Summary
Background
There are indications that prehypertension precedes hypertension. Like hypertension, it is associated with increased cardiovascular risk.
Objective
To determine the prevalence, awareness and correlates of prehypertension and hypertension among adults in Delta State, Nigeria.
Methods
This was a cross-sectional study. We recruited adults aged ≥18 years from two communities in Delta State, Nigeria, using the multi-stage sampling technique. The study instrument was a modified WHO-STEPS questionnaire. Prehypertension and hypertension were defined using the JNC-7 criteria. Ethical approval was obtained before the recruitment of participants.
Results
Of the 852 adults studied, the mean (±SD) age was 42.64 (±16.07) years, females (55.9%) and urban dwellers (55.8%). The prevalence of prehypertension and hypertension were 42.5% and 29.3%, respectively; both were higher among urban dwellers. The peak age-group for prehypertension and hypertension were 25–34 and 35–44 years, respectively. Awareness of hypertension was low; 12.0% (102/852). Blood pressure category significantly correlated with age, body mass index, place of residence, level of education, employment status and fruit intake.
Conclusion
The prevalence of prehypertension and hypertension in this study were high. Based on the premise that prehypertension is a precursor of hypertension and occurred more among youths, the higher prevalence of prehypertension gives an inkling to rising prevalence of hypertension.
Funding
Nil
Keywords: Prehypertension, hypertension, adults, Nigeria, WHO STEPS
Introduction
Noncommunicable diseases (NCD) are a growing source of public health concern worldwide. Cardiovascular disease (CVD) is the foremost contributor to NCD-related morbidity and mortality among adults.1 Several factors interplay in the aetiopathogenesis of cardiovascular disease, of which hypertension is a significant player. Hypertension develops from complex and inter-related aetiologies and risk factors. While a few are non-modifiable, others are lifestyle-related and thus modifiable.
Hypertension accounts for about half of the deaths from heart disease and stroke, and indeed 12.8% of total all-cause deaths globally.2 Several studies have demonstrated the benefits of prevention, early diagnosis and adequate control of hypertension.3–5 However, the global distribution of hypertension burden is inequitable as most of the deaths occur in low- and middle-income countries.2, 6 Whereas there is a decline in the prevalence of hypertension in many developed countries because of improved awareness and better treatment and control, the opposite appears to be the situation in low- and middle-income countries like Nigeria.
In a systematic review and meta-analysis of selected data from population-based studies between 1980–2013, Adeloye et al. showed that the pooled awareness rate of hypertension in Nigeria was only 17.4%.7 In another systematic review by Ogah et al., the pooled prevalence of hypertension in Nigeria increased from 8.6% to 22.5% between 1970–1979 and 2000–2011, respectively.8
The reported change in the prevalence rate of hypertension may be attributable to the upsurge in the aetiological risk factors for hypertension as well as the cut-off values used to define hypertension.
The definition of hypertension based on arbitrary blood pressure readings has evolved over the years. In the 1980s, the definition of hypertension was systolic blood pressure (SBP) of ≥160mmHg or diastolic blood pressure (DBP) of ≥95mmHg.9 In 2003, the report of the seventh Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-7) redefined hypertension as SBP ≥140mmHg or DBP ≥90mmHg and normal blood pressure as SBP <120mmHg and DBP <80mmHg.10 More recently, in 2017, the American Heart Association /American College of Cardiology further reduced the cut-off value for hypertension to SBP ≥130mmHg and DBP ≥80mmHg but retained the JNC-7 definition of normal blood pressure. 11
The gap between normal blood pressure reading and hypertension has also been differently defined and named. According to 2003 JNC-7 SBP of 120–139mmHg or DBP of 80–89mmHg is defined as prehypertension while the 2017 AHA /ACC guideline defines the gap as elevated blood pressure, 120–129mmHg (SBP) or 80mmHg (DBP). The prevalence and significance of prehypertension among adults are understudied, unlike hypertension. However, there are indications that prehypertension precedes hypertension and is associated with increased cardiovascular risk.12
Although several other studies have reported the prevalence of hypertension, its risk factors, socio-demographic correlates and barriers to care in Nigeria, there are only a few studies on prehypertension among adults in Nigeria. This paper, therefore, aims to describe the prevalence and correlates of prehypertension and hypertension among apparently healthy adults in Delta State, Nigeria.
Methods
The study design is cross-sectional, descriptive and population based. The study population was from among adults aged 18 years and above living in Delta State, Nigeria. Administratively, there are three senatorial districts in the State: Delta North, Delta South and Delta Central, and twenty-five Local Government Areas.
