Abstract
Background
Limited data are available regarding the predictors, clinical relevance, and bleeding rate by surgical devices of intracranial hemorrhage after endovascular thrombectomy. This is partially explained by the difference in the classification and definition of hemorrhage among studies. The purpose of this study was to identify the predictors of hemorrhagic transformation and isolated subarachnoid hemorrhage after endovascular thrombectomy.
Methods
This was a retrospective, multicenter observational cohort study of consecutive patients who underwent endovascular thrombectomy between January 2015 and December 2018. Univariate and logistic regression analyses were performed to determine the predictors, the impact on clinical outcomes, and the bleeding rate by surgical devices of hemorrhagic transformation and isolated subarachnoid hemorrhage.
Results
Among 610 eligible patients, hemorrhagic transformations occurred in 93 (15.2%). Fourteen patients (2.3%) were classified as having symptomatic intracranial hemorrhage. Isolated subarachnoid hemorrhage was found in 60 (9.8%) patients. In the logistic regression analyses, diabetes mellitus (odds ratio: 1.92; 95% confidence interval: 1.06–3.49) was associated with hemorrhagic transformation, and the number of device passes (odds ratio: 1.33; 95% confidence interval: 1.11–1.59) was associated with isolated subarachnoid hemorrhage. Both hemorrhagic transformation and isolated subarachnoid hemorrhage were associated with poor 90-day functional outcomes. There was a significant correlation between treatment with stent retrievers and isolated subarachnoid hemorrhage.
Conclusions
Patients with diabetes mellitus were vulnerable to hemorrhagic transformation, whereas those who underwent several attempts of thrombectomy were susceptible to isolated subarachnoid hemorrhage. Both hemorrhage types worsened the functional outcome. Treatment with the stent retriever was significantly associated with postprocedural isolated subarachnoid hemorrhage.
Keywords: Thrombectomy, hemorrhage, postoperative complications, stroke
Introduction
A series of randomized trials have consistently demonstrated the benefits of endovascular thrombectomy (EVT) with or without intravenous thrombolysis (IVT) over IVT alone for the treatment of acute ischemic stroke (AIS) caused by a large vessel occlusion (LVO) in the anterior circulation.1 However, both IVT and EVT have potential risks of intracranial hemorrhage (ICH), especially symptomatic ICH results in poor outcomes. Although several prediction models for ICH after IVT have been reported,2 none has been sufficiently validated for ICH after EVT. Although predictors of ICH after EVT have been discussed in the literature,3–10 they have not been established. This was partially explained by the difference in the classification and definition of hemorrhage between studies.
The European Cooperative Acute Stroke Study (ECASS) classification11 has been widely used in IVT trials because hemorrhagic transformation of the ischemic tissue is the major event after lytic treatment. However, the widespread availability of EVT devices that resulted in additional types of bleeding (i.e., intraventricular hemorrhage, subarachnoid hemorrhage [SAH], and subdural hemorrhage), precipitated an expansion of the classification of ICH. Although SAH as well as hemorrhagic infarction (HI) and parenchymal hematoma (PH) are the frequently reported types of hemorrhagic complications after EVT, information about their predictors was limited. Hence, we aimed to determine the predictors of hemorrhagic transformation and SAH after EVT.
Materials and methods
We conducted a retrospective cohort study using data from the Tama-Registry of Acute endovascular Thrombectomy (TREAT), a region-wide retrospective survey of acute mechanical thrombectomy in Tama, a suburban in Tokyo. The TREAT involved 12 thrombectomy capable centers and included AIS patients who received endovascular recanalization therapy (including intra-arterial thrombolysis and percutaneous transluminal angioplasty with or without stenting) to the internal carotid artery, middle cerebral artery, anterior cerebral artery, vertebral artery, and basilar artery. Further details regarding the TREAT have been reported elsewhere.12
We included patients if they (1) were registered in TREAT between January 2015 and December 2018, (2) suffered AIS out of the treating hospitals, (3) were diagnosed with AIS caused by LVO in the anterior circulation, and (4) received mechanical thrombectomy. We excluded patients if they (1) had aortic dissections and (2) had frank mechanical complications.
Each patient had preprocedural non-contrast computed tomography (CT) or magnetic resonance imaging for determination of an Alberta Stroke Program Early CT Score (ASPECTS) or diffusion-weighted imaging (DWI) ASPECTS. Occluded arteries including the internal carotid artery, middle cerebral artery (M1 or M2), or anterior cerebral artery (A1 or A2) were confirmed by CT angiography, magnetic resonance angiography, or digital subtraction angiography.
Intravenous tissue plasminogen activator (IV-tPA) (0.6 mg/kg) was administered to most patients who were eligible according to the Japanese guideline. Mechanical thrombectomy consisted of stent retriever thrombectomy alone, thrombectomy with a large bore aspiration system alone, and combined technique using both devices. The choice of devices and adjunctive endovascular techniques was left to the discretion of the local neurointerventionists.
