum, we gave a nick with a needle at the eyelid margin that facilitated the impacted hair to pop out, which was then plucked and visualized under the dermatoscope. The coiled nature of the follicle was revealed on dermoscopy (Fig. 2a). Dermoscopic examination of trichostasis spinulosa revealed hair within follicular openings, and on needling, expression of a tuft of vellus hair was appreciated under the dermatoscope (Fig. 2c). Dermoscopy of keratosis pilaris showed looped and circular hair shafts within follicular openings. Extraction dermoscopy examination of this hair revealed retention of the coiled nature of hair (Fig. 2b). Extraction dermoscopy of lesions of molluscum contagiosum revealed white bodies with visible vessels running across the surface of the body (Fig. 3a). Dermoscopy of lesions of milia extracted revealed yellow-white “pearl-like” circular keratinous material (Fig. 3b).
Fig. 1.
a Eruptive vellus hair cyst: in vivo dermoscopy showing hyperpigmented papule with bluish hue in the center (×10, polarized mode, Heine Delta 20T dermatoscope). b Eruptive vellus hair cyst: extraction dermoscopy showing brown colored cyst (×10, polarized mode, Heine Delta 20T dermatoscope). c Eruptive vellus hair cyst: extraction dermoscopy showing bunch of pigmented hair after rupturing the cyst (×10, polarized mode, Heine Delta 20T dermatoscope).
Fig. 2.
a Cilia incarnata externum: extraction dermoscopy revealing the coiled nature of misdirected hair (×50, polarized mode, Dino-Lite Premier AM4113T). b Keratosis pilaris: extraction dermoscopy showing circular hair shaft from a lesion (×50, polarized mode, Dino-Lite Premier AM4113T). c Trichostasis spinulosa: tuft of vellus hair seen on extraction dermoscopy of trichostasis spinulosa (×50, polarized mode, Dino-Lite Premier AM4113T).
Fig. 3.
a Molluscum contagiosum: extraction dermoscopy showing a white globular molluscum body with overlying crown vessels with in vivo dermoscopy of the same lesion (inset) (×50, polarized mode, Dino-Lite Premier AM4113T). b Milia: extraction dermoscopy of milia showing yellow-white “pearl-like” circular keratinous material, with in vivo dermoscopy of the same (inset) (×200, polarized mode, Dino-Lite Premier AM4113T).
Discussion
Extraction dermoscopy involves in vitro examination of a lesion immediately after its removal from the body with the help of a dermatoscope. It holds its utility in various lesions which pose a diagnostic challenge to the treating clinician, thereby obviating the need for biopsy. Needling of papules of eruptive vellus hair cyst followed by extraction of its contents revealed a bunch of pigmented hair within the cyst. Daulatabad et al. [3] as well reported a cluster of multiple pigmented vellus hair present in a membrane-bound brown structure, giving the appearance of a bundle of wool on extraction and dermoscopic examination. In the case of cilia incarnata externum, the coiled nature of the follicle was revealed on dermoscopy, thereby reflecting the cause of misdirection. Trichostasis spinulosa, initially named “Pinselhaar” (paintbrush hair), presents as black macules on the nose. Dermoscopic examination reveals hair within follicular openings. The real beauty is appreciated after plucking the hair and visualization under a dermoscope. Extraction dermoscopy of keratosis pilaris reveals retention of the coiled nature of hair. It was believed that the “loss-of-function” mutations in the structural protein filaggrin leading to epithelial barrier abnormality were the primary pathogenetic mechanism in keratosis pilaris [4]. However, the finding of coiled hair indicates that the defect may not be of keratinization, but of the circular hair shaft which ruptures the follicular epithelium, leading to inflammation and abnormal follicular keratinization as reported by Thomas et al. [5]. In cases of molluscum contagiosum, the presence of intact vessels running across the surface of the molluscum body explains the in vivo finding of crown vessels. In all the above cases, extraction dermoscopy helped confirm the diagnosis without visualization under a microscope.
Conclusion
The application of dermoscopy has made the explanation of the nature of many disorders to patients easier, and further demonstration of extracted lesions improves the doctor-patient communication by an assurance of the lesion being removed. Extraction dermoscopy not only has diagnostic and therapeutic implications but also opens avenues for further research on the pathogenesis and therapy of various conditions.
Statement of Ethics
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The subjects have given their written informed consent, and the study protocol was approved by the institute's ethics committee.
Disclosure Statement
The authors declare that there are no conflicts of interest.
Funding Sources
The authors did not receive any funding.
Author Contributions
| Contributor 1 | Contributor 2 | Contributor 3 | Contributor 4 | Contributor 5 | |
|---|---|---|---|---|---|
| Concepts | ✓ | ||||
| Definition of intellectual content | ✓ | ✓ | ✓ | ||
| Literature search | ✓ | ||||
| Clinical studies | |||||
| Experimental studies | |||||
| Data acquisition | ✓ | ✓ | ✓ | ✓ | |
| Data analysis | ✓ | ✓ | |||
| Statistical analysis | |||||
| Manuscript preparation | ✓ | ||||
| Manuscript editing | ✓ | ||||
| Manuscript review | ✓ | ✓ | |||
| Guarantor | ✓ | ✓ |
References
- 1.Rosendahl C. Dermatoscopy in general practice. Br J Dermatol. 2016;175((4)):673–4. doi: 10.1111/bjd.14609. [DOI] [PubMed] [Google Scholar]
- 2.Errichetti E, Stinco G. Dermoscopy in general dermatology: a practical overview. Dermatol Ther. 2016;6((4)):471–507. doi: 10.1007/s13555-016-0141-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daulatabad D, Grover C, Sharma S. “Extraction dermoscopy” as a rapid and innovative diagnostic tool for eruptive vellus hair cyst. Clin Exp Dermatol. 2017;42((4)):438–40. doi: 10.1111/ced.13096. [DOI] [PubMed] [Google Scholar]
- 4.O'Regan GM, Sandilands A, McLean WH, Irvine AD. Filaggrin in atopic dermatitis. J Allergy Clin Immunol. 2009;124((3 Suppl 2)):R2–6. doi: 10.1016/j.jaci.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Thomas M, Khopkar US. Keratosis pilaris revisited: is it more than just a follicular keratosis? Int J Trichology. 2012;4((4)):255–8. doi: 10.4103/0974-7753.111215. [DOI] [PMC free article] [PubMed] [Google Scholar]