Recruitment of respondents was by multi-stage sampling method. Firstly, simple random sampling using balloting was used to select two out of the three Senatorial Districts in the State: Delta Central and Delta South. One study site was selected from each of the chosen senatorial districts using a non-probability convenience sampling method. A rural community, Jesse was selected from Delta Central while Warri, an urban metropolis was selected from Delta South. The study sites are 47 kilometres apart.
Whereas Jesse is sparsely populated and majorly agrarian, Warri is densely populated and the commercial hub of Delta State, especially as it relates to the oil and gas industry.
Furthermore, the eligibility criteria for recruitment were consenting apparently healthy adults aged at least 18 years who have lived in the study sites for at least one (1) year. Study participants were recruited using a two-stage cluster sampling method. Jesse, the rural study site, has seven clans which were considered as natural clusters. Adults who met the eligibility criteria were recruited from households within the natural clusters. Warri, the urban study site, has twelve (12) wards. Each ward was considered as a cluster. Because of their relatively large sizes, four (4) wards were randomly selected from the sampling frame of twelve wards. Each of the selected wards was a cluster. Adults within the households in the selected clusters who met the inclusion criteria were recruited until the sample size was reached. Visitors to the study sites and adult residents who had lived less than 1-year in the study sites were excluded from the study. Also, visibly pregnant women were excluded from the study as their anthropometric indices may result in skewed data.
Using the pooled prevalence of hypertension of 22.5%,8 and assuming a 95% confidence interval, 5% error margin (α) and a 10% non-response, the calculated minimum sample is two hundred and ninety-five (295) per study site. Before the commencement of the study, trained research assistants pre-tested the study instrument on 20 adults from Oghara, Delta State, a non-participating community. The World Health Organization STEPwise approach to chronic disease risk factor surveillance (WHO STEPS) questionnaire13 was modified by removing the section on biochemical measurements and adapted for use in this study.
The questionnaires were administered by the interviewer, and assessed socio-demographic profile, risk factors, awareness of the personal history of hypertension and care for hypertension. All the respondents had physical measurements of their anthropometry and blood pressure.
Each participant had their weight in kilograms and the height in metres measured after removing their footwear, head-dressing and heavy outer clothing with the Prestige HM0016D (India) stadiometer. The quotient of the weight and the square of the height defined the body mass index (BMI) in kg/m2. Overweight and obesity were BMI of 25.0–29.9kg/m2 and ≥30.0kg/m2, respectively irrespective of gender.14
A non-elastic tape was used to measure the waist circumference in centimetres. The waist circumference was measured twice in the horizontal plane at a level midway between the lower rib and the iliac crest, and the average calculated to minimise errors. Central obesity was defined as waist-to-height ratio (WHtR) ≥0.5.15
Blood pressure measurement was obtained using the Omron® BP-785 Intellisense automated sphygmomanometer in the right hand of seated respondents after at least 10 minutes rest. Blood pressure measurements were done thrice at an interval of 1 minute, and the average systolic and diastolic blood pressures calculated in mmHg. Classification of blood pressure readings was according to the JNC -7:10
Normal: SBP <120mmHg and DBP <80mmHg
Prehypertension: SBP 120–139mmHg, or DBP 80–89mmHg
Stage 1 Hypertension: SBP 140–159mmHg, or DBP 90–99mmHg
Stage 2 Hypertension: SBP ≥160mmHg, or DBP ≥100mmHg
Respondents who self-reported a history of hypertension as diagnosed by a healthcare professional were also classified as having hypertension, irrespective of their current blood pressure readings or use of anti-hypertensive drugs.
Definition of terms:
Ever smoked: This refers to respondents who have smoked cigarette ever; irrespective of their current smoking status.
Alcohol use: This refers to respondents who have ever drunk any alcoholic beverage (wine, spirit or beer); irrespective of the quantity drank.
Fruit intake: A portion of fruit is likened to one (1) medium-sized orange; irrespective of the type of fruit.
Added Salt: This refers to the practice of adding table salt to already cooked food; irrespective of the quantity and frequency of practice.
The independent variables were coded as either present or absent.
Ethical approval (DELSUTH/HREC/2015/002) was obtained from the Health Research Ethics Committee (HREC) of the Delta State University Teaching Hospital, Oghara prior to commencement of the study.
The conduct of this study was in line with the tenets of the Helsinki Declaration. Eligible persons were informed that participation in the study was voluntary, and they reserve the right to either decline or opt-out of the study at any time. Respondents who had either hypertension or prehypertension were encouraged to visit the nearest healthcare facility if they do not already have a healthcare provider.
