Abstract
Purpose
The coronavirus disease 2019 (COVID-19) is associated with high rates of acute respiratory distress syndrome (ARDS). Prone positioning improves mortality in moderate-to-severe ARDS. Strategies to increase prone positioning under crisis conditions are needed.
Material and methods
We describe the development of a mobile prone team during the height of the crisis in New York City and describe characteristics and outcomes of mechanically ventilated patients who received prone positioning between April 2, 2020 and April 30, 2020.
Results
Ninety patients underwent prone positioning for moderate-to-severe ARDS. Sixty-six patients (73.3%) were men, with a median age of 64 years (IQR 53–71), and the median PaO2:FiO2 ratio was 107 (IQR 85–140) prior to prone positioning. Patients required an average of 3 ± 2.2 prone sessions and the median time of each prone session was 19 h (IQR 17.5–20.75). By the end of the study period, proning was discontinued in sixty-seven (65.1%) cases due to clinical improvement, twenty (19.4%) cases due to lack of clinical improvement, six (5.8%) cases for clinical worsening, and ten (9.7%) cases due to a contraindication.
Conclusion
The rapid development of a mobile prone team safely provided prone positioning to a large number of COVID-19 patients with moderate-to-severe ARDS.
Keywords: Coronavirus disease 2019 (COVID-19), Acute respiratory distress syndrome (ARDS), Prone positioning
Highlights
-
•
A mobile prone team can effectively prone intubated patients during crisis conditions.
-
•
A mobile prone team can be rapidly developed using redeployed healthcare workers.
-
•
Treating COVID-19 requires new strategies to provide standard of care practices.
1. Introduction
During the coronavirus disease 2019 (COVID-19) pandemic, an overwhelming majority of those requiring ICU level of care had acute hypoxemic respiratory failure requiring mechanical ventilation for acute respiratory distress syndrome (ARDS) [1]. ARDS is common. In one large observational study, 23.4% of patients requiring mechanical ventilation for acute respiratory failure met criteria for ARDS. Mortality from ARDS depends on severity, and ranges from 35 to 46% [2]. Prone positioning, when used in conjunction with low tidal volume ventilation, has been shown to significantly reduce mortality in moderate-to-severe ARDS [[3], [4], [5]]. Despite the evidence, the use of prone positioning in moderate-to-severe ARDS remains low [2,6]. Barriers to implementation of prone positioning include lack of provider recognition of ARDS, uncertainty of evidence, and resource utilization [2,3].
Our medical intensive care unit (MICU) instituted a prone positioning program in 2014 for the management of moderate-to-severe ARDS. The MICU Prone Program was a nursing-led initiative that trained MICU nurses in safe manual placement of patients with ARDS in the prone position. Indications for proning were based on prior evidence [4], including patients with moderate-to-severe ARDS with a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen (PaO2:FiO2) of <150 despite standard-of-care management with low-volume, low-pressure ventilation and adequate ventilator synchrony. Between 2014 and 2019, our MICU successfully proned seventy-nine patients, with increasing experience over time.
New York City was an epicenter of the coronavirus disease 2019 (COVID-19) pandemic. In the face of this pandemic, our hospital increased our ICU capacity by over 250% in the setting of a surge of critically ill COVID-19 patients with acute respiratory failure. ICUs were created throughout the hospital in non-traditional areas including operating rooms, medical-surgical floors, post-procedural observation units and in the emergency department. Additionally, other subspecialty ICUs, including neurologic, pediatric, post-surgical and cardiac were repurposed to treat primarily adult patients with COVID-19-associated acute respiratory failure and ARDS requiring mechanical ventilation. Many of these patients met criteria for moderate-to-severe ARDS, but ICU staff outside of the MICU were not familiar with prone positioning. In an effort to increase our ability to meet this demand, we rapidly developed and trained a mobile prone team, capable of servicing ICUs throughout the hospital. Here we describe the series of patients with moderate-to-severe ARDS treated during the COVID-19 pandemic with prone positioning.
2. Methods
2.1. Prone team development
The COVID-19 Prone Team at NewYork-Presbyterian – Columbia University Irving Medical Center was developed as a dedicated mobile team comprised of a MICU clinical nurse specialist (CNS), occupational therapists (OTs), and physical therapists (PTs), who were redeployed to this role from their usual clinical jobs. Twelve OTs and twelve PTs were trained to be part of the team during the height of the pandemic. They all had cardiopulmonary rehabilitation experience, and most have worked with ICU patients as part of our early mobilization program. In addition to knowledge of body mechanics and positioning critically ill patients, they had experience in securing airways, lines, drains, and monitoring devices in an ICU setting.
