Abstract
Study Objectives:
Although weekend catch-up sleep is common among children, the association between weekend catch-up sleep and executive functions remains unclear. We aimed to determine whether weekend catch-up sleep was related to executive functions in school-aged children.
Methods:
We analyzed data for 4,699 children (9.00 years ± 1.73 years old, 52.9% boys) from 5 primary schools in Guangzhou, China. Executive functions performance was examined by the Behavior Rating Inventory of Executive Function Parent Form. Validated self-report questionnaires were used to assess sleep status, socioeconomic status, and health behaviors. Multiple linear regression analyses were used to assess the association of weekend catch-up sleep duration with executive functions.
Results:
Weekday sleep was negatively associated with scores on three composite indices (Behavioral Regulation Index, Metacognition Index, Global Executive Composite), while weekend catch-up sleep was positively associated with them. Children with < 9 hours weekday sleep duration had higher scores in all indices, and there was no correlation between weekend catch-up sleep and scores of all indices (P > .05). For children who slept ≥ 9 hours on weekdays, weekend catch-up sleep of more than 1 hour was associated with increased scores of Behavioral Regulation Index, Metacognition Index, and Global Executive Composite (P < .05). There was no interaction between sex, age, and weekend catch-up sleep and executive functions (P > .05).
Conclusions:
Weekend catch-up sleep could not restore the executive functions deficits related to short weekday sleep. Weekend catch-up sleep over 1 hour may have adverse effects on executive functions in school-aged children.
Clinical Trial Registration:
Registry: ClinicalTrials.gov; Title: Prospective Cohort Study on Cognition and Cardiovascular Disease of Sedentary Behaviors in Children; URL: https://clinicaltrials.gov/ct2/show/NCT03582709; Identifier: NCT03582709
Citation:
Lv Y, Cai L, Zeng X, et al. Association between weekend catch-up sleep and executive functions in Chinese school-aged children. J Clin Sleep Med. 2020;16(8);1285–1293.
Keywords: executive functions, sleep duration, brief, children
BRIEF SUMMARY
Current Knowledge/Study Rationale: It is a common phenomenon that school-aged children increase sleep duration on the weekend to recover from sleep loss incurred during the weekdays. Although it has long been established that short sleep duration impairs executive functions, the association between weekend catch-up sleep and executive functions in school-aged children remains unclear.
Study Impact: This study indicates that weekend catch-up sleep could not restore the executive functions deficits related to short weekday sleep. An irregular sleep pattern, ie, weekend catch-up sleep over 1 hour, may have adverse effects on executive functions in school-aged children.
INTRODUCTION
Sleep plays a crucial role in a healthy child’s development.1 Despite the fact that the United States National Sleep Foundation recommends a sleep duration of 9–11 hours per night for school-aged children (6–13 years old),2 a considerable proportion of children worldwide do not meet these recommendations.3 A cross-sectional study from 12 countries showed that the mean overall adherence to sleep time recommendations was 42% in children.4 A 2019 online survey reported that only 40.2% of Chinese students aged 6–12 slept more than 9 hours per night.5 As sleep duration decreases worldwide, sleep loss and its consequences have drawn more attention in both public and academic domains.
Executive functions (EFs) as high-order cognitive functions are central control systems for complex behavior and include three core domains: inhibition, working memory, and cognitive flexibility.6 Neuroimaging evidence suggests that lack of sleep affects cognitive function by triggering a complex set of two-way changes in brain activity and connectivity,7 and sleep deprivation can particularly degrade complex EFs that rely on prefrontal regions of the brain.8 Nevertheless, inconsistent findings on the effects of sleep deprivation on high-level EFs pervade the literature, with many studies reporting deficits on EF tasks as a result of sleep deprivation,9 and others failing to find such effects.10,11 Most neuropsychological tests alone (laboratory or clinical performance tests) attempt to separate integrated functions into component parts, but this may not be sufficient to capture more complex everyday executive problem-solving. Thus, there is a need for a method that corresponds to the actual situation on a daily basis of measuring EFs, such as the Behavior Rating Inventory of Executive Function (BRIEF, Psychological Assessment Resources, Florida, America), which assess the broader and more comprehensive aspects of daily problem-solving demands. On the other hand, most of the previous findings were based on laboratory-induced sleep deprivation. More work is necessary to determine the relationship between EFs and sleep loss under natural conditions.
Weekend catch-up sleep is a common way school-age children recover from sleep loss incurred on weekdays,12 as their weekday sleep duration is often compromised because of school schedules and academic, social, and recreational activities.13 The average reported weekend catch-up sleep in school-aged children could be up to 3 hours, with 1.17 hours in the US,14 1.5 hours in China,15 and 3 hours in Korea.16 There was a hypothesis proposed that the brain exhibits compensatory neural activity that can enable partial recovery of the performance of certain behaviors after sleep deprivation.17 However, the few studies that have evaluated the effect of weekend catch-up sleep on children’s EFs have produced inconsistent results. An observational study indicated that catch-up sleep has minor associations with intelligence and executive functioning in early adolescence,18 while a study conducted on adolescents aged 12–18 in Hong Kong showed that weekend catch-up sleep duration of more than 2 hours was associated with lower academic performance.19
EFs play a critical role in daily behavior and educational, vocational, and social achievements for children and adults.20 Studying the relationship between sleep duration and EFs in children may be even more relevant, because children are at a critical stage of brain development and detrimental effects can last well into adulthood.21,22 Most of the epidemiologic studies about EFs have only assessed the effects of short sleep duration measured by averaging sleep duration over 7 days,23 sleep duration on school days only,24 or any given day.25 These study designs ignored the variation in sleep duration during the week. Weekend catch-up sleep represents an irregular sleep pattern. Whether weekend catch-up sleep compensates for the accumulated sleep debt and modulates the effect of insufficient weekday sleep on neurocognitive function need to be confirmed.
We conducted a cross-sectional study of 4,699 school-aged children to examine the association of weekday sleep and weekend catch-up sleep with EFs. We hypothesized that (1) children with less weekday sleep would be more problematic in their EFs; and (2) children with more weekend catch-up sleep would show higher EFs. In light of the acknowledged weekday sleep loss and weekend catch-up sleep epidemic that now pervades school-aged children, this study was intended to provide evidence on which to base sleep recommendations for both public and professional health policies.