The data from the questionnaire were checked for completeness, entered and analysed using the Statistical Package for Social Sciences (SPSS) version 22.0 (SPSS Inc, Chicago, IL, USA) software. Categorical variables were reported as frequencies, percentages, and charts while means and standard deviation were used to summarise continuous variables. The differences between categorical and means of continuous variables were tested using Chi-square and Independent t-test, respectively. Correlation was tested using the Spearman rank test. The level of statistical significance for bivariate analyses was set at p < 0.05.
Results
Of the 866 adults recruited for the study, 14 (1.62%) had unusual blood pressure readings documented and were excluded from statistical analysis. There were slightly more females than males in a ratio of 1.3:1. The mean (±SD) age of the study population was 42.64 (±16.07) years. About 60% of the study population were aged less than 45 years.
Majority of the study population were urban dwellers (55.8%), Urhobos (68.0%), Christians (87.9%), married (58.5%), had at the most secondary level of education (45.0%), and self-employed (66.7%). Table 1 shows the urban-rural differences in the socio-demographic and biophysical characteristics of the study population. The mean age of urban dwellers was significantly lower than their rural counterparts. The mean blood pressures, systolic and diastolic, were significantly higher among urban dwellers, as shown in Table 1.
Table 1.
Sociodemographic and biophysical profile of the study population
| Variable | Category | All N = 852 (%) |
Urban n=475 (%) |
Rural n=377 (%) |
p-value |
| Sex | Male | 376 (44.1) | 188 (39.6) | 188 (49.9) | 0.003 |
| Female | 476 (55.9) | 287 (60.4) | 189 (50.1) | ||
| Age (years) |
18–24 | 96 (11.3) | 44 (9.3) | 52 (13.8) | <0.001 |
| 25–-34 | 202 (23.7) | 130 (27.4) | 72 (19.1) | ||
| 35–44 | 210 (24.6) | 156 (32.8) | 54 (14.3) | ||
| 45–54 | 149 (17.5) | 82 (17.3) | 67 (17.8) | ||
| 55–64 | 91 (10.7) | 48 (10.1) | 43 (11.4) | ||
| ≥65 | 104 (12.2) | 15 (3.2) | 89 (23.6) | ||
| Mean (±SE) | 42.64 (0.55) | 39.08 (0.56) | 47.13 (0.98) | <0.001 | |
| Marital Status | Single | 168 (20.6) | 115 (25.2) | 53 (14.8) | <0.001 |
| Married | 477 (58.5) | 296 (64.9) | 181 (50.4) | ||
| Previously married* | 82 (10.1) | 17 (3.7) | 65 (18.1) | ||
| Co-habiting | 88 (10.8) | 28 (6.1) | 60 (16.7) | ||
| N/A | 37 | 19 | 18 | ||
| Highest Level of Education |
None | 78 (9.5) | 7 (1.5) | 71 (19.3) | <0.001 |
| Primary | 163 (19.8) | 38 (8.3) | 125 (34.1) | ||
| Secondary | 371 (45.0) | 205 (44.9) | 166 (45.2) | ||
| Tertiary | 212 (25.7) | 207 (45.3) | 5 (1.4) | ||
| N/A | 28 | 18 | 10 | ||
| Religion | Christianity | 715 (87.9) | 437 (96.3) | 278 (77.4) | <0.001 |
| Islam | 7 (0.9) | 2 (0.4) | 5 (1.4) | ||
| ATR** | 83 (10.2) | 10 (2.2) | 73 (20.3) | ||
| Others*** | 8 (0.9) | 5 (1.1) | 3 (0.8) | ||
| N/A | 39 | 21 | 18 | ||
| Ethnicity | Urhobo | 579 (68.0) | 244 (51.4) | 335 (88.9) | <0.001 |
| Itsekiri | 27 (3.2) | 24 (5.1) | 3 (0.8) | ||
| Ijaw | 38 (4.5) | 32 (6.7) | 6 (1.6) | ||
| Igbo | 100 (11.7) | 93 (19.6) | 7 (1.9) | ||
| Hausa | 12 (1.4) | 8 (1.7) | 4 (1.1) | ||
