Highlights
-
•
Cerebrovascular disease as a risk factor for COVID-19 mortality.
-
•
Future studies will allow the development of risk scales in patients with COD19 and a history of stroke.
-
•
More clinical trials are need to explore the effect of history of stroke and COVID19.
Keywords: COVID-19, Stroke, Mortality
Abstract
Background and objectives
Past history of stroke has been associated with an increased risk of a new ischemic stroke. Several studies have indicated increased prevalence of strokes among coronavirus patients. However, the role of past history of stroke in COVID19 patients is still unclear. The purpose of this systematic review is to evaluate and summarize the level of evidence on past history of stroke in COVID19 patients.
Methods
A systematic review was performed according to the PRISMA guidelines was performed in PubMed, Embase, EBSCO Host, Scopus, Science Direct, Medline, and LILACS. Eligibility criteria: We evaluated studies including patients with diagnosis of COVID 19 and a past history of stroke. Risk of bias: was evaluated with the Newcastle- Ottawa Scale (NOS) and experimental studies were evaluated using the ROBINS-I scale.
Results
Seven articles out of the total 213 articles were evaluated and included, involving 3244 patients with SARS VOC 2 Disease (COVID19) of which 198 had a history of cerebrovascular disease. Meta-analysis of the data was performed, observing an increase in mortality in patients with a history of cerebrovascular disease compared to those with different comorbidities or those without underlying pathology (OR 2.78 95 % CI [1.42–5.46] p = 0.007; I2 = 49 %) showing adequate heterogeneity. The presence of publication bias was evaluated using the Egger test in a funnel plot, showing adequate. Asymmetry, indicating that there is no publication bias; however, due to the low number of included studies, we could not rule out or confirm the presence of bias.
Conclusions
The history of cerebrovascular disease was associated with a 2.78-fold increased risk of mortality compared to patients with other comorbidities or without underlying pathologies.
1. Introduction
Coronavirus infection had spread around the world at high speed, to rapidly became a pandemic [1]. On March 11, 2020, the world health organization (WHO) officially declares this disease as a pandemic, with an exponential increase in the number of cases, with social and economic implications [2,3]. Clinical predictors of mortality have been described in patients with underlying cardiovascular and metabolic diseases such as hypertension, diabetes, and hypothyroidism [4,5]. There is a growing interest in the study of clinical factors of severity and predictors of mortality that guide us to which patient special attention should be paid and thus optimize to the maximum the health systems of these patients at risk, however, the history of brain disease vascular is poorly studied [6,7]. A systematic review by Aggarwal et al. in 2020 shows an increased risk of a severe form disease i.e. COVID-19 secondary to infection by the SARS-COV 2 virus, without conclusive results in other clinical outcomes [17]. Multiple reports have linked COVID19 patients and the development acute ischemic stroke [21]. History of stroke had been associated with an increased risk of a new ischemic stroke. Few articles have dedicated the real value that the history of cerebrovascular disease (ischemic or hemorrhagic) has in the subsequent development of this disease, so this systematic review and meta-analysis is conducted to summarize the existing evidence on the impact on mortality of history of previous cerebrovascular disease in patients suffering from the disease known as COVID-19 [21].
2. Methods
A systematic review and meta-analysis was performed in accordance with the PRISMA Guidelines.
2.1. Search and inclusion criteria
A search for randomized clinical trials is performed in the following databases: PUBMED (until May 2020); Cochrane Injuries Group Specialized Registry (until May 2020); The Cochrane Central Register of Controlled Trials (The Cochrane Library) (until May 2020); MEDLINE (Ovid) until May 2020; EMBASE (Ovid); PubMed [http://www.ncbi.nlm.nih.gov/sites/entrez] (May 2020); in addition to the reference list of included studies and other relevant data in addition to potentially eligible studies. The search was constructed using Medical Subject Heading (MeSH) terms and descriptors, all combined with Boolean operators. The search was not limited by dates or languages.
