Abstract
Objective
To explore associations between temperature, humidity and hand, foot and mouth disease (HFMD) incidence in Guangzhou, China from 2013 to 2017.
Methods
A distributed lag non-linear model was applied to estimate the effects of daily temperature and humidity on HFMD incidence after adjusting for long-term trends, seasonal trends, and day of the week.
Results
In total, 353,431 confirmed HFMD cases were reported in Guangzhou over the study period. A bimodal seasonal pattern was observed. High temperatures had acute short-term effects on HFMD incidence that declined quickly over time. The effects of low humidity declined over lag periods, but increased when the humidity surpassed 60.5%. Temperature and humidity were both inversely associated with HFMD incidence during lag days 0 to 3 and with lag periods
Conclusions
Temperature and humidity play important roles in HFMD incidence. These data are important for developing public health strategies.
Keywords: Hand, foot, and mouth disease, temperature, humidity, distributed lag non-linear model, Guangzhou, lag period
Introduction
Hand, foot, and mouth disease (HFMD) is a common infection caused by various enteroviruses. Children under 5 years old are the most susceptible.1 Most patients show a self-limiting illness with symptoms that typically include fever, eruptions on the hands, feet, and buttocks, and oral vesicles.2 However, a small number of patients rapidly develop neurological and systemic complications that can be fatal.3
HFMD has become an endemic childhood disease in East and Southeast Asia, especially in China.4 HFMD has the highest prevalence among all the notifiable infectious diseases in China, and is among the top five infections in terms of associated deaths.5 HFMD poses a serious threat to children’s lives and places a heavy burden on families. At present, there is no effective chemoprophylaxis available for individuals with HFMD.6 Therefore, studies of HFMD epidemiology provide important data for health officials to develop targeted strategies for HFMD control and prevention.
HFMD occurs seasonally in temperate Asia with a summer peak3,4,7–9 and in subtropical Asia with spring and fall peaks.10–16 This seasonal variation suggests that HFMD incidence might be influenced by environmental factors. The relationships between environmental factors and HFMD have been explored in some studies. Several studies found that temperature and humidity had the most significant effects on HFMD infection,17–20 but these results remain controversial. For example. Onozuka and Hashizume found that the weekly number of HFMD cases increased by 11.2% (95% confidence interval [CI]: 3.2–19.8) for every 1°C increase in average temperature and by 4.7% (95% CI: 2.4–7.2) for every 1% increase in relative humidity in Japan.21 Another study from Japan found that the number of days per week with average temperatures >25°C was negatively associated with HFMD incidence and that an increased number of days per week with relative humidity under 90% was negatively associated with HFMD incidence.22
Materials and Methods
Study area
Guangzhou city, the capital of Guangdong Province in southeast China, is 7434 km2 in size and has a population of 14 million.23 The city has a typical monsoon-influenced climate with wet and hot summers and mild and dry winters.
Data sources
HFMD has been classified as a “c” class notifiable disease by the Ministry of Health of China since May 2, 2008. Thus, all cases of HFMD must be reported to the Chinese Information System for Disease Control and Prevention (CISDCP) within 24 hours of diagnosis. In this study, daily HFMD data in Guangzhou city from 1 January 2013 to 31 December 2017 were obtained from the CISDCP. All HFMD cases were confirmed using the unified diagnostic criteria of the Ministry of Health of China.
Meteorological data including daily mean temperature, daily mean relative humidity, and daily rainfall in Guangzhou were obtained from the Daily Report of the Guangzhou Meteorological Bureau over the study period.