| Yoruba | 29 (3.4) | 25 (5.3) | 4 (1.1) | ||
| Others | 67 (7.9) | 49 (10.3) | 18 (4.8) | ||
| Employment status | Government employed | 86 (10.3) | 86 (18.7) | 0 (0.0) | <0.001 |
| Non-Government employed |
31 (3.7) | 29 (6.3) | 2 (0.5) | ||
| Self-employed | 556 (66.7) | 243 (52.9) | 313 (83.7) | ||
| Retired | 4 (0.5) | 4 (0.9) | 0 (0.0) | ||
| Unemployed | 65 (7.8) | 59 (12.9) | 6 (1.6) | ||
| Student | 91 (10.9) | 38 (8.3) | 53 (14.2) | ||
| N/A | 19 | 16 | 3 | ||
| BMI (kg/m2) | Underweight | 67 (7.9) | 36 (7.6) | 31 (8.2) | <0.001 |
| Normal | 517 (60.7) | 254 (53.5) | 263 (69.8) | ||
| Overweight | 175 (20.5) | 112 (23.6) | 63 (16.7 | ||
| Obese | 93 (10.9) | 73 (15.4) | 20 (5.3) | ||
| Mean (±SE) | 24.09 (0.21) | 24.92 (0.25) | 23.04 (0.36) | <0.001 | |
| Blood Pressure (mmHg) |
Mean SBP (±SE) | 125.01 (0.55) | 126.19 (0.69) | 123.53 (0.88) | 0.016 |
| Mean DBP (±SE) | 75.66 (0.43) | 78.37 (0.53) | 72.25 (0.68) | <0.001 |
widowed, divorced, separated
African Traditional Religion
N/A: Not available, BMI: Body Mass Index, DBP: Diastolic Blood Pressure, SBP: Systolic Blood Pressure, SE: Standard Error of Mean
A diagnosis of hypertension before this study was reported by 102 (12.0%) of the respondents. Of the respondents who were aware of their hypertensive status, 85 (83.3%) were urban dwellers, 59 (57.9%) were aged between 35–54years, and 53 (52.0%) were males. The association between awareness of hypertension was statistically significant for the place of residence (p<0.001) and age (p<0.001) but not for sex (p=0.187).
Of the respondents who self-reported a history of hypertension, 89 (87.3%) were currently on anti-hypertensive medications, and 42 (41.2%) had blood pressure readings less than 140/90 mmHg. Whereas treatment for hypertension did not differ by place of residence, a significantly higher proportion of males, 50 (94.3%), were on treatment (p=0.001).
Using the JNC-7 classification of blood pressure readings, the frequency distribution of blood pressure readings as normal, prehypertension and hypertension was 257 (30.2%), 387 (45.4%) and 208 (24.4%), respectively. Among the respondents with blood pressure readings in the hypertensive range, 157 (75.5%) were Stage 1, and 51 (24.5%) were Stage 2.
The overall prevalence of prehypertension and hypertension in this study, however, was 42.5% (362/852) and 29.3% (250/852), respectively. More than half of the respondents with prehypertension (55.5%) and hypertension (55.6%) were females.
The observed gender differences in blood pressure category were not statistically significant (χ2 = 0.087, df=2, p=0.958). The mean (±SD) ages of respondents with prehypertension and hypertension was 40.1 (±15.7) years and 48.5 (±14.4) years, respectively. The observed difference in mean age was statistically significant (t=−6.696; 95% CI: −10.814 to −5.909; p<0.001).
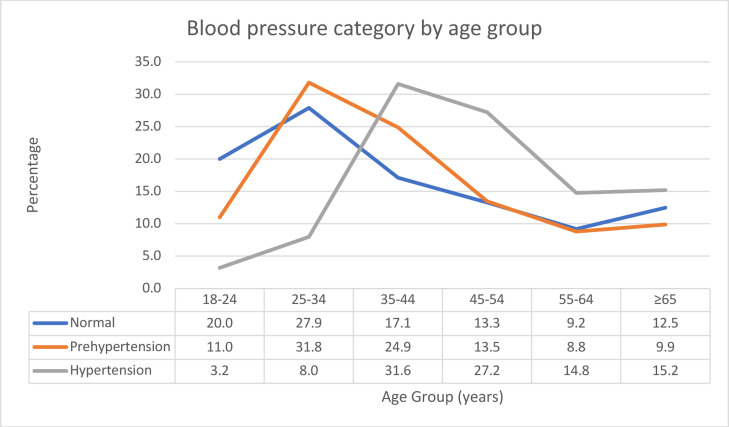
More than half (56.7%) of the respondents with prehypertension were aged between 25–44 years, while the majority (88.8%) of the respondents with hypertension were aged 35 years and above. (Figure 1) The association between age group and blood pressure category was statistically significant (χ2 = 106.999, df=10, p<0.001).
Figure 1.