A postprocedural modified thrombolysis in cerebral infarction grade 2b or 3 was defined as successful recanalization. CT was usually performed 24 ± 8 and 72 ± 8 h after the procedure or whenever neurological symptoms worsened. Hemorrhagic transformation consisted of the following four subtypes: HI 1: scattered small petechiae, no mass effect; HI2: confluent petechiae, no mass effect; PH 1: hematoma within infarct tissue and occupied <30% of the infarct volume, no substantive mass effect; and PH2: hematoma occupied ≥30% of the infarct volume, with an obvious mass effect. SAH was defined as postinterventional subarachnoid hyperdensities on CT and was further classified into the following two groups: isolated SAH and SAH with PH. We did not distinguish SAH from a mixed SAH and contrast extravasation because TREAT did not include information about Hounsfield unit of the postinterventional subarachnoid hyperdensities. The analyses of the predictors were performed for hemorrhagic transformation and isolated SAH. Symptomatic ICH was diagnosed if the newly observed PH2 within 90 days was associated with >4-point increase in the score on the National Institutes of Health Stroke Scale (NIHSS), primarily according to the definition used in the Safe Implementation of Thrombolysis in Stroke–Monitoring Study (SITS-MOST).13 Good functional outcome was defined as a modified Rankin Scale (mRS) score of 0, 1, or 2 at 90 days.
This study was conducted in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments. All study protocols were approved by the ethical committee of each participating institution. Informed consent was obtained in the form of opt-out in each hospital.
Statistical analysis
Continuous variables were analyzed with the Mann–Whitney U test. Categorical variables were analyzed, and univariate analysis was performed with χ2 or Fisher’s exact tests. Binary logistic regression analyses were then performed to determine the independent predictors of hemorrhagic transformation and isolated SAH using variables with a p < 0.10. Multicollinearity was assessed by the variance inflation factor, with the tolerance value set at <2. The level of significance was defined as p < 0.05. All statistical analyses were performed using R software (version 3.5.0; R Foundation for Statistical Computing, Vienna, Austria).
Results
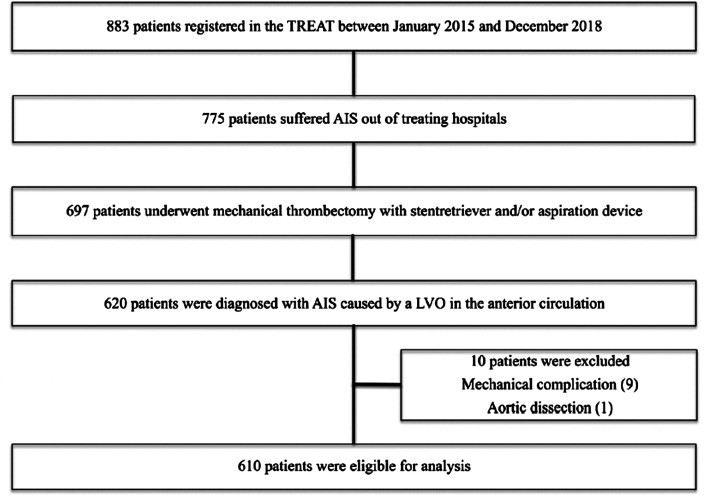
During the study period, a total of 883 patients were registered in the TREAT. Of those, 610 patients were identified according to the inclusion and exclusion criteria. The flow diagram of the patient selection process is shown in Figure 1. Median age for the cohort was 79 (70–85) years. Median baseline NIHSS score and DWI-ASPECTS were 18 (13–23) and 7 (6–9), respectively. A total of 298 patients (48.9%) underwent IVT prior to EVT. Successful recanalization was achieved in 511 patients (83.8%), and the mean time from symptom onset to recanalization was 4.1 (3.1–6.2) h. Hemorrhagic transformations occurred in 93 (15.2%) patients. Of these, 14 patients (2.3%) were classified as symptomatic ICH according to the SITS-MOST definition. Isolated SAH was found in 60 (9.8%) patients, whereas SAH with PH was found in 14 (2.3%). In total, 114 patients were treated with both the stent retriever and aspiration device, whereas 357 were treated with the stent retriever only and 139 were treated with the aspiration device only.
Figure 1.
The flow diagram of the patient selection process.
Patients’ characteristics according to whether hemorrhagic transformation, SAH, and symptomatic ICH had occurred are shown in Tables 1, 2, and 3, respectively. In the univariate analyses, the prevalence of diabetes mellitus was higher in patients with hemorrhagic transformation than in patients without (30.1% vs. 17.2%; p = 0.006). The proportion of patients taking oral anticoagulant was higher in patients with hemorrhagic transformation (30.1% vs. 19.3%; p = 0.026). Patients with hemorrhagic transformation had lower baseline DWI-ASPECTS (7 [5–8] vs. 8 [6–9]; p = 0.016) and longer onset to reperfusion time (294.5 [195–461] min vs. 241 [185–354] min; p = 0.017). Differences occurred in the distribution of occlusion site between patients with and without SAH. (p = 0.008). The proportion of patients taking oral anticoagulants was higher in those with SAH (31.7 vs. 19.8%; p = 0.044). The number of device passes was more in patients with SAH (2 [1–2] vs. 2 [1–3]; p < 0.001). We found no associated factor of symptomatic ICH.
