Retinoblastoma (Rb), an intraocular malignancy of childhood, is most often (98%) caused by a mutation in the RB1 retinoblastoma tumor suppressor gene contained in the long arm of chromosome 13. In 60% of cases, the RB1 mutation exists only in the tumor (i.e., somatic), while in 40% of cases, patients have a germline mutation found in all cells of the body (i.e., germinal) (1). In 1971, Knudson proposed the two hit hypotheses of RB1 stating that patients with the hereditary form of the disease have their first hit (or mutation) in the germline and need one further hit in a somatic cell in the developing retina to cause Rb while the somatic form requires both hits in a single retinal cell to cause Rb (2). This hypothesis was borne from the observation that the bilateral, germline form of the disease presents at approximately 12 months of age, while the somatic form, due to the delay in acquiring the second mutation, presents at approximately 24 months of age(2).
While it is true that sporadic cases typically manifest as unilateral, unifocal disease consistent with somatic disease, 15% of unilateral patients without a positive family history may still harbor the hereditary, germline mutation(3). Children with germline mutations have a risk of developing multiple ocular tumors, secondary non-ocular cancers (4,5), an increased risk of secondary cancers when exposed to radiation(6) and an approximate 50% chance of passing this heritable cancer syndrome onto their future progeny. Thus, determining the presence or absence of a germline mutation in RB1 is a critical tool in the management of unilateral Rb. There remains a perception that age at presentation for children with unilateral Rb can help stratify the risk for the presence of a germline mutation and thus identify those children that need genetic testing. However, modern access to molecular testing and more recent publications suggest otherwise (7,8). In this retrospective study, we evaluated a cohort of patients with unilateral disease, without a family history of Rb, for a correlation of age with the presence or absence of a germline RB1 mutation.
Our protocol is as follows: we completed retrospective chart review of patients diagnosed with unilateral Rb between January 1990 and April 2017 at Children’s Hospital Los Angeles (CHLA). This protocol was approved by the Institutional Review Board. Inclusion criteria consisted of (1) a clinical diagnosis of unilateral Rb, (2) the absence of family history of Rb, and (3) the results of serum testing for germline RB1 mutations available for review.
Data were collected on laterality including the absence of bilateral or multifocal disease, family history, demographics, and tumor group status. Genetic testing was evaluated for a mutation in the RB1, mutation type, and the presence of mosaicism.
In order to evaluate the association between age at diagnosis of unilateral Rb and genetic status, we examined differences between those with a normal genetic test result and those who carry an RB1 mutation in terms of age. Statistical analyses were performed in JMP Pro 13. Because age was positively skewed, we used a non-parametric Wilcoxon rank-sum test to compare age between study groups. The tumor groups were compared using a Fisher’s exact test.
We identified a total of 182 patients who were diagnosed with unilateral Rb without a family history, received genetic testing which was available for review, and were included in this analysis.
Of the 182 patients included in the review, age at diagnosis was between 1 and 130 months. The average age at diagnosis for all patients with unilateral Rb was 23 months with a median age of 19 months. Tumors groups included groups B and C (8%), group D (42%), and group E (49%), with no significant difference in tumor groups between germline RB1 and non-germline patients (p = 0.8753). Forty-seven percent of patients were of Hispanic ethnicity with the next largest groups, Non-Hispanic White and Other as 17% each. Patient demographics and age-related data are presented in Table 1.
Table 1.