Age group and blood pressure category among respondents
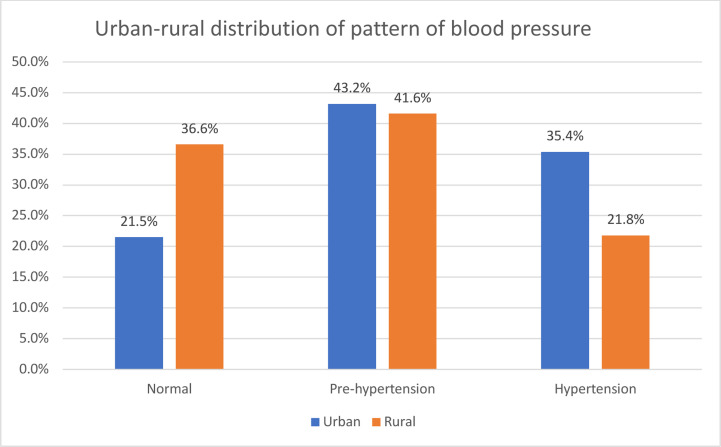
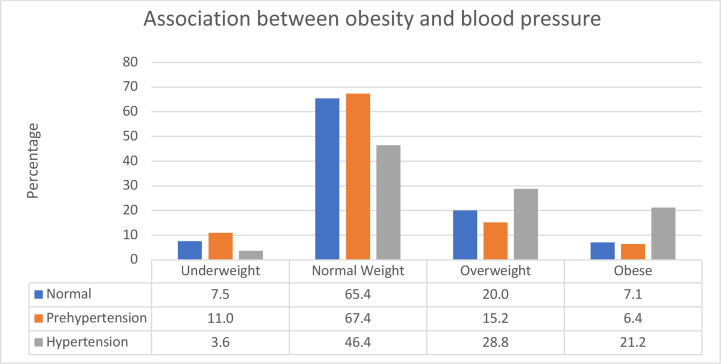
The prevalence of prehypertension and hypertension were significantly higher among urban dwellers (χ2 = 30.480, df=2, p<0.001). (Figure 2). The mean (±SD) BMI of respondents with prehypertension and hypertension was 22.97 (±4.64) kg/m2 and 25.82 (±5.15) kg/m2, respectively. The observed difference in mean BMI was statistically significant (t=−7.134; 95% CI: −3.633 to −2.064; p<0.001). About half of the respondents with hypertension were either overweight or obese.
Figure 2.
Prevalence of prehypertension and hypertension by area of residence
Among the respondents who were overweight and obese, a higher proportion had hypertension. (Figure 3) The association between body mass index and blood pressure category was statistically significant (χ2 = 70.210, df = 6, p <0.001).
Figure 3.
Association between blood pressure category and body mass index
The blood pressure category significantly correlated with age, place of residence, level of education, employment status, body mass index and fruit intake less than five portions daily. (Table 2).
Table 2.
Correlates of blood pressure categories among the study population
| Variable | Correlation Coefficient |
p-value |
| Sex | 0.008 | 0.815 |
| Age Group | 0.243 | <0.001** |
| Place of residence | −0.188 | <0.001** |
| Marital Status | 0.059 | 0.090 |
| Level of Education | 0.096 | 0.006* |
| Employment Status | −0.146 | <0.001** |
| Ever Smoked Cigarette | −0.039 | 0.259 |
| Alcohol Use | 0.014 | 0.680 |
| Fruit Intake (<5 portions per day) | −0.105 | 0.005* |
| Body Mass Index | 0.162 | <0.001** |
| Waist-to-Height Ratio | 0.034 | 0.322 |
Significant Correlation at <0.01
Significant Correlation at <0.001
Discussion
The high prevalence of hypertension and prehypertension in this study reaffirms the substantial and waxing contribution of high blood pressure as a public health challenge in Nigeria. The prevalence of hypertension in this study is comparable to previous reports from Nigeria that used the blood pressure readings of ≥140/90mmHg as the cut-off.7, 16–19
The prevalence of prehypertension reported in South-East Nigeria,16, 20 was also similar to that from this study. The awareness of high blood pressure was low in this study, as only two-fifths of the respondents with hypertension had prior knowledge. Low awareness is a bane to stemming the scourge from hypertension, especially as the condition while uncomplicated is relatively asymptomatic. The low awareness of hypertension in the index and other previous studies across Nigeria,7, 8, 16, 21–23 give credence to the poor practice of screening for hypertension among Nigerians.24, 25 Even among healthcare workers in Nigeria, the level of awareness of hypertension could be better.26
Although the majority of the respondents who were aware of their hypertensive status reported the use of antihypertensives, blood pressure control was unsatisfactory as about less than half of them had blood pressure readings <140/90mmHg. Uncontrolled hypertension predisposes humans to various end-organ damage, chief among which are stroke and heart disease. Indeed, hypertension, the “silent killer”, continues to contribute significantly to mortality and morbidity around the globe,27 Nigeria inclusive.