Table 1.
Characteristics of patients with and without hemorrhagic transformation.
| Without | With | P value | |
|---|---|---|---|
| Variables | N = 517 | N = 93 | |
| Local anesthesia, n (%) | 514 (99.4) | 93 (100.0) | 1 |
| Atrial fibrillation, n (%) | 286 (55.3) | 57 (61.3) | 0.31 |
| Diabetes mellitus, n (%) | 89 (17.2) | 28 (30.1) | 0.006 |
| Dyslipidemia, n (%) | 137 (26.5) | 27 (29.0) | 0.61 |
| Male sex, n (%) | 281 (54.4) | 53 (57.0) | 0.65 |
| Hypertension, n (%) | 339 (65.6) | 62 (66.7) | 0.91 |
| Intra-arterial thrombolysis, n (%) | 3 (0.6) | 1 (1.1) | 0.49 |
| Occlusion site, n (%) | |||
| Intracranial ICA | 55 (10.6) | 8 (8.6) | 0.28 |
| ICA with involvement of the M1 middle cerebral artery segment | 64 (12.4) | 19 (20.4) | |
| M1 middle cerebral artery segment | 259 (50.1) | 45 (48.4) | |
| M2 middle cerebral artery segment | 86 (16.6) | 10 (10.8) | |
| A2 anterior cerebral artery segment | 2 (0.4) | 0 (0.0) | |
| Extracranial ICA | 51 (9.9) | 11 (11.8) | |
| Anticoaglant, n (%) | 100 (19.3) | 28 (30.1) | 0.026 |
| Antiplatelet, n (%) | 97 (18.8) | 23 (24.7) | 0.2 |
| Statin, n (%) | 87 (16.8) | 14 (15.1) | 0.76 |
| Prestroke mRS | 0 [0, 2] | 0 [0, 2] | 0.45 |
| mTICI ≥2b, n (%) | 437 (84.5) | 74 (79.6) | 0.23 |
| Stroke cause, n (%) | |||
| Cardioembolism | 387 (74.9) | 72 (77.4) | 0.05 |
| Atherosclerosis | 71 (13.7) | 11 (11.8) | |
| Dissection | 1 (0.2) | 3 (3.2) | |
| Others | 17 (3.3) | 1 (1.1) | |
| Unknown | 41 (7.9) | 6 (6.5) | |
| Intravenous thrombolysis, n (%) | 256 (49.5) | 42 (45.2) | 0.5 |
| Age–year | 79 [69, 85] | 79 [73, 84] | 0.5 |
| DWI ASPECTS | 8 [6, 9] | 7 [5, 8] | 0.016 |
| NIHSS on admission | 18 [13, 22] | 18 [14, 24] | 0.29 |
| Number of device passes | 2 [1, 3] | 2 [1, 3] | 0.29 |
| Onset to reperfusion time–hour | 4.02 [3.08, 5.89] | 4.91 [3.25, 7.67] | 0.017 |
Numeric variables are expressed as medians (25th–75th percentiles).
ICA: internal carotid artery; mRS: modified Rankin Scale; mTICI: modified thrombolysis in cerebral infarction; DWI: diffusion-weighted imaging; ASPECTS: Alberta Stroke Program Early Computed Tomography Score; NIHSS: National Institutes of Health Stroke Scale.
Table 2.
Characteristics of patients with and without isolated subarachnoid hemorrhage.
