Abstract
This study from the Chinese CDC describes epidemiologic features of a second outbreak of COVID-19 in Beijing, China, in June and July 2020, and the public health response that contained it.
Since its initial outbreak in Wuhan, China, between December 2019 and March 2020,1,2,3,4 severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has quickly spread worldwide. Although the epidemic abated in China, a second outbreak began in June 2020 in Beijing. We assessed preliminary Beijing outbreak data and present a timeline of the investigation and public health response.
Methods
Data from case reports and associated records for all individuals with a positive SARS-CoV-2 reverse transcriptase–polymerase chain reaction (RT-PCR) test result in Beijing (excluding imported cases) from June 11 to July 10, 2020, were extracted from national public health databases.2,4 Case definition included coronavirus disease 2019 (COVID-19)–like symptoms plus a positive SARS-CoV-2 RT-PCR test result from a nasopharyngeal swab. If positive but asymptomatic, the individual was considered to have asymptomatic infection and not counted as a confirmed case.5 Active and passive surveillance was ongoing in Beijing at the time of the outbreak.4 Cases were required to be reported within 2 hours of diagnosis and investigated within 24 hours of reporting.3 Only 1 case was required to trigger an alert. Response plans dictated immediate personnel deployment, aggressive case finding and contact tracing, isolation of cases and asymptomatic persons, quarantining of close contacts, movement restrictions, and thorough environmental testing.4 Epidemiologic curves present number of confirmed cases by date of diagnosis and date of symptom onset. Given the public health emergency, individual informed consent was not required. The institutional review boards of the Chinese Center for Disease Control and Prevention and the Beijing Center for Disease Prevention and Control approved this study.
Results
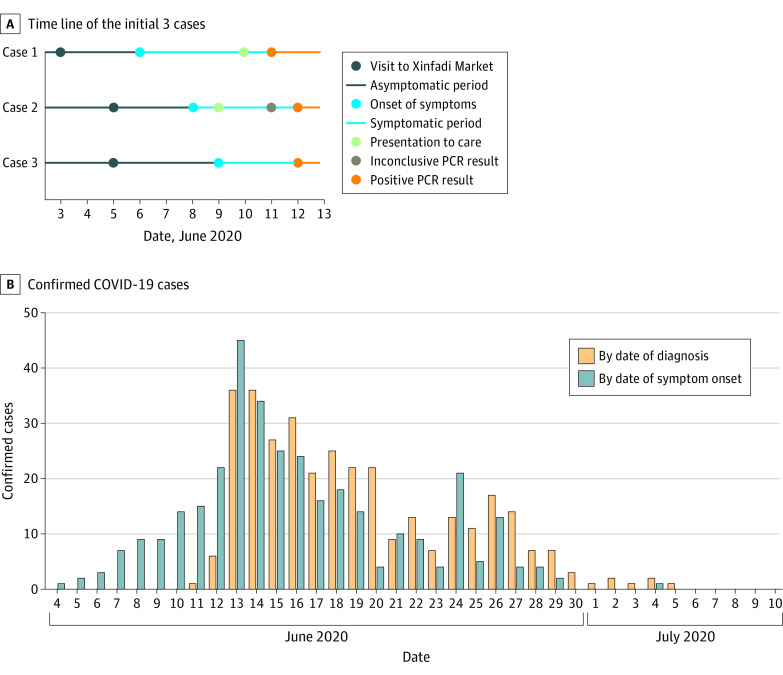
After 56 consecutive days of no local transmission events in Beijing, the first new case of COVID-19 was diagnosed on June 11 in a man in his 50s with headache, fever, and infiltrates on chest computed tomography scan but no contact or travel history. An outbreak alert was triggered that same day (Figure). The first 2 confirmed cases had epidemiologic links to the Xinfadi Agricultural Wholesale Market and had no other locations, persons, or events in common during the prior 14 days. The market was shut on June 12. All market workers, recent visitors, close contacts of cases, and residents of surrounding communities were actively sought for RT-PCR testing. A total of 335 confirmed cases were diagnosed, and another 33 persons with asymptomatic infection were identified. All were isolated and treated in Beijing Ditan Hospital. The interval from earliest symptom onset (June 4) to first confirmed case and outbreak alert (June 11) was 7 days, with community containment measures implemented within 24 hours (Figure). Ninety-three persons (27.8%) were presymptomatic at time of diagnosis. Among the 368 persons isolated and treated, 272 (73.9%) had epidemiologic links to the market—169 (46%) were market workers and 103 (28%) were visitors. The remaining 96 (26%) were close contacts of the other cases. Among the 169 market workers, 79 (47%) were seafood vendors, 33 (20%) dried fruit/vegetable vendors, 30 (18%) meat vendors, 14 (8%) bean product vendors, and 13 (8%) cleaners or drivers. After July 5, no further cases were detected.