The prevalence of prehypertension and hypertension were found to be higher in urban than rural respondents in this study. Previous studies have also reported similar findings.7, 28–30 Urbanisation alters lifestyle patterns; is associated with reduced physical activity, intake of high-calorie diet, smoking, alcohol consumption, increased workload/stress, and poor sleep.31–33 As in this study, obesity, a modifiable risk factor for the development of hypertension, was more prevalent among urban dwellers. On the other hand, rural dwellers are less exposed to health education and promotion activities. Indeed, many targets for crucial intervention strategies to prevent noncommunicable diseases are in facilities located in urban areas. The inequity in domiciling strategic interventions may fuel rural dwellers' poor awareness and utilisation of healthcare facilities. In this study, over 80% of respondents who were aware of a prior diagnosis of hypertension were urban dwellers.
The high prevalence of prehypertension in this study is worrisome. Prehypertension is an important predictor of the development of hypertension in later life.34–37 Particularly, Blacks have an accelerated progression to hypertension from prehypertension.37 Evidence from existing literature show that prehypertension can amplify the possibility of a cardiovascular event especially in the presence of unhealthy habits such as alcohol intake, excess fat consumption and a sedentary lifestyle.34, 12 Indeed, the high prevalence of prehypertension in this study is an indication for urgent public health action across all ecological levels to stem the scourge.
Hypertension and prehypertension are both associated with age. The respondents with hypertension were significantly older than those with prehypertension in this study. Ageing has been positively associated with the development of prehypertension, and subsequently hypertension with increasing age.38 In humans, systolic blood pressure gradually increases in an upward fashion with age. In contrast, diastolic blood pressure rises, peaking at approximately 50years before declining gradually until old age.39 This may, in part, explain the findings in this study of a younger peak of prehypertension between 25–34years and an older peak of hypertension 45–54years which showed a statistically significant difference (p <0.001). Isezuo et al. also reported a similar pattern of younger peak age for prehypertension compared with hypertension.19
This finding suggests that the progression of prehypertension to hypertension is a slow but steady one indicating that prehypertension is a precursor of hypertension.34–37 The higher prevalence of prehypertension compared to hypertension in this study gives an inkling to rising prevalence of hypertension in the near future as this population ages if no action is taken especially with regards to education and lifestyle modification. Besides, increasing age and urbanisation contribute to both stressful and sedentary lifestyle that is injurious to health and promote the development of hypertension.
Although prehypertension and hypertension were more prevalent in females than males in this study, the observed differences were not statistically significant. Many studies have shown a male preponderance in the prevalence of hypertension and even prehypertension.40–44 However, observed gender differences have not translated to sex-specific management.45 Although women are likely to have a better knowledge of hypertension than men due to better healthcare utilisation than men, this does not necessarily translate into better blood pressure control.46
Conclusion
This study has shown a high prevalence of prehypertension and hypertension among Nigerian adults. Significant correlates of prehypertension and hypertension in this study were age, place of residence, level of education, employment status, body mass index and fruit intake less than five portions daily.
References
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2010;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization, author. Global Health Observatory (GHO) Data: Raised Blood Pressure. [08/03/2019]. Available from: https://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/
- 3.Volpe M, Gallo G, Tocci G. Is early and fast blood pressure control important in hypertension management? Int J Cardiol. 2018;254:328–332. doi: 10.1016/j.ijcard.2017.12.026. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz CL, McManus RJ. What is the evidence base for diagnosing hypertension and for subsequent blood pressure treatment targets in the prevention of cardiovascular disease? BMC Med. 2015;13:256. doi: 10.1186/s12916-015-0502-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turnbull F. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively designed overviews of randomised trials. Lancet. 2003;362:1527–1535. doi: 10.1016/S0140-6736(03)14739-3. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization, author. Global status report on noncommunicable diseases 2010. [08-03-2019]. Available from: https://www.who.int/nmh/publications/ncd_report_full_en.pdf.