| Without | With | P value | |
|---|---|---|---|
| Variables | N = 550 | N = 60 | |
| Local anesthesia, n (%) | 548 (99.6) | 59 (98.3) | 0.27 |
| Atrial fibrillation, n (%) | 311 (56.5) | 32 (53.3) | 0.68 |
| Diabetes mellitus, n (%) | 110 (20.0) | 7 (11.7) | 0.17 |
| Dyslipidemia, n (%) | 147 (26.7) | 17 (28.3) | 0.76 |
| Male sex, n (%) | 304 (55.3) | 30 (50.0) | 0.5 |
| Hypertension, n (%) | 366 (66.5) | 35 (58.3) | 0.2 |
| Intraarterial thrombolysis, n (%) | 4 (0.7) | 0 (0.0) | 1 |
| Occlusion site, n (%) | |||
| Intracranial ICA | 57 (10.4) | 6 (10.0) | 0.008 |
| ICA with involvement of the M1 middle cerebral artery segment | 72 (13.1) | 11 (18.3) | |
| M1 middle cerebral artery segment | 283 (51.5) | 21 (35.0) | |
| M2 middle cerebral artery segment | 77 (14.0) | 19 (31.7) | |
| A2 anterior cerebral artery segment | 2 (0.4) | 0 (0.0) | |
| Extracranial ICA | 59 (10.7) | 3 (5.0) | |
| Anticoaglant, n (%) | 109 (19.8) | 19 (31.7) | 0.04 |
| Antiplatelet, n (%) | 105 (19.1) | 15 (25.0) | 0.3 |
| Statin, n (%) | 87 (15.8) | 14 (23.3) | 0.14 |
| Prestroke mRS | 0 [0, 2] | 0 [0, 1.25] | 0.77 |
| mTICI ≥ 2b, n (%) | 463 (84.2) | 48 (80.0) | 0.46 |
| Stroke cause, n (%) | |||
| Cardioembolism | 414 (75.3) | 45 (75.0) | 0.16 |
| Atherosclerosis | 76 (13.8) | 6 (10.0) | |
| Dissection | 4 (0.7) | 0 (0.0) | |
| Others | 18 (3.3) | 0 (0.0) | |
| Unknown | 38 (6.9) | 9 (15.0) | |
| Intravenous thrombolysis, n (%) | 270 (49.1) | 28 (46.7) | 0.79 |
| Age–year | 78.5 [69, 85] | 79 [72, 85] | 0.63 |
| DWI ASPECTS | 7 [6, 9] | 7 [5, 8] | 0.36 |
| NIHSS on admission | 18 [13, 23] | 18 [12, 22] | 1 |
| Number of device passes | 2 [1, 2] | 2 [1, 3] | 0.001 |
| Onset to reperfusion time–hour | 4.12 [3.08, 6.17] | 4.18 [3.09, 6.97] | 0.63 |
Numeric variables are expressed as medians (25th–75th percentiles).
ICA: internal carotid artery; mRS: modified Rankin Scale; mTICI: modified thrombolysis in cerebral infarction; DWI: diffusion-weighted imaging; ASPECTS: Alberta Stroke Program Early Computed Tomography Score; NIHSS: National Institutes of Health Stroke Scale.
Table 3.
Characteristics of patients with and without symptomatic intracranial hemorrhage.
| Without | With | P value | |
|---|---|---|---|
| Variables | N = 591 | N = 19 | |
| Local anesthesia, n (%) | 588 (99.5) | 19 (100) | 1 |
| Atrial fibrillation, n (%) | 332 (56.2) | 11 (57.9) | 1 |
| Diabetes mellitus, n (%) | 112 (19.0) | 5 (26.3) | 0.385 |
| Dyslipidemia, n (%) | 161 (27.2) | 3 (15.8) | 0.429 |
| Male sex, n (%) | 322 (54.5) | 12 (63.2) | 0.492 |
| Hypertension, n (%) | 389 (65.8) | 12 (63.2) | 0.809 |
| Intraarterial thrombolysis, n (%) | 4 (0.7) | 0 (0.0) | 1 |
| Occlusion site, n (%) | |||
| Intracranial ICA | 62 (10.5) | 1 (5.3) | 0.219 |
| ICA with involvement of the M1 middle cerebral artery segment | 77 (13.0) | 6 (31.6) | |
| M1 middle cerebral artery segment | 297 (50.3) | 7 (36.8) | |
| M2 middle cerebral artery segment | 94 (15.9) | 2 (10.5) | |
| A2 anterior cerebral artery segment | 2 (0.3) | 0 (0.0) | |
| Extracranial ICA | 59 (10.0) | 3 (15.8) | |
| Anticoaglant, n (%) | 125 (21.2) | 3 (15.8) | 0.777 |
| Antiplatelet, n (%) | 117 (19.8) | 3 (15.8) | 1 |
| Statin, n (%) | 100 (16.9) | 1 (5.3) | 0.341 |
| Prestroke mRS | 0 [0, 2] | 0 [0, 1] | 0.541 |
| mTICI ≥2b, n (%) | 495 (83.8) | 16 (84.2) | 1 |
| Stroke cause, n (%) | |||
| Cardioembolism | 444 (75.1) | 15 (78.9) | 0.957 |
| Atherosclerosis | 79 (13.4) | 3 (15.8) | |
| Dissection | 4 (0.7) | 0 (0.0) | |
| Others | 18 (3.0) | 0 (0.0) | |
| Unknown | 46 (7.8) | 1 (5.3) | |
| Intravenous thrombolysis, n (%) | 290 (49.1) | 8 (42.1) | 0.644 |
| Age–year | 79 [70, 85] | 81 [73, 85] | 0.323 |
| DWI ASPECTS | 7.00 [6.00, 9.00] | 7.00 [5.00, 8.00] | 0.254 |
| NIHSS on admission | 18 [13, 23] | 17 [11, 22.5] | 0.42 |
| Number of device passes | 2 [1, 3] | 1 [1, 2] | 0.401 |
| Onset to reperfusion time–hour | 4.09 [3.08, 6.14] | 5.44 [3.65, 11.44] | 0.088 |
Numeric variables are expressed as medians (25th–75th percentiles).