Data analysis
As daily counts of HFMD cases typically follow a Poisson distribution, we used Poisson generalized linear regression combined with distributed lag non-linear models (DLNMs) to explore the effects of temperature and humidity on HFMD incidence. In preliminary analyses, we found that the effects of temperature and humidity were negligible for lags above 30 days, so a maximum lag of 30 days was used to explore associations. Three degrees of freedom were used to smooth temperature, humidity and rainfall. Dow was an indicator of the day of the week, and the Trend variable representing the year and calendar month was used to control for seasonality and long-term trends. Holiday was a binary variable and was assigned a value of “1” if day t was a public holiday. The model can be expressed as:
In the model, Yt represents the daily number of HFMD cases on day t; a is the intercept; cb(temperature) or cb(humidity) indicate the cross-basis functions obtained from the DLNM to model non-linear and distributed lag effects on temperature/humidity; and ns was a smooth function based on the natural cubic spline. The Akaike information criterion (AIC) was used to determine the number of degrees of freedom for humidity and lag.
All analyses were carried out using the “dlnm” and “spline” packages in R software version 3.5.2 (www.r-project.org).
Results
From 1 January 2013 to 31 December 2017, 353,431 confirmed HFMD cases were reported in Guangzhou. Of these, 61.07% (215,837) were male patients and 38.93% (137,594) were female patients. The majority (90.98%, 321,550) of cases were under 5 years old, and the seven cases who died were all younger than 5 years old. Descriptive statistics for daily HFMD cases and environmental variables are shown in Table 1. An average of 194 HFMD cases occurred daily over the study period. The average daily weather conditions from 2013 to 2017 were as follows: temperature 22.36°C; relative humidity 78.04%; rainfall 6.55 mm; and wind speed 2.14 m/s.
Table 1.
Daily weather conditions and HFMD cases in Guangzhou, 2013–2017.
| Variable | Minimum | P25 | Median | P75 | Maximum | Mean | SD |
|---|---|---|---|---|---|---|---|
| Mean temperature (°C) | 3.60 | 17.50 | 23.90 | 27.50 | 33.50 | 22.36 | 6.17 |
| Relative humidity (%) | 26.00 | 72.00 | 80.00 | 86.00 | 100.00 | 78.04 | 12.09 |
| Rainfall (mm) | 0.00 | 0.00 | 0.00 | 4.00 | 164.10 | 6.55 | 16.89 |
| Wind speed (m/s) | 0.00 | 2.00 | 2.00 | 3.00 | 7.00 | 2.14 | 0.92 |
| Number of HFMD cases | 1 | 37 | 117 | 325 | 1010 | 194 | 186 |
HFMD, hand, foot and mouth disease; P25, 25th percentile; P75, 75th percentile; SD, standard deviation.
Figure 1 shows daily HFMD cases and mean temperature, relative humidity, wind speed and rainfall over time. Seasonal patterns can be observed. The seasonal peak of HFMD differed from year to year, although it typically occurred during the late spring, early summer and autumn months. The first seasonal peak occurred between April and July, followed by the second peak between September and October.
Figure 1.
Daily distribution of meteorological variables and HFMD cases in Guangzhou, 2013–2017.
HFMD, hand, foot and mouth disease.
Figure 2 shows the three-dimensional relationship between daily mean temperature, daily relative humidity and HFMD incidence over 30 lag days. Overall, the estimated effects of temperature and humidity on HFMD incidence were non-linear, with larger relative risks (RRs) at high temperature and high humidity.
Figure 2.
Three-dimensional plot of the relationships between mean temperature, mean relative humidity and HFMD cases over 30 lag days.
HFMD, hand, foot and mouth disease.