METHODS
Study design and participants
We carried out a cross-sectional analysis using the baseline data from a school-based setting cohort study.26 We used clustered stratified random sampling to select 5 ordinary primary schools in Guangzhou, China. The baseline data were collected from January 2017 to December 2018 from children in grades 1–6 (aged 6–12 years). A multicomponents questionnaire for children’s sleep status and EFs performance was distributed to children at school, and children and their parents filled it out together at home. Questionnaire collection and quality control were then carried out in the school. The eligibility criteria for each participant was as follows: (1) 6–12 year old; (2) normal visual acuity; (3) right-handed. Students were excluded if they: (1) had a severe physical disease which may have adversely affected daily physical activity; (2) had a mental disease or medical condition leading to unavailability for the questionnaire; (3) had a severe medical condition that made them absent from school; and (4) were suspected of having developmental behavioral disorders according to the Strengths and Difficulties Questionnaire (SDQ) or (5) had any history of medication that could potentially influence sleep. Of the 5,305 participants who gave informed consent, 606 were excluded due to missing data or outlier status in sleep duration (n = 185), Behavior Rating Inventory of Executive Function Parent Form (BRIEF-P; n = 164), or covariates (n = 257). The remaining 4,699 children (88.6%, 2,488 boys and 2,211 girls) were included in the final analysis. Procedures described in this article were approved by the Ethical Review Committee for Biomedical Research, School of Public Health, Sun Yat-sen University (L2016-010). All parents or guardians of participants signed an informed consent form voluntarily before taking part in the study.
Exposures: sleep duration
The major independent variables for our study were weekday and weekend sleep durations. Children reported their bedtimes, waketimes, sleep latency, and nap durations over the previous week. These responses were recorded separately for weekdays and weekends. Sleep duration was calculated as follows: sleep duration (hours) = (waketimes – bedtimes) – sleep latency; weekly sleep duration (hours) = [5 × (weekday sleep duration) + 2 × (weekend sleep duration)] / 7. Weekend catch-up sleep was calculated as weekend sleep duration minus weekday sleep duration. We examined sleep duration as a continuous measure, but for stratified analysis, weekend catch-up sleep duration was categorized into four groups: no catch-up (≤ 0 hours, reference group), 0–1 hour, 1–2 hours, and > 2 hours; weekday sleep duration was categorized into three groups: < 9 hours, 9–11 hours, and > 11 hours, based on the recommendations of the United States National Sleep Foundation.2
Outcome: executive functions
BRIEF-P was selected to assess EFs; it is an assessment of executive function behaviors during the past 6 months in the home environment for children aged 5–18 years, and the Chinese version had been revised with good reliability and validity.27 It consisted of 86 items, and every item had a choice of 1 of 3 dimensions: “No” (scored 1), “Sometimes” (scored 2), and “Often” (scored 3). The Behavioral Regulation Index (BRI) represents a child’s ability to shift cognitive set and modulate emotions and behavior via appropriate inhibitory control. It comprises Inhibit, Shift, and Emotional Control scales. The Metacognition Index (MI) is interpreted as the ability to cognitively self-manage tasks, and it reflects a child’s ability to self-monitor performance. It comprises scales for Initiate, Working Memory, Plan/Organize, Organization of Materials, and Monitor. Additionally, Global Executive Composite (GEC) summary score is composed of BRI and MI. For all BRIEF-P scales, a higher T-score (adjusted for age and sex) indicates more problems with executive function–related tasks. Even a 1-point difference can affect the percentile of a child’s executive function in the group.28
Covariates
Sociodemographic and behavioral characteristics, including age, sex, paternal and maternal educational level, family income, moderate-to-vigorous physical activity, sedentary behavior (including doing homework/reading, watching television, playing computer games/surfing the Internet, and sitting during transportation), and other sleep-related variables (sleep timing and nap duration), were derived from the physical health surveillance system questionnaire for primary school students in Guangzhou29. Height and weight were measured by standard anthropometric measurements. Body mass index (kg/m2) was calculated as weight divided by height squared (kg/m2). The quantification of the sleep timing (chronotype) was based on the midpoint of sleep on free days (MSF), corrected for sleep extension on free days (MSFsc).30 MSFsc was calculated as follows: MSFsc = midpoint of sleep on weekends – .5 × (sleep duration on weekends – [5 × sleep duration on weekdays + 2 × sleep duration on weekends]/7).
Statistical analysis
Analyses were performed with statistical software SPSS version 21.0 (IBM, Armonk, NY) Continuous variables were presented as mean ± standard deviation. Categorical variables were presented as percentages. Differences between groups were determined by analysis of variance or chi-square test.
We performed multiple linear regressions with unstandardized regression coefficients and 95% confidence intervals (95% CI) to examine the associations of weekday sleep and weekend catch-up sleep duration (entered into the same model; hours/night) with EFs score. Then, we investigated the distribution of EFs scores stratified by weekday sleep duration and catch-up sleep duration. Further, we set dummy variables into the multiple linear regression model to investigate the relationship between weekend catch-up sleep and EFs at different weekday sleep duration levels. Finally, the interaction between sex, age, and weekend catch-up sleep duration in relation to EFs were tested by adding interaction terms, respectively.
The models were adjusted for sociodemographic and behavioral characteristics including age, sex, paternal and maternal educational level, family income, MSFsc, nap duration, body mass index, moderate-to-vigorous physical activity, and sedentary behavior. The unstandardized regression coefficients reflect the T-score change per 1-unit change in standard deviation of catch-up sleep. A 2-tailed 5% level of significance was used for all statistical tests.
RESULTS
Sample characteristics
There were no significant differences in sociodemographic or behavioral characteristics, average sleep duration of weekdays and weekends, or scores of EFs between the final study population and those excluded from the present analysis (data not shown). As shown in Table 1, sleep data were available in 4,699 participants with 52.9% boys, mean age 9.00 years ± 1.73 years. The participants had an average weekly sleep duration of 9.12 hours ± .70 hours (8.92 hours ± .74 hours on weekday and 9.61 hours ± 1.02 hours on weekends). The average weekend catch-up sleep duration was .69 hours ± .97 hours. Weekend catch-up sleep was reported by 73.4% of participants, including 0–1 hour (44.6%), 1–2 hours (21.0%), and > 2 hours (7.8%). Weekend catch-up sleep duration was associated with age, sex, weekday sleep duration, MSFsc, nap duration, and sedentary behavior (P < .01). There were no significant differences for paternal and maternal educational levels, family income, body mass index, and moderate-to-vigorous physical activity across the weekend catch-up sleep duration categories (P > .05).