2.2. The search strategy was as below
(“Stroke” OR “cerebral ischemia” OR “ischemic stroke” OR “cerebrovascular disease”) AND (“SARS-COV2 infection “OR” coronavirus “OR” COVID19 “OR” novel coronavirus”) AND (“mortality “OR” dead”) NOT (“aneurysmal subarachnoid hemorrhage” OR “Arteriovenous malformation bleeding” OR “traumatic brain injury” OR “traumatic ischemia”)
After applying the search strategy in databases and removing duplicates and extracting full text of potentially eligible studies, it is carried out independently, the studies included in the meta-analysis are chosen, disagreements were resolved by consensus. Case series, prospective and retrospective observational studies evaluating mortality from COVID19 including patients with a clinical history of cerebrovascular disease were included.
2.3. Assessment of quality and risk of bias
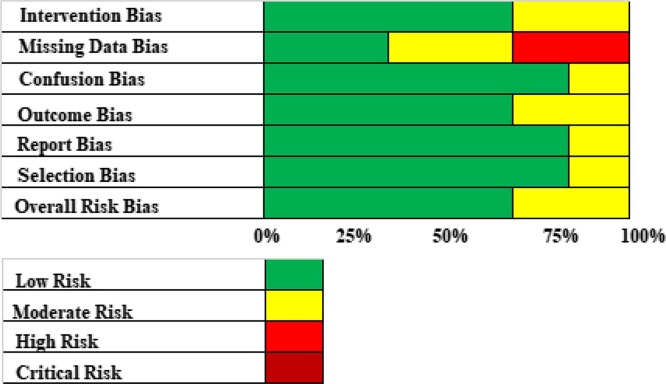
The outline followed was according to the recommendations of meta-analysis and systematic reviews of the PRISMA statement, for the presentation of systematic reviews, meta-analyzes, and the Cochrane manual of systematic reviews and meta-analyzes. The quality of the included studies was assessed through the Newcasttle Ottawa Scale (NOS), according to their score in low quality (less than 4 points), Moderate-High (5 points), High (6 and 7 points). [8]The risk of bias assessment was performed using the ROBINS-I scale that evaluates the risk of bias in "Low risk", "Moderate risk", "High risk", "Critical risk". in the domains "selection", "intervention", "missing data", "confusion", "measurement of results", "report" and an overall evaluation expressed in "global risk of bias" [9].
2.4. Extraction, management and statistical analysis of the data
The following data were extracted: COVID 19 patients with a history of cerebrovascular disease and mortality. Authors were contacted for missing data. Statistical analysis was performed using relative risk using the Mantel-Haenszel methodology for dichotomous variables with a randomized effect analysis model calculated using Review Manager 5.3 software. Heterogeneity was assessed by calculating I2, with high heterogeneity of the studies included in the analysis being above 60 %.
3. Results
3.1. Selection of studies
The selection process of the studies was based on the PRISMA foundations as shown in Fig. 1 . After carrying out the systematic search for information following our strategy, 213 bibliographic citations were identified, of which 30 were considered potentially eligible based on title or abstract, or both, and the full texts were obtained. After a full-text review, 20 studies were deemed eligible, 13 were not included as these were not meeting inclusion criteria (Fig. 1), and a total seven articles met the inclusion criteria for the review. Table 1 summarizes the characteristics of the included studies. (Supplementary material) The quality of included studies was assessed and it was found that three of the included studies obtained a score of five, considering that 42.28 % of the included studies were of moderate quality, three studies (42.28 %) were of moderate high quality obtaining a score of 6/7 and the one study obtained a score of 7/7, considering it the only included study of high quality (see Table 2 ). The risk of bias was evaluated for the different studies chosen using the ROBINS-I tool. It was found that overall, a low risk of bias was obtained in 71.43 % of the included studies and the bias of missing data is the one that presented the highest risk of bias with high risk of bias in 33 % of included studies (Fig. 2 ). Seven studies were chosen for the final analysis, involving 3244 patients with SARS VOC 2 Disease (COVID19) of which 198 had history of cerebrovascular disease. Meta-analysis of the data was performed, the study finding were, an increase in mortality in patients with a past history of cerebrovascular disease compared to those with a different medical history or those without any disease (OR 2.78 95 % CI [1.42–5.46] p = 0.007; I2 = 49 %) with adequate heterogeneity (see Fig. 3 ). The presence of publication bias was evaluated using the Egger test in a funnel plot with an adequate symmetry, indicating that there was no publication bias, however, due to the low number of included studies, we could not rule out or confirm the presence of bias (Fig. 4 ).