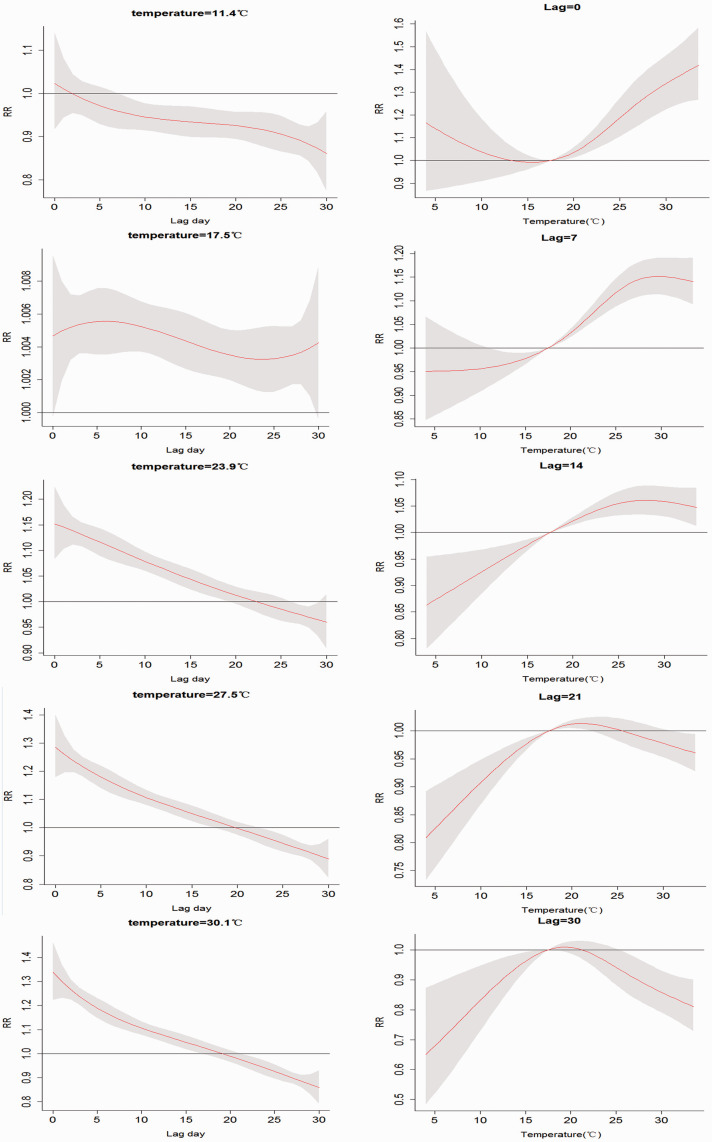
Figure 3 shows the RR by temperature at specific lags (0, 7, 14, 21, and 30 days) and at specific temperatures (11.4°C, 17.5°C, 23.9°C, 27.5°C, and 30.1°C) corresponding approximately to the 5th, 25th, 50th, 75th, 95th percentiles of temperature distribution. High temperatures had acute short-term effects on the RR that declined quickly over time lags, while the effects of low temperature ranges persisted over longer lag periods. During lag days 0 to 3, the effects of temperature on RR decreased to a minimum and then began to increase. The effects then peaked and then decreased over lag days 4 to 30.
Figure 3.
Plot of relative risk (RR) according to temperature at specific lags (left), and RR according to lag at specific temperatures (right).
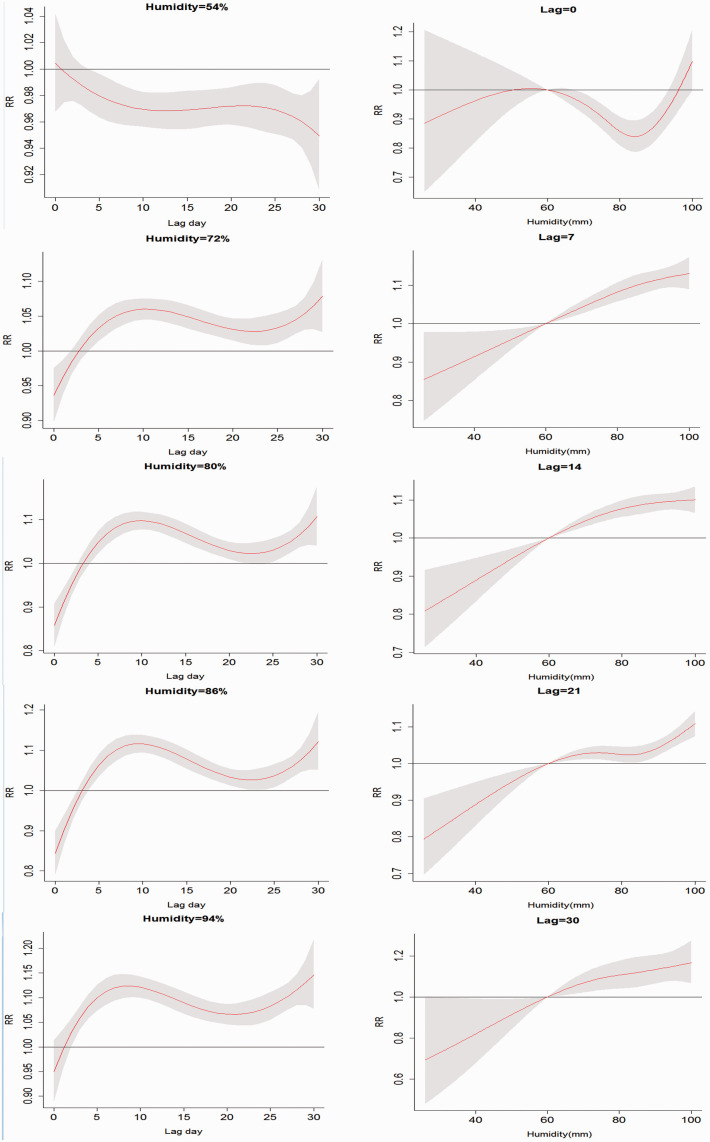
Figure 4 shows the RR by temperature at specific lags (0, 7, 14, 21, and 30 days) and at specific relative humidities (54%, 72%, 80%, 86%, and 94%) corresponding approximately to the 5th, 25th, 50th, 75th, and 95th percentiles of humidity distribution. The effects of low humidity declined over lag periods, but increased when the humidity surpassed 60.5%. The effects of humidity over lag days 0 to 3 days were persistent, while past lag day 4, the effects kept increasing as humidity increased.
Figure 4.
Plot of relative risk (RR) according to relative humidity at specific lags (left), and RR according to lag at specific relative humidities (right).
