Abstract
The Woven EndoBridge Device (WEB) is efficient and safe in the treatment of wide-neck bifurcation intracranial aneurysms. A crucial step in operative planning is establishing the appropriate dimension of the device, and there are limitations to the therapeutic solutions provided by WEBs. We describe a case of a right middle cerebral artery bifurcation wide-neck aneurysm treated with WEB. After the initial deployment of a WEB proven oversized, we substituted it with a smaller one that presented immediate post-detachment intra-aneurysmal tilt probably resulting from undersizing. The 24-h angiographic control identified a partial displacement of the device in the superior middle cerebral artery branch. We describe rescue techniques with review of the literature and our treatment strategy, including effort to reposition the device followed by stent deployment. The treatment was electively completed by the coil-through technique. The post-detachment WEB tilt should be considered an unstable position and treated either by removal of the device or with adjunctive implants. Each WEB size adapts to a range of aneurysmal height and width. This range is not always the same for each specific WEB dimension, based on the table provided by the manufacturer. This eventually predisposes to a different behavior of different WEB sizes regarding the modification of the device’s height in relation to the modification of the diameter after deployment.
Keywords: Woven EndoBridge Device, dislocation, intracranial aneurysm, rescue techniques
Introduction
The efficacy and safety of the Woven EndoBridge Device (WEB) have been confirmed in a series of studies for the treatment of wide-neck bifurcation intracranial aneurysms.1–3
There are limitations to the therapeutic solutions provided by WEBs, as the available devices are not suitable for aneurysms smaller than 2 mm in diameter and 2.5 mm in height or exceeding 10 mm in diameter and 10.6 mm in height. In addition, they are frequently inappropriate for aneurysms in which the ratio height/diameter is too much in favor of diameter.
We present the case of an immediate post-detachment WEB tilt with displacement of the device at the 24-h angiographic control and asymptomatic partial occlusion of the superior middle cerebral artery (MCA) branch. We describe our rescue treatment with review of the literature.
Case report
A 63-year-old woman with a history of endovascular treatment for a ruptured left pericallosal artery aneurysm, completed later by flow diverter stent due to recanalization, has been readmitted in our department for the treatment of an incidental right MCA bifurcation aneurysm. The aneurysm presented irregular shape with multiple blebs and wide neck from which originated the inferior division of the MCA (Figure 1(a) to (c)). We opted for the treatment with a WEB device (MicroVention, Tustin, CA, USA).
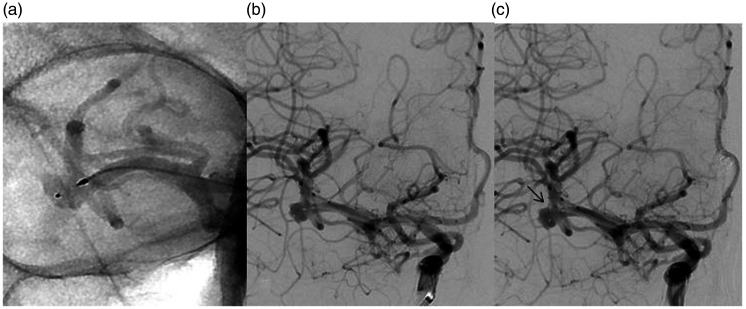
Figure 1.
(a) Right MCA bifurcation aneurysm presenting with irregular shape, multiple blebs, and wide neck from which originates the inferior division in subtraction DSA working projection. (b and c) Three-dimensional angiography in two orthogonal projections presenting the aneurysm morphology and dimensions, excluding the blebs.
The device selection is based on subtracting 1 mm from the height and adding approximately 1 mm to the average width of the aneurysm to adjust for the longitudinal increase caused by the horizontal compression.4,5 MicroVention provides a precise sizing table defining the appropriate range of aneurysm’s dimensions corresponding to each WEB. According to this table, our aneurysm (average diameter 4.8 mm, height 3.4 mm, neck 4.5 mm, excluding the blebs) (Figure 1(b) and (c)) would be ideally treated by an 6 × 2 mm WEB SL device, which does not exist. To assure a proper wall apposition, we opted alternatively for the 6 × 3 mm WEB SL.