Fig. 1.
Process of study selection – Flow chart of our search strategy and inclusion and exclusion criteria.
Table 1.
Summary of the characteristics of the included studies.
| Study | Sample | Age | Outcomes assessed | Number of patients with a history of CVD | Follow-up |
|---|---|---|---|---|---|
| Chen et al 2020 [10] | 113 | 68 years old (37−88) | Mortality Severity Complications (heart failure, kidney failure, sepsis) |
10 | In Hospital |
| Grasselli et al 2020 [11] | 1591 | 63 years old (56−70) | Mortality Severity Complications (heart failure, kidney failure, sepsis) |
109 | 30 days |
| Guan et al 2020 [12] | 1099 | 47 years old (33−67) | Mortality Severity Complications (heart failure, kidney failure, sepsis) |
15 | In Hospital |
| Wang et al 2020 [13] | 107 | 51 years old (36−65) | Mortality Severity Evidence of co-infection Effectiveness of pharmacological therapy |
6 | 30 days |
| Yang et al 2020 [14] | 52 | 59.7 years (46.2−86.6) | Mortality | 7 | In Hospital |
| Zhao et al 2020 [15] | 91 | 46 years old (30−68) | Mortality Severity Effectiveness of pharmacological therapy Need for mechanical ventilation Complications (heart failure, kidney failure, sepsis) |
7 | In Hospital |
| Zhou et al 2020 [16] | 191 | 56 years old (46−67) | Mortality Severity Complications (heart failure, kidney failure, sepsis) |
44 | 30 days |
Table 2.
Quality assessment of studies included through the Newcasttle-Ottawa scale (NOS).
| Study | Representative sample | Size of the sample | Course of the information | Outcome not presented at the beginning of the study | Control of the confusion variable | Evaluation of the outcome | Period of monitoring | Total scale score Newcasttle Ottawa |
|---|---|---|---|---|---|---|---|---|
| Chen et al 2020 | ★ | ★ | ★ | ★ | ★ | 5/7 | ||
| Grasselli et al 2020 | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7/7 |
| Guan et al 2020 | ★ | ★ | ★ | ★ | ★ | 5/7 | ||
| Wang et al 2020 | ★ | ★ | ★ | ★ | ★ | ★ | 6/7 | |
| ★ | ★ | ★ | ★ | ★ | ★ | 6/7 | ||
| Zhao et al 2020 | ★ | ★ | ★ | ★ | ★ | 5/7 | ||
| Zhou et al 2020 | ★ | ★ | ★ | ★ | ★ | ★ | 6/7 |
Fig. 2.
Assessment of risk of bias using the ROBINS-I tool: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Fig. 3.
Forest plot for meta-analysis evaluating mortality risk in patients with a history of cerebrovascular disease and COVID-19.
Fig. 4.
Funnel plot that evaluates risk of bias who presents symmetry, quantified in the Egger’s test (Egger’s test = -0.01 p = 0.0123).
4. Discussion
This systematic review reports an analysis of 7 retrospective observational studies showing the clinical characteristics of patients with disease caused by the SARSCOV-2 virus which were conducted in Wuhan, China [10,[12], [13], [14], [15], [16]] and Lombardy, Italy patients with previous history of cerebrovascular disease and covid19 + showed an increase in mortality during the stay at hospital compared to patients with other type of comorbidity. Previous stroke’s history was reported in all this studies with low heterogeneity (I2 = 49 %).