Demographics.
| Total n = 182 | RBI mutation n = 32 (18%) | No RBI mutation n = 150 (82%) | ||
|---|---|---|---|---|
| Gender | Male | 102 (56%) | 18 (56%) | 84 (56%) |
| Female | 80 (44%) | 14 (44%) | 66 (44%) | |
| Age | Mean age at diagnosis | 23 months | 26 months | 22 months |
| Median age at diagnosis | 19 months | 20 months | 19 months | |
| Age range | 1–130 months | 2–120 months | 1–130 months | |
| Laterality | R-sided | 106 (58%) | 19 (59%) | 87 (58%) |
| L-sided | 76 (42%) | 13 (41%) | 63 (42%) | |
| Group | B or C | 15 (8%) | 3 (9%) | 12 (8%) |
| D | 77 (42%) | 14 (44%) | 63 (42%) | |
| E | 90 (49%) | 15 (47%) | 75 (50%) | |
| Ethnicity | Hispanic | 86 (47%) | 14 (44%) | 72 (48%) |
| Non-Hispanic White | 31 (17%) | 6 (19%) | 25 (17%) | |
| Asian/Pacific Islander | 23 (13%) | 3 (9%) | 20 (13%) | |
| Black | 11 (6%) | 2 (6%) | 9 (6%) | |
| Other | 31 (17%) | 7 (22%) | 24 (16%) |
A positive genetic result with a germline RB1 mutation was found in 32 of 182 patients with unilateral Rb (18%). Of the 32 patients with a germline RB1 mutation, 18 patients (56%) were diagnosed between 1 and 24 months of age and 14 patients (44%) were diagnosed between 25 and 130 months of age. Unilateral patients who tested positive for an RB1 mutation had a mean age at diagnosis of 26 ± 22 months. Unilateral patients who tested negative for an RB1 mutation presented with a mean age at diagnosis of 22 ± 18 months. Although patients who tested negative for the RB1 mutation had a slightly younger age at diagnosis, this difference was not statistically significant (z = −0.991, p = 0.32). Furthermore, unilateral patients who carry an RB1 mutation and display mosaicism (z = 0.102, mean age at diagnosis = 31 months ± 33) were not significantly older than unilateral patients who do not display mosaicism (z = −0.102, mean age at diagnosis = 24 months ± 17), p = 0.92.
Of the 32 RB1 mutations identified among this cohort of unilateral, non-familial patients, mosaicism was identified in 10 patients, with five diagnosed before 24 months and 5 diagnosed after 24 months. The majority of mosaic mutations were point mutations including four nonsense mutations, two missense mutations, and two pathogenic mutations of unknown significance. There were also two small deletions.
Non-mosaic mutations consisted of point mutations causing three frameshift mutations, two nonsense mutations, four missense mutations, and two pathogenic mutations of unknown significance. There were three small deletions and eight 13q-chromosomal deletions (large enough to be seen on FISH analysis). Of the non-mosaic mutations above, the largest categories were point mutations (27%) and 13q deletions (36%).
The critical point to address is the correlation of age and RB1 mutational status. Knudson’s initial hypothesis of Rb tumorigenesis in 1971(2) suggested that tumor formation required two mutations, or “hits.” This hypothesis was born from the evaluation of 48 cases of Rb, noting that children with bilateral disease presented at a younger age than unilateral disease, presumably because children with bilateral Rb are born with the first mutation and require less time to acquire the second mutation. However, approximately 15% of children with unilateral Rb also have the germline mutation (3). It is thus often thought that regardless of laterality at presentation, children with germline Rb present at a younger age. However, with the advent of modern genetic testing for the RB1 gene, studies have been published which suggest that in fact there is no correlation between age and genetic status for children with unilateral disease (7–9). Lohmann et al. (9) evaluated 68 patients, Schuler et al. (8) evaluated 188 patients (fully), and Brichard et al. (7) evaluated 36 patients with unilateral non-familial Rb. All authors concluded that contrary to perception, age at presentation for children with unilateral Rb does not correlate with the presence or absence of a germline RB1 mutation.
