Citation:
Ekiz T, Kara M, Özçakar L. Revisiting vitamin D and home-based exercises for patients with sleep apnea facing the COVID-19 quarantine. J Clin Sleep Med. 2020;16(8):1409–1410.
Patients with obstructive sleep apnea syndrome (OSAS) are vulnerable to geriatric syndromes, such as sarcopenia and frailty. Herein, sarcopenia can be defined as the age-related loss of muscle mass and function, which is the physical determinant of frailty.1 Frailty refers to the multisystem impairment related to increased susceptibility to endogenous or exogenous stressors and infections. In this sense, preventive treatments (eg, vitamin D and exercise) for sarcopenia and frailty are noteworthy during the long-lasting quarantine days of COVID-19.2 Accordingly, this letter will guide and encourage sleep physicians to prescribe vitamin D and home-based exercises for OSAS patients to fight against infection, immobility, sarcopenia, and frailty.
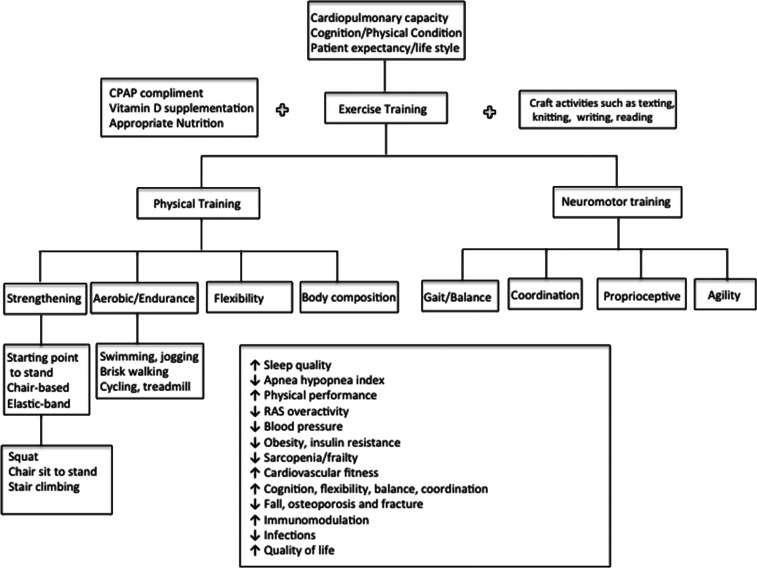
First, the exercise program, preferably multicomponent training, should be planned and tailored for the individual patient. Therefore, the patient should be evaluated for cardiopulmonary capacity, comorbidities (especially those related to overactivity of the renin-angiotensin-aldosterone system), cognitive and physical functions, and the patient’s lifestyle (Figure 1). Herewith, continuous positive airway pressure (CPAP) complement leads to reinforcement in the fight against immobilization because it alleviates OSAS-related symptoms, such as daytime sleepiness, headache, and concentration difficulty. In addition, CPAP treatment regulates renin-angiotensin-aldosterone system and sympathetic activities and thus has a beneficial role in regulating blood pressure, which, in the case of dysregulation, can result in cardiovascular and respiratory complications and cognitive impairment.3 Of note, it should be highlighted once again that force generation and physical functionality are directly related to cognition.1 Keeping in mind the decreased cognitive functions in OSAS patients, it would be reasonable also to encourage activities that improve cognition. In this sense, CPAP complement before initiating exercise training can be vital.
Figure 1. Multicomponent exercise training.
The algorithm/scheme demonstrates the overall patient evaluation and prescription of physical and neuromotor training as well as their systemic effects.
The two main types of skeletal muscle fibers are slow-switch (type 1) and fast-twitch (type 2). The former maintains long-term contractions such as aerobic metabolism and endurance, whereas the latter generates stronger/faster force, which is important for power- and performance-requiring activities.1 Herein, improving power with low-intensity but high-velocity strengthening exercises might be more significant than that of the traditional moderate- to high- intensity but relatively low-velocity strengthening because power can be decreased even in patients with normal muscle strength. Therefore, power training should be seriously considered.