Table 1.
Characteristics of the study population stratified by weekend catch-up sleep duration.
| No catch-up (n = 1,248) | 0–1 hour (n = 2,097) | 1–2 hours (n = 986) | > 2 hours (n = 368) | Total (n = 4,699) | P | |
|---|---|---|---|---|---|---|
| Age (year) | 8.93 ± 1.78 | 8.89 ± 1.74 | 9.16 ± 1.70 | 9.50 ± 1.52 | 9.00 ± 1.73 | <.01 |
| Sex (male, %) | 57.1 | 53.7 | 49.9 | 42.7 | 52.9 | <.01 |
| Paternal educational level (%) | .267 | |||||
| High school or below | 25.8 | 22.8 | 22.0 | 25.9 | 23.7 | |
| Junior college | 24.0 | 23.7 | 23.9 | 24.5 | 23.9 | |
| College or above | 50.2 | 53.5 | 54.1 | 49.6 | 52.5 | |
| Maternal educational level (%) | .237 | |||||
| High school or below | 27.0 | 24.8 | 22.6 | 28.3 | 25.2 | |
| Junior college | 27.1 | 27.0 | 28.1 | 25.5 | 27.1 | |
| College or above | 45.9 | 48.2 | 49.3 | 46.2 | 47.7 | |
| Family income (%) | .763 | |||||
| 5,000 or below | 21.4 | 21.0 | 19.3 | 20.2 | 20.7 | |
| 5,000–12,000 | 42.7 | 44.2 | 45.7 | 43.4 | 44.0 | |
| 12,000 or above | 21.4 | 21.3 | 22.6 | 21.0 | 21.6 | |
| Not clear | 14.5 | 13.5 | 12.3 | 15.5 | 13.7 | |
| Weekly sleep duration (h/d) | 9.05 ± 0.79 | 9.12 ± 0.64 | 9.16 ± 0.68 | 9.21 ± 0.77 | 9.12 ± 0.70 | <.01 |
| Weekday sleep duration | 9.15 ± 0.80 | 8.96 ± 0.65 | 8.74 ± 0.68 | 8.41 ± 0.80 | 8.92 ± 0.74 | <.01 |
| Weekend sleep duration | 8.79 ± 0.87 | 9.53 ± 0.68 | 10.21 ± 0.72 | 11.22 ± 0.91 | 9.61 ± 1.02 | <.01 |
| MSFsc (h) | 03:16 ± 00:49 | 03:13 ± 00:31 | 03:12 ± 00:37 | 03:04 ± 00:50 | 03:13 ± 00:40 | <.01 |
| Nap (min/d) | 39.79 ± 27.12 | 42.45 ± 26.82 | 42.90 ± 26.78 | 46.23 ± 32.62 | 42.14 ± 27.43 | <.01 |
| MVPA (min/d) | 59.67 ± 54.96 | 59.32 ± 54.23 | 59.01 ± 54.79 | 60.39 ± 60.96 | 59.43 ± 55.08 | .982 |
| SB (h/d) | 2.76 ± 1.41 | 2.68 ± 1.32 | 2.90 ± 1.42 | 3.30 ± 1.61 | 2.80 ± 1.40 | <.01 |
| BMI | 17.51 ± 12.67 | 16.94 ± 4.29 | 17.47 ± 15.84 | 16.87 ± 2.90 | 17.20 ± 10.19 | .323 |
Normally distributed continuous data are presented as means ± SD; categorical data are presented in percentages. P-values for trends across the catch-up sleep duration groups were calculated by using chi-square tests for the dichotomous variables and categorical variables and analysis of variance for continuous variables. BMI = body mass index (kg/m2), MSFsc = midpoint of sleep on free days corrected for sleep extension on free days, MVPA = moderate to vigorous physical activity, SB = sedentary behavior, SD = standard deviation.
Continuous sleep duration and EFs
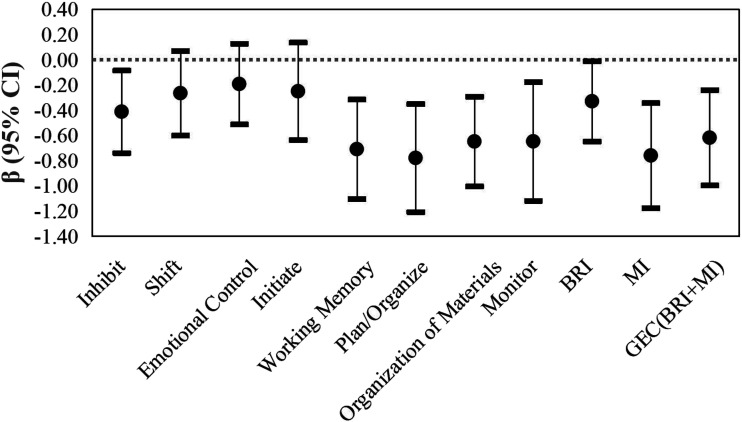
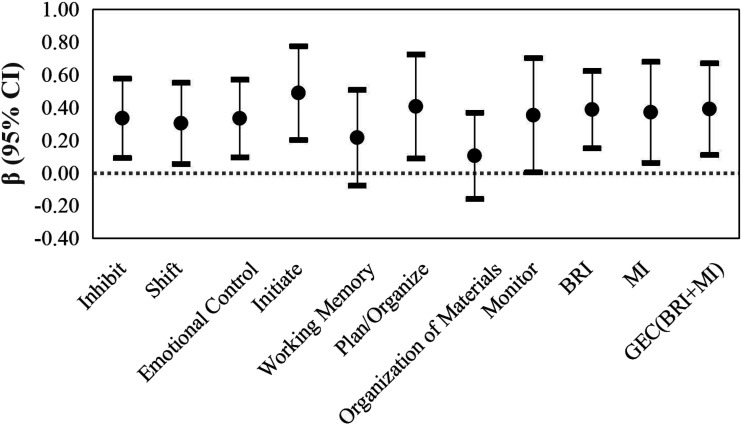
Overall, children slept significantly longer on weekends than weekdays (P < .01). We observed that the shorter the duration of sleep on weekdays, the longer the duration of catch-up sleep on weekends (Table 1). The linear regression analyses of the association between different types of sleep duration and EFs are represented in Figure 1 and Figure 2. After adjustment for covariates, weekday sleep duration had a negative association with scores on the BRI (β, –.33; 95% CI, –.65 to –.01), MI (β, –.76; 95% CI, –1.18 to –.34), and GEC (β,–.62; 95% CI, –1.00–.24), while a significant positive correlation was observed between weekend catch-up sleep and scores on the BRI (β, .39; 95% CI, .15–.62), MI (β, .37; 95% CI, .06–.68), and GEC (β, .39; 95% CI, .11–.67).