- 7.Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens. 2015;33:230–242. doi: 10.1097/HJH.0000000000000413. [DOI] [PubMed] [Google Scholar]
- 8.Ogah OS, Okpechi I, Chukwuonye II, Akinyemi JO, Onwubere BJC, Falase AO, et al. Blood pressure, prevalence of hypertension and hypertension-related complications in Nigerian Africans: A review. World J Cardiol. 2012;4:327–340. doi: 10.4330/wjc.v4.i12.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wolz M, Cutler J, Roccella EJ, Rohde F, Thom T, Burt V. Statement from the National High Blood Pressure Education Program: Prevalence of Hypertension. Am J Hypertens. 2000;13:103–104. doi: 10.1016/s0895-7061(99)00241-1. [DOI] [PubMed] [Google Scholar]
- 10.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 11.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary. A report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71:2199–2269. doi: 10.1016/j.jacc.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Rahmanian K, Shojaie M. The prevalence of prehypertension and its association to established cardiovascular risk factors in south of Iran. BMC Res Notes. 2012;5:386. doi: 10.1186/1756-0500-5-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization, author. Noncommunicable Diseases and Mental Health Cluster. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance/Noncommunicable Diseases and Mental Health, World Health Organization. Geneva: World Health Organization; 2005. [06-05-2015]. Available from: http://www.who.int/iris/handle/10665/43376. [Google Scholar]
- 14.World Health Organization, author. Obesity: Preventing and managing the global epidemic. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. [05/11/15]. Available from: http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [PubMed] [Google Scholar]
- 15.Ashwell M, Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open. 2016;6:e010159. doi: 10.1136/bmjopen-2015-010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ezekwesili CN, Ononamadu CJ, Onyeukwu OF, Mefoh NC. Epidemiological survey of hypertension in Anambra State, Nigeria. Niger J Clin Pract. 2016;19(5):659–667. doi: 10.4103/1119-3077.188710. [DOI] [PubMed] [Google Scholar]
- 17.Ajayi IO, Sowemimo IO, Akpa OM, Ossai NE. Prevalence of hypertension and associated factors among residents of the Ibadan-North Local Government Area of Nigeria. Nig J Cardiol. 2016;13:67–75. doi: 10.4103/0189-7969.165168. [DOI] [Google Scholar]
- 18.Okpechi IG, Chukwuonye II, Tiffin N, Madukwe OO, Onyeonoro UU, Umeizudike TI, et al. Blood pressure gradients and cardiovascular risk factors in urban and rural populations in Abia State South Eastern Nigeria using the WHO STEPwise approach. PLoS One. 2013;8(9):e73403. doi: 10.1371/journal.pone.0073403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Isezuo SA, Sabir AA, Ohwovorilole AE, Fasanmade OA. Prevalence, associated factors and relationship between prehypertension and hypertension: a study of two ethnic African populations in Northern Nigeria. J Hum Hypertens. 2011;25(4):224–230. doi: 10.1038/jhh.2010.56. [DOI] [PubMed] [Google Scholar]
- 20.Okwuonu CG, Ngoka SC, Chimezie OJ, Eze TH, Uwanurochi K, Mbanaso AU. Towards prevention of hypertension in Nigeria: A study of prehypertension and its associations among apparently healthy adults in Umuahia, South-East Nigeria. Int J Prev Med. 2015;6:61. doi: 10.4103/2008-7802.160968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okwuonu CG, Ojimadu NE, Chimezie OJ, Madudonu U, Ogbolafor N, Ogah O. Awareness of blood pressure status, undiagnosed hypertension and proteinuria among adults in Umuahia, South-East Nigeria. Sahel Med J. 2016;19:82–88. doi: 10.4103/1118-8561.186035. [DOI] [Google Scholar]
- 22.Ulasi II, Ijoma CK, Onwubere BJC, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in Enugu, Nigeria. Int J Hypertens. 2011;2011:869675. doi: 10.4061/2011/869675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akpan EE, Ekrikpo UE, Udo AIA, Bassey BE. Prevalence of hypertension in Akwa Ibom State, South-South Nigeria: rural versus urban communities study. Int J Hypertens. 2015;2015:975819. doi: 10.1155/2015/975819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Asuke S, Babatunde JM, Ibrahim MS. A comparative analysis of the awareness and practice of periodic health examination among workers of public and private establishments in Zaria, Northwestern Nigeria. Arch Med Surg. 2017;2:38–42. doi: 10.4103/archms.archms_50_17. [DOI] [Google Scholar]
- 25.Usman SO, Edet-Utan O, Suleiman A, Isola IN, Ojogbede A, Akintayo-Usman NO, Fatunmbi OJ, Adu AS. Periodic medical check-up among residents of three Nigeria Southwestern States. Journal of Contemporary Medicine. 2016;6(3):174–182. doi: 10.16899/ctd.65941. [DOI] [Google Scholar]
- 26.Owolabi AO, Owolabi MO, OlaOlorun AD, Amole IO. Hypertension prevalence and awareness among a health workforce in Nigeria. Internet Journal of Medical Update. 2015;10(2):10–19. doi: 10.4314/ijmu.v10i2.3. [DOI] [Google Scholar]