ICA: internal carotid artery; mRS: modified Rankin Scale; mTICI: modified thrombolysis in cerebral infarction; DWI: diffusion-weighted imaging; ASPECTS: Alberta Stroke Program Early Computed Tomography Score.
In the logistic regression analyses, diabetes mellitus (odds ratio [OR], 1.92; 95% confidence interval [CI], 1.06–3.49) was associated with hemorrhagic transformation, and the number of device passes (OR, 1.33; 95% CI, 1.11–1.59) was associated with SAH. The results of the logistic regression analysis are summarized in Tables 4 and 5. After controlling for age, prestroke mRS, baseline NIHSS, DWI-ASPECTS, IVT, recanalization status, and onset to reperfusion time, the occurrences of hemorrhagic transformation (OR 3.14 (1.51–6.56), p < 0.01) and isolated SAH (OR 4.83 (1.99–11.8), p < 0.001) were associated with poor 90-day functional outcomes. Variance inflation factors for all variables used in the regression analyses were <2, thus eliminating the issue of multicollinearity in our model.
Table 4.
Multivariate analysis of predictors of hemorrhagic transformation.
| Variable | OR [95% CI] | P value |
|---|---|---|
| Diabetes mellitus | 1.92 [1.06–3.49] | 0.032 |
| DWI ASPECTS | 0.92 [0.82–1.02] | 0.125 |
| Onset to reperfusion time–hour | 1.03 [0.99–1.07] | 0.118 |
| Stroke cause | 0.92 [0.71–1.20] | 0.54 |
| Oral anticoaglant | 1.62 [0.86–3.05] | 0.136 |
OR: odds ratio; DWI: diffusion-weighted imaging; ASPECTS: Alberta Stroke Program Early Computed Tomography Score.
Table 5.
Multivariate analysis of predictors of isolated subarachnoid hemorrhage.
| Variable | OR [95% CI] | P value |
|---|---|---|
| Occlusion site | 0.95 [0.86–1.06] | 0.381 |
| Number of device passes | 1.33 [1.11–1.59] | <0.01 |
| Oral anticoaglant | 1.75 [0.97–3.16] | 0.065 |
OR: odds ratio; CI: confidence interval.
Hemorrhagic transformation was found in 15.7% (56/357) and 12.9% (18/139) of patients treated with the stent retriever only and aspiration device only, respectively. There was no significant correlation between hemorrhagic transformation and thrombectomy device in the univariate analysis (p = 0.49). On the other hand, there was a significant correlation between isolated SAH and thrombectomy device (10.1% of patients treated with the stent retriever only and vs. 3.6% of patients treated with the aspiration device only).
Discussion
In this study, we found that diabetes mellitus was an independent predictor of hemorrhagic transformation, whereas number of device passes was an independent predictor of isolated SAH after EVT. In cases without hemorrhage caused by obvious mechanical complications, such as vessel dissection and vessel perforation, it was assumed that the fundamental mechanism leading to ICH was disruption of the blood–brain barrier and rupture of small arterioles caused by displacement of the occluded artery during clot retrieval.14,15 Although mechanisms of the hemorrhages theoretically do not correspond to radiographic classification on a one-on-one basis, predictors of hemorrhagic transformation and isolated SAH are considered different. Our results confirmed that the two hemorrhages had different predictors.
There were several trials reporting that serum glucose level or diabetes mellitus was one of the predictive factors for intracerebral hemorrhage after IVT.16–20 Moreover, these parameters were proposed to be among the predictive factors for ICH even after EVT. Nogueira et al. revealed that diabetes mellitus (OR 2.27 (1.58–3.26)) was an independent predictor of HI.7 Neuberger et al. showed that a higher serum glucose level (OR 1.23, 95% CI 1.10–1.39) was significantly associated with a greater risk of any ICH.8 Kaesmacher et al. demonstrated that a higher admission glucose level (OR 1.493, 95% CI 1.17–1.90) was an independent risk factor for HI.10 This study further confirmed that diabetes mellitus was associated with ICH after reperfusion therapy for AIS. There is an experimental report that demonstrated chronic hyperglycemia aggravated hemorrhagic transformation after ischemia/reperfusion injury by middle cerebral artery occlusion through mitochondrial dysfunction and morphological alteration, leading to caspase-dependent apoptosis of endothelial cells of diabetic mice.21 This might be the reason high serum glucose level or diabetes mellitus predicts hemorrhagic transformation. IV-tPA, antiplatelet pretreatment, and anticoagulant pretreatment were not associated with hemorrhagic transformation, which was consistent with the findings of other previous studies.5,8–10,22,23
Regarding the predictors of SAH, there were fewer studies compared to the number of studies on hemorrhagic transformation.24–27 Some trials demonstrated that the greater number of device passes was one of the predictive factors of SAH. Ng et al. showed that an increased number of device passes was associated with SAH after EVT to middle cerebral artery occlusion in 85 patients; of these, 8 patients had SAH after EVT. A significantly greater proportion of patients with SAH had >2 stent retriever passes compared with those without SAH (62.5% vs. 18.2%, p = 0.01). Only the univariate analysis was performed.26 Nikoubashman et al. reported that a high number of recanalization attempts were one of the predictive factors of SAH. In that study, cases with more than one recanalization attempt were associated with postinterventional subarachnoid hyperdensities on logistic regression analysis (OR and CI were not available, p = 0.039).27 Our finding was in line with the findings in these studies. It was assumed that repeated passes might cause additional mechanical stretch during clot retrieval and increase the likelihood of angiographically occult perforations of small arterioles, thereby resulting in SAH. Oral anticoagulant use showed a trend toward a higher chance of SAH in our study (OR, 1.75; 95% CI, 0.97–3.16). Impact of oral anticoagulant use on SAH after EVT was not well studied so far. Although not only anticoagulation status but also control of international normalized ratio (INR) is important, we could not obtain INR because it was not recorded in the database. Further investigation is needed in this topic.