A triaxial system with a VIA-17 (MicroVention) microcatheter was used. After the deployment of the device, the angiography identified a partial occlusion of the inferior MCA division due to protrusion of the proximal part of the device (Figure 2(a)).
Figure 2.
(a) Non-subtracted angiography demonstrating post-deployment protrusion of the proximal part of the 6 × 3 mm WEB SL, partially occluding the inferior MCA division. (b) Subtracted angiography presenting satisfactory deployment of the 5 × 3 mm WEB SL with patency of the inferior and superior MCA divisions. (c) Post-detachment tilt of the 5 × 3 mm WEB SL with the proximal marker protruding towards the superior division of the MCA (black arrow).
We withdrew the 6 × 3 mm WEB SL and we opted for the 5 × 3 mm WEB SL considering that the reduced lateral compression would allow a smaller height increase after deployment. The post-deployment angiography demonstrated a satisfactory WEB implantation with intra-aneurysmal contrast stasis and patency of the inferior and superior MCA divisions (Figure 2(b)).
Immediately after detachment, an intra-aneurysmal tilt of the WEB was observed with the proximal marker of the device orientated towards the superior division of the MCA (Figure 2(c)).
The angiography after 30 min confirmed an unmodified position of the device, so we decided to repeat the control in 24 h. The patient had no neurological deficit and the control at 24 h identified a WEB displacement and deformation with part of the device inside the aneurysmal sac and another part protruding in the superior branch of the MCA, partially occluding it but without significant hemodynamic changes (Figure 3(a) and (b)).
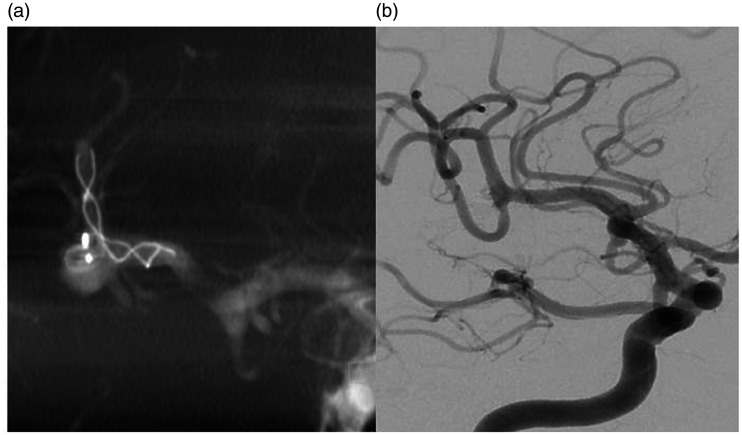
Figure 3.
Dyna-CT reconstruction (a) and non-subtracted angiography (b) at 24-h follow-up presenting 5 × 3 mm WEB SL deformation and displacement with part of the device protruding in the superior branch of the right MCA, partially occluding it.
After this finding, the device could not be left protruding. We considered that the adequate strategy would be to completely remove the WEB or to reposition it inside the aneurysmal sac before deploying a stent. In case of failed repositioning, we would deploy the stent with the objective of compressing the protruding part against the vessel wall and maintain the permeability of the superior branch.
We premedicated the patient with 250 mg of Aspirin and 600 mg of Clopidogrel. She was known to be a Clopidogrel responder due to the previous treatment of the pericallosal artery with flow diverter stent. As for retrieving the WEB, we thought of using a 2 mm Amplatz Goose Neck snare (eV3, Plymouth, USA) and in case of failure to reposition it by aspirating with a 6F Sofia Plus catheter (Microvention).
It was though impossible to gain distal access to the WEB using a 0.018″ microcatheter, so the use of the snare loop was excluded. We performed two attempts to reposition the WEB aspirating it with the 6F Sofia Plus catheter. Even though the catheter fully attached and partially retrieved the device, the latter regained its protruding position.
