To the Editor,
We read with great interest the review by Walsh and colleagues1 summarising the evidence on the detection pattern and viral load of SARS-CoV-2 over the course of an infection (including any asymptomatic or pre-symptomatic phase), and the duration of infectivity. Even though the authors concluded that the duration of COVID-19 infectivity remains uncertain, this is really an important issue for the international audience. In fact, most of the studies on COVID-19 primarily focused on epidemiological, clinical, biological and radiological characteristics of patients with confirmed SARS-CoV-2 infection.2 However, only few studies addressed the importance of the follow-up of recovered patients.
After the acute phase of SARS-CoV-2 epidemic infection, the Fondazione Policlinico A. Gemelli IRCSS of Rome established a post-acute care service for patients discharged from the hospital. Only the subjects who met the following WHO criteria for hospital discharge and/or discontinuation of quarantine have been admitted to the follow-up: a) subject must be fever-free without fever-reducing medications for three consecutive days; b) subject must show an improvement in any other symptoms, including reduced coughing and shortness of breath; c) at least seven days have passed since the onset of symptoms; d) in addition to these requirements, person must test negative for the SARS-CoV-2 virus twice, with the real-time reverse transcriptase-polymerase chain reaction (RT-PCR) tests for COVID-19 nucleic acid taken at least 24 h apart. If the symptom and testing conditions are met, both WHO and US Centers for Disease Control and Prevention consider the subject officially recovered from COVID-19 disease.3
During the first week of post-acute care activity, 29 patients recovered from COVID-19 disease were recalled being assessed.4 , 5 Even though the patients were formally considered recovered from COVID-19 disease, a new RT-PCR test was repeated at the time of post-acute care admission. This study by the Catholic University / Fondazione Policlinico Gemelli IRCCS Institutional Ethics Committee (protocol ID number: 0013008/20).
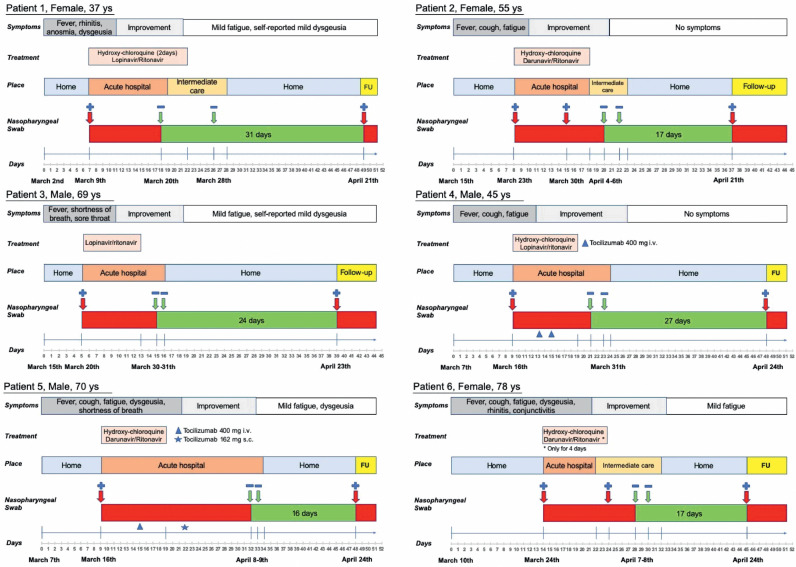
Of the 29 patients who repeated the nasopharyngeal swab, 6 patients (20,6%) tested positive again. All these 6 patients were exposed to the SARS-CoV-2 infection at least one month before (Fig. 1 ). Three were male and the mean age was 59,0 ± 15,9 years (range from 37 to 78 years). All patients had fever as the onset of the COVID-19 infection. The other most frequently observed symptoms were cough, dyspnea, fatigue and dysgeusia. One patient reported symptoms of conjunctivitis, too. The mean number of days before admission to the hospital was 8,6 ± 3,1. All patients had positive RT-PCR test results at the time of hospital admission and the antero-posterior chest radiograph showing patchy ground-glass opacities. Only two patients (numbers 1 and 5) also performed the chest CT scan showing diffuse ground-glass opacities with some consolidation area. Overall, the severity of disease was mild to moderate.
