Abstract
Objectives:
To determine whether diagnosed pre-existing health conditions correlate with Kratom demographics and use patterns.
Methods:
A cross-sectional, anonymous US national online survey was conducted among 8049 Kratom users in October, 2016 to obtain demographic, health, and Kratom use pattern information.
Results:
People who use Kratom to mitigate illicit drug dependence self-reported less pain and better overall health than individuals who used Kratom for acute/chronic pain. Self-reported improvements in pre-existing mental health symptoms (attention deficit and hyperactivity disorder/attention deficit disorder, anxiety, bipolar disorder, post-traumatic stress disorder, and depression) attributed to Kratom use were greater than those related to somatic symptoms (back pain, rheumatoid arthritis, acute pain, chronic pain, fibromyalgia). Demographic variables, including female sex, older age, employment status, and insurance coverage correlated with increased likelihood of Kratom use.
Conclusions:
Kratom use may serve as a self-treatment strategy for a diverse population of patients with pre-existing health diagnoses. Healthcare providers need to be engaging with patients to address safety concerns and potential limitations of its use in clinical practice for specific health conditions.
Keywords: health impact, Kratom, Mitragyna speciosa, opioid
Kratom (Mitragyna speciosa Korth.)—a tree native to Southeast Asia—continues to be investigated for its use as a herbal self-treatment for various health maladies. Traditionally, the fresh leaves are either chewed briefly to provide a stimulant effect, or are ingested after longer steaming and brewing, to provide a relaxing and mild sedative effect (Ahmad and Aziz, 2012; Singh et al., 2016). Although the pharmacology of the complex composition of Kratom is not entirely understood, the focus of current research is on the activity of the alkaloids mitragynine and 7-hydroxymitragynine that bind to opioid receptors as partial agonists. Their mechanism has been distinguished from classical opioids such as morphine, in that they present with G-protein-biased signaling at the opioid receptors and do not recruit beta-arrestin 2, which may be responsible for many of the adverse effects associated with classical opioid use (Kruegel et al., 2016). The alkaloids have been shown to bind to multiple receptors such as serotonergic and adrenergic receptors, but it remains unclear how this contributes to the effects of the overall leaf extract (Boyer et al., 2008). Furthermore, the alkaloid 7-hydroxymitragynine is absent in many products, and, if present, occurs at such low levels in natural leaf products to contribute significantly, if at all, to Kratom’s effects—desired or undesired.
The potential beneficial health effects associated with Kratom use include antidepressant (Idayu et al., 2011), anti-inflammatory (Shaik Mossadeq et al., 2009), analgesic, muscle-relaxant, and anorectic activity (Prozialeck et al., 2012; Hassan et al., 2013) that are, to date, based on case reports, preclinical animal studies, and derived from its traditional use in Southeast Asia. One review reported that people have used Kratom to self-treat anxiety and mood disorders (Swogger and Walsh, 2018). Among regular Kratom users, the powdered leaf is more frequently used to enhance overall feelings of well-being (30%), increase energy and alertness (29%−84%), or increase focus (70%) (Swogger et al., 2015; Grundmann, 2017). The initial analysis of the online survey dataset used for this study found that 67% of survey respondents used Kratom for the self-treatment of a mental or emotional condition, of which approximately 80% reported a less depressed or less anxious mood (Grundmann, 2017).
Presently, the medical and legal community is concerned about the effects of Kratom use, because Kratom is claimed to be addictive and produce adverse effects with prolonged use (Suwanlert, 1975; McWhirter and Morris, 2010; Khazaeli et al., 2018). Despite its habit-forming properties, long-term Kratom use did not appear to alter the hematology and biochemical parameters of people who regularly used it in a traditional context (Singh et al., 2018). Several case reports have shown that users tend to develop dependence when Kratom is excessively used in higher doses to self-manage opioid withdrawal (Hassan et al., 2013; Galbis-Reig, 2016). However, preliminary research investigating motives for Kratom use among people who use multiple drugs in the United States has found that people with extensive substance misuse histories did not prefer Kratom as an addictive drug, compared with heroin, prescription opioids, or Suboxone, indicating the possibility that Kratom’s dependence potential may be comparatively lower (Smith and Lawson, 2017). However, some evidence suggests that regular Kratom consumption may subtly impair cognition by affecting visual memory and new learning among some people who use it (Singh et al., 2015). Though people who have used Kratom developed dependence, they never viewed their habitual Kratom use as a hindrance to their daily functioning (Ahmad and Aziz, 2012; Singh et al., 2019).
Aims
The aim of this investigation was to analyze additional data collected as part of an anonymous online survey which was conducted in 2016 (Grundmann, 2017) among current Kratom users for the purposes of identifying the relationship between Kratom use, self-reported overall health, pain severity, and demographic characteristics. A related aim included documenting the self-reported perceived effectiveness of Kratom in self-treating diagnosed health conditions and symptoms depending on the intended Kratom use for illicit or prescription drug dependence, acute or chronic pain, and mental or emotional conditions.
METHODS
Data Collection
From October 2 to October 26, 2016, 10,000 responses were collected using an online anonymous survey format in a cross-sectional manner. The survey was made available through the website of the American Kratom Association (http://www.americankratom.org/) and various social media outlets (Facebook, website forums, membership e-mail distribution) with no incentive and used Qualtrics (Qualtrics, Provo, UT) to collect the data in a secure manner. The protocol followed standard procedures to ensure anonymity of responses by deleting internet protocol addresses at the completion of the survey while preventing ballot box stuffing from the same device. The research was approved by the Institutional Review Board at the University of Florida (IRB #2016–01581) and incorporated a consent form before starting the survey requiring participants to acknowledge they were 18 years or older and participating of their own free will in the study. The survey (Appendix 1) was designed and classified based on common variables used by the CDC Behavioral Risk Factor Surveillance System (BRFSS) (Silva, 2014). Only completed responses (8049 or 80.5%) were included in the data analysis.