Figure. Time Course of the COVID-19 Outbreak in Beijing, China—June 11 to July 10, 2020.
A, Case 1 was a man in his 50s with headache, fever, and chest imaging showing pneumonia. Only 2 environmental samples from places he had visited were positive for severe acute respiratory syndrome coronavirus 2, both from Xinfadi Market. Case 2 was a man in his 20s with sore throat, runny nose, and fever who had also visited Xinfadi Market. Case 3 was a man in his 30s with sore throat, cough, and headache, was a close contact of case 2, and had also visited Xinfadi Market. A team was dispatched to the market on June 12, where they screened more than 500 people and took additional environmental samples. More cases were found, and the market was shut down the same day. All persons inside were immediately quarantined. Starting on June 13, response measures escalated to accelerate case finding and isolation and contact tracing and quarantine. Moreover, active testing and epidemiologic investigation were expanded to nearby areas, movement restrictions were implemented, and quarantine times were lengthened. B, Epidemic curves of the outbreak displayed as confirmed coronavirus disease 2019 (COVID-19) cases by date of diagnosis and by date of symptom onset. PCR indicates polymerase chain reaction.
Discussion
An outbreak of SARS-CoV-2 infection in Beijing was rapidly detected and contained, based on lessons learned from the Wuhan outbreak.4 The findings highlight the benefit of highly sensitive surveillance, immediate response, and rapid containment. Application of a risk assessment tool based on SARS-CoV-2 seeding and doubling times6 indicated there was high probability of the Beijing outbreak escalating. However, the speed and magnitude of the response was associated with lengthened doubling time and control of the outbreak and may have averted a large epidemic wave. The outbreaks in both Wuhan and Beijing were linked to seafood markets, but further investigation is required to determine the root cause. The main limitations of the study were that only preliminary case data were available, and results of environmental testing and response measures are still being analyzed. Nevertheless, this study underscores the effectiveness of sensitive surveillance, immediate investigation, and rapid response in combination with public health interventions in containing an outbreak of SARS-CoV-2.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Li Q; 2019-nCoV Outbreak Joint Field Epidemiology Investigation Team . An outbreak of NCIP (2019-nCoV) infection in China—Wuhan, Hubei Province, 2019–2020. China CDC Wkly. 2020;2(5):79–80. doi: 10.46234/ccdcw2020.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team . The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Wkly. 2020;2(8):113–122. doi: 10.46234/ccdcw2020.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. doi: 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 4.Zhou L, Wu Z, Li Z, et al. One hundred days of COVID-19 prevention and control in China. Clin Infect Dis. Published online June 5, 2020. doi: 10.1093/cid/ciaa725 [DOI] [Google Scholar]
- 5.Wu Z, McGoogan JM. Asymptomatic and pre-symptomatic COVID-19 in China. Infect Dis Poverty. 2020;9(1):72. doi: 10.1186/s40249-020-00679-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou L, Liu JM, Dong XP, McGoogan JM, Wu ZY. COVID-19 seeding time and doubling time model: an early epidemic risk assessment tool. Infect Dis Poverty. 2020;9(1):76. doi: 10.1186/s40249-020-00685-4 [DOI] [PMC free article] [PubMed] [Google Scholar]