These therapists underwent prone positioning training, developed by the MICU CNS, based on education materials that had been previously developed for the MICU Prone Program.
The MICU CNS led the development of the MICU Prone Program and had developed its protocol and nursing policy. In addition, the MICU CNS was certified in wound, continence and ostomy (CWOCN) with experience in pressure injury prevention and treatment. Training included education in basic principles of ARDS management and indications for prone positioning. It involved review of an instructional video [4], repetitive demonstration of equipment usage and positioning techniques, communication exercises to enhance overall teamwork during positioning, and proper donning and doffing of personal protective equipment (PPE).
To simulate a typical patient, a manikin equipped with an endotracheal tube, central venous catheter, arterial line, chest tube, foley catheter, cardiac monitor leads and a pulse oximeter lead was used for practice of positioning technique. The team performed multiple iterations of placement in prone and supine positions (Supplemental Image S1), including emergent positioning. Roles for team members included: team leader, airway manager (AM), turn team, line manager, recorder and vital signs monitor. Outside of the simulation environment, the role of AM was filled by a member of the ICU treating team or respiratory therapy. Training emphasized safety checks during positions to avoid loss of the airway, chest tubes, the central venous line or the arterial line. To avoid staff injury the training emphasized the importance of team members moving in sync.
Patients were manually positioned with the Tortoise Turning and Positioning System Prone (Mölnlycke Health Care, Gothenburg, Sweden) consisting of two low-pressure air-filled pads and two fluidized positioners to support and offload the patient. When this system was not available sheets were used to aid in the procedure. Due to the rapidly growing need for prone positioning beyond the MICUs, this training was completed in only two days prior to team launch.
The COVID-19 Prone Team covered 14 separate ICUs, a combined total of 240 COVID ICU beds. Their day-to-day availability increased based on demand, up to 7 days a week, from 7 am to 7 pm at the peak, for 22 days. If a patient needed to be emergently repositioned outside of the COVID-19 Prone Team hours, they were repositioned by MICU nurses. In the event of cardiac arrest, if a patient could not be safely placed in the supine position, the protocol specified the prone position should be maintained for cardiopulmonary resuscitation in an effort to minimize risk of ventilator circuit disconnect with the associated risk of aerosolization of viral particles [7,8]. To date during this pandemic, our institution has not had a patient in cardiac arrest while in the prone position.
The daily COVID-19 Prone Team included the MICU CNS and five to six OTs and PTs. During proning, the MICU CNS and four therapists would enter the patient's room, and the remaining therapists acted as a scribe and runner and remained outside of the room. A note was placed in the electronic medical record indicating time, safety checklist, positioning of patient, and PaO2:FiO2 ratio prior to repositioning. A member of the primary ICU treating team was required to be present during repositioning to manage emergencies. All patients who were proned were deeply sedated and receiving neuromuscular blockade during their proning session and during repositioning as previously described [4,9], and in an effort to minimize risk of virus exposure to the COVID-19 Prone Team via ventilator circuit disconnect or coughing by the patient [10].
2.2. Indications for proning
Patients who met criteria for prone positioning by the mobile prone team included those who were invasively mechanically ventilated with ARDS and a PaO2:FiO2 < 150 despite standard-of-care management with low-volume, low-pressure ventilation and adequate ventilator synchrony, and required an FiO2 ≥ 60% with positive end-expiratory pressure (PEEP) ≥10; the same indications established prior to the COVID-19 pandemic. Contraindications included clinical or physical conditions that precluded safe prone positioning (Table 3). Patients remained prone for 16–24 h per session. This length of time depended on the COVID-19 Prone Team availability. Proning was continued if the PaO2:FiO2 remained <150 when supine with FiO2 ≥ 60% and PEEP ≥10. Proning was discontinued when the PaO2:FiO2 was ≥150 with FiO2 ≤ 60% and PEEP ≤10 while supine, if a patient did not tolerate positioning as determined by the treating team, or if the treating team declined.
Table 3.