Although predictors of symptomatic ICH after EVT have been discussed in the literature,5,6,8 we did not analyze the predictors of symptomatic ICH for two reasons. First, the number of patients was not enough to perform logistic regression analysis considering the 10 events per variable rule. In our study, the number of patients with symptomatic ICH was 14/610 (2.3%), which is consistent with the result of the Revascularization With Solitaire FR Device Versus Best Medical Therapy in the Treatment of Acute Stroke due to Anterior Circulation Large Vessel Occlusion Presenting Within Eight Hours of Symptom Onset (REVASCAT) that reported that number of patients with symptomatic ICH, defined according to the SITS-MOST criteria, was 4/206 (1.9%).28 Regarding the predictors of symptomatic ICH, Hao et al. reported that cardioembolic stroke, poor collateral circulation, delayed endovascular treatment, multiple passes with a stent retriever device, lower pretreatment ASPECTS, and higher baseline neutrophil ratio may increase the risk of symptomatic ICH in a multicenter registry study.5 In that study, symptomatic ICH defined according to the Heidelberg bleeding classification accounted for 16.0% of cases (101/632). However, this was substantially high even if the difference in study setting and definition of the symptomatic ICH was considered. Predictors of symptomatic ICH after EVT should be investigated in a larger cohort, with the rate of symptomatic ICH similar to that in previous randomized trials.
Second, both predictors of symptomatic ICH and of hemorrhagic transformation are considered important, because it still remains unclear whether the newly observed imaging findings bring additional neurological deficit. In this study, we revealed that postprocedure hemorrhagic transformation was associated with poor 90-day functional outcomes. In the ECASS, only PH2, but not PH1 or HI, was associated with early deterioration and three-month mortality.11 Lee et al. reported that PH was the most powerful independent predictor of poor outcome, whereas HI was not an independent predictor of poor outcome.9 In contrast, some previous studies reported that HI is not a benign imaging sign. Nogueira et al. demonstrated that both HI and PH were independent predictors of poor 90-day functional outcomes.7 Similarly, Kaesmacher et al. showed that both HI and PH were independently associated with lower rates of good neurologic outcome defined as NIHSS score <5 at the day of discharge.10 Moreover, the Canadian Alteplase for Stroke Effectiveness Study (CASES) Registry revealed that HI2, along with PH1 and PH2, was a negative predictor of good 90-day functional outcomes.29
With respect to the effect of SAH on functional outcomes, we found that postprocedural isolated SAH was associated with poor 90-day functional outcomes. Previous studies obtained controversial results regarding the effect of postprocedural SAH. In their analysis of 12 cases, Yoon et al. reported that SAH after mechanical thrombectomy had a benign prognosis.15 Furthermore, Ng et al. demonstrated that one out of eight patients developed a postinterventional Sylvian fissure hematoma and experienced neurological deterioration, with a 9-point increase in the NIHSS score several hours after the procedure.26 This could be partially explained by the extent of damage to the vessels during thrombectomy. Further studies are required to confirm the effect of postprocedural SAH.
There was a significant correlation between isolated SAH and thrombectomy with the stent retriever in our study. Peschillo et al. reported that both the stent retriever and aspiration device can damage the vessel walls; however, the former appeared to be more harmful to all layers of the arterial wall, particularly the endothelium.30 Our result was consistent with this report.
Several limitations of the present study must be noted when interpreting the results. First, the possibility of residual confounding factors exists because of the retrospective nature of the study. Second, some important parameters, such as serum glucose level and INR, were not available in TREAT. Third, imaging studies were not reviewed in the core laboratory. Fourth, although selection of the devices and periprocedural use of antiplatelets or anticoagulants might have an influence on postprocedural bleeding status, participating centers did not have an organized treatment protocol.
