Abstract
Objective:
Rising clinical demand and changes to Radiologists’ job plans mean it is becoming ever more difficult for Radiologists to teach medical students.
The aim of this study was to assess the current role of Radiologists in undergraduate medical education in Scotland.
Methods:
Consultant Radiologists working across all 14 Scottish Health Boards were invited by email to participate in an anonymous short online survey. The survey ran for 6 weeks from November 2019. One reminder email was sent a week before the survey closed.
Results:
102 responses were recorded, representing 34% of the total whole time equivalent Radiologists in Scotland. All agreed Radiology should be taught to medical students. Over 70% (n = 73) taught medical students, most often during supporting professional activity time. 76 percent of Radiologists who did not teach expressed a desire to do so. The most common barrier to teaching was not having enough time in their job plan. Scottish Radiologists delivered a median of 10 h (IQR 0–22) a year of teaching to medical students. Thematic analysis of free comments revealed staffing/time constraints severely limiting ability to teach.
Conclusion:
This is the first national survey to assess the current role of Radiologists in teaching medical students. While most are teaching or want to teach, there is a large drop-off between current Scottish and previously reported UK median teaching hours. Engagement from Universities, Royal College of Radiologists and Health Boards is urgently needed to reverse this trend.
Advances in knowledge:
This is the first national survey into the current role of Radiologists in undergraduate medical education. There is a large drop-off between current Scottish and previously reported UK median teaching hours.
Introduction
Radiology has been espoused as an excellent tool for teaching medical students since 1925.1 Modern clinical medicine is increasingly reliant on Radiology. It is important we teach our students the role it plays in the diagnostic process. Many of the General Medical Council (GMC) Outcome for Graduates are applicable to Radiology, not least the ability to interpret X-rays and the results of the diagnostic procedures as explicitly stated.2 The Royal College of Radiologists have responded by publishing the Undergraduate Radiology Curriculum, mapped to the Outcomes, to aid the Radiologist teacher.3
Rising clinical demand and changes to Radiologists’ job plans mean it is becoming ever more difficult for Radiologists to teach medical students. Also in a busy undergraduate medical curriculum, it can be difficult to find space for Radiology. Finally, there is an increasing trend for clinicians and medical educators to teach image interpretation without Radiology input.4–7 The aim of this study was to assess the current role of Radiologists in undergraduate Medical Education in Scotland.
Methods
An online survey was developed to determine how much teaching was delivered by Scottish Radiologists to medical students. Multiple choice and open-ended questions made up the survey, which was designed to take less than 5 min to complete (Supplementary Material 1). Institutional Board Review was sought but was waived, as this work was deemed an evaluation of service provision.
The survey was launched at the Annual General Meeting of the Scottish Radiological Society. 154 Radiologists attended this meeting, representing both teaching and non-teaching hospitals. Radiology clinical leads from each of the 14 Scottish health boards were contacted by email to invite their team of consultant radiologists to participate in the anonymous survey in November 2019. The survey was open for 6 weeks and 1 follow-up email was sent a week before the survey was closed. Respondents were incentivised by being given the option to participate in a raffle for a small monetary token.
Quantitative data were presented as median and interquartile ranges where appropriate. Qualitative analysis was performed on the free text responses, using a widely accepted six step process as described by Braun and Clarke.8 Briefly, this involved (both authors separately and together) familiarising themselves with data, generating initial codes, searching for themes, reviewing themes, defining and naming themes and producing a report.8,9
Results
Quantitative analysis
102 responses were recorded, representing 34% of the total whole time equivalent (WTE) Radiologists working in Scotland.10 There were 68 (66.7%) male and 32 (31.4%) female respondents. A third (n = 34) of respondents were in the 36–45 years age range, while a further 29 (28.3%) were between 46 and 55 years (Table 1). Over 70% (n = 73) of respondents taught medical students.
Table 1.
Respondents’ age (N = 102)
| Age range | N (%) |
|---|---|
| 26–35 | 19 (18.6) |
| 36–45 | 34 (33.3) |
| 46–55 | 29 (28.3) |
| 56–65 | 18 (17.6) |
| 66–76 | 0 |
| Prefer not to say | 2 (2.1) |
Not having time in their job plan and not being asked were the most frequent barriers to teaching for the 29 respondents who did not teach (Table 2). However, when asked, 22 (76%) of the 29 who did not currently teach expressed a desire to do so.
Table 2.