Potential contraindications to prone positioning.
| Significant hemodynamic instability |
| Severe acidemia |
| Cerebral perfusion pressure < 30 mmHg |
| Increased ICP >30 |
| Pregnancy |
| History of difficult intubation or nasotracheal intubation |
| DVT treated for <2 days |
| Facial surgery or severe facial trauma |
| Massive hemoptysis |
| Pelvic fractures |
| Active intra-abdominal process |
| LVAD, BiVAD, IABP, ECMO |
| Inability to tolerate face down position |
| Serious burn (20% body surface area) |
| Unstable fracture |
| Spinal instability |
| Recent sternotomy or major abdominal surgery |
| Recent tracheostomy |
| Life-threatening cardiac arrhythmia within 24 h |
| Bronchopleural fistula |
ICP = intracranial pressure; DVT = deep vein thrombosis; LVAD = left ventricular assist device; BiVAD = biventricular assist device, IABP = intraaortic balloon pump; ECMO = extracorporeal membrane oxygenation.
2.3. Data collection and analysis
Baseline characteristics and clinical measures, including sex, age, height, weight, date of endotracheal intubation, date of prone position initiation, mechanical ventilator settings and Sequential Organ Failure Assessment (SOFA) score at time of prone position initiation were retrospectively collected for all patients treated by the COVID-19 Prone Team from April 2 through April 30, 2020. Further clinical measures and patient outcomes, including number of daily positionings completed, duration of proning, PaO2:FiO2 during proning, adverse events during proning, patient tolerance of prone positioning, days on mechanical ventilation, tracheostomy, and mortality were collected through May 14, 2020. Continuous variables were expressed as means (+/− Standard Deviation) and medians (Interquartile range). Categorical variables were summarized as counts and percentages. This study was approved by Columbia University Irving Medical Center Institutional Review Board (study number AAAT0603).
3. Results
Between April 2 and April 30, 2020, ninety patients were treated by the COVID-19 Prone Team. Of these ninety patients, thirteen required two unique proning episodes at separate time points during their hospitalization due to recurrent moderate-to-severe ARDS that met criteria for prone positioning. All patients requiring proning during this time were proned by this team, including within the MICUs. During this same period, 314 patients were admitted to our hospital with COVID-19 requiring invasive mechanical ventilation. Baseline characteristics of these patients are shown in Table 1 . The majority of patients who required prone positioning were men (73.3%), with a median age of 64 years (range 53–71). There was a high prevalence of comorbid hypertension (55.6%) and diabetes (46.7%). All of the ICUs, including those newly created during the COVID-19 pandemic, had patients treated by the COVID-19 Prone Team.
Table 1.
Baseline characteristics.
| Study Population | N = 90 |
|---|---|
| Age, median (IQR) | 64 (53–71) |
| Sex, n (%) | |
| Female | 24 (26.7) |
| Male | 66 (73.3) |
| Height, inches, mean ± SD | 66.1 ± 3.62 |
| BMI, median (IQR) | 29.4 (26.1–33.9) |
| Comorbidities, n (%) | |
| Hypertension | 50 (55.6) |
| Diabetes mellitus | 42 (46.7) |
| SOFA score on day of first prone session, mean ± SD | 10.3 ± 2.5 |
| ICU location, n (%) | |
| Medical | 15 (16.7) |
| Neurologic | 12 (13.3) |
| Cardiac | 13 (14.4) |
| Surgical | 10 (11.1) |
| Operating Room | 16 (17.8) |
| Medical/Surgical Floor Converted | 9 (10) |
| Pediatric | 6 (6.7) |
| Cardiothoracic | 7 (7.8) |
| Post-procedural observation units | 1 (1.1) |
| Emergency Department | 1 (1.1) |
| Tidal Volume at time of first prone session, cc/kg of predicted body weight, median (IQR) | 6.0 (5.5–6.26) |
| Median plateau pressure at time of first prone session, cm H20, median (IQR) | 30 (28–34) |
| PEEP prior to prone session, mean ± SD | 14 ± 3.96 |
| FiO2 prior to prone sessions, median (IQR) | 0.8 (0.7–1.0) |
| PaO2:FiO2 prior to prone sessions, median (IQR) | 107 (85–140) |
| Time from intubation to first prone session, days, median (IQR) | 6 (IQR 2–11) |
BMI = body mass index; SOFA = sequential organ failure assessment; ICU = intensive care unit; cc/kg = centimeters per kilogram; cm H20 = centimeters of water; PEEP = positive end expiratory pressure; FiO2 = fraction of inspired oxygen; PaO2 = partial pressure or arterial oxygen.