Fig. 1.
Main characteristics of the patients according to the duration of symptoms, treatment, days of hospitalization, and nasopharyngeal swabs execution.
Antiviral treatment was provided for all the 6 patients. Three patients received lopinavir/ ritonavir 200/50 mg, 2 tablets x 2 per day for ten days and three patients received darunavir/ritonavir 800/100 mg, 1 tablet per day for ten days. Four subjects received hydroxychloroquine 200 mg, 1 tablet x 2 per day for ten days. One subject received hydroxychloroquine for only two days. Two patients (number 4 and 5) with more severe respiratory symptoms were treated with antiinterleukin-6-receptor monoclonal antibody medication (Tocilizumab). The three male patients required oxygen therapy during hospital stay, too.
The mean hospital stay, including intermediate care, was 17,5 ± 4,9 days. All patients before hospital discharge showed a clear improvement in COVID-19 disease related symptoms and had two consecutive negative RT-PCR test results. The mean time from the onset of SARS-CoV-2 infection symptoms to recovery was 22,3 ± 6,4 days (ranged from 15 to 32 days). After hospital discharge, patients stayed home with no isolation requirement for a mean of 18,2 ± 5,0 days (ranged from 13 to 24 days). During this period patients continue to be substantially asymptomatic or with mild symptoms. In compliance with the lock-down rules in force in Italy at that time, they had contact with family members and left the house for the needs of daily life, such as shopping in the supermarket. Two patients had returned to work. Finally, they did not report contact with person with COVID-19 disease related symptoms, such as fever, cough, fatigue, myalgia, shortness of breath, and sore throat and they declared no family member infected at the time of post-acute care admission, too.
These findings suggest that a significant proportion of recovered COVID-19 disease patients still could be potentially asymptomatic carriers of the virus. While false-negative RT-PCR test results have been previously described, two consecutive negative RT-PCR test results together with the clinical evidence of symptoms improvement clearly suggest that these six patients were eligible to be declare as COVID-19 recovered and as consequence for hospital discharge and discontinuation of quarantine.
As an emerging and new infectious disease, the clinical and virologic course of SARS-CoV-2 infection remain to be better investigated. These case series of COVID-19 patients highlight important characteristics that need to be considered, including extensive clinical course, persistent fragments of the virus's RNA during recovery period, and the potential failure of viral antibody for a real virus clearance. As a consequence, the criteria for discontinuation of quarantine and the patient management with a specific follow-up protocols need to be evaluated.6 It is absolutely mandatory to make sense of patients who seem to have recovered from COVID-19 but who still test positive for the virus based on nasopharyngeal swabs. This will be a very important contribution to understanding both the natural history of COVID-19 as well as the public health implications of viral shedding. Scientific evidence on the new coronavirus and COVID-19 increases day by day and guidelines about the recovery criteria will continue to change.1 However, the main question for the containment of the SARS-Cov-2 pandemic infection that still needs to be answered is: "Does viral detection mean that the patient is still contagious?". Tests are conducted using PCR – polymerase chain reaction – which looks for tiny sections of the RNA of the virus. This type of test can reveal whether a patient is still shedding viral debris but are not able to indicate whether the person is still infectious.7
Declaration of Competing Interest
All authors have no conflict of interest.
Acknowledgments
Abbreviations
None.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Università Cattolica del Sacro Cuore (Rome, Italy) (protocol ID number: 0013008/20). Specifically, for this paper there is no chance that a patient can be identified (or can identify themselves) from the text and/or figure. Written informed consents have been obtained.
Consent for publication
Not applicable.
Availability of data and material
All the data and material are available by emailing the corresponding author.
Consent for publication
The author gives consent for publication of this paper.
Funding
None
Authors' contributions
LF and RB coordinated the overall study.
LF, CF, TM, BF, BG, BV, and CA were involved in the concept and the design of the study.