Reasons for not teaching* (N = 29)
| Reasons for not teaching | N (%) |
|---|---|
| No time in job plan | 19 (65.5) |
| Not been asked | 18 (62.0) |
| Less than 2.5 SPA | 11 (38.0) |
| Prefer not to say | 3 (10.03) |
| Not a teaching hospital | 2 (6.9) |
SPA, Supporting Professional Activities.
Multiple answers possible per respondent.
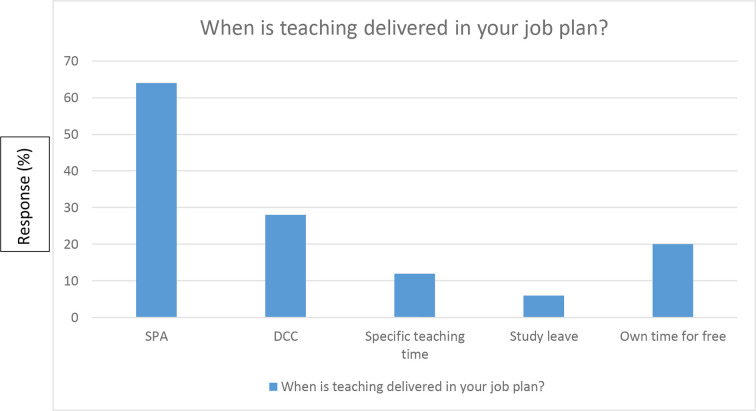
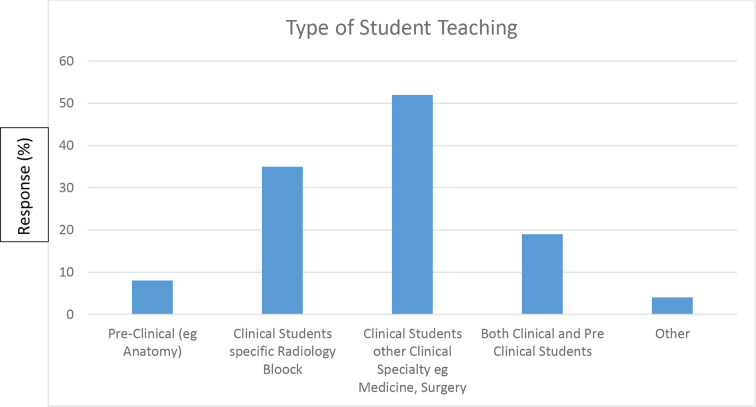
Of those who taught, the most common scenario was opportunistic ad hoc in nature, during Supporting Professional Activities (SPA) time (Figure 1). Most teaching was clinically based, usually as part of another clinical attachment (Figure 2). Most Radiologists who taught did not have formal University ties (75%). Only 2 (11%) respondents with University affiliation had the ability to influence the curriculum.
Figure 1.
When is teaching delivered in your job plan*? (* Multiple answers possible per respondent. DCC, direct clinical care; SPA, supporting professional activities.)
Figure 2.
Type of student teaching: (* Multiple answers possible per respondent.)
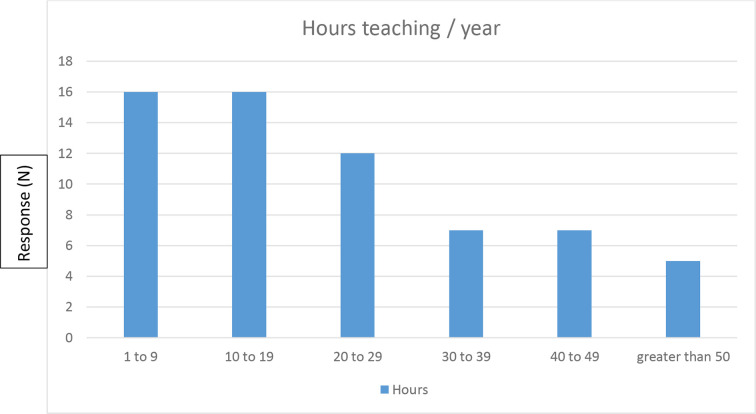
Scottish Radiologists delivered a median of 10 h (IQR 0–22) a year of teaching to medical students. Of those who taught, most (63.6%) delivered between 1 and 29 h a year of Radiology teaching (median 17.5 h, IQR 8.5–33.75), with a minority (n = 5) delivering 50–280 h a year (Figure 3).
Figure 3.
How many hours a year teaching medical students? (>50 h breakdown 50, 60, 120, 168, 280 h.)
100% of respondents agreed Radiology should be taught to medical students. When asked who should teach Radiology, all respondents agree Radiology should be taught by Radiologists while 30% think other clinicians also have a role in teaching Radiology. Only eight (7.8%) agreed that medical educators should teach Radiology.