Figure 1. Multiple linear regression for the associations of weekday sleep duration with EFs score.
Adjusted for age, sex, paternal and maternal educational level, family income, MVPA, SB, BMI, MSFsc, Nap, and weekend catch-up sleep duration. BMI = body mass index, kg/m2, BRI = Behavioral Regulation Index, EF = executive functions, GEC = Global Executive Composite, MI = Metacognition Index, MSFsc = midpoint of sleep on weekends corrected for sleep extension on weekends, MVPA = moderate-to-vigorous physical activity, SB = sedentary behavior.
Figure 2. Multiple linear regression for the associations of weekend catch-up sleep duration with EFs score.
Adjusted for age, sex, paternal and maternal educational level, family income, MVPA, SB, BMI, MSFsc, Nap, and weekday sleep duration. BMI = body mass index, kg/m2, BRI = Behavioral Regulation Index, EF = executive functions, GEC = Global Executive Composite, MI = Metacognition Index, MSFsc = midpoint of sleep on weekends corrected for sleep extension on weekends, MVPA = moderate-to-vigorous physical activity, SB = sedentary behavior.
Categorical sleep duration and EFs
We conducted analyses for participants stratified by weekday sleep duration and catch-up sleep duration. The proportions of weekday sleep duration for < 9 hours, 9–11 hours, and > 11 hours were 2,566 (54.4%), 2,049 (44.6%), and 49 (1.0%), respectively. (The sample size of weekday sleep duration for > 11 hours was too small, so it is not shown in the following results.) Table 2 shows the distribution of EFs scores stratified by weekday sleep duration and weekend catch-up sleep duration. Overall, EFs scores were higher in the < 9 hours’ weekday sleep duration group than in the 9–11 hours’ weekday sleep duration group (P < .01).
Table 2.
Distribution of EFs scores stratified by weekday sleep duration and weekend catch-up sleep duration.
| Executive function | Weekday sleep duration | No catch-up | 0–1 hour | 1–2 hours | >2 hours | Total | P total |
|---|---|---|---|---|---|---|---|
| n (%) | <9 hours | 519 (20.3%) | 1,093 (42.8%) | 653 (25.5%) | 291 (11.4%) | 2,566 (54.4%) | |
| 9–11 hours | 705 (33.7%) | 984 (47.0%) | 328 (15.7%) | 77 (3.7%) | 2,049 (44.6%) | ||
| >11 hours | 24 (49.0%) | 20 (40.8%) | 5 (10.2%) | 0 (.0%) | 49 (1.0%) | ||
| Inhibit | <9 hours | 46.31 ± 7.27 | 46.31 ± 7.20 | 46.67 ± 7.25 | 47.33 ± 7.44 | 46.52 ± 7.26 | <.01 |
| 9–11 hours | 45.31 ± 6.77 | 45.41 ± 6.54 | 46.72 ± 7.12 | 47.35 ± 8.34 | 45.65 ± 6.80 | ||
| Shift | <9 hours | 46.25 ± 7.22 | 46.43 ± 7.30 | 46.15 ± 7.13 | 47.94 ± 7.79 | 46.49 ± 7.31 | <.01 |
| 9–11 hours | 45.58 ± 6.86 | 45.40 ± 6.81 | 46.30 ± 7.61 | 46.57 ± 6.90 | 45.65 ± 6.96 | ||
| Emotional control | <9 hours | 42.80 ± 7.05 | 42.85 ± 6.83 | 42.94 ± 7.15 | 44.22 ± 7.44 | 43.02 ± 7.04 | <.01 |
| 9–11 hours | 42.24 ± 6.64 | 42.11 ± 6.31 | 43.50 ± 6.99 | 43.35 ± 6.75 | 42.42 ± 6.56 | ||
| Initiate | <9 hours | 47.48 ± 8.04 | 47.58 ± 8.66 | 47.52 ± 8.42 | 49.62 ± 9.08 | 47.78 ± 8.55 | <.01 |
| 9–11 hours | 46.55 ± 8.10 | 46.89 ± 7.96 | 48.24 ± 8.48 | 48.52 ± 7.67 | 47.05 ± 8.10 | ||
| Working memory | <9 hours | 50.57 ± 8.87 | 50.22 ± 8.54 | 50.42 ± 8.73 | 52.43 ± 9.19 | 50.59 ± 8.75 | <.01 |
| 9–11 hours | 49.09 ± 8.51 | 49.06 ± 8.19 | 50.43 ± 8.60 | 51.14 ± 8.13 | 49.36 ± 8.38 | ||
| Plan/organize | <9 hours | 52.30 ± 9.74 | 51.56 ± 9.25 | 52.29 ± 9.34 | 53.79 ±10.15 | 52.15 ± 9.50 | <.01 |
| 9–11 hours | 50.42 ± 9.36 | 50.64 ± 9.23 | 52.29 ± 9.80 | 51.32 ± 7.90 | 50.85 ± 9.34 | ||
| Organization of materials | <9 hours | 45.44 ± 7.97 | 45.32 ± 7.69 | 45.32 ± 7.67 | 46.34 ± 7.77 | 45.46 ± 7.75 | <.01 |
| 9–11 hours | 44.77 ± 7.91 | 44.39 ± 7.42 | 45.34 ± 7.36 | 46.12 ± 8.32 | 44.73 ± 7.62 | ||
| Monitor | <9 hours | 51.97 ± 10.22 | 51.78 ± 10.09 | 51.96 ± 9.73 | 53.86 ± 10.63 | 52.10 ± 10.10 | <.01 |
| 9–11 hours | 50.98 ± 10.63 | 50.81 ± 9.97 | 52.49 ± 10.00 | 53.01 ± 10.04 | 51.21 ± 10.22 | ||
| BRI | <9 hours | 44.15 ± 7.06 | 44.25 ± 6.92 | 44.37 ± 7.16 | 45.75 ± 7.33 | 44.43 ± 7.07 | <.01 |
| 9–11 hours | 43.23 ± 6.65 | 43.21 ± 6.32 | 44.67 ± 7.15 | 44.99 ± 7.44 | 43.51 ± 6.64 | ||
| MI | <9 hours | 49.77 ± 9.36 | 49.42 ± 9.08 | 49.71 ± 9.00 | 51.70 ± 9.71 | 49.82 ± 9.21 | <.01 |
| 9–11 hours | 48.22 ± 9.13 | 48.25 ± 8.74 | 49.91 ± 9.14 | 50.19 ± 8.49 | 48.57 ± 8.95 | ||
| GEC(BRI+MI) | <9 hours | 47.52 ± 8.41 | 47.31 ± 8.26 | 47.55 ± 8.25 | 49.43 ± 8.74 | 47.66 ± 8.36 | <.01 |
| 9–11 hours | 46.16 ± 8.23 | 46.12 ± 7.76 | 47.82 ± 8.30 | 48.16 ± 7.99 | 46.48 ± 8.04 |
EFs scores are presented as mean ± SD. Data were compared by analysis of variance. Ptotal represents the significance of distribution difference in EFs scores on different weekday sleep duration levels. BRI = Behavioral Regulation Index, EF = executive functions, GEC = Global Executive Composite, MI = Metacognition Index.