We opted for the 2.5 mm × 18 mm LEO baby stent deployment (Balt Extrusion, Montmorency, France). Distal access was gained with an Echelon 10 microcatheter (eV3, Plymouth) and a 0.012″ microguidewire. The angiography confirmed restauration of the superior branch with the protruding part of the WEB compressed by the stent (Figure 4(a)).
Figure 4.
(a) Dyna-CT reconstruction after revision treatment with LEO baby stent deployment. There is complete restauration of the superior branch caliber with the protruding part of the deformed WEB covered by the stent. (b) DSA working projection: complete aneurysm occlusion performed by coil-through technique in elective treatment.
The treatment was completed electively with the coil-through technique. To point out that the WEB was found located entirely inside the aneurysmal sac (Figure 4(b)).
Discussion
The intrasaccular flow disruption with the WEB device is a well-established technique.1,6,7 Based on our series of 81 aneurysms treated by WEB from September 2014 to December 2019, we consider that the crucial step is establishing the appropriate dimensions of the WEB. In addition to the recommendation of subtracting 1 mm from the height and adding approximately 1 mm to the average width of the aneurysm, MicroVention provides a sizing table, consisting in “cells,” defining the appropriate range of aneurysm’s width and height corresponding to each WEB. There are certain dimensions to which no device corresponds. According to this table, our aneurysm would be ideally treated by a 6 × 2 mm WEB SL device, which does not exist. We opted for the 6 × 3 mm WEB SL as it is of appropriate width and very slightly oversized in height. WEB oversizing plays an important role in the quality of anatomic results.3
It is well-known that the height and the diameter of the WEB are inversely modified when the device is in place. It is also to point out that in the table proposed by the manufacturer each type of WEB SL corresponds to a range of aneurysmal height always equal to 0.9 mm. On the contrary, each type of WEB SL corresponds to a different range of aneurysmal diameter that varies from a minimum of 0.4 mm to a maximum of 0.9 mm in relation to the WEB’s dimensions. This may predispose to a different behavior of each WEB regarding the modification of the device’s height in relation to the modification of the diameter after deployment.
Following the 6 × 3 mm WEB SL post-deployment partial occlusion of the superior branch, we substituted it with the 5 × 3 mm WEB SL considering that the reduced lateral compression would allow for a smaller height increase.
Despite the initial appropriate positioning, the post-detachment angiography presented an intrasaccular tilt of the device. In our opinion, the rotation resulted from the inadequate lateral wall apposition which implies that a WEB should preferentially be reduced by height and not by width in the cases that a smaller device is indicated.
The initial post-detachment position was considered acceptable, despite the tilt because of contrast stagnation, intra-aneurysmal WEB location without protrusion, as well as the specific flow pattern at the MCA vessel bifurcation. However, the 24-h follow-up presented a displacement indicating that the device was unstable. Indeed, the post-detachment tilt was certainly a clue for undersizing.
The stent deployment could have been immediately considered as a rescue technique after the tilt so as to prevent the subsequent displacement. In the case of stent deployment, dual antiplatelet therapy is considered necessary, but there is no general consensus to premedicate the patients treated electively by WEB. There is though at least a recommendation according to which unruptured complex large aneurysms with wide-neck should be premedicated with double antiplatelet therapy for a minimum of 4 days allowing the potential use of adjunctive intraluminal device.8
Adjunctive implants (coils or stents) after WEB deployment have been used in 1.9% to 8.3% of cases.1,3 In these series, a stent has been used in only two cases because of protrusion consequent to oversizing. On the contrary, in our case, we applied the stent deployment rescue technique because of a displacement of the device consequent to undersizing. Considering that the therapeutic mechanism of the WEB is intrasaccular flow disruption, we have not routinely used antiplatelet premedication in our series of 81 aneurysms. This has been the only case in which we have resorted to stent deployment.