Measures
As part of the online survey, respondents were asked to respond to several items.
Demographic characteristics included age, sex, marital status, ethnicity, employment status, insurance coverage, level of education, and annual household income.
Self-rated pain severity, overall health, and change in diagnosed health conditions with Kratom use were measured using a 5-point Likert scale and modified visual face scale as reported in the literature (Garra et al., 2013).
Health diagnoses were measured by asking participants to check from a nonexhaustive list all pre-existing health conditions which were diagnosed by a physician: acute pain, chronic pain, back pain, rheumatoid arthritis, fibromyalgia, anxiety, attention deficit and hyperactivity disorder (ADHD) or attention deficit disorder (ADD), bipolar disorder, depression, post-traumatic stress disorder (PTSD), substance use disorder (SUD), no medical condition diagnosed, or other.
Kratom use conditions included 4 nonexclusive motivations for Kratom use, whereby respondents reported using Kratom to address or self-treat 1 or more of the following: illicit drug dependence, prescription drug dependence, acute or chronic pain, and mental/emotional conditions.
Data Analysis
The data were analyzed in Microsoft Excel 2013 (version 15.0, Microsoft, Seattle, WA) and GNU PSPP (http://www.gnu.org/software/pspp/, version 0.10.4-g50f7b7). Chi-square analysis was applied for level comparison among nominal and ordinal variables against expected values with Pearson chi-square statistics for nominal variables (eg, sex, marital status, employment, ethnicity, and insurance) and linear-by-linear statistics for ordinal variables (eg, age, education, and income) for significance determination. Binomial logistic regression was used to compare levels of variables against a reference level to obtain odds ratios (ORs) and 95% confidence intervals (CIs). Significance was set at the 0.05 level.
RESULTS
Demographic Characteristics
Respondent demographic characteristics are displayed in Table 1. The majority of the respondents (72%) were 31 years and older. More than half were married or partnered (54%), male (57%), employed (57%), and described themselves as white non-Hispanics (89%). Insurance type and educational attainment was diverse, with close to half (47%) receiving health insurance through their employer and 35% holding a Bachelor degree or higher. Household income was variable, with about two-thirds of respondents (63%) making at least $35,000 annually (Table 1).
TABLE 1.
Demographics of People Who Use Kratom
| Frequency | Percent | Frequency | Percent | ||
|---|---|---|---|---|---|
| Age* | Insurance coverage* | ||||
| 18–20 yrs (+) | 212 | 2.63 | Private insurance through employer (+) | 3808 | 47.31 |
| 21–30 yrs | 2038 | 25.32 | Private insurance through self-insurance | 1127 | 14 |
| 31–40 yrs | 2788 | 34.64 | Medicaid | 650 | 8.08 |
| 41–50 yrs | 1646 | 20.45 | Medicare or Medicare & supplement | 620 | 7.7 |
| 51–60 yrs | 966 | 12 | No insurance | 1134 | 14.09 |
| 61 yrs and older | 391 | 4.86 | Other | 404 | 5.02 |
| Do not wish to answer | 8 | 0.1 | Do not wish to answer | 306 | 3.8 |
| Sex* | Education* | ||||
| Female | 3468 | 43.09 | Did not complete high school (+) | 112 | 1.39 |
| Male (+) | 4581 | 56.91 | High school graduate or equivalent | 1269 | 15.77 |
| Marital status* | Some college (eg, AA, AS, or no degree) | 3785 | 47.02 | ||
| Single/never married (+) | 2612 | 32.45 | Bachelor degree (eg, BA, BS, AB) | 2013 | 25.01 |
| Married | 3639 | 45.21 | Advanced degree (eg, MBA, MS, PhD, JD, MD) | 828 | 10.29 |
| Partnered | 728 | 9.04 | Do not wish to answer | 42 | 0.52 |
| Divorced | 964 | 11.98 | |||
| Widowed | 106 | 1.32 | |||
| Ethnicity* | Household income* | ||||
| Black or African- American | 61 | 0.76 | Less than $20,000 (+) | 944 | 11.73 |
| American Indian or Alaska Native | 97 | 1.21 | $20,000–$24,999 | 681 | 8.46 |
| Asian | 95 | 1.18 | $25,000–$34,999 | 897 | 11.14 |
| Hispanic or Latino/a | 275 | 3.42 | $35,000–$49,999 | 1248 | 15.51 |
| White (non-Hispanic) (+) | 7195 | 89.39 | $50,000–$74,999 | 1534 | 19.06 |
| Other | 164 | 2.04 | $75,000 or more | 2308 | 28.67 |
| Do not wish to answer | 162 | 2.01 | Do not wish to answer | 437 | 5.43 |
| Employment status* | |||||
| Employed for wages (+) | 4574 | 56.83 | |||
| Self-employed | 1210 | 15.03 | |||
| Out of work for 1 yr or more | 124 | 1.54 | |||
| Out of work for less than 1 yr | 107 | 1.33 | |||
| Homemaker | 498 | 6.19 | |||
| Student | 455 | 5.65 | |||
| Retired | 288 | 3.58 | |||
| Unable to work | 683 | 8.49 | |||
| Do not wish to answer | 110 | 1.37 |
Chi-square test was used to compare groups with P < 0.05 as significance level.