Figure 5 summarizes the estimated overall effects of temperature on HFMD risk by gender and age group over the 30 lag days. The overall effect of temperature on the RR of HFMD did not depend on gender: the R increased with increasing temperature, reaching a peak at 27.5°C, then began to decrease. However, the effects of temperature differed by age group. The overall effect of temperature on the RR of HFMD in cases of 0- to 2-year-olds increased with increasing temperature and then increased slowly for temperatures above 27.5°C. By contrast, the effect of temperature in cases of 3- to 5-year-olds and patients more than 5 years old increased and then sharply declined for temperatures above 27.5°C.
Figure 5.
Temperature dependence of relative risks (RRs) of HFMD infection by gender and age group over 30 lag days.
HFMD, hand, foot and mouth disease.
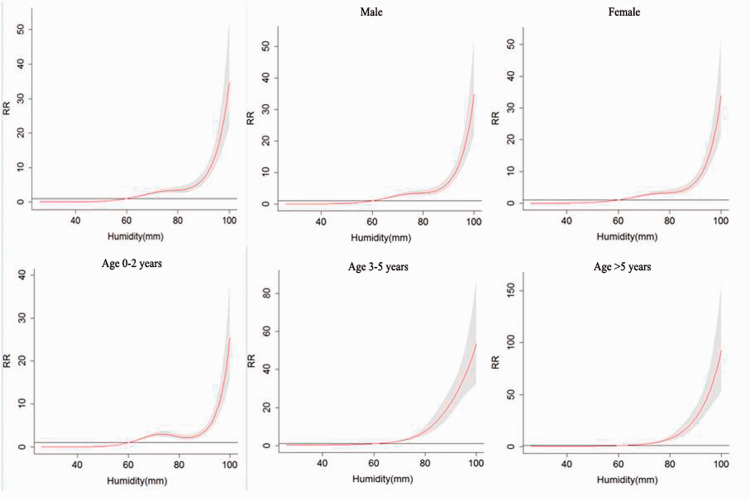
Figure 6 summarizes the estimated overall effects of humidity on HFMD risk by gender and age group over the 30 lag days. The overall effect of humidity on the incidence of HFMD did not depend on gender: the effect increased gradually with increasing relative humidity but then much more acutely for humidity over 90%. The pattern for HFMD cases of 0- to 2-year-olds was similar. By contrast, the effect of humidity on the RR of HFMD in cases of 3- to 5-year olds and patients more than 5 years old increased more slowly for humidity above 90%.