FL, GE, and RE drafted the manuscript.
LMMR, MAM, PF, PA, PL, RS, SA, SM, and GA contributed to the acquisition and the interpretation of the data.
All the authors revised the manuscript and approved its final version.
The Gemelli Against COVID-19 Post-Acute Care Study Group is composed as follows
Steering committee: Landi F, Gremese E
Coordination: Bernabei R, Fantoni M, Gasbarrini A
Field investigators:
Gastroenterology team: Settanni CR
Geriatric team: Benvenuto F, Bramato G, Brandi V, Carfì A, Ciciarello F, Lo Monaco MR, Martone AM, Marzetti E, Napolitano C, Pagano F, Rocchi S, Rota E, Salerno A, Tosato M, Tritto M, Calvani R, Catalano L, Picca A, Savera G
Infectious disease team: Cauda R, Tamburrini E, Borghetti A, Di Gianbenedetto S, Murri R, Cingolani A, Ventura G, Taddei E, Moschese D, Ciccullo A
Internal Medicine team: Stella L, Addolorato G, Franceschi F, Mingrone G, Zocco MA
Microbiology team: Sanguinetti M, Cattani P, Marchetti S
Neurology team: Bizzarro A, Lauria A
Ophthalmology team: Rizzo S, Savastano MC, Gambini G, Cozzupoli GM, Culiersi C
Otolaryngology team: Passali GC, Paludetti G, Galli J, Crudo F, Di Cintio G, Longobardi Y, Tricarico L, Santantonio M
Pediatric team: Buonsenso D, Valentini P, Pata D, Sinatti D, De Rose C
Pneumology team: Richeldi L, Lombardi F, Calabrese A
Psychiatric team: Sani G, Janiri D, Giuseppin G, Molinaro M, Modica M
Radiology team: Pirronti T, Natale L, Larici AR, Marano R, Infante A, Larosa L
Rheumatology team: Paglionico A, Petricca L, Gigante L, Natalello G, Fedele AL, Lizzio MM
Vascular team: Santoliquido A, Santoro L, Nesci A, Popolla V
Acknowledgment
The Gemelli Against COVID-19 Post-Acute Care team thanks La Torre R, Brisetti S, Fella L, Sofo MT and all the nursing staff of “Post-COVID Day Hospital Unit” for their extraordinary dedication and expertise in treating COVID-19 patients.
References
- 1.Walsh K.A., Jordan K., Clyne B., Rohde D., Drummond L., Byrne P. SARS-CoV-2 detection, viral load and infectivity over the course of an infection. J Infect. 2020;81(3):357–371. doi: 10.1016/j.jinf.2020.06.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rokadiya S., Gil E., Stubbs C., Bell D., Herbert R. COVID-19: outcomes of patients with confirmed COVID-19 re-admitted to hospital. J Infect. 2020;81(3):e18–e19. doi: 10.1016/j.jinf.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y., Chow A. Dancing with COVID-19 after the hammer is lifted: enhancing healthcare worker surveillance. J Infect. 2020 doi: 10.1016/j.jinf.2020.07.037. S0163-4453(20)30533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landi F., Barillaro C., Bellieni A. The new challenge of geriatrics: saving frail older people from the SARS-CoV-2 pandemic infection. J Nutr Health Aging. 2020 doi: 10.1007/s12603-020-1356-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gemelli Against COVID-19 Post-Acute Care Study Group Post-COVID-19 global health strategies: the need for an interdisciplinary approach. Aging Clin Exp Res. 2020:1–8. doi: 10.1007/s40520-020-01616-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lan L., Xu D., Ye G. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323(15):1502–1503. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Birgand G., Blanckaert K., Deschanvres C., Vaudron A., Loury P. King L; Group for Covid-19 control in Vendée. Testing strategies for the control of COVID-19 in nursing homes: universal or targeted screening? J Infect. 2020 doi: 10.1016/j.jinf.2020.08.002. S0163-4453(20)30535-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data and material are available by emailing the corresponding author.