Agrawal et al. conducted a systematic review in which 6 studies were included to asses’ mortality rates and severe form of disease in COVID19 patients, concluding that the previous history of cerebrovascular disease increased the risk of critical condition by 2,5 times; however, mortality didn’t show a significant result [17]. In this review, the search strategy and the inclusion criteria were “COVID19” AND “Stroke” connectors, however the outcomes were not included. We did not include certain type of studies such as series of cases in our analysis to try to avoid bias in the quality of the design [18] (Table 3 ).
Table 3.
Details Bias Risk Assessment using the ROBINS-1 tool for observational studies.
| Estudios | Bias related to intervention | Bias of Lost Data | Bias of confusion | Bias in the outcome | Bias of reporting | Bias of selection | Risk of global bias |
|---|---|---|---|---|---|---|---|
| Chen et al 2020 | Low | High | Moderate | Moderate | Low | Low | Moderate |
| Grasselli et al 2020 | Moderate | Moderate | Low | Low | Low | Low | Low |
| Guan et al 2020 | Low | Low | Low | Low | Low | Low | Low |
| Wang et al 2020 | Moderate | Moderate | Low | Moderate | Low | Low | Moderate |
| Yang et al 2020 | Low | Moderate | Low | Low | Low | Low | Low |
| Zhao et al 2020 | Low | High | Low | Low | Low | Low | Low |
| Zhou et al 2020 | Low | Low | Low | Low | Moderate | Moderate | Low |
As limitations we found the small number of patients with a history of CVD, mainly in studies carried out in Wuhan, China. The type of included studies is a persistent limitation because they are all retrospective observational, therefore no clinical conclusions or factors can be drawn to establish this as a risk factor, lack of follow-up more than 30 days, evaluation of characteristics were not evaluated fundamental as is the cognitive and functional prognosis, however, due to the world situation given by this virus, there is a limitation of health resources, which include human talent, so establishing possible risk factors is important in the situation of Pandemic, since, it helps to optimize health resources. These findings could provide a basis for future risk scales in the care of patients with COVID19 in intensive care units or emergency services.
We considered that there is an important participation of the hemostatic system and disseminated intravascular coagulation that is present in sepsis and in patients affected by COVID19. Coronavirus produces endothelial damage, leading to an increase in mortality in patients with previous endothelial damage, which includes diabetics, cardiac patients, and with a history of cerebrovascular disease [19,20].
5. Conclusions
The history of cerebrovascular disease is associated with a 2.78-fold increased risk of mortality compared to patients with other comorbidities or without underlying pathologies. However, prospective studies are needed, confirming cerebrovascular disease as a risk factor for COVID-19 mortality.
5.1. Summary of evidence
This systematic review gives an overview of the available literature on the role history stroke in the risk of mortality in COVID19 patients. This study only provides evidence 3b.
5.2. Limitations
Our study has some limitations. Most studies focused largely on an experimental level. All articles included in this review are peer-reviewed. There is a possibility of publication bias.
Finally, the inclusion of only articles in English and Spanish could affect the generalization of our findings.
Authors’ contributions
WF had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: WF. Acquisition of data: WF Analysis and interpretation of data: All authors. Drafting of the manuscript: All authors. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: All authors Administrative, technical, and material support: All authors. Study supervision: All authors.
CRediT authorship contribution statement
William Andrés Florez-Perdomo: Conceptualization, Methodology, Writing - original draft, Supervision, Writing - review & editing. Sergio Andrés Serrato-Vargas: Supervision. Pilar Bosque-Varela: Supervision, Writing - review & editing. Luis Rafael Moscote-Salazar: Supervision, Writing - review & editing. Andrei F. Joaquim: Supervision, Writing - review & editing. Amit Agrawal: Supervision, Writing - review & editing. Álvaro Ricardo Soto-Angel: Conceptualization, Methodology, Writing - original draft, Supervision. Leidy Tatiana Tovar-Montenegro: Conceptualization, Methodology, Writing - original draft, Supervision.