Further, linear regression analyses were performed to test the associations between different levels of catch-up sleep duration and EFs at different levels of weekday sleep duration. (Table 3) For participants who slept for 9–11 hours during weekdays, compared to the no catch-up group, catch-up sleep for 1–2 hours was associated with increased scores on the BRI (β, 1.46; 95% CI, .52–2.40), MI (β, 1.74; 95% CI, .48–3.01), and GEC (β, 1.71; 95% CI, .57–2.85). Weekend catch-up sleep for > 2 hours was significantly associated with increased scores on the BRI (β, 2.04; 95% CI, .31–3.76), MI (β, 2.72; 95% CI, .40–5.04), and GEC (β, 2.64; 95% CI, .55–4.73). However, these associations were not observed among participants with < 9 hours of weekday sleep duration.
Table 3.
Linear regression of the associations between weekend catch-up sleep duration and EFs stratified by weekday sleep duration.
| Executive function | Weekday sleep duration | No catch-up | 0–1 hour | 1–2 hours | >2 hours |
|---|---|---|---|---|---|
| Inhibit | <9 hours | Ref | –.07 (–.90, .77) | 0.17 (–.76, 1.10) | .25 (–.93, 1.43) |
| 9–11 hours | Ref | .06 (–.66, .79) | 1.59 (.62, 2.55)** | 2.26 (.49, 4.03)* | |
| Shift | <9 hours | Ref | .11 (–.73, .96) | –.25 (–1.19, .69) | 1.66 (.46, 2.85)** |
| 9–11 hours | Ref | –.43 (–1.17, .31) | 0.51 (–.48, 1.50) | 1.43 (–.39, 3.26) | |
| Emotional control | <9 hours | Ref | –.05 (–.86, .77) | 0.05 (–.85, .96) | 1.12 (–.04, 2.27) |
| 9–11 hours | Ref | –.07 (–.77, .63) | 1.34 (0.41, 2.28)** | 1.34 (–.38, 3.07) | |
| Initiate | <9 hours | Ref | .01 (–.97, .98) | –.40 (–1.48, .68) | 1.21 (–.17, 2.59) |
| 9–11 hours | Ref | .38 (–.49, 1.25) | 1.73 (.57, 2.89)** | 2.85 (0.72, 4.99)** | |
| Working memory | <9 hours | Ref | –.41 (–1.40, .58) | –.69 (–1.79, .41) | 0.47 (–.93, 1.87) |
| 9–11 hours | Ref | –.07 (–.95, .82) | 1.36 (.17, 2.54)* | 2.42 (.24, 4.60)* | |
| Plan/organize | <9 hours | Ref | –1.10 (–2.16, –.04)* | –.65 (–1.83, .53) | .59 (–.91, 2.10) |
| 9–11 hours | Ref | .07 (–.91, 1.05) | 1.93 (0.62, 3.23)** | 2.00 (–.39, 4.40) | |
| Organization of materials | <9 hours | Ref | –.31 (–1.20, .57) | –.49 (–1.47, .49) | .38 (–.87, 1.63) |
| 9–11 hours | Ref | –.62 (–1.43, .19) | .63 (–.45, 1.71) | 1.55 (–.44, 3.54) | |
| Monitor | <9 hours | Ref | –.65 (–1.81, .50) | –.75 (–2.03, .53) | .85 (–.79, 2.48) |
| 9–11 hours | Ref | –.15 (–1.25, .94) | 1.67 (.22, 3.13)* | 3.04 (.37, 5.72)* | |
| BRI | <9 hours | Ref | .02 (–.79, .83) | .04 (–.85, .94) | 1.10 (–.05, 2.24) |
| 9–11 hours | Ref | –.10 (–.81, .60) | 1.46 (.52, 2.40)** | 2.04 (.31, 3.76)* | |
| MI | <9 hours | Ref | –.61 (–1.65, .42) | –.69 (–1.84, .46) | .81 (–.66, 2.27) |
| 9–11 hours | Ref | –.05 (–1.00, .90) | 1.74 (.48, 3.01)** | 2.72 (.40, 5.04)* | |
| GEC(BRI+MI) | <9 hours | Ref | –.43 (–1.37, .51) | –.49 (–1.53, .56) | .94 (–.39, 2.27) |
| 9–11 hours | Ref | –.12 (–.97, .73) | 1.71 (.57, 2.85)** | 2.64 (.55, 4.73)* |
Adjusted for age, sex, paternal and maternal educational level, family income, MSFsc, Nap, MVPA, SB, BMI, and weekday sleep duration. * P < 0.05. ** P < 0.01. BMI = body mass index, kg/m2, BRI = Behavioral Regulation Index, EF = executive functions, GEC = Global Executive Composite, MI = Metacognition Index, MSFsc = midpoint of sleep on free days corrected for sleep extension on free days, MVPA = moderate-to-vigorous physical activity, REF = reference, SB = sedentary behavior.