P < 0.001 versus comparator group indicated by (+).
Pain Severity
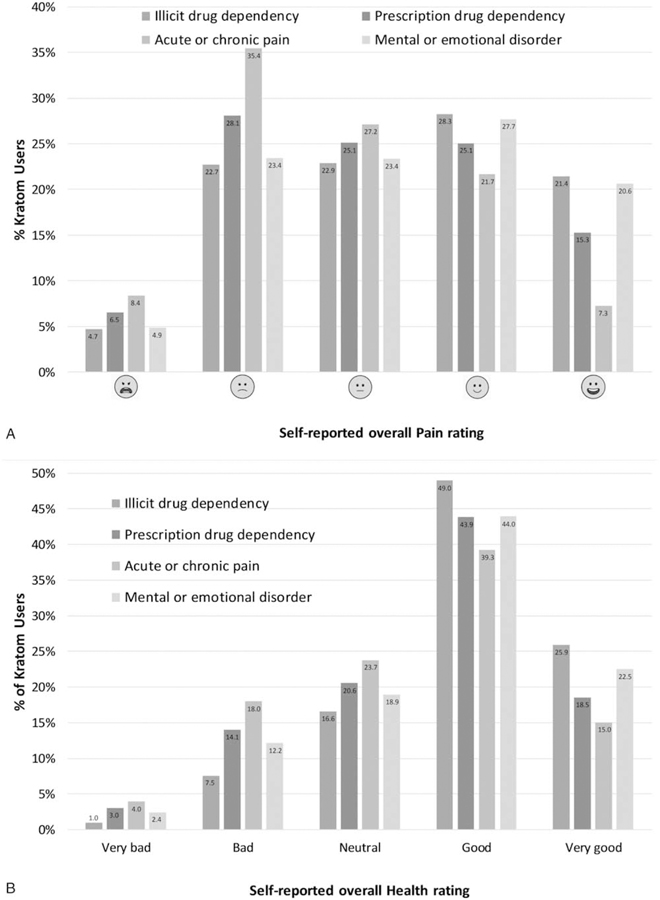
Participants who took Kratom for illicit drug dependency or a mental/emotional health condition had lower pain severity scores, with 49.7% and 48.3% reporting “somewhat good” and “very good” pain rating, respectively. Just over 40% of respondents who used Kratom for prescription drug dependency rated their pain as “good” or “very good,” whereas only 29% of respondents who took Kratom to self-treat acute or chronic pain rated their pain as “good” or “very good” (Fig. 1A).
FIGURE 1.
(A) Self-reported pain rating by Kratom use condition. (B) Self-reported overall health rating by Kratom use condition. All values in percent of total respondents who used Kratom for this condition, multiple responses allowed (n = 598 for illicit drug dependence, n = 2007 for prescription drug dependence, n = 5348 for acute/chronic pain, n = 5213 for mental/emotional condition).
Current Health Condition
In contrast to self-reported pain specifically, respondents rated their overall current health as generally favorable, “good,” or “very good,” for all 4 Kratom use conditions. The lowest rating was among respondents using Kratom for acute or chronic pain (54.3%), followed by those using Kratom for prescription drug dependency (62.4%) or a mental/emotional health condition (66.5%) (Fig. 1B). Those taking Kratom for an illicit drug dependency reported the best overall health, with 74.9% reporting “good” or “very good” health.
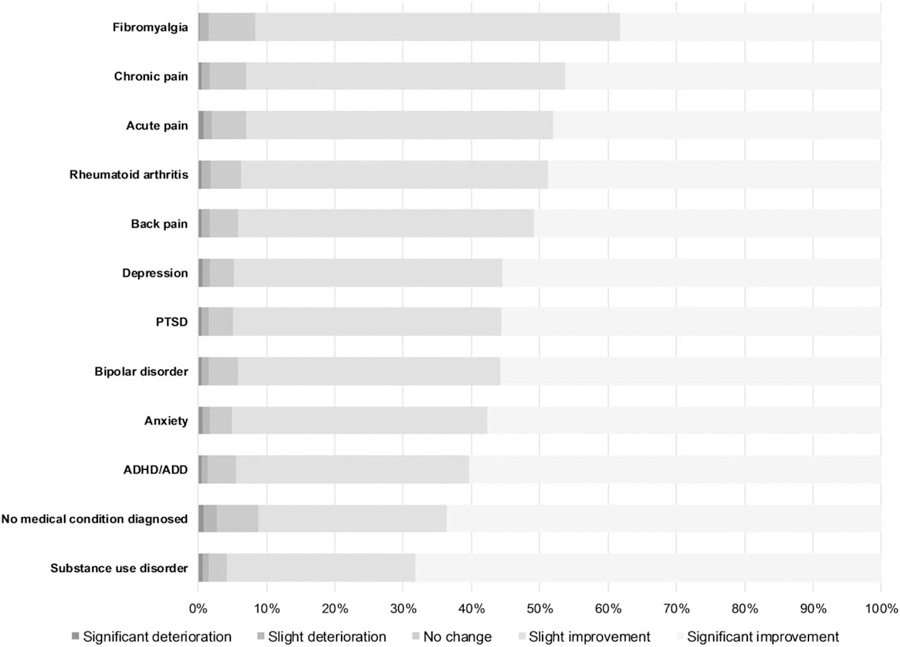
For changes in medical condition severity since initiating Kratom use, chi-square analysis identified slight or significant improvement across each condition (P < 0.001) (Fig. 2). The percentage of “significant improvement” was highest for respondents with SUDs (63.6%) and no diagnosed medical condition (68.2%), whereas it was lowest among respondents with fibromyalgia (38.2%) and chronic pain (46.2%). The self-perceived “slight” or “severe deterioration” in any health condition was <3.0%.