Acknowledgment
P.B.V received a predoctoral fellowship from the Fundacion Alfonso Martin Escudero (Spain). The authors have no conflict of interest to declare pertaining to this review.
References
- 1.Kofi Ayittey F., Dzuvor C., Kormla Ayittey M. Updates on Wuhan 2019 novel coronavirus epidemic. J. Med. Virol. 2020;92(4):403–407. doi: 10.1002/jmv.25695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Coronavirus. https://www.who.int/health-topics/coronavirus [Online]. Available from: URL:
- 3.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19 — Studies needed. N. Engl. J. Med. 2020 doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 4.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020:531–538. doi: 10.1007/s00392-020-01626-9. Epub 2020 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schiffrin E.L., Flack J.M., Ito S., Muntner P., Webb R.C. Hypertension and COVID-19. Am. J. Hypertens. 2020;33:373–374. doi: 10.1093/ajh/hpaa057. United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA – J. Am. Med. Assoc. 2020:1–8. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang J.J., Dong X., Cao Y.Y. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1001/jama.2020.5394. Epub ahead of print. 19 February 2020. DOI: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 8.Wells G., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P., Ga S.W., Zello G.A., Petersen J., Wells G.A. 2014. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses.http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp from: URL. [Google Scholar]
- 9.Sterne J.A.C., Hernán M.A., Reeves B.C., Savovic J., Berkman N.D., Viswanathan M., Henry D., Altman D.G., Ansari M.T., Boutron I., Carpenter J.R., Chan A.W., Churchill R., Deeks J.J., Hróbjartsson A., Kirkham J., Jüni P., Loke Y.K., Pigott T.D., Ramsay C.R., Regidor D., Rothstein H.R., Sandhu L., Santaguida P.L., Schünemann H.J., Shea B., Shrier I., Tugwell P., Turner L., Valentine J.C., Waddington H., Waters E., Wells G.A., Whiting P.F., Higgins J.P.T. ROBINS-I: a tool for assessing risk of bias in non- randomized studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368(March):1–14. doi: 10.1136/bmj.m1091. [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA – J. Am. Med. Assoc. 2020:1–8. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang D., Yin Y., Hu C., Liu X., Zhang X., Zhou S. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit. Care. 2020;24(1):188. doi: 10.1186/s13054-020-02895-6. https://ccforum.biomedcentral.com/articles/10.1186/s13054-020-02895-6 [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single- centered, retrospective, observational study. Lancet Respir. Med. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao X.Y., Xu X.X., Yin H.S., Hu Q.M., Xiong T., Tang Y.Y. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect. Dis. 2020;20(1):1–8. doi: 10.1186/s12879-020-05010-w. 201. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [Internet], Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aggarwal G., Lippi G., Michael Henry B. Cerebrovascular disease is associated with an increased disease severity in patients with Coronavirus Disease 2019 (COVID- 19): apooled analysis of published literature. Int. J. Stroke. 2020;0(0):1–5. doi: 10.1177/1747493020921664. [DOI] [PubMed] [Google Scholar]
- 18.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. Epub ahead of print. 3 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lillicrap D. Disseminated intravascular coagulation in patients with 2019- nCoV pneumonia. J. J. Thromb. Haemost. 2020;18(4):786–787. doi: 10.1111/jth.14781. Epub 2020 Mar 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020;109(May (5)):531–538. doi: 10.1007/s00392-020-01626-9. Epub 2020 Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conde Cardona G., Quintana Pájaro L.D., Quintero Marzola I.D., Ramos Villegas Y., Moscote Salazar L.R. Neurotropism of SARS-CoV 2: mechanisms and manifestations. J. Neurol. Sci. 2020;412 doi: 10.1016/j.jns.2020.116824. [DOI] [PMC free article] [PubMed] [Google Scholar]