In older children (10–12 years old), longer weekend catch-up sleep (> 2 hours) was related to higher scores on the BRI (β, 1.66; 95% CI, .34–2.99), MI (β, 2.67; 95% CI, .97–4.37), and GEC (β, 2.39; 95% CI, .82–3.95). There were no statistically significant results for children aged 6–9. In boys, longer weekend catch-up sleep (> 2 hours) was related to higher scores on the BRI (β, 2.05; 95% CI, .63–3.47), MI (β, 2.54; 95% CI, .75–4.33), and GEC (β, 2.50; 95% CI, .85–4.16). We did not observe a significant interaction effect between sex, age, and weekend catch-up sleep duration and EFs (P > .05) (Table S1 and (Table S2 in the supplemental material).
DISCUSSION
In this school-based cross-sectional study, we examined the relationship between weekend catch-up sleep duration and EFs performance in school-aged children. We found that sleep duration on weekdays was positively related with EFs, while catch-up sleep duration on weekends was negatively related with EFs. Furthermore, among those with adequate sleep duration on weekdays, more than 1 hour weekend catch-up sleep was associated with poor EFs.
As early as 1998, a study found a decreased performance in verbal creativity and abstract thinking after 5 hours of sleep restriction.31 The association between short weekday sleep duration and poor EFs was supported by a meta-analysis of 86 studies.22 However, in most of these studies, individual differences in weekday and weekend sleep duration were obscured. Several studies have shown that weekend catch-up sleep has a different relationship with health than weekday sleep. More weekend catch-up sleep may potentially reduce the risk of obesity,13 hypertension,32 and asthma33 in children and adolescents with weekday sleep deprivation, but children and youths with longer weekend catch-up sleep may be more likely to have poorer academic performance, more depressive symptoms, more substance use, and an increased risk for being overweight/obese.34 These findings highlight the potential importance of sleep variability and irregularity. In our study, when sleep duration was examined separately for weekdays and weekends, weekend catch-up sleep was inversely correlated with EFs, while weekday sleep duration was positively correlated with EFs. Our results have added the observation that differences in sleep duration between weekday and weekend may have unique associations with poor EFs.
Weekend catch-up sleep represents an irregular sleep pattern and is assumed to be an indicator of cumulative sleep debt.35 Although weekend catch-up sleep increased average sleep duration per week, short sleep during the weekday was still associated with poor EFs. Subgroup analysis also supported the association between short weekday sleep (< 9 hours) and poor EFs, regardless of weekend catch-up sleep. This result was complementary to that of a recent experimental study of healthy male adults, which showed no efficacy in one recovery night to remedy EF deficits related to sleep restriction.36 The negative effects of weekday sleep restriction on neurobehavioral function accumulated even after recovery sleep.37,38 Meanwhile, an experimental study showed that gradual sleep extension during the week was related to changes in some aspects of cognitive performance.39 The discrepancies may be caused in part by differences in the age of participants, methods of assessment, and statistical methods applied. In particular, the experimental studies did not utilize the typical and habitual sleep patterns of school-age children that include successive cycles of weekday sleep restriction and weekend sleep extension.
Interestingly, we found that weekend catch-up sleep for more than 1 hour was associated with poor EFs among children who had adequate weekday sleep duration (9–11 hours). For children who had adequate sleep duration (9–11 hours), the link between catch-up sleep duration and EFs has several possible explanations. First, because individual sleep needs vary, weekend catch-up sleep may be reflecting a degree of sleep insufficiency that average sleep duration does not.33 To be more specific, the children categorized as sleeping 9–11 hours on weekdays included those who actually needed longer sleep duration. However, the long sleep duration on weekends indicated that the sleep needs of these children could not be satisfied at ordinary times. Thus, more weekend catch-up sleep is seen as indirect evidence of sleep deprivation, which is associated with impaired daytime functioning.40 Second, weekend catch-up sleep is considered as an indicator of irregular sleep patterns, and children’s neurobehavioral functions may not adapt to successive cycles of relative sleep restriction and sleep extension.38 Previous studies have reported that sleep irregularity increases risks related to health outcomes.41 A previous study also reported that weekday-weekend sleep variations of over 2 hours led to an increased risk of behavioral difficulties in children aged 5–10 years.42 However, studies have also observed an inverted U-shaped association between sleep duration and health outcomes.43,44 Longer sleep than usual might worsen sleep quality and, as a consequence, cognitive functioning.25,45 However, due to the very limited number of prospective studies, these results should be interpreted cautiously.
The differences in sleep between weekdays and weekends pertain not only to sleep duration but also to sleep timing. Chronotype describes individual differences in sleep timing,28 which was expressed in terms of MSFsc in our study. When we corrected for MSFsc, the associations of weekend catch-up sleep duration with EFs remained. Previous epidemiological studies have also reported that the link between sleep duration and EFs could be influenced by age and sex. Neural development is dynamic and EFs experience a critical period between 7 and 9 years of age and are relatively mature by 12 years.21 Studies have found that sleep patterns are affected by pubertal development, and children’s need for sleep gradually decreases with age.21,46 Meanwhile, prior research suggests that circadian biology varies by sex, with the consequences of inadequate sleep often being more pronounced in girls.18 In the present study, results from a subgroup analysis suggested an association between weekend catch-up and EFs in older children or boys, but not in younger children and girls. However, the interaction terms between age or sex and weekend catch-up sleep were not statistically significant in this study. More studies are needed before any firm conclusions can be drawn.
To our knowledge, this is the first study to examine the relationship between weekend catch-up sleep and everyday executive functions in children. The contribution of weekend catch-up sleep to EFs has not been captured in most studies due to study design. Our study differed in that we assessed weekday and weekend sleep separately. Previous findings have highlighted the importance of compliance with the recommendations for optimal sleep duration in children and adolescents. Our data support these initiatives and, more importantly, reveal the possible consequences of weekend catch-up sleep.