FIGURE 2.
Percent distribution of Likert scale responses to self-perceived changes in diagnosed health conditions.
Relationship Between Kratom Use and Demographic Variables
Demographic variables were compared for all Kratom use conditions (eg, use for acute or chronic pain, illicit drug dependency, etc). Intended Kratom use was statistically significantly correlated with several demographic variables (Fig. 3). For somatic health conditions (fibromyalgia, chronic pain, acute pain, rheumatoid arthritis, and back pain), employment, marital status, age, sex, and insurance were frequently correlated with significant differences among Kratom uses. Respondents who were unable to work or who were unemployed were more likely to use Kratom for any of the 4 uses if they had also been diagnosed with any of the somatic health conditions. Similarly, married or partnered respondents were more likely to be diagnosed with a somatic health condition. There were also significant correlations found between age and somatic health conditions dependent on the Kratom use condition, except for illicit drug dependence (Fig. 3A).
FIGURE 3.
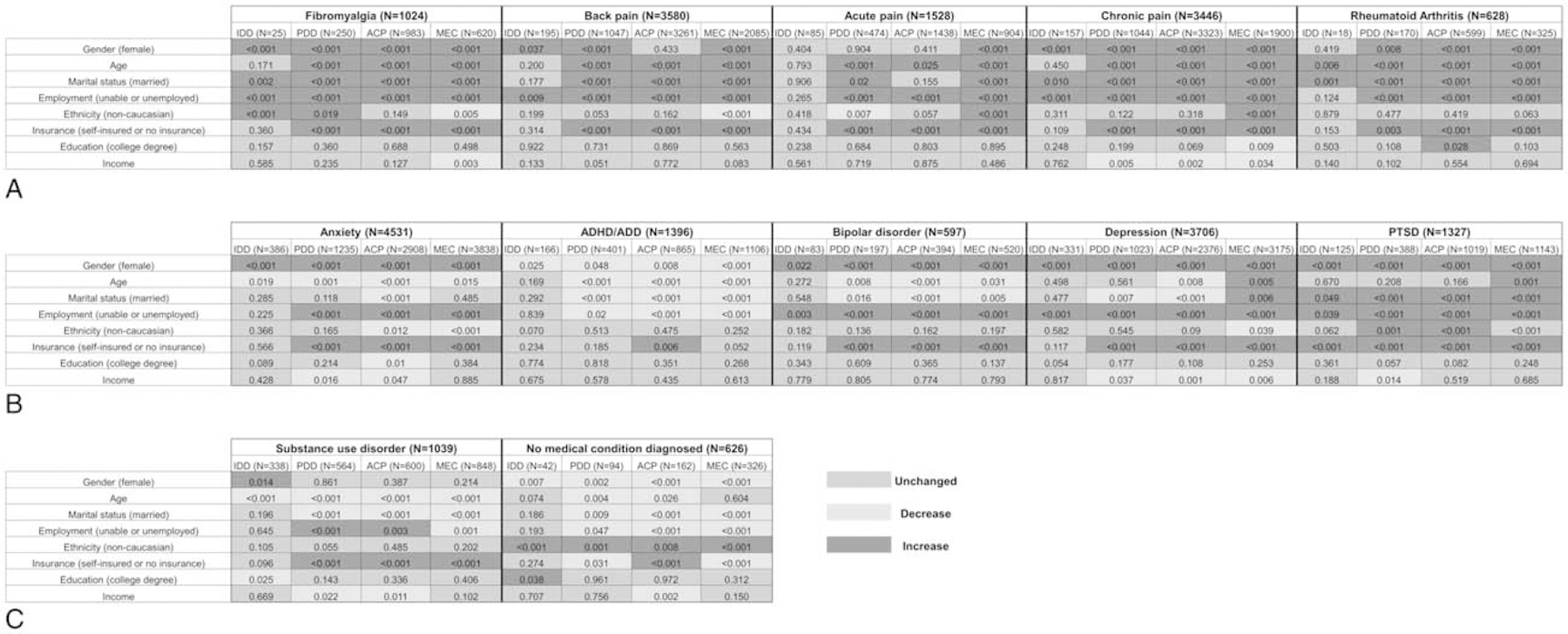
(A) Correlation of demographic variables with diagnosed somatic health conditions. (B) Correlation of demographic variables with diagnosed mental health conditions. (C) Correlation of demographic variables with a diagnosed SUD or no medical condition. All correlations used a Pearson chi-square test for nominal or linear-by-linear statistic for ordinal variables at a significance level of P < 0.05.
Education and income showed the fewest correlations with somatic health conditions. For respondents using Kratom for a mental/emotional condition or acute/chronic condition who were also diagnosed with chronic pain, a higher educational degree was correlated with decreased likelihood (P = 0.009) to use Kratom (Fig. 3A). Conversely, those who were using Kratom for acute/chronic pain with a diagnosis of rheumatoid arthritis were more likely (P = 0.028) to have higher educational attainment. Household income, in all 4 instances where it was significant, demonstrated a graded relationship with Kratom use, whereby higher income was negatively correlated with increased likelihood to use Kratom (Fig. 3A).
Respondents who were taking Kratom to address an illicit drug dependency differed less demographically (11) than respondents taking Kratom in powdered leaf form for acute or chronic pain (25), a prescription drug dependency (27), or a mental/emotional health condition (32).