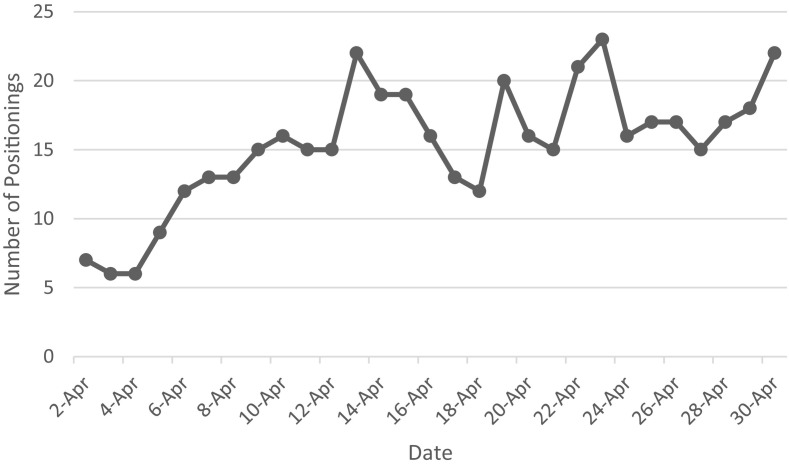
The median time between intubation and first prone session was 6 days (IQR 2–11). A total of 244 individual prone positionings were performed by the COVID-19 Prone Team during the study period. Patients were maintained in the prone position for a median of 19 h (IQR 17.5–20.75) per session. Patients required an average of 3 ± 2.2 sessions. The COVID-19 Prone Team completed an average of 15.3 ± 4.5 positionings per daily shift (Fig. 1 ).
Fig. 1.
Number of interventions per day: Daily number of interventions completed by the prone team. Includes placing in both the supine and prone position. X axis represents dates in April 2020.
By the end of the study period, proning was discontinued in sixty-seven (65.1%) cases due to improvement in gas exchange, in twenty (19.4%) cases due to lack of clinical improvement, in six (5.8%) cases for clinical worsening and in ten (9.7%) cases due to the development of a contraindication. Thirty-six patients died and 54 remained alive (Table 2 ). Recorded adverse events during prone sessions included peripheral intravenous line dislodgement in one patient, severe periorbital edema in one patient, brachial plexus injury in one patient, facial pressure injury in one patient, pressure injury to the ear in two patients and hypotension and hypoxemia in five patients requiring placement back into the supine position. No patients had a cardiac arrest while in the prone position.
Table 2.
Outcomes.
| Reason for Discontinuing Proning, n(%)a | N = 103 prone episodes |
|---|---|
| Improvement in gas exchange | 67 (65.1) |
| Lack of clinical improvement | 20 (19.4) |
| Clinical worsening | 6 (5.8) |
| Developed a contraindication | 10 (9.7) |
| Outcome at end of study period, n(%) | N = 90 unique patients |
| Dead | 36 (40) |
| Alive | 54 (60) |
| Extubated | 11 (20.4) |
| Remains orally intubated at end of study period | 17 (31.5) |
| Underwent Tracheostomy | 26 (48.1)) |
Thirteen patients required 2 unique proning episodes at separate time periods due to recurrent episodes of moderate-to-severe ARDS.
4. Discussion
The rapid implementation of the mobile COVID-19 Prone Team that travelled to multiple ICUs at our institution during the height of the COVID-19 pandemic, increased the ability to prone patients with moderate-to-severe ARDS. In a 28-day period, 90 patients were proned by this team with 244 individual proning sessions. After implementation of the COVID-19 Prone Team, more patients who met criteria for prone positioning were actually proned, as 12 patients intubated were proned between March 2, 2020 and March 31, 2020 [1] compared to 90 during the study period. By utilizing OTs and PTs who were familiar with critical illness and positioning patients, and by developing a careful but efficient training program, the COVID-19 Prone Team was able to safely provide an evidence-based intervention to critically ill patients with ARDS in a variety of ICU settings.
Prone positioning has been shown to have a mortality benefit in patients with moderate-to-severe ARDS, but has been underutilized due to provider under-recognition of ARDS, frequent misunderstanding of its indications, disbelief in quality of evidence, and resource utilization [11], which during times of crisis is more pronounced [2,12]. During the COVID-19 pandemic, the concentration of patients with moderate-to-severe ARDS increased considerably. This increase required rapid expansion of educational efforts on ARDS management. Additionally, as part of a clinical staffing strategy, critical care trained physicians provided clinical oversight across all ICU beds, allowing for relative consistency in the management of these patients with ARDS, as evidenced by the consistent use of a low tidal volume ventilation strategy, and identification of patients who met criteria for prone positioning. From a resource perspective, the staffing of a COVID-19 Prone Team with OTs and PTs available for redeployment during the crisis avoided additional strain on clinical nursing and other bedside clinicians who were already understaffed during this time. The ability to focus the training on a small group of individuals dedicated to proning appeared to enhance efficiency, expertise and safety.