There are several limitations to our study. First, the available data was limited by self-reported measures. However, the use of objective methods (such as accelerometer) is usually not feasible for sleep-duration assessment over a long period in large populations. The questionnaire we used was validated in an earlier pilot study, which showed its high reliability and validity. The mean reliability coefficient was .63, and the mean validity coefficient was .6629. Self-reported sleep duration and BRIEF-P produced results closer to actual situations by assessing children’s performance in a natural environment. Second, despite best efforts to make extensive adjustments, we did not account for the role of sleep quality, exact puberty factors, genetic factors, and other relevant diagnoses in the current study. Last, this study used a cross-sectional study design, which was unable to evaluate the causality or temporal order of the reported associations. Longitudinal investigations are needed to establish the underpinnings of these associations and for the appropriate policy to achieve healthier and more balanced sleep patterns in the school-aged children.
Collectively, these findings stress that weekend catch-up sleep could not restore the EF deficits related to short weekday sleep. Weekend catch-up sleep over 1 hour may have adverse effects on EFs in school-aged children. A good practice for children is always to ensure adequate sleep, and to maintain regular sleep by avoiding for more than 1 hour weekend catch-up sleep. This study can contribute to appropriate policy to achieve healthier and more balanced sleep patterns in the school-aged children.
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. The authors report that this work was supported by the National Natural Science Foundation of China (81673193) and Natural Science Foundation of Guangdong Province, China (2019A1515011462). The authors declare no conflict of interest.
SUPPLEMENTARY MATERIAL
ACKNOWLEDGMENTS
The authors thank all individuals who volunteered to participate in this study.
ABBREVIATIONS
- BRI
Behavioral Regulation Index
- BRIEF-P
Behavior Rating Inventory of Executive Function Parent Form
- EFs
executive functions
- GEC
Global Executive Composite
- MI
Metacognition Index
- MSFsc
midpoint of sleep on free days corrected for sleep extension on free days
REFERENCES
- 1.Matricciani L, Paquet C, Galland B, Short M, Olds T. Children’s sleep and health: A meta-review. Sleep Med Rev. 2019;46136–150. 10.1016/j.smrv.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 2.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. 10.1016/j.sleh.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 3.Short MA, Blunden S, Rigney G, et al. Cognition and objectively measured sleep duration in children: a systematic review and meta-analysis. Sleep Health. 2018;4(3):292–300. 10.1016/j.sleh.2018.02.004 [DOI] [PubMed] [Google Scholar]
- 4.Roman-Viñas B, Chaput J, Katzmarzyk PT, et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int J Behav Nutr Phy. 2016;13(1):123. 10.1186/s12966-016-0449-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Iresearch. White paper on sleep health of Chinese adolescents and children in 2019. https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CPFD&dbname=CPFDLAST2019&filename=ASSC201904001006&uid=WEEvREcwSlJHSldRa1FhdXNzY2Z2d21lZi9vWVAyTG1TYlVKV0pKUkZXMD0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4IQMovwHtwkF4VYPoHbKxJw!!&v=MjY3ODhxeGRFZU1PVUtyaWZaZVp2RXl2blU3cklKVjRVSkQ3WWJiRzRIOWpNcTQ5Rlplc1BDaE5LdWhkaG5qOThUbmpx. Accessed May 23, 2020.
- 6.Diamond A. Executive functions. Annu Rev Psychol. 2013;64(1):135–168. 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krause AJ, Simon EB, Mander BA, et al. The sleep-deprived human brain. Nat Rev Neurosci. 2017;18(7):404–418. 10.1038/nrn.2017.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Killgore WD. Effects of sleep deprivation on cognition. Prog Brain Res. 2010;185105–129. 10.1016/B978-0-444-53702-7.00007-5 [DOI] [PubMed] [Google Scholar]
- 9.Jones K, Harrison Y. Frontal lobe function, sleep loss and fragmented sleep. Sleep Med Rev. 2001;5(6):463–475. 10.1053/smrv.2001.0203 [DOI] [PubMed] [Google Scholar]
- 10.Pace-Schott EF, Hutcherson CA, Bemporad B, et al. Failure to find executive function deficits following one night’s total sleep deprivation in university students under naturalistic conditions. Behav Sleep Med. 2009;7(3):136–163. 10.1080/15402000902976671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tucker AM, Whitney P, Belenky G, Hinson JM, Van Dongen HPA. Effects of sleep deprivation on dissociated components of executive functioning. Sleep. 2010;33(1):47–57. 10.1093/sleep/33.1.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Depner CM, Melanson EL, Eckel RH, et al. Ad libitum weekend recovery sleep fails to prevent metabolic dysregulation during a repeating pattern of insufficient sleep and weekend recovery sleep. Curr Biol. 2019;29(6):957–967.e4. 10.1016/j.cub.2019.01.069 [DOI] [PubMed] [Google Scholar]
- 13.Wing YK, Li SX, Li AM, Zhang J, Kong APS. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics. 2009;124(5):e994–e1000. 10.1542/peds.2008-3602 [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, Paksarian D, Lamers F, et al. Sleep patterns and mental health correlates in US adolescents. J Pediatr. 2017;182137–143. 10.1016/j.jpeds.2016.11.007 [DOI] [PubMed] [Google Scholar]
- 15.Chen T, Wu Z, Shen Z, et al. Sleep duration in Chinese adolescents: biological, environmental, and behavioral predictors. Sleep Med. 2014;15(11):1345–1353. 10.1016/j.sleep.2014.05.018 [DOI] [PubMed] [Google Scholar]
- 16.Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005;115(suppl 1):250–256. 10.1542/peds.2004-0815G [DOI] [PubMed] [Google Scholar]
- 17.Yoo SS, Hu PT, Gujar N, Jolesz FA, Walker MP. A deficit in the ability to form new human memories without sleep. Nat Neurosci. 2007;10(3):385–392. 10.1038/nn1851 [DOI] [PubMed] [Google Scholar]
- 18.Liisa Kuulaa, Pesonen AK, Martikainen S. Poor sleep and neurocognitive function in early adolescence. Sleep Med. 2015;16(10):1207–1212. 10.1016/j.sleep.2015.06.017 [DOI] [PubMed] [Google Scholar]