Among respondents with diagnosed mental health conditions, the demographic variables that evidenced the strongest correlation with the Kratom use conditions were sex, employment, and marital status (Fig. 3B). While female respondents were more likely to use Kratom across the four use conditions if they had an existing diagnosis of anxiety, bipolar disorder, depression, or PTSD, men were more likely to use Kratom if they were diagnosed with ADHD/ADD. Participants who were unable to work/unemployed were more likely to use Kratom for any reason if diagnosed with any of the mental health conditions (Fig. 3B), with the exception of ADHD/ADD, in which case participants who were unable to work/unemployed were less likely to use Kratom. Greater variance was found among married and/or partnered respondents who used Kratom based on diagnosed health condition. For instance, while married and partnered respondents were generally less likely to use Kratom for anxiety, ADHD/ADD, bipolar disorder, or depression, they were more likely to use it for PTSD (Fig. 3B).
Similar to diagnosed somatic disorders, respondents who used Kratom for self-treatment of an illicit drug dependency evidenced the fewest demographic differences (11). Conversely, greater demographic heterogeneity was found among respondents who used Kratom to address a prescription drug dependency (25), a mental/emotional condition (26), or acute or chronic pain (30).
For respondents who were diagnosed with a SUD (Fig. 3C), Kratom use significantly decreased as age increased across all Kratom use conditions. Among this group, being married or partnered also decreased the likelihood of Kratom use to self-treat acute/chronic pain, a mental/emotional condition, or a prescription drug dependency. Conversely, respondents in this group who were uninsured, received Medicaid, or were self-insured were more likely to use Kratom for these same conditions.
Finally, among respondents who used Kratom, but did not report having a diagnosed medical condition, several significant demographic differences were observed. Respondents who were female, married/partnered, unable to work, or unemployed were less likely to use Kratom for any condition except for illicit drug dependency, whereas non-Caucasian respondents were more likely to use Kratom for any condition (Fig. 3C).
DISCUSSION
The use of Kratom as a potentially safe herbal supplement for the self-treatment of medical conditions has been increasing in the United States over the past decade, with an estimated 4 to 5 million people using Kratom in the United States (Henningfield et al., 2018). The increased prevalence of both Kratom use and case reports describing adverse health occurrences associated with Kratom use have raised questions about the supplement’s safety and potential health impact (Anwar et al., 2016). Initial results of this survey characterized the demographics of US adults who reported current use of Kratom leaf products (Grundmann, 2017), including the potential for adverse effects and benefits of Kratom by examining the motivations, and experiences self-reported by current Kratom users. The study also provided an initial estimate of Kratom dosage and frequency of dosing, typically 3 g doses up to 3 times per day. Subsequent analyses of survey data presented here describe the correlations between self-reported diagnosed pre-existing health conditions and Kratom use. Among this sample, and other US-based samples, Kratom is primarily used to self-treat acute or chronic pain, or a mental/emotional condition (Grundmann, 2017; Henningfield et al., 2018; Swogger and Walsh, 2018).
Factors Influencing the Variability in Analgesic Effectiveness
The self-reported pain rating of respondents who used Kratom for acute or chronic pain may indicate that the powdered leaf by itself may not provide adequate pain relief, as only 29% rated their pain as “good” or “very good.” Animal models and receptor studies have identified that mitragynine serves as a partial agonist at the m-opioid receptor, which may result in a distinctly different analgesic effect from classical opioids such as morphine (Kruegel and Grundmann, 2017). This may indicate a more complex pharmacological effect of the Kratom powdered leaf than just the single isolated compounds being evaluated can currently reflect. Other compounds in the dried leaf may contribute to analgesic effects or limit those effects through as-of-yet-unknown mechanisms. Another explanation may be that powdered Kratom preparations are low in alkaloid content; hence the ingested dose is insufficient to provide desired pain relief.
Kratom use for a mental/emotional condition or an illicit or prescription drug dependency was associated with both improved pain and overall better health ratings. The mitigation of opioid withdrawal symptoms and improvement of pain with Kratom use have been reported elsewhere, although this is the first survey of people who use Kratom including prescription drugs confirming the potential benefits from self-treatment (Henningfield et al., 2018; Singh et al., 2019). The variability in self-reported ratings for pain and health conditions can be attributed to the dose and frequency of Kratom use, the specific Kratom product (different Kratom extracts in various formulations, eg capsule, tablets, chewable, powder, etc), duration of use, method of consumption (brewed Kratom tea vs oral consumption of dried Kratom products), and if the health condition is being treated with any other medications. People who use Kratom in the West can also be exposed to adverse health incidents if they are not cautious when buying Kratom, as some products may be adulterated, inconsistent with advertised product description, or marketed with dubious claims (Lydecker et al., 2016).
Differential Kratom Effectiveness for Somatic Versus Mental Health Conditions
Participants rated the change in their diagnosed health condition after Kratom initiation as favorable overall (Fig. 2). In general, somatic health conditions were less often rated as “significant improvement” compared with mental health conditions. Fibromyalgia had the lowest proportion of “significant improvement” responses, which is aligned with treatment guidelines that do not suggest prescription of opioids for this pain condition in general. Fibromyalgia is an insidious health condition that manifests with variability across those affected, with symptoms often difficult for physicians to discern and effectively treat (Harris et al., 2005; Chakrabarty and Zoorob, 2007; Perrot et al., 2012). However, 91.7% still ranked their change with Kratom use as “slight or significant improvement,” which may reflect the involvement of Kratom in other signaling pathways that remains to be explored (Matsumoto et al., 1996).