Figure 6.
Humidity-dependence of relative risks (RRs) of HFMD infection by gender and age group over 30 lag days.
HFMD, hand, foot and mouth disease.
Discussion
In this study, a DLNM was used to investigate the temporal associations between daily temperature, daily humidity and daily HFMD cases from 2013 to 2017 in Guangzhou, China. Descriptive analyses showed that there were two peaks per year: the first peak occurred in late spring and early summer, followed by the second peak in autumn. These seasonal patterns were similar to those found in South China and in other countries in subtropical Asia.10–16
We observed that the effects of temperature on HFMD incidence were nonlinear. A DLNM showed that HFMD cases increased with increasing temperature and humidity. Temperature had acute short-term effects on the RR of HFMD, which declined quickly over time lags when the temperature exceeded 20°C. When the temperature surpassed 27.5°C, increasing temperature was negatively associated with the incidence of HFMD. The RR of HFMD increased when the humidity surpassed 60.5%. The RR of HFMD increased gradually with increasing humidity until humidity exceeded 90%, when the RR increased acutely
Enteroviruses can survive for a long time, especially at low temperatures (−20°C). However, the virulence and transmission of enteroviruses under ambient conditions are mainly influenced by temperature and relative humidity.24 Enteroviruses are sensitive to temperature and humidity, and some studies performed in the laboratory showed that the virus survives at 20°C slightly better than at 25°C; similarly, a humidity of 80% may promote survival compared with a humidity of 60%. These results are consistent with our findings concerning the effect of temperature on HFMD incidence.25–27 However, too high or too low temperatures could also affect HFMD incidence by modifying the physical activity of children. We found that there were more male HFMD cases than female cases; this would be expected if boys were more active than girls and thus more likely to be exposed to enterovirus.
Most HFMD cases were under 5 years old. We found that children 0 to 2 years old were more affected by temperature and humidity changes in HFMD risk, perhaps because of their partially developed immune systems. Younger children especially may reduce their outdoor physical activities at higher or lower temperatures, and thus avoid contact with other children. Children older than 6 years may spend most of their time at school, and their physical activities are less affected by temperature.28,29 HFMD is transmitted mainly by close contact and the fecal–oral route. A previous study showed that sharing of toys and other objects among children might contribute to enterovirus transmission. Enterovirus could easily adhere to small particles in the air or on toys and subsequently be transmitted.27,29 However, the potential mechanisms need to be confirmed in future studies.
In this study, we also found that increasing temperature and humidity were inversely associated with HFMD during lag days 0 to 3 and at later lag days. During lag days 0 to 3, the effects decreased to a minimum and then began to increase. The effects then peaked and subsequently decreased during lag days 4 to 30. The effects of humidity on lag days 0 to 3 were persistent, while beyond 4 days lag, the effects increased as the humidity increased. The difference effects of lag days were similar those identified in previous studies. Although the mechanism underlying this phenomenon was unclear, positive associations at longer lag days might be more biologically plausible. The 2- to 10-day incubation period of HFMD might also result in the observed effects at later lag days.29,30
Compared with most studies investigating the effects of temperature and humidity on HFMD incidence using monthly or weekly data, our results may be more accurate. Analyses of the effects of temperature and humidity on HFMD incidence using daily data could be more suitable for HFMD control and prevention. However, our study had some limitations. The results may have been influenced by the biological characteristics of enterovirus, but the absence of laboratory confirmed information on HFMD cases prevented further analyses. Furthermore, our study was preliminary and exploratory. Therefore, we could not exclude the possibility of unmeasured confounding factors that may be associated with temperature, humidity and HFMD incidence.