- 27.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood pressure related disease 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 28.Sabir AA, Isezuo SA, Ohwovoriole OA, Fasamade SA, Iwuala AJ, Umar MT. Rural-Urban difference in plasma lipid levels and prevalence of dyslipidaemia in Hausa-Fulani of North-Western Nigeria. Eth Dis. 2013;23:374–378. [PubMed] [Google Scholar]
- 29.Adediran O, Akintunde AA, Edo AE, Opadijo OG, Araoye AM. Impact of urbanisation and gender on frequency of metabolic syndrome among native Abuja settlers in Nigeria. J Cardiovasc Dis Res. 2012;3:191–196. doi: 10.4103/0975-3583.98890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murthy GV, Fox S, Sivasubramaniam S, Gilbert CE, Mahdi AM, Imam AU, et al. Prevalence and risk factors for hypertension and association with ethnicity in Nigeria: results from a national survey. Cardiovasc J Afr. 2013;24:1–7. doi: 10.5830/CVJA-2013-058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.BeLue R, Okoror TA, Iwelunmor J, Taylor KD, Degboe AN, Agyemang C, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Global Health. 2009;5:10. doi: 10.1186/1744-8603-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carrera-Bastos P, Fontes-Villalba M, O'kefee JH, Lindberg S, Cordian L. The western diet and lifestyle and diseases of civilisation. Research Reports in Clinical Cardiology. 2011;2:15–35. doi: 10.2147/RRCC.S16919. [DOI] [Google Scholar]
- 33.Amuna P, Zotor FB. Epidemiological and nutritional transition in developing countries: Impact on human health and development. Proc Nutr Soc. 2008;67:82–90. doi: 10.1017/S0029665108006058. [DOI] [PubMed] [Google Scholar]
- 34.Zheng L, Sun Z, Zhang X, Xu C, Li J, Hu D, et al. Predictors of progression from prehypertension to hypertension among rural Chinese adults: results from Liaoning Province. Eur J Cardiovasc Prev Rehabil. 2010;17(2):217–222. doi: 10.1097/HJR.0b013e328334f417. [DOI] [PubMed] [Google Scholar]
- 35.Ishikawa Y, Ishikawa J, Ishikawa S, Kario K, Kajii E. Progression from prehypertension to hypertension and risk of cardiovascular disease. J Epidemiol. 2017;27(1):8–13. doi: 10.1016/j.je.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferguson TS, Younger N, Tulloch-Reid MK, Lawrence-Wright MB, Forrester TE, Cooper RS, et al. progression from prehypertension to hypertension in a Jamaican cohort: incident hypertension and its predictors. West Indian Med J. 2010;59(5):486–493. [PMC free article] [PubMed] [Google Scholar]
- 37.Selassie A, Wagner CS, Laken ML, Ferguson ML, Ferdinand KC, Egan BM. Progression is accelerated from prehypertension to hypertension in Blacks. Hypertension. 2011;58:579–587. doi: 10.1161/HYPERTENSIONAHA.111.177410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim Y, Lee S. Prevalence and Risk Factors Associated with Prehypertension by Gender and Age in a Korean population in the KNHANES 2010-2012. Iran J Public Health. 2015;44(12):1594–1602. [PMC free article] [PubMed] [Google Scholar]
- 39.Williams B, Lindholm LH, Serer P. Systolic pressure is all that matters. Lancet. 2008;371:2219–2221. doi: 10.1016/S0140-6736(08)60804-1. [DOI] [PubMed] [Google Scholar]
- 40.Wang R, Lu X, Hu Y, You T. Prevalence of prehypertension and associated risk factors among health check-up population in Guangzhou, China. Int J Clin Exp Med. 2015;6(9):16424–16433. [PMC free article] [PubMed] [Google Scholar]
- 41.Yadav S, Boddula R, Genitta G, Bhatia V, Kongara S, Julka S, et al. Prevalence and risk factors of prehypertension and hypertension in an affluent north Indian population. Indian J Med Res. 2008;128:712–720. [PubMed] [Google Scholar]
- 42.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai- The Chennai Urban Rural Epidemiology Study (CURES-S2) J Assoc Physicians India. 2007;55:326–332. [PubMed] [Google Scholar]
- 43.Parthage PM, Unnikrishnan B, Thankappan KR, Thapar R, Fatt QK, Oldenburg B. Prevalence and correlates of prehypertension among adults in urban South India. Asia Pac J Public Health. 2015;28(1 Suppl):935–1015. doi: 10.1177/1010539515616453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Do HT, Geleijnse JM, Le MB, Kok FJ, Feskens EJ. National prevalence and associated risk factors of hypertension and prehypertension among Vietnamese adults. Am J Hypertens. 2015;28(1):89–97. doi: 10.1093/ajh/hpu092. [DOI] [PubMed] [Google Scholar]
- 45.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the panel members appointed to the eighth Joint National Committee (JNC-8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 46.Rahman M, Williams G, Al Mamun A. Gender differences in hypertension awareness, antihypertensive use and blood pressure control in Bangladeshi adults: findings from a national cross-sectional survey. J Health Popul Nutr. 2017;36(1):23. doi: 10.1186/s41043-017-0101-5. [DOI] [PMC free article] [PubMed] [Google Scholar]