The percentage of respondents who reported “significant improvement” of a mental health condition with the use of Kratom was higher than for somatic health conditions, which confirms Kratom’s central nervous system effects. Nonetheless, pain and other somatic health conditions may also be modulated through central pathways. Kratom may therefore act differentially in both the peripheral and central nervous system. The highest percentage of responses among mental health conditions with “significant improvement” were for ADHD/ADD (60.3%). To date, no studies have addressed the use or effectiveness of Kratom in the treatment or management of ADHD, and only few qualitative studies have indicated potential benefits of Kratom in mitigating or managing anxiety disorders (Swogger and Walsh, 2018). Prescription medications for ADHD/ADD primarily target dopaminergic transmission; however, there is presently conflicting information on affinity and activity of Kratom and its alkaloids for dopamine receptors (Stolt et al., 2014; Vijeepallam et al., 2016). One potential mechanism by which Kratom alkaloids can mediate dopaminergic signaling is through disinhibition of GABAergic interneurons that leads to increased release of dopamine from neighboring neurons in the same manner to classical opioids (Steidl et al., 2017). Increased dopamine levels mediated by opioid receptor agonists may also contribute to the observed stimulant effects of Kratom products as they have been seen in other opioid agonists (Shim et al., 2014).
The highest response rates for “significant improvement” were reported for a diagnosed SUD (68.2%). Both traditional and modern uses of Kratom have included its nonmedical use in mitigating opioid withdrawal symptoms and as a potential harm-reduction agent for some individuals who were formerly used opioids (Swogger et al., 2015; Grundmann, 2017; Smith and Lawson, 2017). Our results suggest that Kratom may have the potential to help some people with a history of illicit drug use and dependency manage their SUD. However, without knowing other important respondent information, such as previous drug treatment history, SUD severity, or preferred addictive drug, these preliminary findings should be interpreted with caution.
The second highest “significant improvement” response was from people who use Kratom with no diagnosed medical condition. This outcome may be consonant with numerous previous findings describing the traditional use of Kratom preparations for increased stamina during the daytime and as a mood enhancer after work (Singh et al., 2015). Given the relative similarity of respondents with no diagnosed medical condition and those who were diagnosed with ADHD/ADD, there may be a specific demographic group of people who use Kratom who are majority male, primarily single, and relatively younger. Unless Kratom was used to address an illicit drug dependency, there was no correlation between educational level and Kratom use. The absence of a pre-existing health condition among some respondents may suggest that Kratom use may be, for some in this sample, largely recreational, or that Kratom is regarded as a drug of abuse, similar to alcohol, cannabis, or other psychoactive drugs. However, Kratom use without a medical condition or concomitant use of Kratom with other drugs may contribute to the development of detrimental effects. Alternately, it may be that these respondents were using Kratom to address unspecified or otherwise undiagnosed conditions.
Kratom is Distinct from Other Opioids in Its Use Patterns
The correlation between demographic variables and diagnosed somatic or mental health conditions as determinants for Kratom use are distinct and at times discordant with the existing literature on opioid use disorder (OUD) or other SUDs. The current preliminary findings, together with prior research, support the characterization of Kratom as a substance that produces some benefits consistent with those of μ-agonist opioids, namely relief of pain and opioid withdrawal symptoms, but also as a substance that is distinct from opioids. Information self-reported by respondents in this sample suggest that Kratom may have some therapeutic potential in addressing various mental health conditions, including depression and ADHD, and may also increase energy and focus—a finding previously reported by Grundmann (2017) in an earlier analysis of survey findings. When compared with μ-opioid agonists approved as either medicines (eg, oxycodone) or illicitly manufactured heroin or fentanyl, which carry well-known high risks of life-threatening respiratory depression, the adverse effects associated with Kratom use are relatively benign and can usually be self-managed (Grundmann, 2017; Grundmann et al., 2018). Young age is often cited as a risk factor for OUD (Webster, 2017), which does not uniformly apply to people who use Kratom to address a somatic health condition or even to most who use Kratom for an illicit drug dependency. A majority of younger people who use Kratom for a mental health condition may indeed not take it with the intent to mitigate withdrawal symptoms.
With the exception of ADHD/ADD, people who used Kratom who were unemployed or unable to work and who had a diagnosed health condition were more likely to use the powdered leaf compared with respondents who were employed or able to work. Unemployment has been identified as an important variable in SUDs (Sherba et al., 2018), often complicating an existing health problem or worsening it. In the traditional context, Kratom use is not associated with unemployment, but rather to enhance physical tolerance to laborious work.
A distinguishing observation is the general absence of education, race/ethnicity, and income as significant influences on Kratom use and a diagnosed health condition. In other studies, lower educational attainment and income have been found to be positively associated with increased prevalence of SUDs, especially illicit drug use (Merline et al., 2004).
Insurance status was correlated with Kratom use for prescription drug dependence, acute/chronic pain, and mental/emotional condition, with a higher likelihood of use if the respondent was uninsured, had Medicaid/Medicare, or self-insured. Access to affordable health care is a factor that often contributes to seeking self-treatment approaches if coverage is not available, unaffordable, or may not be sought because of a SUD (Moulin et al., 2018). Further, access to scientifically-informed OUD and other SUD interventions, including medication for addiction treatment (MAT), is not equitable across drug-using populations (Stein et al., 2018).