After the WEB dislocation in the 24-h follow-up, we decided to remove the device. A displaced WEB has been removed with an Alligator retrieval device in the literature,9 but this was not available in our department. Our alternative was a 2-mm Amplatz Goose Neck snare, but the grasping mechanism of the snare is not as adapt as of the Alligator device. In our case, the proximal marker of the WEB was not accessible, and the use of the snare would be possible only if the access beyond the device could be gained with a 0.018″ microcatheter. Afterwards it would be necessary to grasp the protruding part with the loop of the snare which would be extremely difficult.
There has also been described the use of a microcatheter to push inside the aneurysmal sac a non-deformed device protruding in M1 segment.10 This was not our case, as the deformed device should be initially pulled back from the M2 segment.
To apply traction so as to reposition the WEB and consequently facilitate the deployment of a stent, we attempted twice an aspiration with the Sofia Plus 6F catheter. After a partial withdrawal of the device, this regained its position. Trying to remove the device by aspiration would be impossible since the catheter would be non-occlusive.
Finally, we used a 2.5 mm × 18 mm LEO baby stent which proved of adequate radial force to restore the caliber of the superior branch, compressing the protruding part of the WEB.
In conclusion, based on this experience, an immediate post-deployment intrasaccular tilt of the WEB should be considered as an unstable position and treated immediately.
Conclusion
The WEB is indicated for wide-neck bifurcation aneurysms. Some of these cannot be treated with WEB in first line because of limitations imposed by the need for precise device’s dimensions, not always available. The post-detachment WEB tilt should be considered an unstable position and treated either with removal of the device or with adjunctive implants.
Consent for publication
Written informed consent was obtained from the patient for publication of medical data and images.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Fortunato Di Caterino https://orcid.org/0000-0003-4478-0486
Panagiotis Primikiris https://orcid.org/0000-0002-9547-5791
Giovanni Vitale https://orcid.org/0000-0002-5423-4000
References
- 1.Pierot L, Costalat V, Moret J, et al. Safety and efficacy of aneurysm treatment with WEB: results of the WEBCAST study. J Neurosurg 2016; 124: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 2.Pierot L, Spelle L, Molyneux A, et al. WEBCAST and French Observatory Investigators. Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and French Observatory). Neurosurgery 2016; 78: 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pierot L, Gubucz I, Buhk JH, et al. Safety and efficacy of aneurysm treatment with the WEB: results of the WEBCAST 2 study. AJNR Am J Neuroradiol 2017; 38: 1151–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lescher S, du Mesnil de Rochemont R, Berkefeld J. Woven Endobridge (WEB) device for endovascular treatment of complex unruptured aneurysms – a single center experience. Neuroradiology 2016; 58: 383–390. [DOI] [PubMed] [Google Scholar]
- 5.Cagnazzo F, Ahmed R, Dargazanli C, et al. Treatment of wide-neck intracranial aneurysms with the Woven EndoBridge Device associated with stenting: a single-center experience. AJNR Am J Neuroradiol 2019; 40: 820–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pierot L, Biondi A. Endovascular techniques for the management of wide-neck intracranial bifurcation aneurysms: a critical review of the literature. J Neuroradiol 2016; 43: 167–175. [DOI] [PubMed] [Google Scholar]
- 7.Pierot L, Biondi A, Narata AP, et al. Should indications for WEB aneurysm treatment be enlarged? Report of a series of 20 patients with aneurysms in “atypical” locations for WEB treatment. J Neuroradiol 2017; 44: 203–209. [DOI] [PubMed] [Google Scholar]
- 8.Spelle L, Liebig T. Letter to the editor. Neuroradiol J 2014; 27: 369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.König I, Weber A, Weber W, et al. Dislocation of a WEB device into the middle cerebral artery: removal with the alligator retrieval device. Clin Neuroradiol 2019; 29: 361–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.John S, Navarro R, Hussain SI, et al. Rescue maneuver for dislocated Woven EndoBridge Device in middle cerebral artery. World Neurosurg 2019; 130: 467–469. [DOI] [PubMed] [Google Scholar]