This study has several limitations. While we are able to describe the characteristics of the patients treated, we have limited data to define the overall population of moderate-to-severe ARDS patients in our hospital during the study period. It is unclear what proportion of patients with moderate-to-severe ARDS received this therapy when indicated. Also, with limited data on the incidence of moderate-severe ARDS in our hospital prior to the COVID-19 pandemic, it is unclear if our proning rate changed with this implementation. However, prior to COVID-19, proning was only available to patients in the MICUs therefore limiting this treatment to the capacity of the MICU. Lastly, our outcomes data is limited by the study duration. At the end of the study, forty-five patients were still hospitalized, therefore the outcome of these treated patients is yet to be determined. However, of the fifty-four patients whose hospital survival is yet to be determined, thirty-six (80%) patients had prone therapy stopped due to clinical improvement.
The feasibility and success of the COVID-19 Prone Team has created the possibility of sustaining and even expanding prone positioning capabilities across our hospital network in case of a future crisis. Further education and training can be disseminated to nurses and clinicians working in non-medical ICUs, utilizing some of the training materials and personnel in the COVID-19 Prone Team.
5. Conclusions
During the COVID-19 pandemic, the rapid development and implementation of a mobile prone team allowed for increased capacity to prone patients with moderate-to-severe ARDS in ICUs beyond the MICUs to meet the surge of critically ill patients during the height of the pandemic. This was done effectively and with tolerable adverse outcomes.
Acknowledgments
Acknowledgements
We would like to acknowledge the physical therapist, occupational therapists and nurses who worked tirelessly on the COVID-19 Prone Team for their extraordinary efforts throughout this pandemic. We would also like to acknowledge our fellow healthcare workers for their dedication to outstanding patient care during this unprecedented pandemic and express our profound sympathy to our patients, their families and the community for all those who suffered during the pandemic.
Funding
None.
Declaration of Competing Interest
Dr. Brodie receives research support from ALung Technologies, he was previously on their medical advisory board. He has been on the medical advisory boards for Baxter, BREETHE, Xenios and Hemovent. Patrick Ryan reports honorarium from Mölnlycke Health Care. The other authors report no other conflicts of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcrc.2020.08.020.
Appendix A. Supplementary data
Supplementary material
References
- 1.Cummings M.J., Baldwin M.R., Abrams D., Jacobson S.D., Meyer B.J., Balough E.M. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in new York City: a prospective cohort study. Lancet. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellani G., Laffey J.G., Pham T., Fan E., Brochard L., Esteban A. Pesenti a, Investigators LS, group ET. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 3.Guerin C., Beuret P., Constantin J.M., Bellani G., Garcia-Olivares P., Roca O. Mercat a, investigators of the Apronet study group tRNtRrdlSFdA-R, the ETG. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS prone position Network) study. Intensive Care Med. 2018;44:22–37. doi: 10.1007/s00134-017-4996-5. [DOI] [PubMed] [Google Scholar]
- 4.Guerin C., Reignier J., Richard J.C., Beuret P., Gacouin A., Boulain T. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 5.Sud S., Friedrich J.O., Taccone P., Polli F., Adhikari N.K., Latini R. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. 2010;36:585–599. doi: 10.1007/s00134-009-1748-1. [DOI] [PubMed] [Google Scholar]
- 6.Fan E., Brodie D., Slutsky A.S. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319:698–710. doi: 10.1001/jama.2017.21907. [DOI] [PubMed] [Google Scholar]
- 7.Mazer S.P., Weisfeldt M., Bai D., Cardinale C., Arora R., Ma C. Reverse CPR: a pilot study of CPR in the prone position. Resuscitation. 2003;57:279–285. doi: 10.1016/s0300-9572(03)00037-6. [DOI] [PubMed] [Google Scholar]
- 8.Edelson D.P., Sasson C., Chan P.S., Atkins D.L., Aziz K., Becker L.B. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines((R))-resuscitation adult and pediatric task forces of the American Heart Association in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists: supporting organizations: American Association of Critical Care Nurses and national EMS physicians. Circulation. 2020;141(25):e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Papazian L., Forel J.M., Gacouin A., Penot-Ragon C., Perrin G., Loundou A. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 10.Alhazzani W., Moller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E. Surviving Sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1578. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gattinoni L., Coppola S., Cressoni M., Busana M., Rossi S., Chiumello D. COVID-19 does not Lead to a “typical” acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material