In conclusion, patients with diabetes mellitus were vulnerable to hemorrhagic transformation, whereas those who underwent several attempts of thrombectomy were susceptible to SAH. Both hemorrhage types worsened the functional outcome. Treatment with the stent retriever was significantly associated with postprocedural isolated SAH. Our data contribute to better patient selection and understanding of the hemorrhagic events. However, further investigation in a larger cohort is warranted.
IRB approval number
Disaster Medical Center 2017-5.
Acknowledgment
The TREAT enrolling hospitals and investigators. Fussa Hospital: Takahisa Fuse. Hino Municipal Hospital: Yoshi-aki Kuroshima. Kitahara International Hospital: Hirotaka Yoshida. Kyorin University: Tatsuo Amano, Teruyuki Hirano and Yoshiaki Shiokawa. Musashino Red Cross Hospital: Youhei Sato. National Hospital Organization Disaster Medical Center: Keigo Shigeta. Nippon Medical School Tama Nagayama Hospital: Junya Kaneko. Sassa General Hospital: Atushi Shimada. Showa General Hospital: Akira Saito and Osamu Ishikawa. Tokai University Hachioji Hospital: Masami Shi- moda and Shigeru Nogawa. Tokyo Medical University Hachioji Medical Center: Hiroyuki Jimbo and Junya Tsurukiri. Tokyo Metropolitan Tama Medical Center: Takahiro Ota and Masayuki Ueda.
Author contributor
M Enomoto wrote the statistical analysis plan, cleaned and analysed the data, and drafted and revised the paper. K Shigeta and T Ota designed data collection tools, monitored data collection for the whole trial, and revised the paper. T Amano, Y Matsumaru, Y Shiokawa, and T Hirano did final approval of the version to be published.
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M Enomoto, K Shigeta, T Ota, and T Amano declare that they have no competing interests. Y Matsumaru received honoraria from Medtronic, Stryker, and Johnson&Johnson. Y Shiokawa received research grant from AbbVie GK and ONO Pharmmedical Co., Ltd. T Hirano received honoraria from Bayer, Boehringer-Ingelheim, Bristol-Myers Squibb, Daiichi-Sankyo, Otsuka Pharma, Pfizer, and Sanofi.
Ethical approval
This study was conducted in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments. All study protocols were approved by the ethical committee of each participating institution. Informed consent was obtained in the form of opt-out in each hospital.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was partially supported by the Japanese Society for Neuroendovascular Therapy and Taiju Life Social Welfare Foundation.
ORCID iDs
Masaya Enomoto https://orcid.org/0000-0002-1084-8780
Takahiro Ota https://orcid.org/0000-0002-5108-6719
References
- 1.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 2.Yaghi S, Willey JZ, Cucchiara B, et al. Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017; 48: e343–e361. [DOI] [PubMed] [Google Scholar]
- 3.Jiang S, Fei A, Peng Y, et al. Predictors of outcome and hemorrhage in patients undergoing endovascular therapy with solitaire stent for acute ischemic stroke. PLoS One 2015; 10: 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raychev R, Jahan R, Liebeskind D, et al. Determinants of intracranial hemorrhage occurrence and outcome after neurothrombectomy therapy: insights from the solitaire FR with intention for thrombectomy randomized trial. Am J Neuroradiol 2015; 36: 2303–2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hao Y, Yang D, Wang H, et al. Predictors for symptomatic intracranial hemorrhage after endovascular treatment of acute ischemic stroke. Stroke 2017; 48: 1203–1209. [DOI] [PubMed] [Google Scholar]
- 6.Sugiura Y, Yamagami H, Sakai N, et al. Predictors of symptomatic intracranial hemorrhage after endovascular therapy in acute ischemic stroke with large vessel occlusion. J Stroke Cerebrovasc Dis 2017; 26: 766–771. [DOI] [PubMed] [Google Scholar]
- 7.Nogueira RG, Gupta R, Jovin TG, et al. Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: a multicenter retrospective analysis of 1122 patients. J Neurointerv Surg 2015; 7: 16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neuberger U, Kickingereder P, Schönenberger S, et al. Risk factors of intracranial hemorrhage after mechanical thrombectomy of anterior circulation ischemic stroke. Neuroradiology 2019; 61: 461–469. [DOI] [PubMed] [Google Scholar]
- 9.Lee YB, Yoon W, Lee YY, et al. Predictors and impact of hemorrhagic transformations after endovascular thrombectomy in patients with acute large vessel occlusions. J Neurointerv Surg 2019; 11: 469–473. [DOI] [PubMed] [Google Scholar]