Qualitative analysis
Thematic analysis of the respondents’ free text comments (n = 40) was performed using an inductive and semantic approach (Table 3). The strongest theme (n = 20) which emerged was overwhelmingly one of Radiologists citing excessive clinical work and time/staffing constraints severely limiting their ability to teach. Several people (n = 4) described dropping teaching to ensure clinical demands are met. The next most common theme (with half as many comments) was an appeal for a syllabus from which Radiologists could refer to inform their teaching. Despite the curriculum published by the Royal College of Radiologists, there was a feeling that more should be done by the College to strengthen the voice of Radiology in the Undergraduate arena and help prioritise what should be taught. Also an increase in training numbers to improve recruitment and address staffing shortage was suggested. Some Radiologists (n = 5) think teaching medical students how to use/ what radiology test to request and what results mean is as, if not more, important than how to interpret the tests (e.g. CT or CXR) themselves.
Table 3.
Thematic analysis (40 respondents)
| Theme | Number of comments |
|---|---|
| Time constraints | 20 |
| Lack of syllabus | 8 |
| Best use of Radiology | 5 |
| University/Student related logistics issues | 5 |
| Clinical-Radiology combined teaching | 4 |
Another theme that emerged was a willingness to teach if the time and resources (n = 5) were available. An opinion that radiology teaching should ideally dove-tail and be within the context of clinical teaching (n = 4) was also expressed.
Discussion
The GMC mandates the Doctor as a Professional has to reflect, learn and teach others.2
This is the first national survey to directly sample Radiologists to determine Medical Student Teaching activity in Scotland. Previous similar studies polled Universities.11 The survey demonstrates a good proportion of Radiologists are involved in teaching medical students—despite increasing clinical demands and lack of resource. Even those who do not currently teach would like to teach.
While there are a few exceptional outliers, the median total hours of teaching was 10 h, with the majority of those who teach delivering 1–29 h a year. This falls far short of the reported UK median range of 44–112 h and European median total of 76 h (range 19–212 h) in the 2011 European Survey.12 The majority of European Universities (Denmark and UK excepted) report Radiology as part of the formal curriculum with half reporting Radiology as an independent discipline with its own examination.12
Previous studies have suggested the presence of “Chairs of Radiology” as being associated with higher hours of student teaching.13 While five exceptional respondents cite high annual teaching hours (50, 60, 120, 168 and 280), the anonymous nature of the survey meant it was impossible to link them back to the Professors who participated. In fact, many of the Radiologists who teach do so without formal association with Universities and some even do so out of their own free time or take study leave to teach. This is particularly remarkable given the acknowledged exponential increase in clinical Radiology demand and loss of SPA time.
Similarities are noted between our results and to those from a study performed in 2015 by Darragh et al evaluating the attitudes of consultants, across all medical specialities, to teaching medical students.14 They reported active medical student teaching by consultants. They also reported consultant perception of inadequate financial reward and cited time constraints as a barrier to teaching. To counteract this, they suggested a desire to have teaching included in job plans.14 While there are recommendations regarding specific post holders (e.g. module/block leads or teaching leads employed by NHS Boards) by the NHS Education for Scotland (NES) of a minimum of 0.25 SPA to allow for accreditation under Recognition of Trainer within a consultant’s job plan, no such recommendation exists regarding less formal teaching activity.15 Indeed, many consultant jobs are being advertised with 9:1 (Direct Clinical Care: SPA) job plan split since 2010. This could account for the apparent large fall between the current level of Radiology teaching in Scotland and that reported in the UK some 9 years ago.12 If this trend were to continue, continued education of medical students by Consultant Clinicians across specialities could be seriously jeopardised.
The thematic analysis further paints a picture of a willing body of professionals who want to teach the next generation of doctors despite the overwhelming time and staffing constraints. Radiology is a shortage specialty and respondents call for more to be done by the College to strengthen the Undergraduate voice, to improve recruitment for the future. The comments also suggest a syllabus for teaching would be welcomed. Many radiologists feel radiology should be taught in conjunction with clinical specialities, not as an isolated speciality.
A potential limitation of this study was inviting consultants only (not registrars) to participate in the survey. While many registrars are involved in teaching medical students, these are almost never performed without consultant input—either directly or indirectly. In this way, we do not feel that the teaching being delivered by Radiology is underestimated. Sampling bias was mitigated against by including every radiologist in all Scottish Health Boards in the survey—including many district general hospitals not “traditionally” considered as major contributors to medical student teaching. The response rate of 34% is low, yet all the factors known to improve response rates were utilised.16 These included a short survey, monetary incentive (raffle), personal connection between researcher and potential respondents and multiple attempts to obtain response. Also, we know there is a poor correlation between response rates and bias.17 102 respondents is a good sample size in a small field of medical professionals.