In conclusion, our study suggests that temperature and humidity may be important factors affecting HFMD transmission in Guangzhou. Our data revealed non-linear relationships between daily temperature and humidity and HFMD incidence in Guangzhou city, and provide a better understanding of the effect of temperature and humidity variation on HFMD incidence. More consideration of temperature, humidity and other environmental conditions on HFMD incidence is important for HFMD interventions as well as control and prevention strategies.
Abbreviations
HFMD: Hand, foot, and mouth disease
DLNM: Distributed lag non-linear model
CISDCP: System for Disease Control and Prevention
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics statement
Data were collected from the Chinese Information System for Disease Control and Prevention (CISDCP) and the Daily Report of the Guangzhou Meteorological Bureau as part of government-mandated health surveillance programs. All data were analyzed anonymously so ethical approval was not needed.
Funding
This work was supported by The Project for Key Medicine Discipline Construction of Guangzhou Municipality (grant number 2017-2019-07); the Medical Science Foundation of Guangdong (grant number B201849); the Medical Science and Technology Research of Guangdong Province (grant number A2016056); the Science and Technology Program of Guangzhou (grant number 201707010451); and the Major Projects of the Guangzhou Municipal Health and Family Planning Commission (grant number 2018A031002).
ORCID iD
Chun Chen https://orcid.org/0000-0001-8336-8844
References
- 1.Ho M, Chen ER, Hsu KH, et al. An epidemic of enterovirus 71 infection in Taiwan. Taiwan Enterovirus Epidemic Working Group. N Engl J Med 1999; 341: 929–935. [DOI] [PubMed] [Google Scholar]
- 2.McMinn PC. An overview of the evolution of enterovirus 71 and its clinical and public health significance. FEMS Microbiol Rev 2002; 26: 91–107. [DOI] [PubMed] [Google Scholar]
- 3.Chang LY, Huang LM, Gau SS, et al. Neurodevelopment and cognition in children after enterovirus 71 infection. N Engl J Med 2007; 356: 1226–1234. [DOI] [PubMed] [Google Scholar]
- 4.Koh WM, Bogich T, Siegel K, et al. The epidemiology of hand, foot and mouth disease in Asia. Pediatr Infect Dis J 2016; 35: e285–e300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Health and Family Planning Commission. National notifiable infectious disease report. (2016-05-01)[2017-04-01]. http: //www.moh.gov.cn/jkj/. (in Chinese)
- 6.Zheng Y, Yang J. Estimation of social economic burden caused by fatal hand, foot and mouth disease in China, 2013-2015. Disease Surveillance 2017. (in Chinese)
- 7.Liu Y, Wang X, Liu Y, et al. Detecting spatial-temporal clusters of HFMD from 2007 to 2011 in Shandong Province, China. PLoS One 2013; 8: e63447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tagaya I, Tachibana K. Epidemic of hand, foot and mouth disease in Japan, 1972–1973: difference in epidemiologic and virologic features from the previous one. Jpn J Med Sci Biol 1975; 28: 231–234. [DOI] [PubMed] [Google Scholar]
- 9.Baek K, Yeo S, Lee B, et al. Epidemics of enterovirus infection in Chungnam Korea, 2008 and 2009. Virol J 2011; 8: 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma E, Lam T, Chan KC, et al. Changing epidemiology of hand, foot, and mouth disease in Hong Kong, 2001–2009. Jpn J Infect Dis 2010; 63: 422–426. [PubMed] [Google Scholar]
- 11.Deng T, Huang Y, Yu S, et al. Spatial-temporal clusters and risk factors of hand, foot, and mouth disease at the district level in Guangdong Province, China. PLoS One 2013; 8: e56943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang TT, Huang LM, Lu CY, et al. Clinical features and factors of unfavorable outcomes for non-polio enterovirus infection of the central nervous system in northern Taiwan, 1994-2003. J Microbiol Immunol Infect 2005; 38: 417–424. [PubMed] [Google Scholar]