To evaluate this finding in our cohort of patients, we retrospectively evaluated 182 patients diagnosed with unilateral non-familial Rb who underwent genetic testing. In total, 47% of patients were Hispanic with non-Hispanic groups as the minorities: 17% White, 13% Asian/Pacific Islander, 6% Black, and 17% Other. In line with previously published literature on Rb, the average age at diagnosis for these children with unilateral disease was 23 months. Furthermore, 18% of unilateral patients harbored a germline RB1 mutation, which is again similar to previous investigations. In identifying the germline RB1 mutation in the peripheral blood of these 32 patients, slightly more than half (56%) of these patients were diagnosed between 1 and 24 months of age and 44% were diagnosed after 24 months of age. The oldest child with a positive germline mutation and unilateral Rb was 120 months of age at presentation (Figure 1). Thus, our results corroborate the findings of previous studies of genetic positivity with unilateral Rb in determining that age at diagnosis does not correlate with the genetic status in unilateral Rb (7–9). In our cohort, the wide range of ages of patients rendered age a poor predictor of RB1 status. Our patients were found to have RB1 mutations well after the age of 24 months, and in fact one child in our series was diagnosed with unilateral Rb with a positive RB1 mutation (27% mosaic status) at 10 years (120 months) of age. As expected, mosaicism was more common in older children presenting with unilateral disease; however, this too was not significant.
Figure 1.
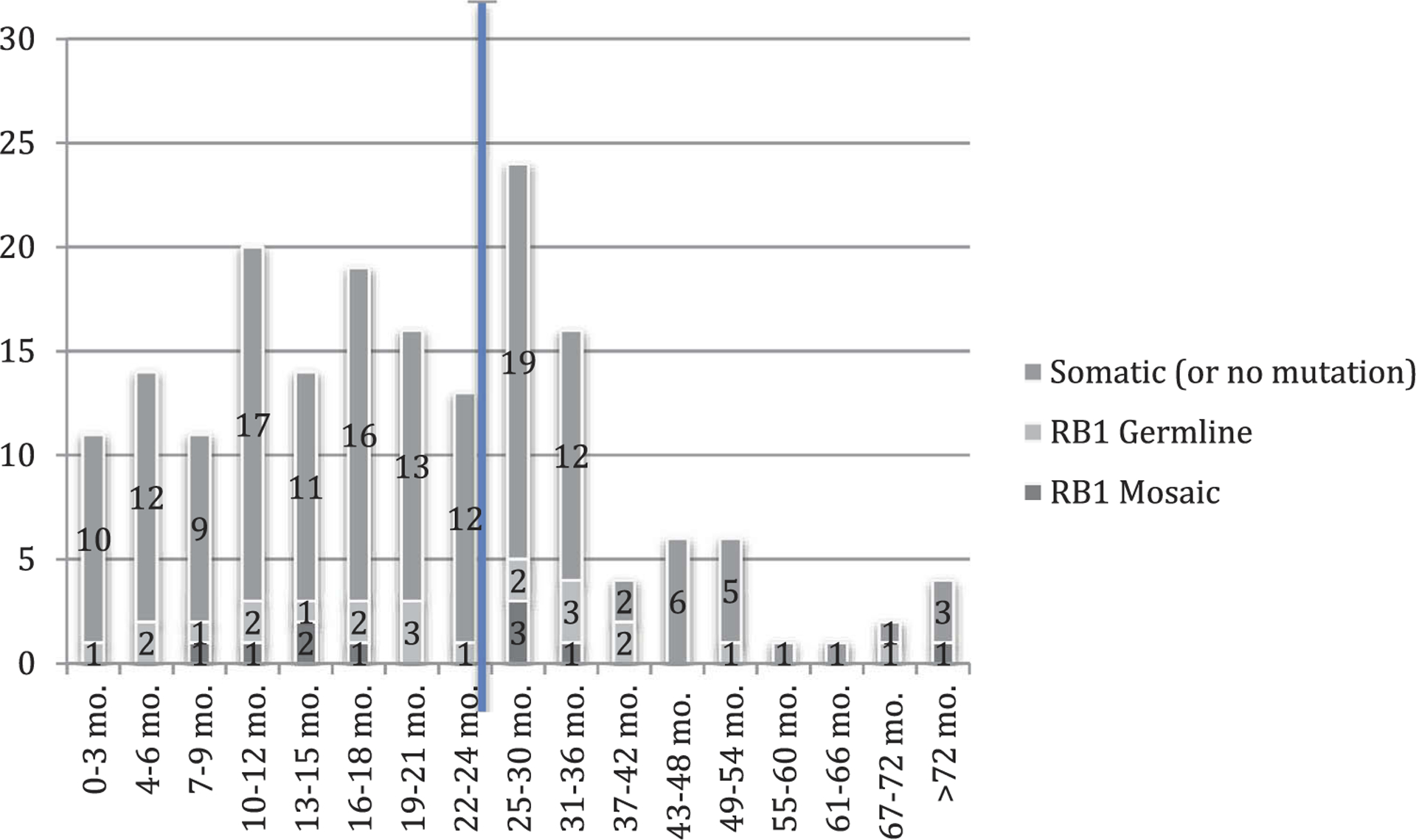
Incidence of RB1 mutations by age for children with unilateral non-familial retinoblastoma.