The loss of muscle strength and contraction velocity (ie, power) is seen earlier in the anterior thigh, which is rich in type 2 fibers. In this context, anterior-thigh strengthening exercises (squat, chair sit-to-stand, or stair-climbing; 3 × 10–12 repetitions) combined with aerobic exercises (walking or treadmill; 30 min/day) on consecutive days can be easily performed. Flexibility exercises, dynamic or slow-movement stretching, static or proprioceptive neuromuscular facilitation can improve range of motion (10–30 seconds, 2–5 times, everyday). Additionally, neuromotor training (such as tai chi, agility, balance, or coordination exercises) will also improve cognition and physical functionality (20-30 min/session, 2 or 3 day/week) (Figure 1).4
On the other hand, vitamin D is absolutely necessary for normal homeostasis of calcium and phosphorus, development and maintenance of bone tissue, cell proliferation, hormone secretion (prevention of insulin resistance), immune system, cognition, regulation of the renin-angiotensin system, as well as muscle mass and function. Although vitamin D deficiency has been reported in all ages, a positive association between body mass index and vitamin D deficiency has been reported. It has been also suggested that vitamin D deficiency promotes lipogenesis through increasing parathyroid hormone levels and increasing the inflow of calcium into adipocytes. Moreover, the active form of vitamin D decreases lipogenesis.5 The relationship between obesity and vitamin D deficiency should be considered bidirectional.5 Herein, vitamin D deficiency is more important, as obesity is a significant comorbidity in OSAS patients who have a tendency to gain weight and develop insulin resistance because of prolonged immobilization during the quarantine days. This fact is also crucial for muscle mass and function because sarcopenic obesity affects muscle function deleteriously. In this regard, we believe that vitamin D supplementation and/or food fortification will have synergistic effects.2 In people at higher risk of viral infections, such as influenza or COVID-19, the aim should be to escalate the 25-hydroxyvitamin D levels up to 40–60 ng/ml. In this regard, 10.000 IU of vitamin D3 per day is suggested for up to a month to rapidly increase the 25-hydroxyvitamin D levels and then 5.000 IU per day in the follow-up period.2
In conclusion, given their rare or no side effects and wide safety, prophylactic vitamin D supplementation and/or food fortification with exercise treatment might reasonably serve as a very convenient adjuvant protocol for the two pandemics (ie, vitamin D deficiency and COVID-19.2 Last, but not least, keeping in mind their immunomodulation effects, vitamin D supplementation and exercise training are native but unparalleled “defense weapons” against obesity, sarcopenia, frailty, and COVID-19 as well.
DISCLOSURE STATEMENT
The authors report no conflict of interests.
REFERENCES
- 1.Kara M, Kaymak B, Ata AM, et al. Sonographic thigh adjustment ratio—STAR A golden formula for the diagnosis of sarcopenia. Am J Phys Med Rehabil. 2020;10.1097/PHM.0000000000001439.. 10.1097/PHM.0000000000001439 [DOI] [PubMed] [Google Scholar]
- 2. doi: 10.1017/S0007114520001749. 10.1017/S0007114520001749 Kara M, Ekiz T, Ricci V, Kara Ö, Chang KV, Özçakar L. ‘Scientific Strabismus’ or two related pandemics: coronavirus disease and vitamin D deficiency [published online ahead of print, 2020 May 12]. Br J Nutr. 2020;1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicholl DDM, Hanly PJ, Zalucky AA, Handley GB, Sola DY, Ahmed SB. Sex differences in renal hemodynamics and renin-angiotensin system activity post-CPAP therapy in humans with obstructive sleep apnea. Am J Physiol Renal Physiol. 2020;318(1):F25–F34. 10.1152/ajprenal.00290.2019. 10.1152/ajprenal.00290.2019 [DOI] [PubMed] [Google Scholar]
- 4.Pescatello LS; American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. Philadelphia, PA: Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 5.de Oliveira LF, de Azevedo LG, da Mota Santana J, de Sales LPC, Pereira-Santos M. Obesity and overweight decreases the effect of vitamin D supplementation in adults: systematic review and meta-analysis of randomized controlled trials. Rev Endocr Metab Disord. 2020;21(1):67–76. 10.1007/s11154-019-09527-7. 10.1007/s11154-019-09527-7 [DOI] [PubMed] [Google Scholar]