If diagnosed with SUD, participants were generally less likely to use Kratom if they were younger, married, or had lower income. SUD withdrawal symptoms have both a somatic and psychological component, which may explain the overlap in many of the trends seen with other comorbid mental health conditions. Given that a majority of respondents were using Kratom to mitigate illicit and prescription drug dependency and withdrawal symptoms, it may not be surprising that they also experienced improved pain, increased overall health ratings, and greater response proportions for “slight or significant improvement” of this condition after taking the powdered leaf. Kratom may potentially ease the somatic and psychological symptoms characteristic of drug withdrawal (Swogger et al., 2015).
Limitations
The current study has limitations of self-reported outcomes and health diagnosis, and small sample sizes for specific Kratom uses and health conditions. The survey was conducted in 2016, and since then, a variety of Kratom products have entered the US market, some of which may be adulterated, thus presenting risks and uncertainties to consumers. As such, results should not be generalized and serve as the most recent available epidemiological investigation on Kratom. The survey was distributed with the help of the American Kratom Association—an advocacy group that seeks to keep Kratom legal in the United States. Thus, the respondents were current Kratom consumers who may have viewed Kratom favorably.
CONCLUSIONS
Kratom use may serve as a self-treatment strategy for a diverse population of patients with pre-existing health diagnoses. The general improvement and favorable view of Kratom for mental health conditions points to its potential medical benefits that distinguish it from classical opioids. Some of the unidentified compounds in Kratom products may serve as lead structures in drug development for the treatment of depressive and anxiety disorders or assist illicit drug users in abstaining. Based on the current literature and the findings of this study, it is reasonable to suggest that Kratom powdered leaves likely contain a variety of active compounds with diverse targets apart from the opioid receptors. Because of the unknown side-effect profile, healthcare providers need to actively engage patients to address safety concerns and potential limitations of its use in clinical practice for specific health conditions.
ACKNOWLEDGMENTS
The authors would like to thank the American Kratom Association for distribution of the survey and assisting in collection of responses.
Financial disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
The authors state no conflict of interest.
Contributor Information
Rhiannon Bath, Midwestern University, College of Pharmacy, Department of Pharmaceutical Sciences, Glendale, AZ.
Tanner Bucholz, Midwestern University, College of Pharmacy, Department of Pharmaceutical Sciences, Glendale, AZ.
Amy F. Buros, Midwestern University, Office of Research and Sponsored Programs, Glendale, AZ.
Darshan Singh, Centre for Drug Research, Universiti Sains Malaysia, 11800 Minden, Penang, Malaysia.
Kirsten E. Smith, Kent School of Social Work, University of Louisville, Louisville, KY.
Charles A. Veltri, Midwestern University, College of Pharmacy, Department of Pharmaceutical Sciences, Glendale, AZ.
Oliver Grundmann, Midwestern University, College of Pharmacy, Department of Pharmaceutical Sciences, Glendale, AZ, College of Pharmacy, Department of Medicinal Chemistry, University of Florida, FL.
REFERENCES
- Ahmad K, Aziz Z. Mitragyna speciosa use in the northern states of Malaysia: a cross-sectional study. J Ethnopharmacol 2012;141:446–450. [DOI] [PubMed] [Google Scholar]
- Anwar M, Law R, Schier J. Notes from the field: Kratom (Mitragyna speciosa) exposures reported to poison centers: United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65:748–749. [DOI] [PubMed] [Google Scholar]
- Boyer EW, Babu KM, Adkins JE, McCurdy CR, Halpern JH. Self-treatment of opioid withdrawal using kratom (Mitragynia speciosa korth.). Addiction 2008;103:1048–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarty S, Zoorob R. Fibromyalgia. Am Fam Physician 2007;76:247–254. [PubMed] [Google Scholar]
- Galbis-Reig D A case report of Kratom addiction and withdrawal. WMJ 2016;115:49–52 [quiz 53]. [PubMed] [Google Scholar]
- Garr G, Singer AJ, Domingo A, Thode HC Jr. The Wong-Baker pain FACES scale measures pain, not fear. Pediatr Emerg Care 2013; 29: 17–20. [DOI] [PubMed] [Google Scholar]
- Grundmann O Patterns of Kratom use and health impact in the US: results from an online survey. Drug Alcohol Depend 2017;176:63–70. [DOI] [PubMed] [Google Scholar]
- Grundmann O, Brown PN, Henningfield J, Swogger M, Walsh Z. The therapeutic potential of kratom. Addiction 2018;113:1951–1953. [DOI] [PubMed] [Google Scholar]
- Harris RE, Williams DA, McLean SA, et al. Characterization and consequences of pain variability in individuals with fibromyalgia. Arthritis Rheum 2005;52:3670–3674. [DOI] [PubMed] [Google Scholar]
- Hassan Z, Muzaimi M, Navaratnam V, et al. From Kratom to mitragynine and its derivatives: physiological and behavioural effects related to use, abuse, and addiction. Neurosci Biobehav Rev 2013;37:138–151. [DOI] [PubMed] [Google Scholar]
- Henningfield JE, Fant RV, Wang DW. The abuse potential of kratom according the 8 factors of the controlled substances act: implications for regulation and research. Psychopharmacology (Berl) 2018;235:573–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idayu NF, Hidayat MT, Moklas MA, et al. Antidepressant-like effect of mitragynine isolated from Mitragyna speciosa Korth in mice model of depression. Phytomedicine 2011;18:402–407. [DOI] [PubMed] [Google Scholar]