- 19.Mak KK, Lee SL, Ho SY, Lo WS, Lam TH. Sleep and academic performance in Hong Kong adolescents. J Sch Health. 2012;82(11):522–527. 10.1111/j.1746-1561.2012.00732.x [DOI] [PubMed] [Google Scholar]
- 20.LeMay-Russell S, Tanofsky-Kraff M, Schvey NA, et al. Associations of weekday and weekend sleep with children’s reported eating in the absence of hunger. Nutrients. 2019;11(7):1658. 10.3390/nu11071658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychol. 2002;8(2):71–82. 10.1076/chin.8.2.71.8724 [DOI] [PubMed] [Google Scholar]
- 22.Astill RG, Van der Heijden KB, Van IJzendoorn MH, Van Someren EJW. Sleep, cognition, and behavioral problems in school-age children: A century of research meta-analyzed. Psychol Bull. 2012;138(6):1109–1138. 10.1037/a0028204 [DOI] [PubMed] [Google Scholar]
- 23.Erath SA, Tu KM, Buckhalt JA, El-Sheikh M. Associations between children’s intelligence and academic achievement: the role of sleep. J Sleep Res. 2015;24(5):510–513. 10.1111/jsr.12281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stea TH, Knutsen T, Torstveit MK. Association between short time in bed, health-risk behaviors and poor academic achievement among Norwegian adolescents. Sleep Med. 2014;15(6):666–671. 10.1016/j.sleep.2014.01.019 [DOI] [PubMed] [Google Scholar]
- 25.de Bruin EJ, van Run C, Staaks J, Meijer AM. Effects of sleep manipulation on cognitive functioning of adolescents: A systematic review. Sleep Med Rev. 2017;3245–57. 10.1016/j.smrv.2016.02.006 [DOI] [PubMed] [Google Scholar]
- 26.Lv Y, Cai L, Gui Z. Effects of physical activity and sedentary behaviour on cardio-metabolic risk factors and cognitive function in children: protocol for a cohort study. BMJ Open. 2019;9(10):e030322. 10.1136/bmjopen-2019-030322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ying Q, Yufeng W. Reliability and validity of behavior rating scale of executive function parent form for school age children in China. Beijing Da Xue Xue Bao Yi Xue Ban [JOURNAL OF PEKING UNIVERSITY]. 2007;39(03):277–283 [PubMed] [Google Scholar]
- 28. Gioia GA, Isquith PK, Guy SC, Kenworthy L. The Behavior Rating Inventory of Executive Function. Professional Manual. Psychological Assessment Resources (PAR); 2000. [Google Scholar]
- 29.Yajie Lv, Lijuan Lai, Danling Li, et al. Study on the reliability and validity of physical health surveillance system questionnaire for primary school students in Guangzhou. Maternal and Child Health Care of China. 2020;35(08):1511–1516. 10.1016/j.cub.2012.03.038 [DOI] [Google Scholar]
- 30.Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–943. 10.1016/j.cub.2012.03.038 [DOI] [PubMed] [Google Scholar]
- 31.Randazzo AC, Muehlbach MJ, Schweitzer PK, Walsh JK. Cognitive function following acute sleep restriction in children ages 10-14. Sleep. 1998;21(8):861–868 [PubMed] [Google Scholar]
- 32.Gupta N, Maranda L, Gupta R. Differences in self-reported weekend catch up sleep between children and adolescents with and without primary hypertension. Clin Hypertens. 2018;24(1):7. 10.1186/s40885-018-0092-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Han CH, Chung JH. Association of asthma and sleep insufficiency among South Korean adolescents: analysis of web-based self-reported data from the Korean youth risk behavior web-based survey. J Asthma. 2020;57(3):253–261. 10.1080/02770903.2019.1565827 [DOI] [PubMed] [Google Scholar]
- 34.Sun W, Ling J, Zhu X, Lee TM, Li SX. Associations of weekday-to-weekend sleep differences with academic performance and health-related outcomes in school-age children and youths. Sleep Med Rev. 2019;4627–53. 10.1016/j.smrv.2019.04.003 [DOI] [PubMed] [Google Scholar]
- 35.Kuula L, Pesonen AK, Merikanto I, et al. Development of late circadian preference: sleep timing from childhood to late adolescence. J Pediatr. 2018;194182–189.e1. 10.1016/j.jpeds.2017.10.068 [DOI] [PubMed] [Google Scholar]
- 36. doi: 10.3389/fnins.2019.00591. Rabat A, Arnal PJ, Monnard H, et al. Limited benefit of sleep extension on cognitive deficits during total sleep deprivation: illustration with two executive processes. Front Neurosci. 2019;13:591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhao Z, Zhao X, Veasey SC. Neural consequences of chronic short sleep: reversible or lasting?. Front Neurol. 2017;8235. 10.3389/fneur.2017.00235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lo JC, Lee SM, Teo LM, Lim J, Gooley JJ, Chee MW. Neurobehavioral impact of successive cycles of sleep restriction with and without naps in adolescents. Sleep. 2017;40(2. 10.1093/sleep/zsw042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: an experimental study. Sleep Med. 2013;14(6):510–517. 10.1016/j.sleep.2013.01.012 [DOI] [PubMed] [Google Scholar]
- 40.Jarrin DC, McGrath JJ, Silverstein JE, Drake C. Objective and subjective socioeconomic gradients exist for sleep quality, sleep latency, sleep duration, weekend oversleep, and daytime sleepiness in adults. Behav Sleep Med. 2013;11(2):144–158. 10.1080/15402002.2011.636112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hwangbo Y, Kim W, Chu MK, Yun C, Yang KI. Association between weekend catch-up sleep duration and hypertension in Korean adults. Sleep Med. 2013;14(6):549–554. 10.1016/j.sleep.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 42.Biggs SN, Lushington K, van den Heuvel CJ, Martin AJ, Kennedy JD. Inconsistent sleep schedules and daytime behavioral difficulties in school-aged children. Sleep Med. 2011;12(8):780–786. 10.1016/j.sleep.2011.03.017 [DOI] [PubMed] [Google Scholar]
- 43.Patel VC, Spaeth AM, Basner M. Relationships between time use and obesity in a representative sample of Americans. Obesity (Silver Spring). 2016;24(10):2164–2175. 10.1002/oby.21596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiao Q, Keadle SK, Hollenbeck AR, Matthews CE. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol. 2014;180(10):997–1006. 10.1093/aje/kwu222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wild CJ, Nichols ES, Battista ME, Stojanoski B, Owen AM. Dissociable effects of self-reported daily sleep duration on high-level cognitive abilities. Sleep. 2018;41(12. 10.1093/aje/kwu222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gau S, Soong W. The transition of sleep-wake patterns in early adolescence. Sleep. 2003;26(4):449–454. 10.1093/sleep/26.4.449 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.