- 10.Kaesmacher J, Kaesmacher M, Maegerlein C, et al. Hemorrhagic transformations after thrombectomy: risk factors and clinical relevance. Cerebrovasc Dis 2017; 43: 294–304. [DOI] [PubMed] [Google Scholar]
- 11.Fiorelli M, Bastianello S, von Kummer R, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct. Stroke 2011; 30: 2280–2284. [DOI] [PubMed] [Google Scholar]
- 12.Ota T, Shigeta K, Amano T, et al. Regionwide retrospective survey of acute mechanical thrombectomy in Tama, suburban Tokyo: a preliminary report. J Stroke Cerebrovasc Dis 2018; 27: 3350–3355. [DOI] [PubMed] [Google Scholar]
- 13.Wahlgren N, Ahmed N, Dávalos A, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet 2007; 369: 275–282. [DOI] [PubMed] [Google Scholar]
- 14.Khatri R, McKinney AM, Swenson B, et al. Blood-brain barrier, reperfusion injury, and hemorrhagic transformation in acute ischemic stroke. Neurology 2012; 79: S52–S57. [DOI] [PubMed] [Google Scholar]
- 15.Yoon W, Jung MY, Jung SH, et al. Subarachnoid hemorrhage in a multimodal approach heavily weighted toward mechanical thrombectomy with solitaire stent in acute stroke. Stroke 2013; 44: 414–419. [DOI] [PubMed] [Google Scholar]
- 16.Cucchiara B, Tanne D, Levine SR, et al. A risk score to predict intracranial hemorrhage after recombinant tissue plasminogen activator for acute ischemic stroke. J Stroke Cerebrovasc Dis 2008; 17: 331–333. [DOI] [PubMed] [Google Scholar]
- 17.Lou M, Safdar A, Mehdiratta M, et al. The HAT Score: a simple grading scale for predicting hemorrhage after thrombolysis. Neurology 2008; 71: 1417–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Strbian D, Engelter S, Michel P, et al. Symptomatic intracranial hemorrhage after stroke thrombolysis: the SEDAN score. Ann Neurol 2012; 71: 634–641. [DOI] [PubMed] [Google Scholar]
- 19.Mazya M, Egido JA, Ford GA, et al. Predicting the risk of symptomatic intracerebral hemorrhage in ischemic stroke treated with intravenous alteplase: Safe Implementation of Treatments in Stroke (SITS) symptomatic intracerebral hemorrhage risk score. Stroke 2012; 43: 1524–1531. [DOI] [PubMed] [Google Scholar]
- 20.Menon BK, Saver JL, Prabhakaran S, et al. Risk score for intracranial hemorrhage in patients with acute ischemic stroke treated with intravenous tissue-type plasminogen activator. Stroke 2012; 43: 2293–2299. [DOI] [PubMed] [Google Scholar]
- 21.Mishiro K, Imai T, Sugitani S, et al. Diabetes mellitus aggravates hemorrhagic transformation after ischemic stroke via mitochondrial defects leading to endothelial apoptosis. PLoS One 2014; 9: e103818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Benavente L, Larrosa D, Garcia-Cabo C, et al. Safety and efficacy of mechanical thrombectomy in acute ischemic stroke of anticoagulated patients-a prospective observational study. J Stroke Cerebrovasc Dis 2016; 25: 2093–2098. [DOI] [PubMed] [Google Scholar]
- 23.Pandhi A, Tsivgoulis G, Krishnan R, et al. Antiplatelet pretreatment and outcomes following mechanical thrombectomy for emergent large vessel occlusion strokes. J Neurointerv Surg 2018; 10: 828–833. [DOI] [PubMed] [Google Scholar]
- 24.Shi ZS, Liebeskind DS, Loh Y, et al. Predictors of subarachnoid hemorrhage in acute ischemic stroke with endovascular therapy. Stroke 2010; 41: 2775–2781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurre W, Aguilar-Pérez M, Martinez-Moreno R, et al. Stent retriever thrombectomy of small caliber intracranial vessels using pREset LITE: safety and efficacy. Clin Neuroradiol 2017; 27: 351–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ng PP, Larson TC, Nichols CW, et al. Intraprocedural predictors of post-stent retriever thrombectomy subarachnoid hemorrhage in middle cerebral artery stroke. J Neurointerv Surg 2019; 11: 127–132. [DOI] [PubMed] [Google Scholar]
- 27.Nikoubashman O, Reich A, Pjontek R, et al. Postinterventional subarachnoid haemorrhage after endovascular stroke treatment with stent retrievers. Neuroradiology 2014; 56: 1087–1096. [DOI] [PubMed] [Google Scholar]
- 28.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. [DOI] [PubMed] [Google Scholar]
- 29.Dzialowski I, Pexman JHW, Barber PA, et al. Asymptomatic hemorrhage after thrombolysis may not be benign. Stroke 2007; 38: 75–79. [DOI] [PubMed] [Google Scholar]
- 30.Peschillo S, Diana F, Berge J, et al. A comparison of acute vascular damage caused by aDaPT versus a stent retriever device after thrombectomy in acute ischemic stroke: a histological and ultrastructural study in an animal model. J Neurointerv Surg 2017; 9: 743–749. [DOI] [PubMed] [Google Scholar]