- Khazaeli A, Jerry JM, Vazirian M. Treatment of Kratom withdrawal and addiction with buprenorphine. J Addict Med 2018;12:493–495. [DOI] [PubMed] [Google Scholar]
- Kruegel AC, Grundmann O. The medicinal chemistry and neuropharmacology of kratom: a preliminary discussion of a promising medicinal plant and analysis of its potential for abuse. Neuropharmacology 2018;134:108–120. [DOI] [PubMed] [Google Scholar]
- Kruegel AC, Gassaway MM, Kapoor A, et al. Synthetic and receptor signaling explorations of the Mitragyna alkaloids: mitragynine as an atypical molecular framework for opioid receptor modulators. J Am Chem Soc 2016;138:6754–6764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker AG, Sharma A, McCurdy CR, Avery BA, Babu KM, Boyer EW. Suspected adulteration of commercial Kratom products with 7-hydroxymitragynine. J Med Toxicol 2016;12:341–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto K, Mizowaki M, Suchitra T, et al. Central antinociceptive effects of mitragynine in mice: contribution of descending noradrenergic and serotonergic systems. Eur J Pharmacol 1996;317:75–81. [DOI] [PubMed] [Google Scholar]
- McWhirter L, Morris S. A case report of inpatient detoxification after kratom (Mitragyna speciosa) dependence. Eur Addict Res 2010;16:229–231. [DOI] [PubMed] [Google Scholar]
- Merline AC, O’Malley PM, Schulenberg JE, Bachman JG, Johnston LD. Substance use among adults 35 years of age: prevalence, adulthood predictors, and impact of adolescent substance use. Am J Public Health 2004;94:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulin A, Evans EJ, Xing G, Melnikow J. Substance use, homelessness, mental illness and medicaid coverage: a set-up for high emergency department utilization. West J Emerg Med 2018;19:902–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrot S, Choy E, Petersel D, Ginovker A, Kramer E. Survey of physician experiences and perceptions about the diagnosis and treatment of fibromyalgia. BMC Health Serv Res 2012;12:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prozialeck WC, Jivan JK, Andurkar SV. Pharmacology of kratom: an emerging botanical agent with stimulant, analgesic and opioid-like effects. J Am Osteopath Assoc 2012;112:792–799. [PubMed] [Google Scholar]
- Shaik Mossadeq WM, Sulaiman MR, Tengku Mohamad TA, et al. Anti-inflammatory and antinociceptive effects of Mitragyna speciosa Korth methanolic extract. Med Princ Pract 2009;18:378–384. [DOI] [PubMed] [Google Scholar]
- Sherba RT, Coxe KA, Gersper BE, Linley JV. Employment services and substance abuse treatment. J Subst Abuse Treat 2018;87:70–78. [DOI] [PubMed] [Google Scholar]
- Shim I, Stratford TR, Wirtshafter D. Dopamine is differentially involved in the locomotor hyperactivity produced by manipulations of opioid, GABA and glutamate receptors in the median raphe nucleus. Behav Brain Res 2014;261:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva NM. The behavioral risk factor surveillance system. Int J Aging Hum Dev 2014;79:336–338. [DOI] [PubMed] [Google Scholar]
- Singh D, Muller CP, Murugaiyah V, et al. Evaluating the hematological and clinical-chemistry parameters of kratom (Mitragyna speciosa) users in Malaysia. J Ethnopharmacol 2018;214:197–206. [DOI] [PubMed] [Google Scholar]
- Singh D, Muller CP, Vicknasingam BK, Mansor SM. Social functioning of Kratom (Mitragyna speciosa) users in Malaysia. J Psychoactive Drugs 2015;47:125–131. [DOI] [PubMed] [Google Scholar]
- Singh D, Narayanan S, Vicknasingam B. Traditional and non-traditional uses of Mitragynine (Kratom): a survey of the literature. Brain Res Bull 2016;126:41–46. [DOI] [PubMed] [Google Scholar]
- Singh DPD, Narayanan SPD, Muller CPPD, et al. Long-term cognitive effects of Kratom (Mitragyna speciosa Korth.) use. J Psychoactive Drugs 2019;51:19–27. [DOI] [PubMed] [Google Scholar]
- Smith KE, Lawson T. Prevalence and motivations for kratom use in a sample of substance users enrolled in a residential treatment program. Drug Alcohol Depend 2017;180:340–348. [DOI] [PubMed] [Google Scholar]
- Steidl S, Wasserman DI, Blaha CD, Yeomans JS. Opioid-induced rewards, locomotion, and dopamine activation: a proposed model for control by mesopontine and rostromedial tegmental neurons. Neurosci Biobehav Rev 2017;83:72–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein BD, Dick AW, Sorbero M, et al. A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Subst Abus 2018;39:419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolt AC, Schroder H, Neurath H, et al. Behavioral and neurochemical characterization of kratom (Mitragyna speciosa) extract. Psychopharmacology (Berl) 2014;231:13–25. [DOI] [PubMed] [Google Scholar]
- Suwanlert S A study of kratom eaters in Thailand. Bull Narc 1975;27:21–27. [PubMed] [Google Scholar]
- Swogger MT, Hart E, Erowid F, et al. Experiences of Kratom users: a qualitative analysis. J Psychoactive Drugs 2015;47:360–367. [DOI] [PubMed] [Google Scholar]
- Swogger MT, Walsh Z. Kratom use and mental health: a systematic review. Drug Alcohol Depend 2018;183:134–140. [DOI] [PubMed] [Google Scholar]
- Vijeepallam K, Pandy V, Kunasegaran T, Murugan DD, Naidu M. Mitragyna speciosa leaf extract exhibits antipsychotic-like effect with the potential to alleviate positive and negative symptoms of psychosis in mice. Front Pharmacol 2016;7:464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster LR. Risk factors for opioid-use disorder and overdose. Anesth Analg 2017;125:1741–1748. [DOI] [PubMed] [Google Scholar]