Conclusion
This national survey of Radiologists demonstrates most are involved in or want to teach medical students. The hours spent teaching fall far short of previously reported UK and European levels. This is likely a reflection of the increasing clinical demands placed on the modern Radiologist. Engagement is urgently needed from Universities, Health Boards and College to find a solution for this. Otherwise, these willing teachers may be lost for good.
Footnotes
Acknowledgements: We would like to thank Prof John Murchison, President of Scottish Radiology Society for supporting this survey and allowing its launch at the Annual SRS Meeting. We would also like to thank all the Radiology Clinical Leads and Scottish Radiologists who gave of their time to participate in this survey.
REFERENCES
- 1.Dempster JH. The teaching of radiology to undergraduates. Radiology 1925; 4: 325–6. doi: 10.1148/4.4.325 [DOI] [Google Scholar]
- 2.General Medical Council Outcome for graduates.. Accessed 29 March 2020.
- 3.Undergraduate Radiology Curriculum . . Royal College of Radiologist.(2nd Ed) Available from: https://www.rcr.ac.uk/sites/default/files/documents/undergraduate_radiology_curriculum_second_edition_2017.pdf [Accessed 20 March 2020].
- 4.Patten D. Using ultrasound to teach anatomy in the undergraduate medical curriculum: an evaluation of the experiences of tutors and medical students. Ultrasound 2015; 23: 18–28. doi: 10.1177/1742271X14542173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Findlater GS, Kristmundsdottir F, Parson SH, Gillingwater TH. Development of a supported self-directed learning approach for anatomy education. Anat Sci Educ 2012; 5: 114–21. doi: 10.1002/ase.1255 [DOI] [PubMed] [Google Scholar]
- 6.Kotzé SH, Driescher ND, Mole CG. The translucent cadaver: a follow-up study to gauge the efficacy of implementing changes suggested by students. Anat Sci Educ 2013; 6: 433–9. doi: 10.1002/ase.1365 [DOI] [PubMed] [Google Scholar]
- 7.Chew C, Cannon P, O’Dwyer PJ. Radiology for medical students (1925–2018): an overview.. [DOI] [PMC free article] [PubMed]
- 8.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 9.Kiger ME, Varpio L. Themetic analysis of qualitative data: AMEE guide. Medical Teacher 131No.. [DOI] [PubMed] [Google Scholar]
- 10.Royal College of Radiologists Clinical Radiology : Scotland workforce 2018 Summary Report.. Available from: https://www.rcr.ac.uk/sites/default/files/clinical_radiology_scotland_workforce_census_summary_report_2018.pdf [Accessed 29 March 2020].
- 11.Sadler TJ, Zhang T, Taylor HL, Brassett C. The role of radiology in anatomy teaching in UK medical schools: a national survey. Clin Radiol 2018; 73: 185–90. doi: 10.1016/j.crad.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 12.Kourdioukova EV, Valcke M, Derese A, Verstraete KL. Analysis of radiology education in undergraduate medical doctors training in Europe. Eur J Radiol 2011; 78: 309–18. doi: 10.1016/j.ejrad.2010.08.026 [DOI] [PubMed] [Google Scholar]
- 13.Subramaniam RM, Kim C, Scally P. Medical student radiology teaching in Australia and New Zealand. Australas Radiol 2007; 51: 358–61. doi: 10.1111/j.1440-1673.2007.01750.x [DOI] [PubMed] [Google Scholar]
- 14.Darragh L, Baker R, Kirk S. Teaching medical students, what do consultants think? Ulster Med J 2015; 84: 37–41. [PMC free article] [PubMed] [Google Scholar]
- 15.Scottish Trainer Framework.. Available from: https://www.nes.scot.nhs.uk/media/20681/NES%20Draft%20Scottish%20TrainerDevelopment%20Framework_dec2013.pdf [Accessed 6 April 2020].
- 16.Phillips AW, Reddy S, Durning SJ. Improving response rates and evaluating nonresponse bias in surveys: AMEE guide No. 102. Medical Teacher 2015;: 1–12. [DOI] [PubMed] [Google Scholar]
- 17.Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q 2006; 70: 646–75. doi: 10.1093/poq/nfl033 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.