- 13.Chatproedprai S, Theanboonlers A, Korkong S, et al. Clinical and molecular characterization of hand-foot-and-mouth disease in Thailand, 2008-2009. Jpn J Infect Dis 2010; 63: 229–233. [PubMed] [Google Scholar]
- 14.Tu PV, Thao NTT, Perera D, et al. Epidemiologic and virologic investigation of hand, foot, and mouth disease, southern Vietnam, 2005. Emerg Infect Dis 2007; 13: 1733–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee TC, Guo HR, Su HJJ, et al. Diseases caused by enterovirus 71 infection. Pediatr Infect Dis J 2009; 28: 904–910. [DOI] [PubMed] [Google Scholar]
- 16.Podin Y, Gias EL, Ong F, et al. Sentinel surveillance for human enterovirus 71 in Sarawak, Malaysia: lessons from the first 7 years. BMC Public Health 2006; 6: 180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hii YL, Rocklov J, Ng N. Short term effects of weather on hand, foot and mouth disease. PLoS One 2011; 6: e16796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ma E, Lam T, Wong C, et al. Is hand, foot and mouth disease associated with meteorological parameters? Epidemiol Infect 2010; 13: 1779–1788. [DOI] [PubMed] [Google Scholar]
- 19.Wei J, Hansen A, Liu Q, et al. The effect of meteorological variables on the transmission of hand, foot and mouth disease in four major cities of Shanxi Province, China: a time series data analysis (2009–2013). PLoS Negl Trop Dis 2015; 9: e0003572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang Y, Deng T, Yu S, et al. Effect of meteorological variables on the incidence of hand, foot, and mouth disease in children: a time-series analysis in Guangzhou, China. BMC Infect Dis 2013; 13: 134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Onozuka D, Hashizume M. The influence of temperature and humidity on the incidence of hand, foot, and mouth disease in Japan. Sci Total Environ 2011; 410–411: 119–125. [DOI] [PubMed] [Google Scholar]
- 22.Urashima M, Shindo N, Okabe N. Seasonal models of herpangina and hand-foot-mouth disease to simulate annual fluctuations in urban warming in Tokyo. Jpn J Infect Dis 2003; 56: 48–53. [PubMed] [Google Scholar]
- 23.Guangzhou administrative area and population density[EB/OL]. People’s Government of Guangdong Province: http: //www.gddata.gov.cn/index.php/data/datasetdetail/id/1803.html
- 24.Guangzhou administrative area and population density[EB/OL]. People’s Government of Guangdong Province: http://gddata.gd.gov.cn/data/dataSet/toDataDetails/29000 02700479.
- 25.Pourcher AM, Françoise PB, Virginie F, et al. Survival of fecal indicators and enteroviruses in soil after land-spreading of municipal sewage sludge. App Soil Ecol 2007; 35: 473–479. [Google Scholar]
- 26.Fujioka RS, Loh PC, Lau LS. Survival of human enteroviruses in the Hawaiian Ocean environment: evidence for virus-inactivating microorganisms. Appl Environ Microbiol 1980; 39: 1105–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cai Y, Jiang L, Shi Y, et al. Survey on enterovirus 71 survival ability on different surfaces under different climate. Chin J Infect Dis 2012; 30: 398–401. (in Chinese) [Google Scholar]
- 28.Suminski RR, Poston WC, Market P, et al. Meteorological conditions are associated with physical activities performed in open-air settings. Int J Biometeorol 2008; 52: 189–197. [DOI] [PubMed] [Google Scholar]
- 29.Chen C, Lin H, Li X, et al. Short-term effects of meteorological factors on children hand, foot and mouth disease in Guangzhou, China. Int J Biometeorol 2013; 58: 1605–1614. [DOI] [PubMed] [Google Scholar]
- 30.Yong H, Deng T, Yu S, et al. Effect of meteorological variables on the incidence of hand, foot, and mouth disease in children: a time-series analysis in Guangzhou, China. BMC Infect Dis 2013; 13: 134. [DOI] [PMC free article] [PubMed] [Google Scholar]