Our results are one of the largest cohorts to date and are reported from a largely Hispanic population of patients (47% Hispanic, with the next largest group as 17%). The results are consistent with previous reports, thus further demonstrating that a younger age at diagnosis does not identify patients with isolated unilateral Rb who have a higher risk of harboring an RB1 gene mutation. Age at diagnosis should not be used to stratify the risk for the presence of a germline mutation in the setting of unilateral Rb. Particularly given the ease and accessibility of testing of the RB1 gene, all children with unilateral Rb should undergo genetic testing as a means to risk stratify future ocular and non-ocular disease for the patient and their families.
References
- 1.Theriault BL, Dimaras H, Gallie BL, Corson TW. The genomic landscape of retinoblastoma: a review. Clin Exp Ophthalmol 2014;42(1):33–52. doi: 10.1111/ceo.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knudson AG Jr. Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci U S A 1971;68(4):820–23. doi: 10.1073/pnas.68.4.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dimaras H, Corson TW, Cobrinik D, et al. Retinoblastoma. Nat Rev Dis Primers 2015; (In Press). doi: 10.1038/nrdp.2015.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strong LC, Knudson AG Jr. Letter: second cancers in retinoblastoma. Lancet 1973;2(7837):1086. doi: 10.1016/S0140-6736(73)92691-3. [DOI] [PubMed] [Google Scholar]
- 5.Abramson DH. Second nonocular cancers in retinoblastoma: a unified hypothesis. The Franceschetti Lecture. Ophthalmic Genet 1999;20(3):193–204. doi: 10.1076/opge.20.3.193.2284. [DOI] [PubMed] [Google Scholar]
- 6.Abramson DH, Frank CM. Second nonocular tumors in survivors of bilateral retinoblastoma: a possible age effect on radiation-related risk. Ophthalmology 1998;105(4):573–79. discussion 9–80. doi: 10.1016/S0161-6420(98)94006-4. [DOI] [PubMed] [Google Scholar]
- 7.Brichard B, Heusterspreute M, De Potter P, Chantrain C, Vermylen C, Sibille C, Gala JL. Unilateral retinoblastoma, lack of familial history and older age does not exclude germline RB1 gene mutation. Eur J Cancer 2006;42(1):65–72. doi: 10.1016/j.ejca.2005.07.027. [DOI] [PubMed] [Google Scholar]
- 8.Schüler A, Weber S, Neuhäuser M, Jurklies C, Lehnert T, Heimann H, Rudolph G, Jöckel KH, Bornfeld N, Lohmann DR. Age at diagnosis of isolated unilateral retinoblastoma does not distinguish patients with and without a constitutional RB1 gene mutation but is influenced by a parent-of-origin effect. Eur J Cancer 2005;41(5):735–40. doi: 10.1016/j.ejca.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Lohmann DR, Horsthemke B. No association between the presence of a constitutional RB1 gene mutation and age in 68 patients with isolated unilateral retinoblastoma. Eur J Cancer 1999;35(6):1035–36. [DOI] [PubMed] [Google Scholar]


